Abstract
Objectives:
Despite increased awareness of obesity-related health risks and myriad treatment options, obesity still affects more than one-third of persons in the United States and is a substantial public health problem. Studies show that physicians play a key role in obesity prevention and treatment. The objective of this study was to examine the extent to which obesity is diagnosed and treated at the level of patient-physician interaction.
Methods:
We used data from the National Ambulatory Medical Care Survey (NAMCS), a nationally representative data set of US physician office visits. We estimated the number of obesity diagnoses and prescriptions of weight-loss management solutions (exercise counseling, diet counseling, or weight-loss drugs) in clinical practice from 1996 through 2014. We also calculated rates of obesity diagnosis and compared these rates with national rates of obesity based on body mass index data from the Behavioral Risk Factor Surveillance System (BRFSS) for the same period.
Results:
The estimated number of weight gain–related physician office visits increased from 2.3 million in 1996 to a peak of 7.6 million in 2012, and then fell to 4.5 million in 2014. National estimates of obesity diagnoses resulting from physician office visits ranged from 7.1 million in 1996 to 12.7 million in 2014 and substantially outnumbered the estimates for weight gain–related physician office visits throughout the study period. Estimates of exercise counseling and diet counseling and weight-loss medication prescriptions resulting from physician office visits fluctuated over time but never exceeded obesity diagnoses. When compared with national rates of obesity from the BRFSS, rates of obesity diagnoses resulting from physician office visits were substantially lower in the NAMCS (17%-30% vs 1%). National trends for weight-loss medication prescriptions closely mirrored those of weight gain–related physician office visits, even though fluctuations were substantial.
Conclusions:
Our results suggest that obesity is largely underdiagnosed and undertreated in clinical encounters. Future studies should investigate the structural changes needed to better engage physicians in obesity prevention and care. Practitioners should also reflect on their biases in treating obesity as a chronic disease.
Keywords: obesity, obesity management, primary care, patient-physician interaction, medicalization
The prevention and treatment of obesity is a public health priority in the United States.1 During 2013-2014, an estimated 70.6% of US adults aged >20 had excess weight or obesity (ie, had body mass index [BMI] >25 kg/m2 to 40 kg/m2), and 7.7% had extreme obesity (ie, BMI >40 kg/m2).2 Obesity is associated with increased mortality and serious comorbidities, including type 2 diabetes mellitus, cardiovascular disease, stroke, and some types of cancer.1,3-5 Annual costs related to obesity are about $147 billion.6
Despite increased recognition, research, and myriad available treatments, obesity rates among adults aged ≥20 have steadily increased in the United States during the past 4 decades, from 15% in 1976-1980 to 34% in 2007-2008 and to 39.6% in 2015-2016.7,8 By 2030, approximately half of the US population may have obesity.9 Although effectively addressing this public health problem will require comprehensive efforts from multiple stakeholders (eg, public health agencies, communities, and individuals), studies show that physicians play an important role.10-12 Physician-initiated obesity screenings, counseling, and interventions are linked to improved weight and health outcomes.12 However, even with widespread recognition among medical professionals that obesity is a disease, tools for prevention and treatment appear to be underused in the clinic encounter.11 We hypothesize that the incomplete medicalization of obesity at the level of patient-physician interaction—in other words, the disconnection between the conceptualization of obesity as a disease and its treatment—is one factor that contributes to the growth and persistence of obesity as a public health problem.
Medicalization is the process whereby nonmedical concerns become described, accepted, and treated as medical problems with medical solutions.13,14 The effects of medicalization on individual health and public health may be largely positive (eg, decreased maternal mortality)15 or negative (eg, overuse of expensive, potentially harmful medical technologies), but most medicalization processes result in both positive and negative effects.16 The medicalization process has 3 levels: (1) conceptual (medical definitions are created and used), (2) institutional (disease conceptualizations are codified), and (3) interactional (patient-physician interaction).13 These levels are mutually influential. For example, changes in institutional policy may affect conceptualizations of disease and the patient-physician interaction.17
Fully medicalized disorders (eg, epilepsy, diabetes) are legitimized at all 3 levels: conceptual, institutional, and interactional. Other disorders are incompletely medicalized, with medicalization occurring at only 1 or 2 levels. For example, although diagnostic codes for internet addiction do not exist, internet addiction is treated with behavioral and pharmaceutical interventions14 and, thus, is an example of incomplete medicalization.18
Obesity is another example of an incompletely medicalized disorder. Obesity has evolved from a descriptor of physical corpulence and/or a moral failing19 to a chronic illness with many negative health effects.20 In 2013, the American Medical Association officially declared obesity a disease.21
Previously, however, multiple institutions (eg, US Food and Drug Administration, National Institutes of Health, the Centers for Disease Control and Prevention) framed obesity as a disease21 (ie, a biological malfunction linked to multiple pathological outcomes) that is measurable via standardized BMI cutoffs. Obesity’s reconceptualization and institutional stakeholder buy-in are cited as important for the medicalization of obesity at the conceptual and institutional levels, which has resulted in insurance coverage for some obesity treatments.21
Current obesity treatment options include surgery, behavior modification, and pharmacotherapy. These treatments, as well as physician screening and counseling, may have positive effects on the patient.11,22-24 Patients advised by their physicians to engage in weight-related behavior modification show more confidence and motivation to make dietary changes and increase their physical activity levels.25 According to a US Preventive Services Task Force assessment, screening for obesity and/or referring adults to intensive behavioral interventions have minimal risk and are associated with improvements in weight status and obesity-related comorbidities.12 Multifaceted behavioral interventions (eg, diet, behavioral strategies, and physical activity) combined with long-term intensive clinician contact are even more effective than interventions targeting a single health behavior.22 In addition, behavioral interventions in combination with pharmacotherapy can result in weight loss and improved physiological outcomes.23 Although pharmacotherapy options are limited and may have undesirable side effects (eg, headache, nausea, gastrointestinal side effects), when prescribed with lifestyle interventions, weight-loss medications approved for long-term use produce additional weight loss ranging from 3% to 9% of initial weight.24 Even modest (5%-10%) reductions in weight are associated with improvements in fasting plasma glucose, systolic and diastolic blood pressure, and plasma lipid profiles.26
Despite medicalization at the conceptual and institutional levels and evidence of effective counseling and treatment options, obesity may be underdiagnosed and undertreated in clinical settings.27-29 A study published in 2017 found that among patients with obesity, the rate of weight counseling during primary care visits had decreased by 10% from 1995-1996 to 2007-2008, despite rising obesity prevalence and awareness of the health harms of obesity.30 An evaluation of a large US primary care database found that only 20% of patients with obesity were given an obesity diagnosis, and only 40% received an obesity management plan.31 Furthermore, in comparison with the proportion of Americans who were obese, in 2011, only an estimated 1.2% of US adults (2.74 million) were taking weight-loss medication.32 Suboptimal obesity management in primary care prompts questions about where the disconnection between the national recommendations and policies to improve obesity management and the patient-physician interaction may occur. Further medicalization of obesity at the patient-physician interaction level has risks, including increased expenditures and pharmaceutical side effects; however, obesity experts indicate that the benefits outweigh the risks.33,34
We analyzed quantitative trends in obesity-related physician office visits to explore the degree to which obesity was diagnosed and treated as a medical problem at the level of the patient-physician interaction. We used nationally representative data from 1996-2014 to compare population estimates of obesity prevalence against trends in physician office visits due to weight gain and physician office visits that resulted in obesity diagnoses, weight-loss drug prescriptions, diet counseling, and exercise counseling. For medicalized conditions, the number of diagnoses and treatments typically outpace the rate at which an ailment is listed as a reason for a physician office visit, signaling that the condition is conceptualized by physicians as a commonplace pathology of concern (medicalized at the conceptual level), and preexisting diagnostic codes and/or treatments are available (medicalized at the conceptual and institutional levels).16 Alternately, lack of medicalization or incomplete medicalization would be reflected in (1) higher rates of obesity as a reason for a physician office visit relative to the rates of diagnoses and treatments and/or (2) higher rates of obesity reflected in epidemiological data relative to the rates of diagnoses and treatments emerging from physician office visits.
Methods
Sample
We used data from the National Ambulatory Medical Care Survey (NAMCS),35 a nationally representative study of physician office visits conducted by the National Center for Health Statistics. The NAMCS collects data on health care use during patient visits to non–federally funded, community, and office-based physician practices across the United States. The NAMCS uses a multistate probability sampling design, which consists of sampling from primary sampling units (eg, counties), physicians within primary sampling units, and patients within physician practices. Each year, a randomly selected sample of physicians is assigned to a 1-week reporting period. Visits are randomly selected from the patient visit list. About 30 patient record survey forms are completed during the assigned week by the physician, office staff members, or US Census Bureau representatives. Recorded data include patient demographic characteristics, reason for visit, diagnosis, and treatment. We used 1996-2014 visit-level data for patients aged ≥18. Publicly available data were de-identified; as such, this study was considered exempt from review by the University of Kentucky and Utah State University institutional review boards.
Measures
We created and assessed 5 binary measures based on coded or write-in responses to the patient record forms: (1) obesity diagnosis, (2) weight gain as reason for visit, (3) weight-loss drug prescriptions given, (4) exercise counseling ordered, and (5) diet counseling ordered. In 2012, the NAMCS replaced the pen-and-paper data collection mode with computer-assisted data collection about the reason for patient visits, diagnoses, and medications prescribed. In addition, community health centers were excluded starting in 2012; to maintain consistency during the period of analysis, we removed those observations from the 1996-2011 survey years.
Obesity diagnosis
NAMCS allows up to 3 diagnoses to be recorded in the patient record. Using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)36 codes, we defined obesity diagnosis as a result of any physician office visit in which 1 of the diagnoses recorded was 278.00 (obesity) or 278.01 (morbid [severe] obesity).
Weight gain–related physician office visit
NAMCS provides up to 3 reasons for visit classifications per physician office visit, based on the patient’s motivation for seeking care. We defined a weight gain–related physician office visit as any visit that was assigned a reason for visit code of 1040.00 (patient report of “fat pads,” “fatty deposits,” “obesity,” “overweight,” or “too fat” as reason for visit).
Weight-loss drug prescriptions
From 1996 through 2002, physicians, office staff members, or US Census Bureau representatives recorded up to 6 types of medications in the patient medical chart that were prescribed as an outcome of the physician office visit. From 2003 through 2011, they listed up to 8 medications; during 2012-2013, they listed up to 10 medications; and in 2014, they listed up to 30 medications. Because the average number of medications prescribed did not vary from 2003 to 2014, we did not limit the number of medications that we included in the analyses. We analyzed the following medications approved by the US Food and Drug Administration for weight loss: benzphetamine, dexfenfluramine, diethylpropion, fenfluramine, mazindol, orlistat, phendimetrazine, phentermine, and sibutramine. Data on new agents, including bupropion/naltrexone, liraglutide, lorcaserin, and phentermine/topiramate, were not available.
Exercise and diet counseling
Physicians, office staff members, or US Census Bureau representatives also recorded in the patient medical chart whether diet or exercise counseling was ordered at the time of the patient visit.
Statistical Analysis
We performed all analyses by using Stata release 14,37 treating patient visit as a unit of analysis. To evaluate the extent to which the process of medicalization was taking place at the level of patient-physician interaction, we generated national estimates (in millions) of physician office visits annually. We also estimated physician office visits with weight gain listed as a reason for visit and 4 potential outcomes of health care provider visits: obesity diagnosis, weight-loss drug prescriptions, diet counseling, and exercise counseling. We calculated the mean for each outcome and multiplied it by the subpopulation size for each year of the study period. We calculated standard errors for all results and reported 95% confidence intervals (CIs) from 1996 through 2014. We used sample weights provided by the NAMCS to account for the complex sampling design. We compared our estimated numbers with the numbers based on national BMI data from the Behavioral Risk Factor Surveillance System (1996-2014).38 We also ran a series of bivariate linear regression analyses using NAMCS data to test the direction and significance of the associations between the outcomes of interest and time. Specifically, we regressed national estimates of each outcome on year, such that the regression coefficients (slopes) reflected the average annual change in the outcome during the 19-year period.
Results
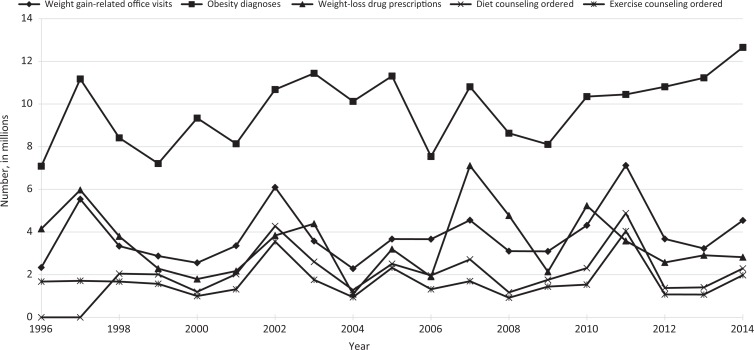
The estimated number of weight gain–related physician office visits increased from 2.3 million in 1996 to 4.5 million in 2014. The estimated number of physician office visits resulting in a diagnosis of obesity ranged from 7.1 million in 1996 to 12.7 million in 2014 and substantially outnumbered the estimates for weight gain–related physician office visits during the study period (Table, Figure 1). The significant positive trend for physician office visits resulting in obesity diagnoses was confirmed by the bivariate linear regression analysis (β = 143 378, P = .03). We observed no significant trend for other outcomes (Table).
Table.
National estimates of all physician office visits, weight gain–related physician office visits, obesity diagnoses, prescriptions for weight-loss drugs, diet counseling ordered, and exercise counseling ordered as the result of physician office visits, National Ambulatory Medical Care Survey, United States, 1996-2014a
| Year | No. of Physician Office Visits in the Sample | Estimated Physician Office Visits, No. in Millions | Estimated Weight Gain–Related Physician Office Visits, No. (95% CI) in Millions | Estimated Obesity Diagnoses as the Result of Physician Office Visits, No. (95% CI) in Millionsb | Estimated Weight-Loss Drug Prescriptions as the Result of Physician Office Visits, No. (95% CI) in Millions | Estimated Diet Counseling Ordered as the Result of Physician Office Visits, No. (95% CI) in Millions | Estimated Exercise Counseling Ordered as the Result of Physician Office Visits, No. (95% CI) in Millions |
|---|---|---|---|---|---|---|---|
| 1996 | 29 805 | 734.5 | 2.3 (1.5-3.1) | 7.1 (4.8-9.4) | 4.1 (2.2-6.0) | — | 1.7 (1.4-2.0) |
| 1997 | 24 715 | 787.4 | 5.5 (2.3-7.8) | 11.2 (7.3-15.1) | 6.0 (3.2-8.8) | — | 1.7 (0.7-2.7) |
| 1998 | 23 339 | 829.3 | 3.3 (1.8-4.8) | 8.4 (4.9-11.9) | 3.8 (0.6-7.0) | 2.0 (1.5-2.5) | 1.7 (1.0-2.4) |
| 1999 | 20 760 | 756.7 | 2.9 (1.9-3.9) | 7.2 (5.5-8.9) | 2.3 (1.4-3.2) | 2.0 (1.6-2.4) | 1.6 (1.2-2.0) |
| 2000 | 27 369 | 823.5 | 2.6 (1.7-3.5) | 9.3 (7.4-11.2) | 1.8 (1.0-2.6) | 1.2 (0.8-1.6) | 1.0 (0.6-1.4) |
| 2001 | 24 281 | 880.5 | 3.4 (2.2-4.6) | 8.1 (6.1-10.1) | 2.2 (1.1-3.3) | 2.0 (1.5-2.5) | 1.3 (0.7-1.9) |
| 2002 | 28 738 | 890.0 | 6.1 (1.9-10.3) | 10.7 (6.4-15.0) | 3.8 (0.1-7.5) | 4.3 (2.9-5.7) | 3.6 (1.7-5.5) |
| 2003 | 25 288 | 906.0 | 3.6 (2.3-4.9) | 11.4 (6.6-16.2) | 4.4 (0.2-8.6) | 2.6 (2.1-3.1) | 1.8 (1.3-2.3) |
| 2004 | 25 286 | 910.9 | 2.3 (1.5-3.1) | 10.1 (7.1-13.1) | 1.1 (0.4-1.8) | 1.3 (0.9-1.7) | 0.9 (0.5-1.3) |
| 2005 | 25 665 | 963.6 | 3.7 (1.7-5.7) | 11.3 (8.3-14.3) | 3.2 (0-6.5) | 2.5 (1.9-3.1) | 2.3 (1.8-2.8) |
| 2006 | 29 392 | 902.0 | 3.7 (2.0-5.4) | 7.5 (5.4-9.6) | 1.9 (0.6-3.2) | 2.0 (1.2-2.8) | 1.3 (0.4-2.2) |
| 2007 | 32 778 | 994.3 | 4.6 (2.0-7.2) | 10.8 (7.7-13.9) | 7.1 (3.4-10.8) | 2.7 (1.9-3.5) | 1.7 (0.9-2.5) |
| 2008 | 28 741 | 956.0 | 3.1 (2.0-4.2) | 8.6 (6.0-11.2) | 4.8 (2.0-7.6) | 1.2 (0.6-1.8) | 0.9 (0.4,1.4) |
| 2009 | 32 281 | 1037.8 | 3.1 (1.8-4.4) | 8.1 (5.7-10.5) | 2.1 (1.1-3.1) | 1.8 (1.2-2.4) | 1.4 (0.7-2.1) |
| 2010 | 31 229 | 1008.8 | 4.3 (1.6-7.0) | 10.3 (6.5-14.1) | 5.2 (0.7-9.7) | 2.3 (1.6-3.0) | 1.5 (0.5-2.5) |
| 2011 | 30 827 | 987.0 | 7.1 (0.5-13.7) | 10.4 (6.6-14.2) | 3.6 (2.1-5.1) | 4.9 (3.1-6.7) | 4.0 (2.4-5.6) |
| 2012 | 76 330 | 928.6 | 3.7 (2.7-4.7) | 10.8 (9.1-12.5) | 2.6 (1.7-3.5) | 1.4 (0.8-2.0) | 1.1 (0.6-1.6) |
| 2013 | 54 873 | 922.6 | 3.2 (2.3-4.1) | 11.2 (9.5-12.9) | 2.9 (2.1-3.7) | 1.4 (1.0-1.8) | 1.1 (0.6-1.6) |
| 2014 | 45 710 | 884.7 | 4.5 (2.4-6.6) | 12.7 (9.6-15.8) | 2.8 (2.1-3.5) | 2.3 (1.2-3.4) | 2.0 (0.8-3.2) |
a National Ambulatory Medical Care Survey data are collected by the National Center for Health Statistics.35
b Significant upward trend demonstrated by bivariate linear regression of national estimate for outcome of interest on year.
Figure 1.
National estimates of weight gain–related physician office visits, obesity diagnoses, prescriptions for weight-loss drugs, diet counseling ordered, and exercise counseling ordered as the result of physician office visits, National Ambulatory Medical Care Survey, United States, 1996-2014.35
The national estimate for physician office visits resulting in at least 1 weight-loss drug prescription increased from 4.1 million in 1996 to 6.0 million in 1997. However, the estimated number of prescriptions decreased substantially in 1998 to 3.8 million, remained in the 1.0-4.0 million prescription range until 2007, increased to 7.1 million in 2007, and then declined again during subsequent years to 2.8 million prescriptions in 2014 (Table, Figure 1). National estimates for physician office visits resulting in orders for exercise counseling and diet counseling paralleled trends in weight gain–related physician office visits, although no consistent pattern emerged. For example, the national estimates for diet counseling were 2 million in 1998 and 2.3 million in 2014.
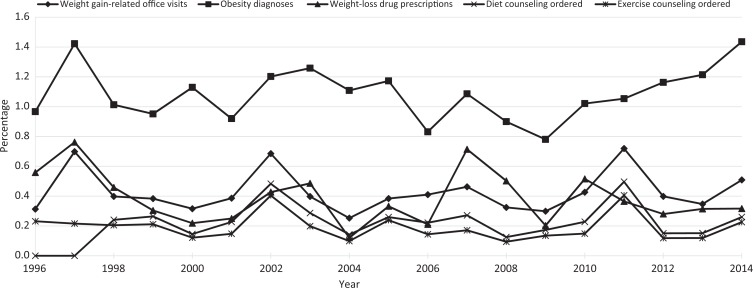
We also calculated rates for all outcomes of interest among all physician office visits recorded in the NAMCS data set during 1996-2014. In 1996, estimated weight gain–related physician office visits accounted for approximately 0.3% of all visits (Figure 2). This rate peaked at 0.7% of physician office visits in 1997 and was 0.5% of all physician office visits in 2014. Rates of estimated diet counseling ordered ranged from 0% to 0.5% during the study period. Rates of estimated exercise counseling ordered were also low, ranging from 0.2% to 0.4%. Rates of estimated physician office visits resulting in at least 1 weight-loss drug prescription ordered varied throughout the period, with a high of 0.8% in 1997 and a low of 0.1% in 2004.
Figure 2.
Estimated percentage of weight gain–related physician office visits, obesity diagnoses, prescriptions for weight-loss drugs, diet counseling ordered, and exercise counseling ordered as the result of physician office visits (calculated by dividing national estimates for each outcome of interest by national estimates of physician office visits for all reasons for each year of the study period), National Ambulatory Medical Care Survey, United States, 1996-2014.35
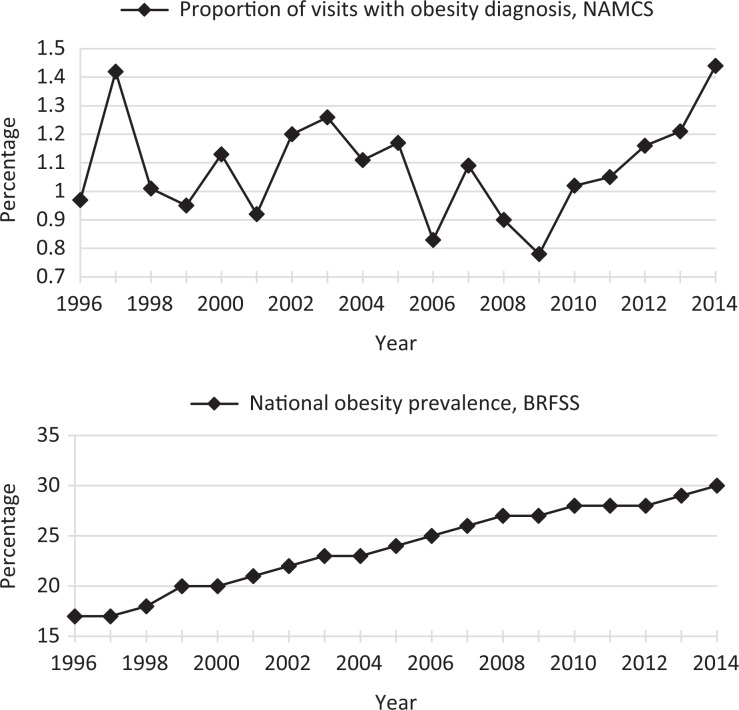
Rates of physician office visits resulting in obesity diagnoses during the study period remained at around 1% (Figure 2, Figure 3). In comparison, we noted a stable increase in population estimates of obesity rates based on the Behavioral Risk Factor Surveillance System data, from about 15% in 1996 to about 30% in 2014 (Figure 3).
Figure 3.
Estimated percentage of physician office visits resulting in obesity diagnoses among National Ambulatory Medical Care Survey (NAMCS) participants aged ≥18 (calculated by dividing national estimates for the number of physician office visits in which 1 of 3 recorded diagnoses was obesity by national estimates of physician office visits for all reasons for each year of the study period) and national estimates for obesity based on body mass index among adults aged ≥18 from the Behavioral Risk Factor Surveillance System (BRFSS) (calculated as the number of persons with body mass index >30 kg/m2 divided by all participants who answered the question about height and weight), United States, 1996-2014. Data sources: National Center for Health Statistics35 and BRFSS.38
Discussion
Analyses of NAMCS data during a 19-year period suggest that medicalization of obesity is only partially occurring. During the study period, we observed a positive and significant slope over time for NAMCS physician office visits resulting in obesity diagnoses. However, the rates of physician office visits resulting in obesity diagnoses remained fairly low, at around 1% each year. Estimates of obesity diagnoses resulting from physician office visits, as well as associated obesity-related outcomes, were lower than expected when compared with national prevalence rates of obesity recorded in the BRFSS. These results suggest that obesity is underdiagnosed and undertreated in clinical settings.
Although NAMCS data do not explain why the medicalization of obesity was incomplete at the patient-physician interaction level, research suggests causal factors from both practitioner and patient perspectives. Physicians’ reluctance to recognize obesity as a chronic disease and to prescribe obesity treatments is well-documented.28,29,31 Reluctance stems from many factors, including widespread obesity stigma among health care professionals,39-44 inadequate training on how to best address weight management,45-48 fears of or frustration with patient noncompliance,45 perceptions of obesity treatment as ineffective,33 lack of teaching materials for patients,49 lack of infrastructure support and places to refer patients,50 substantial time constraints,51 and, importantly, lack of payment by insurance companies for weight-related counseling and care.33,51-54 Furthermore, physicians may be reluctant to offer pharmaceutical and behavioral weight-loss solutions because of the mixed evidence of their success and health risks associated with drug therapy and dieting cycles.55-58 From the patient perspective, mistrust and fear of medical professionals’ judgment impede their desire to ask for and comply with treatment.43 Persons who are obese frequently face unsolicited advice, harsh stereotypes, and lack of empathy from medical professionals.44,59 Patients may also avoid clinical settings where lack of accommodation (eg, accessible seating, larger gowns) causes acute embarrassment.44 Fears of previous, unsafe weight-loss medications also may linger.60 Most patients with obesity have tried multiple weight-loss strategies and require practitioners who are committed to empathetically addressing the complex psychosocial factors related to obesity.59
Health care practitioners must be educated in topics that lead to effective counseling (eg, actionable nutritional topics)61 and in the delivery of compassionate, antistigmatizing care.48 Perceived practitioner bias may cause patients harm,59 including avoidance of physician office visits.62 The Obesity Society63 suggests modeling bias-free interactions to colleagues and offering patients concrete advice (eg, “Let’s discuss starting an exercise program”). Insurance companies should support these endeavors via coverage for weight-reduction counseling and treatments.64
To bridge the gap between the clinical encounter and public health, physicians may wish to adapt techniques used to treat tobacco dependence, such as providing long-term follow-up, encouraging self-monitoring, and assessing patients’ readiness for change.10,11 Understanding patients’ weight-loss expectations and definitions of “success” is also important; evidence suggests that patients with more modest rather than ambitious weight-loss goals have better outcomes, and patients may not realize that a 5%-10% reduction in body weight is linked to positive health outcomes.11
Individually focused dietary and physical activity changes need to be supported by changes in the personal environment (eg, home, work, community),10 food production practices (eg, restricting sugar in processed foods), and environmental policies (eg, enhancing access to public transportation). Outside of clinical practice, physicians could advocate for community-level solutions, such as city plans that reduce automobile use and promote access to walking and cycling.10 However, similar to physician involvement in addressing tobacco dependence, involvement in public health interventions does not preclude physicians from tackling health issues individually with patients.
No medicalization process is universally positive, and further medicalizing obesity may have negative effects, including burdensome medical expenditures, labeling patients as “sick” even if they are not interested in losing weight,65 and the psychological toll associated with failed weight-loss efforts. Nevertheless, obesity experts have concluded that the benefits of medicalizing obesity far outweigh the risks.33,34 One potential benefit, observed in other medicalized conditions,66,67 is that increased physician treatment of obesity may prompt the pharmaceutical industry to invest in new and better drugs and influence the US Food and Drug Administration to approve them.65
Limitations
This study had several limitations. First, the NAMCS did not gauge the use of over-the-counter therapies and bariatric surgery, the latter of which is now considered the most effective method of achieving sustained weight loss.68-70 Second, nonphysician health care providers (eg, physician assistants, nurse practitioners) play an important role in obesity screening and management, but the NAMCS did not provide data on these providers until 2012, thereby limiting their generalizability to only certain types of health care providers. Third, because NAMCS provides data on a maximum of 3 diagnoses, it is possible that in some cases obesity was not recorded, which may have affected our findings. Fourth, the cross-sectional sampling frame of the NAMCS and use of a visit rather than a patient as a unit of observation was a limitation. It is plausible, although unlikely given the 1-week data collection time frame, that more than 1 visit was recorded for the same patient. Moreover, because of the design of the NAMCS, it is possible that some patients who saw their physicians more frequently than other patients received an obesity diagnosis or counseling at a clinical encounter not captured by the survey. Therefore, our estimates for obesity diagnosis might be downwardly biased. Overcoming the limitations of the 1-week sampling frame might be resolved through direct examination of patients or patient records.30,72 Nonetheless, our conclusions are in line with other published studies.30,31,71
Finally, the reporting instrument was revised in 2012 to include write-in responses for several items related to this investigation. Verification of the trends reported by other studies that used different data sources, however, increased our confidence in the reliability of the data reported before and after the revisions.73,74
Strengths
Our study provides recent national statistics on the diagnosis and management of obesity in clinical settings. The study also corroborates research indicating that obese patients are not receiving adequate medical solutions for weight loss and maintenance.71 In addition, it identifies important gaps in the diagnosis and treatment of an acknowledged epidemic. The incomplete medicalization of obesity at the level of patient-physician interaction may serve to perpetuate both poor health outcomes and accompanying stigma. Findings from this study suggest the need to better address obesity management in the context of the physician office visit, on the part of physicians and patients. This study also extends beyond previous medicalization analyses by highlighting the disconnection between conceptualization and practice and emphasizing the potential positive effects of full medicalization of obesity.
Conclusions
Today, more than 70% of persons in the United States have excess weight (overweight) or obesity.8 Stemming this epidemic will require a multipronged effort that supports both individual-level changes and macro-level changes. Physicians are an important and instrumental force in addressing obesity prevention and management. In addition to contending with structural constraints and patient resistance to change, practitioners must work to interrogate their own biases and implement techniques (eg, assessing patient readiness for change) that may enhance patient successes.44
Footnotes
Authors’ Note: Gabriele Ciciurkaite and Mairead Eastin Moloney contributed equally to the article.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Mairead E. Moloney acknowledges the support of the Building Interdisciplinary Research Careers in Women’s Health Program (National Institute on Drug Abuse grant: K12DA035150).
References
- 1. Masters RK, Reither EN, Powers DA, Yang YC, Burger AE, Link BG. The impact of obesity on US mortality levels: the importance of age and cohort factors in population estimates. Am J Public Health. 2013;103(10):1895–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and extreme obesity among adults aged 20 and over: United States, 1960-1962 through 2013-2014. Health E-Stats. 2016. https://www.cdc.gov/nchs/data/hestat/obesity_adult_13_14/obesity_adult_13_14.pdf. Accessed September 18, 2018.
- 3. Pratt CA, Loria CM, Arteaga SS, et al. A systematic review of obesity disparities research. Am J Prev Med. 2017;53(1):113–122. [DOI] [PubMed] [Google Scholar]
- 4. Jia H, Zack MM, Thompson WW. Population-based estimates of decreases in quality-adjusted life expectancy associated with unhealthy body mass index. Public Health Rep. 2016;131(1):177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McDowell MA, Hughes JP, Borrud LG. Health characteristics of U.S. adults by body mass index category: results from NHANES 1999-2002. Public Health Rep. 2006;121(1):67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood). 2009;28(5):w822–w831. [DOI] [PubMed] [Google Scholar]
- 7. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA. 2018;319(16):1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–497. [DOI] [PubMed] [Google Scholar]
- 9. Trust for America’s Health. F as in fat: how obesity threatens America’s future. 2013. https://www.tfah.org/releases/obesity2013. Accessed September 18, 2018.
- 10. Anderson P. Reducing overweight and obesity: closing the gap between primary care and public health. Fam Pract. 2008;25(suppl 1):i10–i16. [DOI] [PubMed] [Google Scholar]
- 11. Ferguson C, Langwith C, Muldoon A, Leonard J. Improving Obesity Management in Adult Primary Care. Washington, DC: George Washington University; 2010. [Google Scholar]
- 12. Moyer VA; U.S. Preventive Services Task Force. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(5):373–378. [DOI] [PubMed] [Google Scholar]
- 13. Conrad P. Medicalization and social control. Annu Rev Sociol. 1992;18(1):209–232. [Google Scholar]
- 14. Conrad P, Mackie T, Mehrotra A. Estimating the costs of medicalization. Soc Sci Med. 2010;70(12):1943–1947. [DOI] [PubMed] [Google Scholar]
- 15. Barker KK. A ship upon a stormy sea: the medicalization of pregnancy. Soc Sci Med. 1998;47(8):1067–1076. [DOI] [PubMed] [Google Scholar]
- 16. Moloney ME, Konrad TR, Zimmer CR. The medicalization of sleeplessness: a public health concern. Am J Public Health. 2011;101(8):1429–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Przepiorka AM, Blachnio A, Miziak B, Czuczwar SJ. Clinical approaches to treatment of internet addiction. Pharmacol Rep. 2014;66(2):187–191. [DOI] [PubMed] [Google Scholar]
- 18. Conrad P, Waggoner M. Anticipatory medicalization: predisposition, prediction, and the expansion of medicalized conditions In: Gadebusch-Biondo M, Sporing F, Gordon JS, eds. Medical Ethics, Prediction, and Prognosis: Interdisciplinary Perspectives. London: Routledge; 2017:101–109. [Google Scholar]
- 19. Jutel A. The emergence of overweight as a disease entity: measuring up normality. Soc Sci Med. 2006;63(9):2268–2276. [DOI] [PubMed] [Google Scholar]
- 20. John-Sowah J. Implications of viewing obesity as a disease. Virtual Mentor. 2005;7(11):759–763. [DOI] [PubMed] [Google Scholar]
- 21. AMA adopts new policies on second day of voting at 2017 annual meeting [press release]. Chicago, IL: American Medical Association; 2017. https://www.ama-assn.org/ama-adopts-new-policies-second-day-voting-2017-annual-meeting. Accessed September 18, 2018. [Google Scholar]
- 22. Lv N, Azar KMJ, Rosas LG, Wulfovich S, Xiao L, Ma J. Behavioral lifestyle interventions for moderate and severe obesity: a systematic review. Prev Med. 2017;100:180–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Glazer G. Long-term pharmacotherapy of obesity 2000: a review of efficacy and safety. Arch Intern Med. 2001;161(15):1814–1824. [DOI] [PubMed] [Google Scholar]
- 24. Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311(1):74–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000;9(5):426–433. [DOI] [PubMed] [Google Scholar]
- 26. Vidal J. Updated review on the benefits of weight loss. Int J Obes Relat Metab Disord. 2002;26(suppl 4):S25–S28. [DOI] [PubMed] [Google Scholar]
- 27. Cleator J, Richman E, Leong KS, Mawdsley L, White S, Wilding J. Obesity: under-diagnosed and under-treated in hospital outpatient departments. Int J Obes Relat Metab Disord. 2002;26(4):581–584. [DOI] [PubMed] [Google Scholar]
- 28. Grizzard T. Undertreatment of obesity. JAMA. 2002;288(17):2177. [PubMed] [Google Scholar]
- 29. Ma J, Xiao L, Stafford RS. Underdiagnosis of obesity in adults in US outpatient settings. Arch Intern Med. 2009;169(3):313–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fitzpatrick SL, Stevens VJ. Adult obesity management in primary care, 2008-2013. Prev Med. 2017;99:128–133. [DOI] [PubMed] [Google Scholar]
- 31. Bardia A, Holtan SG, Slezak JM, Thompson WG. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clin Proc. 2007;82(8):927–932. [DOI] [PubMed] [Google Scholar]
- 32. Hampp C, Kang EM, Borders-Hemphill V. Use of prescription antiobesity drugs in the United States. Pharmacotherapy. 2013;33(12):1299–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168–1177. [DOI] [PubMed] [Google Scholar]
- 34. Allison DB, Downey M, Atkinson RL, et al. Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obesity (Silver Spring). 2008;16(6):1161–1177. [DOI] [PubMed] [Google Scholar]
- 35. National Center for Health Statistics. National Ambulatory Medical Care Survey. Public-Use Data File and Documentation. Atlanta, GA: National Center for Health Statistics; 2018. [Google Scholar]
- 36. Centers for Disease Control and Prevention. International classification of diseases, 9th revision, clinical modification (ICD-9-CM). 1996. https://www.cdc.gov/nchs/icd/icd9 cm.htm. Accessed October 9, 2018.
- 37. StataCorp. Stata: release 14 [computer program] College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 38. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Public-Use Data File and Documentation. Atlanta, GA: Centers for Disease Control and Prevention; 2018. [Google Scholar]
- 39. Miller DP, Jr, Spangler JG, Vitolins MZ, et al. Are medical students aware of their anti-obesity bias? Acad Med. 2013;88(7):978–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25(8):1246–1252. [DOI] [PubMed] [Google Scholar]
- 41. Price JH, Desmond SM, Krol RA, Snyder FF, O’Connell JK. Family practice physicians’ beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3(6):339–345. [PubMed] [Google Scholar]
- 42. Tanneberger A, Ciupitu-Plath C. Nurses’ weight bias in caring for obese patients. Clin Nurs Res. 2018;27(4):414–432. [DOI] [PubMed] [Google Scholar]
- 43. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Fruh SM, Nadglowski J, Hall HR, Davis SL, Crook ED, Zlomke K. Obesity stigma and bias. J Nurse Pract. 2016;12(7):425–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Terre L, Hunter C, Poston WS, Haddock CK, Stewart SA. Treatment of obesity in the primary care setting: are we there yet? Eat Disord. 2007;15(2):135–143. [DOI] [PubMed] [Google Scholar]
- 46. Jay M, Gillespie C, Ark T, et al. Do internists, pediatricians, and psychiatrists feel competent in obesity care? Using a needs assessment to drive curriculum design. J Gen Intern Med. 2008;23(7):1066–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Glauser TA, Roepke N, Stevenin B, Dubois AM, Ahn SM. Physician knowledge about and perceptions of obesity management. Obes Res Clin Pract. 2015;9(6):573–583. [DOI] [PubMed] [Google Scholar]
- 48. Fitzpatrick SL, Wischenka D, Appelhans BM, et al. An evidence-based guide for obesity treatment in primary care. Am J Med. 2016;129(1):115.e1–155.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Timmerman GM, Reifsnider E, Allan JD. Weight management practices among primary care providers. J Am Acad Nurse Pract. 2000;12(4):113–116. [DOI] [PubMed] [Google Scholar]
- 50. Frank E, Wright EH, Serdula MK, Elon LK, Baldwin G. Personal and professional nutrition-related practices of US female physicians. Am J Clin Nutr. 2002;75(2):326–332. [DOI] [PubMed] [Google Scholar]
- 51. Billington CJ. The challenge of obesity management in primary care. J Am Board Fam Pract. 2000;13(3):222–223. [DOI] [PubMed] [Google Scholar]
- 52. Lazovich D, Curry SJ, Beresford SA, Kristal AR, Wagner EH. Implementing a dietary intervention in primary care practice: a process evaluation. Am J Health Promot. 2000;15(2):118–125. [DOI] [PubMed] [Google Scholar]
- 53. Lyznicki JM, Young DC, Riggs JA, Davis RM; Council on Scientific Affairs, American Medical Association. Obesity: assessment and management in primary care. Am Fam Physician. 2001;63(11):2185–2196. [PubMed] [Google Scholar]
- 54. Lee JS, Sheer JL, Lopez N, Rosenbaum S. Coverage of obesity treatment: a state-by-state analysis of Medicaid and state insurance laws. Public Health Rep. 2010;125(4):596–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ioannides-Demos LL, Proietto J, Tonkin AM, McNeil JJ. Safety of drug therapies used for weight loss and treatment of obesity. Drug Saf. 2006;29(4):277–302. [DOI] [PubMed] [Google Scholar]
- 56. Strychar I, Lavoie ME, Messier L, et al. Anthropometric, metabolic, psychosocial, and dietary characteristics of overweight/obese postmenopausal women with a history of weight cycling: a MONET (Montreal Ottawa New Emerging Team) study. J Am Diet Assoc. 2009;109(4):718–724. [DOI] [PubMed] [Google Scholar]
- 57. Wallner SJ, Luschnigg N, Schnedl WJ, et al. Body fat distribution of overweight females with a history of weight cycling. Int J Obes Relat Metab Disord. 2004;28(9):1143–1148. [DOI] [PubMed] [Google Scholar]
- 58. Taing KY, Ardern CI, Kuk JL. Effect of the timing of weight cycling during adulthood on mortality risk in overweight and obese postmenopausal women. Obesity (Silver Spring). 2012;20(2):407–413. [DOI] [PubMed] [Google Scholar]
- 59. Brass CR. Experiences of an obese patient. Narrat Inq Bioeth. 2014;4(2):88–91. [DOI] [PubMed] [Google Scholar]
- 60. Kolata G. How fen-phen, a diet “miracle,” rose and fell. New York Times. 1997;23:16–19. [Google Scholar]
- 61. Bleich SN, Gudzune KA, Bennett WL, Cooper LA. Do physician beliefs about causes of obesity translate into actionable issues on which physicians counsel their patients? Prev Med. 2013;56(5):326–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14(12):554–561. [DOI] [PubMed] [Google Scholar]
- 63. Obesity Society. Obesity, bias, and stigmatization. 2018. http://tosconnect.obesity.org/obesity/resources/facts-about-obesity/bias-stigmatization. Accessed September 18, 2018.
- 64. Kraschnewski JL, Sciamanna CN, Stuckey HL, et al. A silent response to the obesity epidemic: decline in US physician weight counseling. Med Care. 2013;51(2):186–192. [DOI] [PubMed] [Google Scholar]
- 65. Blackburn GL. Medicalizing obesity: individual, economic, and medical consequences. Virtual Mentor. 2011;13(12):890–895. [DOI] [PubMed] [Google Scholar]
- 66. Conrad P. The Medicalization of Society: On the Transformation of Human Conditions Into Treatable Disorders. Baltimore, MD: Johns Hopkins University Press; 2007. [Google Scholar]
- 67. Horwitz AV, Wakefield JC. The Loss of Sadness: How Psychiatry Transformed Normal Sorrow Into Depressive Disorder. New York: Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- 68. Choban PS, Jackson B, Poplawski S, Bistolarides P. Bariatric surgery for morbid obesity: why, who, when, how, where, and then what? Cleve Clin J Med. 2002;69(11):897–903. [DOI] [PubMed] [Google Scholar]
- 69. Encinosa WE, Bernard DM, Du D, Steiner CA. Recent improvements in bariatric surgery outcomes. Med Care. 2009;47(5):531–535. [DOI] [PubMed] [Google Scholar]
- 70. Fisher BL, Schauer P. Medical and surgical options in the treatment of severe obesity. Am J Surg. 2002;184(6B):9S–16S. [DOI] [PubMed] [Google Scholar]
- 71. Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82(1):123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Gilchrist VJ, Stange KC, Flocke SA, McCord G, Bourguet CC. A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits. Med Care. 2004;42(3):276–280. [DOI] [PubMed] [Google Scholar]
- 73. Fink J, Morris GL III, Singh M, Nelson D, Walker R, Cisler RA. Obesity remains underdiagnosed: discordant documentation of obesity body mass index and obesity diagnosis in patients’ electronic medical record. J Patient Centered Res Rev. 2014;1:142. [Google Scholar]
- 74. Talwalkar A, McCarty F. Characteristics of physician office visits for obesity by adults aged 20 and over: United States, 2012. NCHS Data Brief. 2016;237:1–8. [PubMed] [Google Scholar]