Abstract
Background.
Lack of discussion regarding actual asthma medication use by physicians with caregivers of children with asthma may result in low caregiver and physician concordance about prescribed asthma medications.
Objective.
The primary objective was to examine the concordance between primary care providers (PCP) and caregivers regarding child asthma medication use.
Methods.
Current asthma medications in the home with verification from each child’s PCP were obtained for 231 underserved children with persistent asthma. Kappas and chi-square statistics were calculated to measure the strength of the concordance. Caregiver and PCP dyads were categorized as concordant or discordant based on asthma medication use.
Results.
For all asthma prescriptions N = 479, two thirds of caregiver-PCP dyads (67.8) were categorized as concordant with at least one asthma medication. Concordance for asthma medications varied by type of medication ranging from 84% agreement for albuterol and 77% agreement for Flovent. In the final regression model predicting caregiver and PCP concordance, the number of PCP visits within the past 6 months and caregiver report of no limitation of child’s activity due to asthma were significantly higher in caregivers who were considered concordant with their child’s PCP while controlling for child age and frequency of symptom nights and number of ED visits in prior 6 months. In a model predicting the number of PCP visits, the number of ED visits was the only significant variable associated with the number of PCP visits while controlling for caregiver and PCP concordance.
Conclusion.
Caregiver and PCP concordance was significantly associated with increased number of PCP visits suggesting that increased exposure to a health care provider may increase agreement between a child’s PCP and caregiver regarding prescribed asthma medications. However, there may be other important factors including increased emergency department visits that may also be associated with subsequent pediatric primary care visits for asthma.
Keywords: asthma, concordance, children, inner-city
Introduction
Asthma is a complex respiratory disease characterized by underlying airway inflammation (1). National and international asthma guidelines recommend daily inhaled corticosteroids (ICS) as the cornerstone of treatment for patients with persistent asthma (1–5). However, several studies demonstrate an underutilization of inhaled corticosteroids (ICS) in underserved inner-city children with asthma (6–9) resulting in substandard, non–guideline-based care. Underutilization of ICS may result in over dependence on short-acting beta agonist (SABA) or rescue medications (10); one indicator of poorly controlled asthma. Furthermore, patient and caregiver safety concerns of daily ICS use by their child during asymptomatic periods may result in intermittent rather than daily use of ICS (11) or discontinuing ICS medications when their child is asymptomatic (12).
Effective preventive asthma care requires the parent or caregiver to accurately relay the child’s symptom frequency and pattern of rescue and controller medication use to the child’s primary care provider (PCP) to effectively monitor asthma control in the child during clinic visits (13–15). This type of caregiver and PCP communication occurs when caregivers and providers are in a partnership or “concordant” with the child’s treatment regimen (16). Both PCP and caregiver factors contribute to concordance with a child’s treatment regimen. It is estimated that very few PCPs routinely verify patient understanding or their beliefs about the health information provided to the patient or caregiver (17). Caregiver factors associated with discordance include lack of belief in the appropriateness of daily medication use without symptoms and concerns about side effects. Caregiver beliefs about asthma management were the most significant factor associated with caregiver-PCP discordance about asthma controller medications in a study of inner- city school-age children with asthma (18). Additional caregiver factors include passivity during interactions with their child’s PCP (16), or declining to discuss their specific reasons for non-adherence to a prescribed regimen due to lack of understanding or their beliefs in the ineffectiveness of anti-inflammatory medications. Ultimately, the lack of discussion between the care-giver and the child’s PCP regarding asthma medication use, albeit complex, may result in caregiver and PCP discordance regarding prescribed asthma medications (11, 19) resulting in non-adherence to prescribed medications.
The primary objective of this study was to examine the caregiver and PCP concordance regarding prescribed asthma medications in an inner-city sample of school-age children with persistent asthma. Concordance for controller medications including inhaled corticosteroids and rescue medications such as short-acting beta agonists was examined. We hypothesized that the concordance would be high for short-acting beta agonists but low for controller medications based on PCP and caregiver report.
Methods
Participants
Child study participants were recruited from pediatric emergency departments (ED) (72%) and community pediatric practices (28%) of two urban university hospitals in Baltimore, Maryland from December 2004 through December 2006. Eligible children were enrolled in a randomized clinical trial of an asthma communication educational intervention aimed at improving caregiver and child communication with child’s PCP as described in prior reports (20). Inclusion criteria for the 231 enrolled children included children 6 to 12 years of age with physician-diagnosed asthma, current use of asthma medications, or having 1 or more emergency department (ED) visit or hospitalizations during the prior 12 months. Caregivers were asked to identify the child’s PCP who prescribed the child’s asthma medications found in the home by the visiting nurse. The PCP was subsequently asked to verify the asthma medications that they had prescribed and that were demonstrated by the caregiver to be in the home.
Procedures
The study was approved by the Institutional Review Boards of the Johns Hopkins Medical Institutions and the University of Maryland Medical School. After obtaining written informed consent from each child’s caregiver, the caregiver and child received an asthma communication or standard asthma educational program delivered by a home visiting nurse (20). During the initial home visit, the nurse recorded all current asthma medications used by the child as reported by the caregiver and verified to be in the home. For example, the nurse asked the caregiver to show them all asthma medications that the child was currently using to treat their asthma including expired medications. The list of home asthma medications was faxed to the child’s PCP for verification that the medication had in fact been prescribed by the PCP in the past 12 months and to verify the dosage and frequency of administration for each medication. Expired medications were noted on the form sent to the PCP. The PCP was also asked to record any asthma medications not listed on the form that had been prescribed for the child within the past 12 months and then to fax the form to the study team. If there was no response from the PCP within one week, a follow-up fax was sent as a reminder. After a third attempt was made to receive the medication verification form for a PCP, the PCPs received a telephone call from the study team physician or coordinator to encourage completion of the medication verification form.
Symptom days and nights during the past 30 days, limitation of child’s activity due to asthma, presence of asthma action plan in the home, and number of ED and PCP visits during the past 6 months were measured using standardized items from International Asthma and Allergies in Childhood (ISSAC) study (21), NHANES Respiratory Health and Disease (2003–2004) Questionnaire (22) and several child respiratory health studies (23, 24). Asthma severity was assigned using national guidelines categories (2–4).
All asthma medications demonstrated in the home or reported by the PCP were categorized as rescue or controller medications. Rescue medications were defined as short-acting beta agonists (SABAs) and controller medications were defined as inhaled corticosteroids (ICS), leukotriene modifiers (LTM), mast cell stabilizers, and long-acting beta-agonists (LABAs). Common ICS medications encountered were fluticasone (Flovent, GlaxoSmithKline, Philadelphia, PA), budesonide (Pulmicort Turbuhaler and Respules, Astra Zeneca, Westborough, MA), and fluticasone/salmeterol (Advair, GlaxoSmithKline, Philadelphia, PA) inhalers.
Caregiver and PCP Concordance.
Caregiver and PCP concordance was defined as agreement between the caregiver record of medication in the home and the PCP’s verified list of prescribed asthma medications. Caregivers were categorized as “concordant” or able to demonstrate in the home all asthma medications that the child’s PCP prescribed or “discordant” otherwise disagreeing or lacking any asthma medication in the home that was prescribed by the child’s PCP. Discordance was defined as either (1) caregiver demonstrating an asthma medication in the home that was not verified by the PCP or (2) caregiver not demonstrating asthma medication in the home that was verified as prescribed by the PCP.
Data Analysis
Descriptive statistics, including ranges, means, and SDs, were calculated for all variables. Percentage agreement and the Kappa statistic, the index of the agreement against that which might be expected by chance, were used to measure caregiver-PCP concordance and were calculated for each type of medication. Level of agreement based on kappa values are defined as poor agreement: <0.40, moderate agreement: 0.41–0.60, substantial agreement: 0.61–0.80, and excellent agreement: >0.80 (25). Standard chi-square tests of independence and one-way analysis of variance (ANOVA) were used to examine differences by caregiver-PCP concordance category and child asthma severity, limitation of activity, frequency of symptom days and nights, number of emergency department (ED) visits, hospitalizations, PCP visits for asthma during the past 6 months, and presence of written asthma action plan in home. Several logistic regression models were used to model the probability of caregiver and PCP concordance. Variables significant at the 0.05 level in the bivariate analysis and those with theoretical importance (i.e., child age, symptom days and nights) were entered into the multiple logistic regression models. The final logistic model used to predict caregiver and PCP concordance included child age, number of symptom nights during the past 30 days, the number of PCP visits, and ED visits within the last 6 months and caregiver report of child’s activity limitation due to asthma. An alternate logistic regression model used to predict the number of PCP visits included the level of caregiver-PCP concordance, child age, number of symptom nights during the past 30 days, number of ED visits within the last 6 months, and caregiver report of child’s activity limitation due to asthma. Two-sided tests were used and p values ≤ 0.05 were considered significant. All data analyses were performed using SAS V.8.0 (26) and SPSS version 15 software (27).
Results
Sample Characteristics at Baseline
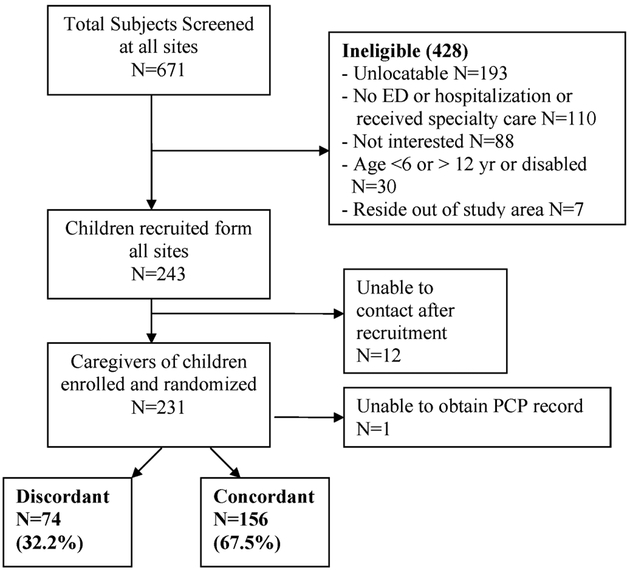
A total of 671 children with asthma were screened, 243 were eligible, and 231 were enrolled and randomized into the study (Figure 1). Study child participants were primarily male (60.6%), African American (92.6%) with a mean age of8.4 years (SD 2.0), and insured by Medicaid health insurance over the entire study period (83.1%) (Table 1). Caregivers of the study participants were primarily the child’s biological mother (87.5%), high school educated or higher (68%), and reported a mean household income of less than $30,000 (56%).
Figure 1.—
Recruitment and retention flow of subject participants.
Table 1.—
Baseline sociodemographic and health characteristics of the study population, N = 231.
| Characteristic | N(%) |
|---|---|
| Sociodemographic | |
| Child gender | |
| Male | 140 (60.6) |
| Female | 90 (39.0 |
| Missing | 1 (0.4) |
| Child race/ethnicity | |
| Black/African American | 214 (92.6) |
| White | 8 (3.5) |
| Asian or Pacific Islander | 1 (0.4) |
| Missing | 8 (3.5) |
| Child age (years) | |
| Mean (SD) | 8.4 (2.0) |
| Child health insurance | |
| Medicaid | 192 (83.1) |
| Private insurance | 33 (14.3) |
| Self pay/other | 6 (2.6 |
| Caregiver relationship to child | |
| Mother | 202 (87.5) |
| Father | 8 (3.5) |
| Grandmother | 12 (5.2) |
| Other relative | 9 (3.8) |
| Missing | 0 (0.0) |
| Caregiver education | |
| < 9th grade | 8 (3.5) |
| Some high school (9–11 grades) | 66 (28.6) |
| High school grad or GED | 88 (38.1) |
| Some college or trade school | 52 (22.5) |
| College grad | 17 (7.3) |
| Income | |
| < $10,000 | 57 (24.7) |
| $10,000–19,999 | 43 (18.6) |
| $20,000–29,999 | 30 (13.0) |
| $30,000–39,999 | 23 (9.9) |
| > $40,000 | 22 (9.5) |
| Refused/missing | 56 (24.2) |
| Child health characteristics | |
| Severity of asthma | |
| Mild intermittent | 52 (22.6) |
| Mild persistent | 111 (48.3) |
| Moderate persistent | 37 (16.1) |
| Severe persistent | 30 (13.0) |
| Activity limitation | |
| YES | 131 (56.7) |
| Symptom days over the past 30 days | |
| 0 | 40 (17.4) |
| 1–2 | 55 (23.8) |
| 3–5 | 70 (30.3) |
| 6–10 | 26 (11.3) |
| ≤ 11 | 39 (16.9) |
| Missing | 1 (0.4) |
| Health care utilization characteristics | |
| Number of admissions for asthma last 6 months | |
| 0 | 180 (77.9) |
| 1 | 36 (15.6) |
| 2 | 8 (3.5) |
| 3 or more | 7 (3.0) |
| Number ED visits last 6 months | |
| 0 | 35 (15.2) |
| 1 | 87 (37.7) |
| 2 | 53 (22.9) |
| 3 or more | 56 (24.2) |
| Written Asthma Action Plan in home | |
| YES | 92 (40.2) |
| Current controller medication use (caregiver-report) | |
| YES | 153 (66.2) |
Asthma morbidity was high with over half (57%) of caregivers reporting their child had a limitation of activity due to asthma. Most children were categorized with persistent asthma (77%) and over one quarter (29%) reporting six or more symptom days during the past 30 days. Use of rescue medication was high with most children reporting rescue medication use at some/a lot or all of the time (62%). Controller medication use was reported by only 66% of caregivers. Although few children were hospitalized for asthma in the past 6 months (22%), almost half (47%) of children had two or more ED visits for asthma during the same time period. Routine asthma care by the PCP was low in that 50% of all children received two or more PCP visits and 12% of children received no PCP visits during the prior 6 months. Only 21% reported receipt of specialty care for asthma within the past 24 months.
One hundred twenty-eight primary care providers treated the 231 study children. Most PCPs (83%) treated 2 or fewer study children. PCPs were primarily female (57%), a physician (96%), and experienced in practicing in private practice settings (42%) and inner-city neighborhoods (100%). (Table 2).
Table 2.—
Characteristics of primacy care providers, N = 128.
| Characteristic | N(%) |
|---|---|
| Gender | |
| Male | 49 (38) |
| Female | 73 (57) |
| Unknown | 6 (5) |
| Type of provider | |
| Physician | 123 (96) |
| Nurse practitioner | 5 (4) |
| Type of practice N = 55 | |
| Private practice | 23 (42) |
| Hospital-based clinic practice | 11 (20) |
| Community-based health care centers | 19 (34) |
| Unknown practice type | 2 (4) |
| Number of child subjects in study | |
| 1 | 83 (65) |
| 2 | 23 (18) |
| 3 | 12 (9) |
| 4 or more | 10 (8) |
Concordance and Discordance between Caregiver and PCP Reports of Asthma Medications
As seen in Figure 1, most of the 231 caregivers were categorized as concordant (68%) with one caregiver-PCP pair unable to be categorized due to lack of PCP verification of prescription records. For all asthma prescriptions N = 479, twothirds of caregiver-PCP dyads (67.8) were categorized as concordant with at least one asthma medication. However, caregiver-PCP concordance differed by type of medication prescribed (Table 3). Short-acting beta agonists had the highest percent caregiver and PCP agreement at 84.1 %, yet almost 16% of caregivers (n = 36) over-rated albuterol in the home that was discordant with the PCP verification record. Percent agreement for anti-inflammatory medications ranged from 63% to 84% with the lowest percent agreement calculated for Pulmicort (budesonide) at 63%. Flovent (fluticasone), the most frequently reported anti-inflammatory medication, had 77% agreement. Discordance between caregiver and PCP for all medications was primarily due to caregiver over-rating each type of medication with no PCP verification of the medication. The overall Kappa was moderate at 0.68 (CI: 0.63,0.72).
Table 3.—
Percent agreement between caregiver report and primary care provider report for child asthma medications, N = 479 medication listings.
| Medication name | Number of caregiver reports of medication use | Number of PCP reports of medication use | Total % agreement (caregiver report as denominator) | Discordance between caregiver and primary care provider |
|---|---|---|---|---|
| Albuterol (ProAir, Teva Specialty Pharmaceuticals, Miami, FL) | 227 | 193 | 191/227 (84.1) | Caregiver over-rating: 36 report albuterol with no PCP report |
| PCP over-rating: 2 report albuterol with no caregiver report | ||||
| Flovent (GlaxoSmithKline, Philadelphia, PA) | 99 | 83 | 76/99 (76.8) | Caregiver over-rating: 23 report Flovent with no PCP report |
| PCP over-rating: 7 report Flovent with no caregiver report | ||||
| Singulair (Merck & Co, Whitehouse Station, NJ) | 66 | 62 | 51/66 (77.3) | Caregiver over-rating: 15 report singulair with no PCP report |
| PCP over-rating: 11 report singulair with no caregiver report | ||||
| Advair (GlaxoSmithKline, Philadelphia, PA) | 37 | 35 | 31/37 (83.8) | Caregiver over-rating: 6 report Advair with no PCP report |
| PCP over rating: 4 report Advair with no caregiver report | ||||
| Pulmicort (Astra Zeneca, Westborough, MA) | 19 | 12 | 12/19 (63.2) | Caregiver over-rating: 7 report Pulmicort with no PCP report |
| 100% concordance for PCP and caregiver report of Pulmicort |
Kappa = 0.68 (95% CI: 0.63,0.72).
Significant unadjusted predictors of caregiver and PCP concordance included a higher mean number of PCP visits within the last 6 months (Concordant: 2.20 (SD 2.6); Discordant: 1.47 (SD1.3) visits, F = 5.23, df = 1, p = 0.02). A trend was noted in more caregivers of children in the discordant group reporting their child had limited activity due to asthma (Discordant: 65.8%; Concordant: 53.6%, X2 = 2.99, df = 1, p = 0.08) as well as a higher mean number of symptom nights in the past 30 days (Concordant: 4.40 [SD 7.3], Discordant: 6.39 [SD 10.6] nights; F = 2.80, df = 1, p = 0.09). There were no significant differences in caregiver and PCP concordance by asthma severity, the number of ED visits, and having an asthma action plan in the home or mean number of symptom days during past 30 days. The frequency of PCP visits during the past 6 months was not significantly associated with caregiver and PCP concordance (0–1 PCP visits during past 6 months: 46% concordant; 2 or more PCP visits during past 6 months: 54% concordant. X2 = 2.26, df = 1, p = 0.13).
In the final regression model predicting caregiver and PCP concordance as shown in Table 4, an increased number of PCP visits during the past 6 months and caregiver report of no limitation of child’s activity due to asthma were significantly associated with caregiver and PCP concordance while controlling for mean number of symptom nights during the past 30 days, the number of ED visits during the past 6 months, and child age. Results did not differ when examining models substituting mean number of symptom days during the past 30 days for mean number of symptom nights. In an alternate model of predicting PCP visits, the only variable significantly associated with the number of PCP visits during the past 6 months was the number of ED visits during the past 6 months while controlling for caregiver and PCP concordance, mean number of symptom nights during the past 30 days, and caregiver report of no limitation of activity due to asthma and child age.
Table 4.—
Unadjusted and adjusted variables predicting caregiver and PCP concordance for asthma medication use, N = 225.
| Variable | Unadjusted | Adjusted OR OR (95% CI) |
|
|---|---|---|---|
| Discordant N = 73 Mean (SD) |
Concordant N = 152 Mean (SD) |
||
| Mean symptom nights last 30 days | 6.39 (10.6) | 4.40 (7.3) | 0.98 (0.95, 1.01) |
| Mean PCP visits last 6 months | 1.47 (1.3) | 2.20 (2.6)* | 1.28 (1.03, 1.60)* |
| Mean ED visits last 6 months | 1.85 (1.8) | 2.15 (3.3) | 1.01 (0.94, 1.22) |
| Child age (years) | 8.14 (1.9) | 8.00 (1.9) | 0.99 (0.85, 1.15) |
| N (%) | N (%) | ||
| Activity limitation due to asthma YES versus NO | 48 (65.8) | 82 (53.6)** | 0.54 (0.29, 0.99)* |
p < 0.05
p = 0.08.
Discussion
The results of this study indicate fair agreement between the caregiver of a child and the child’s PCP regarding asthma medications administered in the home by the caregiver and prescribed by the PCP. The overall kappa value fell in the “substantial agreement” range (25) suggesting good concordance and communication between the caregiver and child’s primary care provider around asthma medication use. The concordance seen in our study, ranging from 63% to 84%, compares favorably with previous reports of concordance ranging from 42% for PCP and 32% for caregivers and a kappa of 0.54 in a comparable group of inner city children but only addressing controller medication (18). An increased number of PCP visits was significantly associated with concordance between the caregiver and PCP in the present study. One possible explanation is that an increase in the number of PCP visits resulted in increased exposure to the PCP and may have led to increased communication with the caregiver regarding medication use. Concordance relies on an open discussion with the patient and caregiver about the illness and treatment options and it is a dynamic concept requiring continual exploration (28). Agreement is reached after negotiation between the health care provider and caregiver regarding whether, when, and how the medication is administered to the child (16). The benefit of high caregiver and PCP concordance regarding child medication use is that medication decisions are overt (16) and caregivers are more forthcoming about nonadherence. Medication use concordance between the caregiver and PCP noted in this sample of children with asthma may indicate some level of agreement for child management of asthma that may not fit the NAEPP guidelines (2–4) but may be a compromise between the PCP and caregiver. For example, as reported by others, some caregivers may be willing to administer controller medications during their child’s asthma exacerbations but favor avoiding these medications when their child is asymptomatic (11). Appreciating that in reality caregivers ultimately make the decision to administer medication to their child (16) and openly discussing caregiver beliefs and concerns regarding asthma medications may increase the PCP’s likelihood of improving medication adherence in their patients.
Because only half of the caregivers reported two or more PCP visits and 12% reported no PCP visits for their child’s routine asthma care during the prior 6 months we examined factors associated with the number of PCP visits. The number of ED visits during the past 6 months was the only significant variable associated with the number of PCP visits during the same time. Just over half of the concordant dyads reported two or more visits with the child’s PCP. Insufficient contact with the child’s PCP may be the pathway for discordance as well as increased ED visits. Current asthma guidelines recommend ongoing, repetitive asthma self-management education that includes negotiating the goals of treatment, specific medications and actions to be taken to reach the goals of asthma control(4), and most likely requires a minimum of two non-urgent care visits per 12 months to achieve proficient self-management. However, lack of insurance reimbursement for asthma education, insufficient clinic time, and lack of trained staff for tailored, individualized asthma education are often cited by providers as barriers to providing routine asthma care.
Level of asthma severity and frequency of day and nighttime symptoms were not associated with concordance, consistent with prior studies of physician and parent concordance (18). However, caregivers reporting limitation of activity in their child due to asthma were more likely to be discordant with the child’s PCP for asthma medications. This may reflect poor asthma control in the child due to nonadherence to the prescribed regimen or lack of caregiver recognizing and/or communicating decreased activity level in their child to the PCP. Alternatively this may suggest caregiver tolerance of suboptimal respiratory status of the child or inappropriate expectation of child exercise capability.
There was uncertainty noted in agreement on albuterol use. Almost one of six caregivers reported albuterol in the home without PCP verification. This may indicate that child subjects were receiving rescue medication from other sources such as the emergency department or specialists. Availability of short-acting beta agonist medication is important for acute relief of asthma symptoms. Alternatively, it may reflect over-reliance on albuterol by the caregiver for the child’s symptom relief. Some PCPs may lack awareness of the increased number of albuterol refills for particular patients due to multiple prescribers, long-term refills, or telephone refills provided by non-medical office or pharmacy staff (29). Conversely, there may be a subgroup of children with appropriate inhaled corticosteroids use who remain symptomatic and require increased beta agonist use (e.g., children requiring pretreatment for exercise or exposure to viral illness or environmental allergens) resulting in concurrent use of quick relief and preventive medications.
Several issues may limit the generalizability of these findings. Most health care utilization outcomes were based on caregiver report without medical record verification of ED and PCP visits and hospitalizations. However, each PCP was asked to verify the frequency of ED and office visits for each child. Because achieving a high response rate from PCPs was critical to study outcomes, we did not request prescription date from each PCP to reduce time spent in review of medical record. Date of prescription would allow comparison of time of prescription written to time medication was filled and present in the home; however, this analysis is precluded in this study. Although we were able to observe the child’s actual asthma medications in the home, we are limited in determining actual medication use and adherence by the child in that filling medications does not reflect actual medication use or include prescriptions obtained from providers other than the respondent PCP. Finally, generalizability beyond this group of children is limited due to the selection bias in this sample. We purposely recruited children with more severe or uncontrolled asthma into this study as to maximize our ability to detect a difference in asthma morbidity between treatment groups related to the goals of the original randomized clinical trial (20).
In conclusion, concordance between the caregivers of children with asthma and the child’s PCP revealed an overall good concordance with the highest concordance in short-acting beta agonist medications. Concordance was significantly associated with increased number of PCP visits suggesting that increased exposure to a health care provider may increase communication regarding child asthma medication use and ultimately improve medication adherence.
Acknowledgment
This research was supported by the National Institute of Nursing Research. NR008544. The authors thank the families and primary care providers for their willingness to participate in this study.
References
- 1.Canonica GW. Treating asthma as an inflammatory disease. Chest 2006;130(1 suppl): 21S–28S. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Service. PHS, NIH, NHLBI. Expert Panel Report #2 Guidelines for the Diagnosis and Management of Asthma. National Asthma Education and Prevention Program (NAEPP), 1997. NIH Publication; 97–4051. [Google Scholar]
- 3.U.S. Department of Health and Human Service. PHS, NIH, NHLBI. Guidelines for the Diagnosis and Management of Asthma: Update on Selected Topics, 2002. National Asthma Education and Prevention Program (NAEPP), 2002. NIH Publication; 97–4051. [Google Scholar]
- 4.U.S. Department of Health and Human Service. NIH, NHLBI. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma Full Report 2007. National Asthma Education and Prevention Program (NAEPP), 2007. NIH Publication; 07–4051. August 2007. [Google Scholar]
- 5.Global Initiative for Asthma (GINA): Global Strategy for Asthma Management and Prevention: Revised 2002. Bethesda, MD, National Institutes of Health, National Heart, Lung and Blood Institute, 2002. [Google Scholar]
- 6.Diaz T, Sturm T, Matte T, Bindra M, Lawler K, Findley S, Maylahn C. Diaz T, Sturm T, Matte T, Bindra M, Lawler K, Findley S, Maylahn C. Medication use among children with asthma in East Harlem. Pediatrics 2000;105:1188–1193. [DOI] [PubMed] [Google Scholar]
- 7.Halterman JS, Yoos HL, Sidora K, Kitzman H, McMullen A. Medication use and health care contacts among symptomatic children with asthma. Ambul Pediatr 2001;1:275–279. [DOI] [PubMed] [Google Scholar]
- 8.Butz AM, Tsoukleris MG, Donithan M, Hsu VD, Zuckerman I, Mudd K, Thompson RE, Rand CS, Bollinger ME. Effectiveness of Home Nebulizer Education Intervention in Young Minority Children with Asthma. Arch Pediatric and Adolesc Med 2006;160:622–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butz AM, Tsoukleris MG, Donithan M, Thompson RE, Rand CS, Bollinger ME. Patterns of inhaled anti-inflammatory medication use in young under-served children with asthma. Pediatrics 2006;118:2504–2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonner S, Matte T, Rubin M, Fagan JK, Ahern J, Evans D. Oral beta2-agonist use by preschool children with asthma in East and Central Harlem, New York. J Asthma 2006;43:31–35. [DOI] [PubMed] [Google Scholar]
- 11.Bender BG, Bender SE. Patient-identified barriers to asthma treatment adherence: responses to interview, focus groups and questionnaires. Immunol Allergy Clin North Am 2005;25:107–130. [DOI] [PubMed] [Google Scholar]
- 12.Bender BG, Rankin A, Tran ZV, Wamboldt FS. Brief-interval telephone surveys of medication adherence and asthma symptoms in the childhood asthma management program continuation study. Ann Allergy Asthma Immunol 2008;101:382–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halterman JS, Yoos HL, Kaczorowski JM, McConnochie K, Holzhauer R, Conn KM, Lauver S, Szilagyi PG. Providers underestimate symptom severity among urban children with asthma. Arch Pediatric and Adoles Med 2002;156:141–146. [DOI] [PubMed] [Google Scholar]
- 14.Yoos HL, McMullen A. Symptom perception and evaluation in childhood asthma. Nurs Research 1999;48:2–8. [DOI] [PubMed] [Google Scholar]
- 15.Yoos HL, Kitzman H, McMullen A, Sidora K. Symptom perception in childhood asthma: How accurate are children and their parents? J Asthma 2003;40:27–39. [DOI] [PubMed] [Google Scholar]
- 16.Cushing A, Metcalfe R. Optimizing medicines management: From compliance to concordance. Therapeutics Clin Risk Manag 2007;3:1047–1058. [PMC free article] [PubMed] [Google Scholar]
- 17.Kettunen T, Poskiparta M, Limatainen L, Sjogren A, Karhila P. Taciturn patients in health counseling at a hospital: passive recipients or active participators? Qual Health Res 2001;11:399–410. [DOI] [PubMed] [Google Scholar]
- 18.Reikert KA, Butz AM, Eggleston PA, Huss K, Winkelstein M, Rand CS. Caregiver-Physician medication concordance and undertreatment of asthma among inner-city children. Pediatrics 2003;111:e214–e220. [DOI] [PubMed] [Google Scholar]
- 19.Cicutto L, Ashby M. The Importance of a Community-based asthma helpline. J Asthma 2007;44:705–710. [DOI] [PubMed] [Google Scholar]
- 20.Butz AM, Walker J, Land CL, Vibbert C, Winkelstein M. Improving asthma communication in high-risk children. J Asthma 2007;44:739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbold B, Stewart AW. International Study of asthma and allergies in childhood (ISSAC): rationale and methods. Eur Respir J 1995;8:483–491. [DOI] [PubMed] [Google Scholar]
- 22.National Health and Nutrition Examination Survey (NHANES) NCHS 1999–2006 Survey. Respiratory Health and Disease. www.cdc.gov/nchs/data/nhanes.
- 23.Nafstad P, Jaakkola JJK, Skrondal A, Magnus P. Day care center characteristics and children’s respiratory health. Indoor Air 2004;15:69–75. [DOI] [PubMed] [Google Scholar]
- 24.Jaakkola JJK, Kosheleva AA, Katsnelson BA, Kuzmin SV, Privalova LI, Spengler JD. Prenatal and postnatal tobacco smoke exposure and respiratory health in Russian children. Respir Res 2006;7:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen J Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 1968;70:213–220. [DOI] [PubMed] [Google Scholar]
- 26.SAS, Version 8.0 SAS Institute, Cary, NC: 1999. [Google Scholar]
- 27.SPSS Version 15.0. SPSS, Inc, Chicago, IL: 2006. [Google Scholar]
- 28.Elwyn G, Edwards A, Britten N. “Doing prescribing”: how doctors can be more effective. BMJ 2003;327:864–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ferrell CW, Aspy CB, Mold JW. Management of prescription refills in primary care: an Oklahoma physicians resource/research network (OKPRN) study. J Am Board Fam Med 2006;19:31–38. [DOI] [PubMed] [Google Scholar]