Abstract
Background:
To prevent diabetic foot disease, proper foot care is essential for early detection and treatment. Pharmacists are well suited to provide accessible foot care to adults with type 2 diabetes. Limited research has examined this role.
Methods:
We conducted a systematic review of community pharmacy–based and pharmacist-led foot care interventions for adults with type 2 diabetes compared to usual care. Data sources included MEDLINE, EMBASE, the Cochrane Library, CINAHL, Academic Search Complete and Health Source: Nursing/Academic Edition and Google Scholar, plus Google and hand-searching. Original research studies reported in English, focused on community pharmacy–based or pharmacist-led foot care interventions were eligible for review. Participants were adults with type 2 diabetes. Studies were summarized narratively; pooled data were not possible.
Results:
Seven studies were included in this review, 3 focusing on improving foot self-care behaviours and 4 on promoting foot examinations by the health care provider. Only 2 studies were randomized and were assessed as high quality. Six out of 7 studies reported significantly positive findings related to foot care practices.
Discussion:
An opportunity to influence foot care exists at each clinical encounter. Pharmacists are accessible health care practitioners and appropriate to provide a range of diabetes foot care interventions.
Conclusions:
Seven studies examined community pharmacy–based and pharmacist-led foot care interventions for people with type 2 diabetes. Community pharmacies and pharmacists are capable of providing a variety of foot care interventions to patients with diabetes, helping detect problems early and leading to prompt intervention.
Knowledge Into Practice.
Pharmacists are capable of providing a variety of foot care interventions to patients with diabetes in the community setting. Limited research has documented the role pharmacists play in foot care practices.
This study reports evidence from many sources, summarizing current community pharmacy–based and pharmacist-led foot care interventions.
This study may influence future pharmacy practice for patients with diabetes, emphasizing the inclusion of foot care interventions into diabetes care planning in the community pharmacy setting.
Mise En Pratique Des Connaissances.
En milieu communautaire, les pharmaciens sont en mesure d’effectuer un éventail d’interventions en matière de soins des pieds chez les patients atteints de diabète. Très peu de recherches ont documenté le rôle du pharmacien à cet égard.
Cette étude présente des données probantes issues de sources diverses et résume les interventions en matière de soins des pieds menées par des pharmaciens dans les pharmacies communautaires.
L’étude pourrait influencer la pratique future des pharmaciens en milieu communautaire en insistant sur l’inclusion d’interventions en matière de soins de pieds dans la planification des soins offerts aux patients atteints de diabète.
Background
Diabetic foot disease is a devastating complication of diabetes. The lifetime incidence of foot disease for people with diabetes has been consistently reported between 15% and 25%,1 with some estimates as high as 34%.2 For the individual, living with foot ulceration, infection and/or amputation can reduce quality of life3,4 and increase risk of death.5 For the community and society, foot infections are the leading cause of hospitalization for people living with diabetes6 and costly for all.
The management of diabetes-related foot complications contributes significantly to the high costs of diabetes care.7 Though amputation is the most severe foot-related complication with highest health care costs, foot ulceration can be considered the precursor.8 Here lies the potential for early intervention and management, preventing further invasive foot disease. Hopkins et al.6 estimated the economic burden associated with diabetic foot ulceration at CAN$540 million, and it is increasing over time. They call on improvements to the management, prevention and early treatment of foot ulcers to slow or halt the human and economic burden.6
Current best practice and clinical practice guidelines state that people with diabetes should examine their own feet daily, with clinical evaluation by a health care provider at least every 12 months.9 The literature has reported low rates of foot examinations,10 and creative new approaches are essential to change practices. Many foot disease prevention programs target primary care, including pharmacy settings, where the majority of diabetes-related encounters take place. There has been recent emphasis on team-based diabetes care, including family physicians, nurses, pharmacists, exercise specialists and dietitians. Many of these health care providers are equipped and knowledgeable to perform a foot exam or intervention. To date, limited work has been done to include community pharmacists in diabetic foot care; however, an opportunity exists at each clinical encounter, and many people with diabetes visit a pharmacy more regularly than other members of the care team.11 Bluml et al.12 reported that more than 93% of Americans live within 5 miles of a community pharmacy, implying patients have dependable access to pharmacists. The aim of this review was to assess the evidence of community pharmacy–based and pharmacist-led foot care interventions for adults with type 2 diabetes compared to usual care.
Methods
A research librarian designed and conducted searches for all available years in the following databases: MEDLINE, EMBASE, the Cochrane Library, CINAHL, Academic Search Complete and Health Source: Nursing/Academic Edition and Google Scholar. Google was searched twice, limited to the first 100 hits for both searches. References from identified systematic reviews were also searched for additional studies. Searches were restricted to the English language. No study design limits or age restrictions were applied. Key words and synonyms included the following: diabet*, foot*, pharm*, drugstore, druggist, apothecar*, dispensary, clinical monitoring, self-care, screening, wound management, pharmacist, podiatr*, chiropod*.
The inclusion criteria were full-text, original studies, published in English, with a community pharmacy–based or pharmacist-led intervention with a foot care component targeting adults with type 2 diabetes. Multicomponent programs with a foot-specific outcome were included, as well as those with either a self-care or health care provider (i.e., pharmacist) foot care focus. Those requiring a referral or located in a hospital/clinic/medical office were excluded. In addition, team-based care and programs where it was unclear which health care provider performed the foot care intervention were excluded.
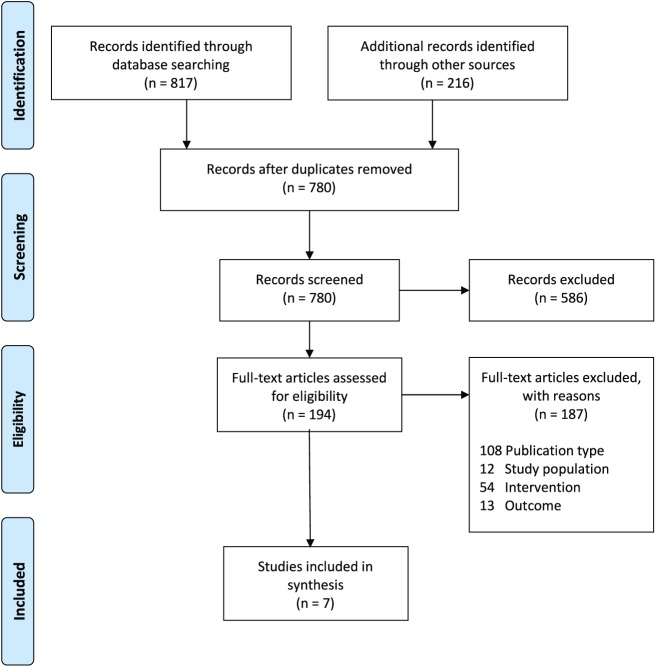
The study selection process is illustrated in Figure 1. Studies were abstracted into EndNote, version X7.8, where duplicate studies were removed. The studies were initially screened for title and abstract by one reviewer. Full-text studies were assessed for eligibility by 2 reviewers. Any discrepancies were discussed with a third reviewer until consensus was reached.
Figure 1.
PRIMSA flow diagram
The following data elements were extracted: general characteristics (author names, year published, country of implementation, study design, sample size, description of the intervention and outcome measured [foot care specific]) and study findings summarized (gender, age, duration of diabetes, baseline A1C). Quality of the included studies was assessed with the Downs and Black13 27-item checklist. This checklist allows the methodological quality assessment of both randomized and nonrandomized studies in 5 dimensions: reporting, confounding, bias, external validity and power. Two independent reviewers conducted the quality assessment separately, discussed discrepancies and came to consensus on scores. In the case of disagreement, a third reviewer was consulted. Studies were classified as either self-care or health care provider exam-focused interventions.
Results
Our database searches identified 817 articles (including Google Scholar). As well, 200 Google results and 16 hand-searched articles were examined. We removed 244 duplicates from the database searches and 9 Google duplicates, moving 780 results forward for initial screening; 402 database and 184 Google articles were removed based on title and abstract. Main exclusions in the initial screening were for animal studies, hospital/acute care settings and specific pharmacotherapy and surgical interventions. Two independent reviewers initially assessed 194 (171 database, 7 Google, 16 additional) articles; 187 were excluded due to the following reasons: 108 publication type (i.e., was not original research), 12 sample population (i.e., was not adults with type 2 diabetes), 54 intervention (i.e., was not pharmacy based or pharmacist led) and 13 outcome (i.e., did not have a foot care–specific outcome). Overall, 7 studies were included in this systematic review.
General characteristics of included studies
Three studies focused on improving foot self-care behaviours, and 4 studies focused on promoting foot examinations by health care providers (pharmacist or other) (Table 1). Six out of 7 studies were multicomponent programs with a foot care element, reporting foot care–specific outcomes as secondary outcomes. Two studies were designed as randomized controlled trials, 4 observational and 1 case study. Sample sizes varied from 28 to 1836. The study settings were international, with 2 from the Middle East, 1 from Europe and 4 from North America (3 from the United States and 1 from Canada).
Table 1.
Characteristics of included studies
| First author | Year | Country | Study design | Sample size | Description of intervention | Data collection time points | Foot care outcome reported |
|---|---|---|---|---|---|---|---|
| Improving foot self-care behaviours | |||||||
| Abduelkarem14 | 2009 | Dubai, UAE | Observational, pre-post comparison | 59 | Diabetes self-care reminders given every week for 3 months | B, 3, 6, 24 months | SDSCA |
| Jahangard-Rafsanjani15 | 2015 | Iran | RCT | 95 | Individualized consultation by pharmacist; 5 follow-up visits every month for 5 months | B, 5 months | SDSCA |
| Mehuys16 | 2008 | Belgium | RCT | 280 | Reminders about foot exams on each visit to pharmacy for 6 months | B, 6 months | SDSCA |
| Promoting foot exams by health care providers | |||||||
| Bluml12 | 2014 | United States | Observational, pre-post comparison | 1836 | Customized diabetes education by pharmacists, enforcing health goals and prevention of complications. Project IMPACT | B, 12 months | Rate of foot exam |
| Fera17 | 2009 | United States | Observational, pre-post comparison | 573 | Coaching by pharmacist regarding processes of care based on national guidelines (HEDIS), focused on clinical assessments and progress towards clinical and self-management goals. Diabetes Ten City Challenge | B, 12 months | Rate of foot exam |
| Pinto18 | 2012 | United States | Prospective, longitudinal | 228 | Individualized visits by pharmacist based on ADA guidelines, including annual foot exams (12 months) | B, 6, 12 months | Rate of podiatrist visit |
| Poulose19 | 2015 | Canada | Case study | 28 | NC-stat DPN check,* point-of-care testing of nerve conduction | B | NC-stat properties |
ADA, American Diabetes Association; B, baseline; HEDIS, Healthcare Effectiveness Data and Information Set; RCT, randomized controlled trial; SDSCA, Summary of Diabetes Self-Care Activities; UAE, United Arab Emirates.
NC-stat DPNCheck, manufactured by NeuroMetrix, Inc.
Quality assessment
Downs and Black13 27-item quality assessment scores are reported as percentages out of a total score of 32, with high-quality studies scoring greater than 50%, medium quality between 40% and 50% and low quality less than 39% (Table 2). Both randomized controlled trials scored over 50%, representing high-quality evaluation. One study scored 44%, and the remaining 4 studies scored 25% to 38%. The 3 highest scoring studies all focused on improving foot self-care behaviours, while the lower scoring studies all focused on promoting health care provider foot examinations.
Table 2.
Downs and Black13 quality assessment checklist scores
Overall findings
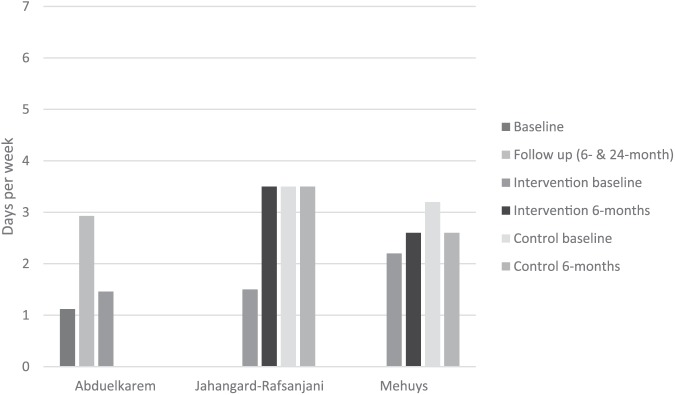
The studies reported in this systematic review varied in purpose, design, intervention and outcome; therefore, we are unable to pool any results. The overall summary of findings is reported in Table 3 and Figure 2.
Table 3.
Baseline characteristics of included studies
| First author | Gender, % male | Average age, years (±SD) | Average duration of diabetes, years (±SD) | Baseline A1C, % (±SD) |
|---|---|---|---|---|
| Abduelkarem14 | 46 | 51 (11.3) | 9 (3.6) | — |
| Jahangard-Rafsanjani15 | 40 | 56.6 (8.7) | 5.2 (5) | 7.6 (1.6) |
| Mehuys16 | 52.4 | 62.7 | — | 7.5 |
| Bluml12 | 42.8 | 54.1 (11.1) | — | 9.0* |
| Fera17 | 51 | 82% of participants >50 | — | 7.5 |
| Pinto18 | — | — | — | 7.14 (1.56) |
| Poulose19 | — | 64 (10) | 8 (6) | 71% of participants >7 |
—, Not reported.
Inclusion criterion was A1C >7%.
Figure 2.
Summary of findings among 3 studies using the Summary of Diabetes Self-Care Activities (SDSCA), average days per week performing foot self-care activities14,15,16
Six out of 7 studies reported an average age of over 50 years, with 40% to 52% of participants being male. The average duration of diabetes was reported in 3 studies and ranged from 5 to 9 years. Baseline A1C was reported in 6 studies, and 5 reported an average over 7%.
The 3 studies focused on improving foot self-care behaviours14,15,16 all used the Summary of Diabetes Self-Care Activities (SDSCA) as the outcome measure20 (Figure 2). All showed significant improvement in the number of days reported performing foot self-care from baseline to 5- or 6-month follow-up (p-value range from 0.02 to <0.001). Abduelkarem and Sackville14 extended the follow-up period to 24 months and found the number of days reported performing foot self-care returned to near-baseline values. The authors suggest that ongoing reminders are needed to support continued progress and achieve lasting behaviour changes.14 Despite reporting significant findings, the overall number of days reported performing foot self-care activities remained well below the recommended guidelines in all 3 studies.
The 3 studies measuring rates of health care provider foot exams or podiatrist visit12,17,18 all showed significant improvements from baseline to follow-up (12 months). These exams were performed, or the referral made, by a pharmacist.
One case study reported a point-of-care nerve conduction foot exam performed by a pharmacist in a community pharmacy. Poulose et al.19 found that the majority (57%) of participants had mild or moderate conduction abnormalities. This contrasted with their same-day survey findings of symptoms of diabetic peripheral neuropathy (DPN), where only 13 (46%) participants reported no signs or symptoms of DPN. The NC-Stat DPN check nerve conduction test detected abnormalities in 8 (61%) of these 13 participants who reported no signs or symptoms of DPN.
Discussion
Pharmacists are an important provider of many aspects of diabetes care. They are highly accessible, are community based, do not usually require appointments and are often open after hours. They are ideally positioned to provide a wide range of services to all types of patients.12 In this study, we have reported interventions including community pharmacists targeting both foot self-care activities, as well as foot examinations by health care providers. Both are extremely important in detecting early problems and prevention of foot disease progression. Our review reports 7 pharmacy-based and pharmacist-led interventions that resulted in improved foot care outcomes for adults with type 2 diabetes.
These 7 studies contribute to the best available evidence for pharmacy and pharmacist involvement in foot care for patients with diabetes. Various levels of pharmacist involvement were reported. Most studies were not randomized and were uncontrolled, with weak analyses; there are, however, some strengths of the individual findings and aspects to consider for future studies.
One study reported a direct pharmacist-led intervention in a community pharmacy setting, examining nerve conduction properties of patients with diabetes.19 This was a simple point-of-care test that took 5 minutes to complete. Their results showed that nerve conduction abnormalities can be detected in people without signs or symptoms of peripheral neuropathy. These data may easily be incorporated into care plans and strategies to prevent long-term neuropathy and complications. It is additional information to supplement the regular assessment of patients with diabetes by pharmacists or other health care providers.
Foot examinations are not a traditional pharmacist responsibility, nor are they typically reimbursed. Although these are well within pharmacists’ scope of practice, it may not be feasible in each setting or case. As well, compensation models would need to be developed, perhaps incorporating advanced practice certifications, for example. First, raising awareness among pharmacists about foot problems and their role in prevention is necessary. From there, novel interventions may be developed to screen, refer or remind patients with diabetes about foot care practices.
Strengths and limitations
This is the first systematic review aimed at examining community pharmacy and pharmacist involvement in foot care for people with type 2 diabetes. The findings here will help inform future interventions in this setting, targeting the prevention of foot disease. This study is not without limitations. First, only studies published in English were considered. Second, only 1 reviewer conducted the preliminary screening of titles and abstracts. Third, the Downs and Black13 quality assessment checklist did not assess the handling of missing data, and we did not consider them in our evaluation. Our final limitation is simply the variation in the studies included. This limited our interpretations and we were unable to pool any data.
Clinical implications for the pharmacist
Foot care for people with diabetes is multifaceted, and there is room for pharmacist involvement in many aspects. Simple reminders for foot self-care at prescription refills, such as those that Mehuys et al.16 studied, may be effective, or other coaching/advocating for health care provider examinations, as in Fera et al.,17 may be more feasible. This review shows that an opportunity exists to promote foot care practices and recommendations at each clinical encounter, and the community pharmacy setting is accessible and ideal for many types of interventions focused on diabetes foot care.
Conclusion
This systematic review identified 7 studies examining the role of community pharmacy–based and pharmacist-led foot care interventions for people with type 2 diabetes. All the studies reviewed reported that pharmacy-based and pharmacist-led interventions resulted in improved foot care outcomes. Regular foot self-care and health care provider examinations play a major role in the early detection of foot problems. Early detection leads to early intervention, reducing costly potential hospitalization and amputation. Community pharmacies and pharmacists are well positioned to provide a variety of foot care interventions to patients with diabetes. Further research regarding the best type of intervention is crucial to respond to the current diabetes epidemic.
Footnotes
Author Contributions:AS initiated and designed the project. LT designed and performed the search strategy. AS and VS performed the review and appraisal. DTE acted as the third reviewer. DTE and JAJ supervised the data extraction and appraisal, as well as provided overall guidance for the project. All authors reviewed the final draft of the manuscript.
Declaration of Conflicting Interests:The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Financial Acknowledgements:No external funding or industry sponsorship was received to conduct this project.
Access:Complete search strategy and data are available upon request to the corresponding author.
ORCID iD:Allison L. Soprovich  https://orcid.org/0000-0002-6143-1555
https://orcid.org/0000-0002-6143-1555
References
- 1. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA 2005;293(2):217-28. [DOI] [PubMed] [Google Scholar]
- 2. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med 2017;376(24):2367-75. [DOI] [PubMed] [Google Scholar]
- 3. Yekta Z, Pourali R, Ghasemi-Rad M. Comparison of demographic and clinical characteristics influencing health-related quality of life in patients with diabetic foot ulcers and those without foot ulcers. Diabetes Metab Syndr Obes 2011;4:393-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ribu L, Hanestad BR, Moum T, Birkeland K, Rustoen T. A comparison of the health-related quality of life in patients with diabetic foot ulcers, with a diabetes group and a nondiabetes group from the general population. Qual Life Res 2007;16(2):179-89. [DOI] [PubMed] [Google Scholar]
- 5. Walsh JW, Hoffstad OJ, Sullivan MO, Margolis DJ. Association of diabetic foot ulcer and death in a population-based cohort from the United Kingdom. Diabet Med 2016;33(11):1493-8. [DOI] [PubMed] [Google Scholar]
- 6. Hopkins RB, Burke N, Harlock J, Jegathisawaran J, Goeree R. Economic burden of illness associated with diabetic foot ulcers in Canada. BMC Health Serv Res 2015;15:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barshes NR, Saedi S, Wrobel J, Kougias P, Kundakcioglu OE, Armstrong DG. A model to estimate cost-savings in diabetic foot ulcer prevention efforts. J Diabetes Complications 2017;31(4):700-7. [DOI] [PubMed] [Google Scholar]
- 8. Boyko EJ, Ahroni JH, Cohen V, Nelson KM, Heagerty PJ. Prediction of diabetic foot ulcer occurrence using commonly available clinical information: the Seattle Diabetic Foot Study. Diabetes Care 2006;29(6):1202-7. [DOI] [PubMed] [Google Scholar]
- 9. Committee DCCPGE. Diabetes Canada Clinical Practice Guidelines Expert Committee Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes 2018;42(Suppl 1):S1-S325.29650079 [Google Scholar]
- 10. Al Sayah F, Soprovich A, Qiu W, Edwards AL, Johnson JA. Diabetic foot disease, self-care and clinical monitoring in adults with type 2 diabetes: the Alberta’s Caring for Diabetes (ABCD) cohort study. Can J Diabetes 2015;39(Suppl 3):S120-6. [DOI] [PubMed] [Google Scholar]
- 11. Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy 2008;28(4):421-36. [DOI] [PubMed] [Google Scholar]
- 12. Bluml BM, Watson LL, Skelton JB, Manolakis PG, Brock KA. Improving outcomes for diverse populations disproportionately affected by diabetes: final results of Project IMPACT: Diabetes. J Am Pharm Assoc 2014;54(5):477-85. [DOI] [PubMed] [Google Scholar]
- 13. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52(6):377-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abduelkarem AR, Sackville MA. Changes of some health indicators in patients with type 2 diabetes: a prospective study in three community pharmacies in Sharjah, United Arab Emirates. Libyan J Med 2009;4(1):29-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jahangard-Rafsanjani Z, Sarayani A, Nosrati M, et al. Effect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trial. Diabetes Educ 2015;41(1):127-35. [DOI] [PubMed] [Google Scholar]
- 16. Mehuys E, De Bolle L, Van Bortel L, et al. Medication use and disease management of type 2 diabetes in Belgium. Pharm World Sci 2008;30(1):51-6. [DOI] [PubMed] [Google Scholar]
- 17. Fera T, Bluml BM, Ellis WM. Diabetes Ten City Challenge: final economic and clinical results. J Am Pharm Assoc 2009;49(3):383-91. [DOI] [PubMed] [Google Scholar]
- 18. Pinto SL, Bechtol RA, Partha G. Evaluation of outcomes of a medication therapy management program for patients with diabetes. J Am Pharm Assoc 2012;52(4):519-23. [DOI] [PubMed] [Google Scholar]
- 19. Poulose S, Cheriyan E, Poulose A, Cheriyan R, Vadakkanezath B, Ziemer P. Usefulness of the NC-stat DPNCheck nerve conduction test in a community pharmacy as an educational tool for patients with diabetes. Can Pharm J (Ott) 2015;148(1):17-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000;23(7):943-50. [DOI] [PubMed] [Google Scholar]