Abstract
Purpose
As life expectancy increases, muscle wasting is becoming a more and more important public health problem. This review summarizes the current knowledge of pathophysiological mechanisms underlying muscle loss in ageing and chronic diseases such as heart failure and discusses evolving interventional strategies.
Recent findings
Loss of skeletal muscle mass and strength is a common phenomenon in a wide variety of disorders associated with ageing and morbidity‐associated catabolic conditions such as chronic heart failure. Muscle wasting in ageing but otherwise healthy human beings is referred to as sarcopenia. Unlike cachexia in advanced stages of chronic heart failure, muscle wasting per se is not necessarily associated with weight loss. In this review, we discuss pathophysiological mechanisms underlying muscle loss in sarcopenia and cachexia, highlight similarities and differences of both conditions, and discuss therapeutic targets and possible treatments, such as exercise training, nutritional support, and drugs. Candidate drugs to treat muscle wasting disease include myostatin antagonists, ghrelin agonists, selective androgen receptor molecules, megestrol acetate, activin receptor antagonists, espindolol, and fast skeletal muscle troponin inhibitors.
Summary
Present approaches to muscle wasting disease include exercise training, nutritional support, and drugs, although particularly the latter remain currently restricted to clinical studies. Optimizing skeletal muscle mass and function in ageing and chronic illness including heart failure is one of the chapters that are far from finished and gains future potential for new therapeutic interventions to come.
Keywords: Muscle wasting, Sarcopenia, Cachexia
Introduction
As a normal phenomenon of the ageing human body, there is a gradual decrease in muscle mass accompanied by gains in fat mass and abdominal circumference. If this age‐related loss of muscle mass in the limbs is marked—roughly defined as appendicular muscle mass two standard deviations below that of young adults of the same ethnic group—it is referred to as ‘sarcopenia’.1, 2 Diagnosis of sarcopenia is increasing with increasing life expectancy in our progressively older societies in Europe and the USA.
However, the whole phenomenon of muscle wasting in these populations is even greater. Muscle wasting in ageing but otherwise weight‐stable healthy human beings is endorsed by the magnitude of people who suffer from a weight loss due to a chronic disease, called ‘cachexia’.3
Cachexia is a multifactorial syndrome defined by continuous loss of skeletal muscle mass—with or without loss of fat mass—which cannot be fully reversed by conventional nutritional support and which may lead to progressive functional impairment and increased risk of death.4 While muscle wasting in sarcopenia is not usually associated with weight loss, use of the term cachexia in muscle wasting characterizes patients with involuntary weight loss associated with chronic inflammatory disorders such as chronic heart failure (CHF). Cardiac cachexia may involve a loss of not only muscle but also fat and bone mass.5 This pathological counterpart of muscle wasting rises as well with advances in medicine and a longer lifespan of patients having a chronic disease such as heart failure. As a result, muscle wasting due to both sarcopenia and cachexia is a condition we are increasingly facing.
At the clinical level, muscle wasting frequently translates into frailty—a poor ability to adapt to the environment, which increases disability1, 6, 7, 8, 9, 10 and consequently welfare and healthcare costs. However, as of now, specific tools for diagnosing and managing loss of muscle mass/function are not widely implemented yet into everyday clinical practice. Therefore, this review outlines the pathophysiology of muscle wasting in the elderly for both sarcopenia and cachexia and discusses evolving interventional strategies.
Diagnosis of muscle wasting
Sarcopenia
The alterations that occur with ageing affect all three entities mass, strength, and quality of the muscle.2 The Society of Sarcopenia, Cachexia, and Wasting Disorders characterizes as sarcopenic ‘…a person with muscle loss whose walking speed is equal to or less than 1 m/s or who walks less than 400 m during a 6‐minute walk, and who has a lean appendicular mass corrected for height squared of 2 standard deviations or more below the mean of healthy persons between 20 and 30 years of age of the same ethnic group…’.11, 12 Furthermore, ‘…the limitation in mobility should not be clearly attributable to the direct effect of specific disease…’,11 thereby defining sarcopenia as an independent disease entity. However, as this term is somewhat loose, efforts are continuing to better classify this chronic muscle wasting disease due to ageing/senescence.13 According to the European Working Group on Sarcopenia in Older People, the clinical diagnosis of sarcopenia can be made in subjects with total or appendicular muscle mass ≥2 standard deviations (SD) below that of sex‐matched and ethnicity‐matched young adults and either low handgrip strength below 20 kg in women and 30 kg in men or a reduced muscle function such as reduced walking speed (<1 m/s over 6 min).1 The group defined three stages of sarcopenia: pre‐sarcopenia with loss of muscle mass only, sarcopenia with loss of both muscle mass and distinct functions, and severe sarcopenia with loss of muscle mass and extensive loss of physical performance.2
However, a terminology named ‘Skeletal Muscle Function Deficit’ was recently suggested by the Foundation for the National Institutes of Health Sarcopenia Project to embrace the various evolving concepts of sarcopenia and age‐related muscle dysfunction.2 Herein, the relationship between mobility impairment (defined as gait speed ≤0.8 m/s) and muscle strength (measured by grip strength) is addressed, and strength cutpoints are determined (<26 kg for men and <16 kg for women) below which low strength is especially likely to contribute to slow gait.2 Additionally, by relating these strength cutpoints to muscle mass [estimated by appendicular lean mass adjusted to body mass index (BMI)], cutpoints were determined (<0.789 for men and <0.512 for women), below which low lean mass is especially likely to contribute to low muscle strength.2 Of note, the thereby maintained cutpoints were found to have a predictive value on incident mobility impairment over 3 years of follow‐up.14 Furthermore, the term ‘skeletal muscle function deficit’ helps to integrate functional deficits distinct from ageing such as diabetic polyneuropathy or secondary malnutrition and impairments in muscle strength or power that are independent of muscle mass.2
This is important because a more specific definition of age‐related muscle wasting is highly desirable on practical grounds because specific criteria are critical for identifying candidate patients for clinical trials that test therapies aimed at reversing or alleviating the complications of sarcopenia and its associated manifestations.2, 15 However, a current review article on sarcopenia argues ‘…that what we have…’ would be ‘…an amalgamated and often conflicted description, rather than a definition, of the sarcopenic condition…’.11
Cachexia
In contrast to age‐related muscle wasting, the term cachexia describes the wasting in patients with weight loss and chronic diseases such as CHF, cancer, chronic kidney disease, chronic obstructive pulmonary disease, neuromuscular disease, chronic infection, and metabolic disease‐associated disease processes.13 In 2008, Evans et al. suggested a multidimensional approach to diagnose cachexia, incorporating weight loss of >5% in the preceding year or a BMI of <20 along with the presence of any three of the following: fatigue, anorexia, decreased muscle strength, laboratory evidence of anaemia (haemoglobin < 12 g/dL), hypoalbuminemia (<3.2 g/dL), or elevated markers of inflammation (e.g. interleukin‐6 or C‐reactive protein).16 Recently, an international consensus on definition and classification of cancer cachexia confirmed this weight cut‐off by stating that patients who have more than 5% loss of stable body weight over the previous 6 months, or a BMI of less than 20 kg/m2, and ongoing weight loss of more than 2% are classified as having cachexia.17 However, patients with sarcopenia and ongoing weight loss of more than 2% are now additionally classified as cachectic, too.17
Muscle wasting diseases
According to these overlaps and as the common phenomenon of both sarcopenia and cachexia is loss of muscle, a more integrative definition of age‐related sarcopenia and chronic disease‐related cachexia has been proposed recently, namely, the term ‘muscle wasting diseases’.18 This new classification allows a more general view on the clinical feature of muscle wasting. It distinguishes between muscle wasting in acute and chronic disease settings.15, 18 The chronic one is the most frequent form and can be classified by its aetiology (i.e. that they are due to an underlying chronic illness or ageing, which is then termed sarcopenia) and by disease severity or progression.18 Classification according to disease severity is used to describe pre‐cachexia as well as any form of cachexia where, beyond muscle wasting, loss of fat tissue accompanies this wasting process that is extreme in the latter and typically associated with frailty.18
The new term makes no assumption about a particular pathophysiology of the disease process.18 However, distinct pathophysiological studies have been carried out up to now in both sarcopenic patients on one hand and cachectic patient populations on the other hand that may in synopsis shed further light on the pathophysiology of muscle wasting in general.
Pathophysiologic mechanisms contributing to sarcopenia
Numerous pathways are proposed to be involved in the development of age‐dependent muscle degeneration.19 As a striking histological phenomenon of sarcopenia in the elderly, atrophy of muscle fibres, especially of the fast Type II fibres, a decrease in motor units, and an accumulation of fat within the muscle have been documented.1, 18 First, immobility can trigger muscle wasting. However, muscle loss can lead to immobility as well.1 Furthermore, there is a reduced anabolic drive in ageing leading to a decrease in synthetic capacity of the muscle.1, 20 This is because ageing is associated with lower testosterone levels, insulin‐like growth factor 1 (IGF‐1), and insulin resistance, leading to decreased protein synthesis as testosterone, insulin, and IGF‐1 are potent activators of the Akt pathway, resulting in increased muscle protein synthesis and decreased degradation by inhibiting Fox‐O.1, 21 Testosterone also stimulates myoblasts, inhibits myostatin, and increases satellite cells, which normally help in the repair of myocytes that are reduced with decreasing levels of testosterone in ageing.1 However, there is still a lack of consensus regarding various aspects of sarcopenia. Alchin et al., for example, defined sarcopenia as a problem of neuromuscular junction rather than describing the condition in terms of muscular pathology.15 Indeed, loss of lower motor neurons has been shown to play a role in tipping the balance towards muscle breakdown in the elderly.1, 22 With ageing, motor units undergo successive reduction in numbers with limited adaptation, leading to a decline in motor control.15 When innervation of a myofiber is lost, a neighbouring motor unit will expand to re‐innervate the myofiber in question, leading to an enlargement of the motor unit area.15 A significant fibre‐type switching occurs when mainly Type II myofibers are re‐innervated by slower Type I motor neurons.15 It is still a matter of debate whether this motor unit remodelling is a cause of sarcopenia or a secondary effect of impaired neuronal function and therefore a compensatory adaptive response to sarcopenia.15, 23
In a study by Ling et al., motor unit characteristics with ageing were measured, taking surface representations of human quadricep motor units electromyographically.24 This study found an increase in the size of the motor units and furthermore a decline in the motor unit firing rate with age at contractions relevant to general mobility.24 While these changes were slight until the age of 75, beyond this age, the effects were substantial. Motor unit alterations occurred later than the age of sarcopenic onset, thus indirectly referring to the condition as an initially muscular pathology.24 On the other hand, a variety of other studies indicate that denervation, and by extension motor unit enlargement, occurs before myofiber degradation. Deschenes et al., for example, analysed the neuromuscular junction of early aged rats by cytofluorescent staining to determine whether denervation is a precipitous neuromuscular junction of sarcopenic myofiber alterations.25 In both the plantaris and soleus muscles, significant signs of denervation were observed with little change in myofiber phenotype, which adds weight to the hypothesis that the trigger factor for sarcopenia is pre‐synaptic.25 However, there is a third possibility that sarcopenia is a result of both pre‐synaptic and post‐synaptic degeneration.
Additionally, a decrease in mitochondrial function and content has been described in aged muscles, and interestingly enough, this is prevented by exercise at least in animal models of sarcopenia.26 Finally, muscle apoptosis has been documented to be increased.1
Importantly, inflammatory pathways involving nuclear factor κB (NF‐κB) are typically not activated in sarcopenia,1, 4 and inflammation is believed not to contribute to this muscle wasting; resting energy expenditure is even decreased, and there is an increase in fat mass. These features are important to discriminate sarcopenia from cachexia, the latter being an extreme wasting disease characterized by weight loss, inflammation, and increased energy expenditure.18
Pathophysiologic mechanisms contributing to cachexia
Elevated resting energy expenditure is a major determinant in the development of malnutrition in cachexia. Resting energy expenditure describes the sources needed to provide energy for metabolic processes involved in maintaining the function and integrity of cells and body organs.27, 28 It is presumed that in cachexia, abnormalities in carbohydrate, lipid, and protein metabolism are major biochemical bases of elevated resting energy expenditure, while diet‐induced thermogenesis and energy expenditure associated with exercise are not altered.27
Some studies with cachectic patients show that part of the changes in metabolism can be attributed to altered absorption of nutrients16 as energy intake is one of the key components of energy balance. In cancer cachexia, for example, lipid and carbohydrate alterations in intestinal absorption have been reported.4 Chemotherapy is, in part, responsible for the intestinal alterations.4 In the case of CHF, an increased sympathetic activity leads to a redistribution of blood flow away from the splanchnic circulation.29 Thus, in CHF patients, a decrease in intestinal mucosal pH has been observed, indicating that intestinal ischaemia may contribute to malabsorption and thus trigger weight loss via decreased absorption of nutrients, with cachectic patients displaying a high loss of fat and protein via stool.30 However, intestinal ischaemia with decreased absorption of nutrients is not the only reason for continuous catabolism in cachexia. Additionally, loss of gastrointestinal barrier integrity is thought to play a major role in an amplification of systemic inflammation in cachexia.29, 31 Inflammation is purported to be a trigger in the pathogenesis of cachexia (Figure 1). Specifically, lipopolysaccharide (LPS), a cell wall component of gram‐negative bacteria, is believed to interact with the damaged intestinal tract and to promote local and systemic cytokine release.29 LPS can enter the circulation through the gut wall if barrier function is impaired in various diseases, not only cancer and CHF but also burn injury, sepsis, and liver cirrhosis, that lead to wasting.32 In the circulation of cachectic patients, LPS may activate monocytes and macrophages to release pro‐inflammatory mediators, thus triggering an inflammatory state, which generates more energetic inefficiency. This is because cytokines are able to activate, for instance, mitochondrial‐uncoupling proteins.32, 33 Inflammatory cytokines including interleukin (IL)‐1, IL‐6, and tumour necrosis factor α induce myofibrillar breakdown by activation of the ubiquitin proteasome pathway, via NF‐κB‐dependent and NF‐κB‐independent mechanisms.1, 34, 35 Down‐regulation of anabolic factors/pathways including IGF‐1, androgens, and satellite cell proliferation1; increases in catabolic pathways/processes such as apoptosis,1 autophagy,36 and mitochondrial dysfunction37; and the myostatin pathway1 all may contribute to muscle mass and function loss in this setting. Cytokine‐mediated release of cortisol and adrenergic hormones may furthermore lead to increased fat oxidation, atrophy, and hypermetabolism.1
Figure 1.
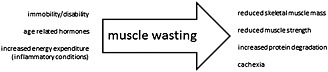
Factors inducing muscle wasting leading to reduced mass and strength of skeletal muscle.
Some studies showed that the growth differentiating factor 15 (GDF‐15) may play an important role in the pathways of muscle wasting and cachexia.38, 39 GDF‐15 is a protein belonging to the transforming growth factor β superfamily that has a role in regulating inflammatory and apoptotic pathways during disease processes.40 In a mouse model, administration of human GDF‐15 resulted in decreased energy expenditure and lower muscle strength.38
Finally, various disease‐related, therapy‐related, and patient‐related factors such as pain, nausea, fatigue, and depression may additionally cause a reduction in appetite in these patients, further aggravating their given hypercatabolic state.1, 41 The elderly, with co‐morbidities, limited mobility, reduced nutrition, low IGF‐1 and testosterone levels, and low muscle mass, seem to be especially prone to cachexia even at earlier stages of chronic disease.1
Diagnostic tools for assessment of skeletal muscle
Skeletal muscle merits more attention in daily clinical work and has received only limited research endeavours so far.42 The availability of tools to easily detect muscle loss or even muscle wasting in affected patients would provide a means for daily clinical practice. The standard method for assessment of lean mass, which includes the muscle is dual‐energy X‐ray absorptiometry.43 However, bioelectrical impedance analysis is an alternative that is widely available and much more suitable for fast and routine clinical application because of mobility and affordable technical application without use of radiation.44, 45 A new recently validated method indicates a decreased rate of myofibrillar, sarcoplasmic, and collagen protein synthesis very early. This isotope‐based method using the deuterium oxide (D2O) method is a valid but invasive approach to quantify muscle anabolism before any changes in muscle mass become detectable.46 Another method allows measurement of a stable (non‐radioactive) isotope of creatine (D3‐creatine) that reflects total muscle mass in a single urine sample.47, 48 Application of these methods seems to be suitable to assess and monitor muscle mass in patients with muscle wasting diseases.
Currently available treatment strategies targeting muscle function
The development of preventive and therapeutic strategies against sarcopenia, cachexia, and wasting disorders in general is an urgent need.5, 49
Despite differences in their pathophysiology, it is widely believed that both sarcopenia and cachexia are likely to respond to interventions and/or drugs that increase muscle mass and muscle strength.40 Despite intensive research efforts in the field of muscle wasting during the last couple of decades, no effective treatment of muscle wasting exists, even though study of the molecular pathways involved in muscle wasting suggests many therapeutic targets. In addition, a large number of smaller clinical trials have been performed with mixed results. Tables 1 and 2 give an overview of clinical trials using potential treatments of muscle wasting or including measurement of body composition in ageing (Table 1) and in patients with CHF (Table 2), which are often similar.
Table 1.
Potential treatment of muscle wasting in elderly patients
| Treatment | Study design | Study population: n in total (in treatment group), features | Intervention | Comparison | Outcomes (intervention group) | Reference |
|---|---|---|---|---|---|---|
| Nutritional supplementation | Randomized controlled trial | 210 (105), hospital‐admitted malnourished elderly patients (≥60 years) | Nutritional supplementation (energy‐enriched and protein‐enriched diet, oral nutritional support, calcium–vitamin D supplement, telephone counselling by a dietitian) for 3 months post‐discharge | Usual care | • Increase in body weight in the intervention group; significant for the highest body weight category (mean difference 3.4 kg) | Neelemaat et al.66 |
| • Decrease in functional limitations (more in the intervention group than in the control group) | ||||||
| • No significant differences for physical performance, physical activities, fat‐free mass, or handgrip strength | ||||||
| Oral growth hormone (capromorelin) | Randomized, double‐masked, placebo‐controlled, multicentre study | 395 (314), men and women aged 65–84 years | 2 years of treatment to four dosing groups (10 mg three times/week, 3 mg twice a day, 10 mg each night, and 10 mg twice a day) | Placebo during 2 years | • A rise in peak nocturnal growth hormone (prompted by each capromorelin dose) | White et al.63 |
| • Increase in body weight by 1.4 kg (capromorelin) at 6 months and decrease by 0.2 kg (placebo group) (P = 0.006) | ||||||
| • Increase in LBM 1.4 vs. 0.3 kg (P = 0.001) | ||||||
| • Improved tandem walk by 0.9 s (P = 0.02) in the pooled treatment vs. placebo groups | ||||||
| • Improved stair climb by 12 months (P = 0.04) | ||||||
| The selective androgen receptor modulator GTx‐024 (enobosarm) | Randomized, double‐blind, placebo‐controlled, multicentre study | 120, healthy elderly men (>60 years of age) and post‐menopausal women | Four different dose groups (doses of 0.1, 0.3, 1, and 3 mg of GTx‐024 daily) for 86 days | Placebo for 86 days | • Significant dose‐dependent increase in LBM (P < 0.001, 3 mg vs. placebo) | Dalton et al.64 and Russ et al.67 |
| • Significant improvements in physical function (P = 0.013, 3 mg vs. placebo) and insulin resistance (P = 0.013, 3 mg vs. placebo) | ||||||
| Angiotensin‐converting enzyme inhibitor (perindopril) | Randomized, double‐blind, placebo‐controlled study | 130 (65), participants aged 65 years with mobility problems or functional impairment | Perindopril for 20 weeks | Placebo for 20 weeks | • Significantly improved 6‐min walking distance (P = 0.003) | Sumukadas et al.68 |
| • A significant impact on health‐related quality of life (P = 0.046) | ||||||
| • No significant differences between the two groups in the other outcomes | ||||||
| Exogenous testosterone (T) alone or with finasteride (T + F) | Randomized, blinded, placebo‐controlled study | 70 (46), men age 65 years and older with low testosterone serum (<350 ng/dL) | (1) Enanthate, 200 mg every 2 weeks, with placebo pills daily (T‐only); (2) enanthate, 200 mg every 2 weeks, with 5 mg F daily (T + F) over 36 months | (3) Placebo injections and pills (placebo) over 36 months | • Significantly improved performance in a timed functional test (P < 0.002 for both T and T + F vs. placebo) | Page et al.69 |
| • Increased handgrip strength compared with placebo (P < 0.05) | ||||||
| • Increase in lean body mass [3.77 ± 0.55 kg (T‐only) and 3.64 ± 0.56 kg (T + F) vs. −0.21 ± 0.55 kg for placebo (P < 0.0001)] | ||||||
| • Decrease in fat mass and significant decrease in total cholesterol, low‐density lipoprotein, and leptin, without affecting high‐density lipoprotein, adiponectin, or fasting insulin levels | ||||||
| Exercise training | Randomized, controlled study | Exercise and nutrition group (n = 30), exercise‐only group (n = 28), and control group (n = 31) | (1) Exercise and nutrition, (2) exercise only | Control group over 12 weeks | • Combined physical training and nutrition intervention significantly improves health‐related quality of life and handgrip strength | Kwon et al.70 |
| • The exercise‐only group showed a significantly increased handgrip strength |
LBM, lean body mass.
Table 2.
Potential treatment of muscle wasting in patients with heart failure
| Treatment | Study design | Study population: n in total (in treatment group) | Outcomes | Body composition, other | Reference | ||
|---|---|---|---|---|---|---|---|
| Body weight (kg) | Exercise capacity: peak VO2 (mL/kg/min) | 6‐min walk test (m) | |||||
| Essential amino acid supplement | Randomized, placebo controlled, double blind | 38 (21) | Increase in body weight by >1 kg in 80% of supplemented patients (mean 2.96 kg) and in 30% of controls (mean 2.3 kg) (P < 0.05) | BL: 13,5 ± 1.7; EoS: 14.9 ± 1.9 (P < 0.05) | BL: 331 ± 124; EoS: 405 ± 130 (P < 0.001) | • Increase in maximum work output (P < 0.05) | Ebner et al.4 and Aquilani et al.71 |
| Recombinant human growth hormone | Randomized, placebo controlled, double blind | 50 (25) | Unchanged | Not performed | Unchanged | • Increased left ventricular mass and septal wall thickness (P = 0.0001, P = 0.03) | Ebner et al.4 and Osterziel et al.72 |
| • No significant change in posterior wall thickness | |||||||
| • Increased serum level of insulin‐like growth factor 1 (P < 0.0001) | |||||||
| Testosterone | Randomized, placebo controlled, double blind | 70 (35) | BL: 64 ± 14; EoS: 67 ± 11 | BL: 13.4 ± 4.4; EoS: 16.3 ± 1.7 (P < 0.05) | BL: 387 ± 121; EoS: 437 ± 138 (P < 0.05) | • Increase in maximum work output (P < 0.05) | Ebner et al.4 and Caminiti et al.73 |
| Exercise training (bicycle ergometer) | Randomized, controlled, open label | 24 (12) | Not changed | BL: 15.1 ± 3; EoS: increase of 17.5 ± 17 (P < 0.01) | Not performed | • Reduction of myostatin mRNA (P = 0.02) | Ebner et al.4 and Lenk et al.74 |
| • Reduction of myostatin protein (P = 0.02) | |||||||
| Administration of salbutamol (per os) | Randomized, placebo controlled, double blind | 12 (6) | No significant changes | BL: 18.9 ± 1.9; EoS: 17.9 ± 1.4 (P = 0.41) | Not performed | • No significant change in right quadricep strength | Ebner et al.4 and Harrington et al.75 |
BL, baseline; EoS, end of study.
To date, exercise training is the treatment of choice. There is discussion about the best way of muscle training.50, 51 Endurance exercise has been shown to decrease systemic inflammatory markers52 and improve endothelial function in elderly individuals.53 These effects could potentially counteract the anabolic resistance in elderly individuals, as discussed earlier. In line with this, endurance training combined with immediate protein ingestion leads to improved muscle oxidative capacity, indicating that protein feeding improves the qualitative muscle adaptations to endurance training such as mitochondrial biogenesis.54 Endurance exercise seems to improve muscle quality more than muscle quantity. Contrastingly, light‐load resistance training is known to exert better hypertrophic effects on the musculature compared with endurance exercise.51, 55 A combination of both along with each of the exercise regimens alone should be tested in future clinical trials.
It is important to keep in mind that not only the limb musculature but also a reduced inspiratory muscle capacity might account for lower exercise capacity in the elderly. In patients with CHF, for example, among whom 5% and 15% are affected by cachexia, exercise intolerance and dyspnoea have been attributed partially to the dysfunction of the skeletal and the respiratory musculature.56 This is underlined by the study by Laoutaris et al. who investigated the work capacity of inspiratory muscle by assessing the inspiratory strength and the sustained maximal inspiratory pressure in patients with heart failure.57 Among 60 patients and 30 control subjects, they found both parameters to be reduced by 46% and 23%, respectively. Reduced inspiratory muscle performance correlated with lower peak oxygen consumption and lower 6‐min walk distance, indicating an association of inspiratory muscle dysfunction with reduced exercise capacity. A pilot study on 27 patients with CHF showed that combined aerobic training with resistance training and inspiratory muscle training resulted in incremental benefits in both peripheral and respiratory muscle weakness, cardiopulmonary function, and quality of life compared with that of aerobic training alone.57 The mechanisms involved in exercise‐induced improvement of functional capacity await to be completely elucidated. However, there is evidence that physical exercise may target myostatin regulation, thereby increasing muscle growth and mass.57, 58 Furthermore, exercise training has long been shown to induce favourable skeletal muscle angiogenesis.51, 52, 53, 54
In daily clinical practice, in addition to exercise training, patients' nutrition should be optimized to prevent nutritional lack of protein and micronutrients. All factors that are important for muscle function should be identified and addressed including therapy of iron deficiency and lack of vitamin D.59 The latter is underestimated but very common, for example, in European patients with heart failure and reduced kidney function, and may lead to additional muscle symptoms, such as weakness and cramps.60
Effects of specific nutritional therapy alone on the underlying catabolic process of muscle wasting, if existing, remain to be established. Meanwhile, the provision of nutritional supplements incorporating essential amino acids combined with exercise training has been suggested to be the best method of attenuating muscle wasting.50, 61
According to this, potential synergistic effects that could accrue from nutritional therapy in conjunction with new drugs are conceivable and should be searched for in future clinical trials. Candidate drugs to treat muscle wasting disease that are available or in development include myostatin antagonists, ghrelin agonists, selective androgen receptor molecules, megestrol acetate, activin receptor antagonists, espindolol, formoterol, and fast skeletal muscle troponin inhibitors.62, 63, 64 Recently, the first promising results of a phase III trial ‘Prevention and treatment of muscle wasting in patients with cancer’ were demonstrated where the selective androgen receptor modulator enobosarm had consistently demonstrated increases in lean body mass and better physical function across several populations without the toxic effects associated with androgens along with a lower hazard ratio for survival in cancer patients.65 Therefore, the selective androgen receptor enobosarm may become one of the first available drug against muscle wasting in man.
Conclusion
Maintaining muscle mass and strength is a key challenge in order to confer good quality of life in patients with chronic illness and in the elderly. Although effective treatments beyond exercise training currently remain to be established, the pathophysiological findings may pave the way for therapeutic approaches to muscle wasting disease. Optimizing skeletal muscle mass and function in ageing and in chronic illness is one of the chapters that are far from finished and gains future potential for new therapeutic targets to come.
Conflict of interest
None declared
Acknowledgement
We acknowledge the support of the German Research Foundation and the Open Access Publication Funds of Göttingen University.
Ebner, N. , Sliziuk, V. , Scherbakov, N. , and Sandek, A. (2015), Muscle wasting in ageing and chronic illness. ESC Heart Failure, 2, 58–68. doi: 10.1002/ehf2.12033.
References
- 1. Ali S, Garcia JM. Sarcopenia, cachexia and aging: diagnosis, mechanisms and therapeutic options—a mini‐review. Gerontology 2014; 60: 294–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Correa‐de‐Araujo R, Hadley E. Skeletal muscle function deficit: a new terminology to embrace the evolving concepts of sarcopenia and age‐related muscle dysfunction. J Gerontol A Biol Sci Med Sci 2014; 69: 591–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Coats AJ. Research on cachexia, sarcopenia and skeletal muscle in cardiology. J Cachexia Sarcopenia Muscle 2012; 3: 219–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ebner N, Elsner S, Springer J, von Haehling S. Molecular mechanisms and treatment targets of muscle wasting and cachexia in heart failure: an overview. Curr Opin Support Palliat Care 2014; 8: 15–24. [DOI] [PubMed] [Google Scholar]
- 5. Kalantar‐Zadeh K, Rhee C, Sim JJ, Stenvinkel P, Anker SD, Kovesdy CP. Why cachexia kills: examining the causality of poor outcomes in wasting conditions. J Cachexia Sarcopenia Muscle 2013; 4: 89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sillanpää E, Stenroth L, Bijlsma AY, Rantanen T, McPhee JS, Maden‐Wilkinson TM, Jones DA, Narici MV, Gapeyeva H, Pääsuke M, Barnouin Y, Hogrel JY, Butler‐Browne GS, Meskers CG, Maier AB, Törmäkangas T, Sipilä S. Associations between muscle strength, spirometric pulmonary function and mobility in healthy older adults. Age (Dordr) 2014; 36: 9667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 2002; 50: 889–896. [DOI] [PubMed] [Google Scholar]
- 8. Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, Studenski S, Berkman LF, Wallace RB. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000; 55: M221–M231. [DOI] [PubMed] [Google Scholar]
- 9. Villani AM, Miller MD, Cameron ID, Kurrle S, Whitehead C, Crotty M. Development and relative validity of a new field instrument for detection of geriatric cachexia: preliminary analysis in hip fracture patients. J Cachexia Sarcopenia Muscle 2013; 4: 209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Knops M, Werner CG, Scherbakov N, Fiebach J, Dreier JP, Meisel A, Heuschmann PU, Jungehülsing GJ, von Haehling S, Dirnagl U, Anker SD, Doehner W. Investigation of changes in body composition, metabolic profile and skeletal muscle functional capacity in ischemic stroke patients: the rationale and design of the Body Size in Stroke Study (BoSSS). J Cachexia Sarcopenia Muscle 2013; 4: 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alchin DR. Sarcopenia: describing rather than defining a condition. J Cachexia Sarcopenia Muscle 2014; doi: 10.1007/s13539-014-0156-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fülster S, Tacke M, Sandek A, Ebner N, Tschöpe C, Doehner W, Anker SD, von Haehling S. Muscle wasting in patients with chronic heart failure: results from the studies investigating co‐morbidities aggravating heart failure (SICA‐HF). Eur Heart J. 2013; 34(7): 512–519. [DOI] [PubMed] [Google Scholar]
- 13. Anker SD, Coats AJ, Morley JE, Rosano G, Bernabei R, von Haehling S, Kalantar‐Zadeh K. Muscle wasting disease: a proposal for a new disease classification. J Cachexia Sarcopenia Muscle 2014; 5: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McLean RR, Shardell MD, Alley DE, Cawthon PM, Fragala MS, Harris TB, Kenny AM, Peters KW, Ferrucci L, Guralnik JM, Kritchevsky SB, Kiel DP, Vassileva MT, Xue QL, Perera S, Studenski SA, Dam TT. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the Foundation for the National Institutes of Health (FNIH) Sarcopenia Project. J Gerontol A Biol Sci Med Sci 2014; 5: 576–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roman D, Mahoney K, Mohamadi A. Sarcopenia: what's in a name? JAMDA 2012; 1–3. [DOI] [PubMed] [Google Scholar]
- 16. Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, Jatoi A, Kalantar‐Zadeh K, Lochs H, Mantovani G, Marks D, Mitch WE, Muscaritoli M, Najand A, Ponikowski P, Rossi Fanelli F, Schambelan M, Schols A, Schuster M, Thomas D, Wolfe R, Anker SD. Cachexia: a new definition. Clin Nutr 2008; 27: 793–799. [DOI] [PubMed] [Google Scholar]
- 17. Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, Jatoi A, Loprinzi C, MacDonald N, Mantovani G, Davis M, Muscaritoli M, Ottery F, Radbruch L, Ravasco P, Walsh D, Wilcock A, Kaasa S, Baracos VE. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 2011; 12: 489–495. [DOI] [PubMed] [Google Scholar]
- 18. Muscaritoli M, Anker SD, Argiles J, Aversa Z, Bauer JM, Biolo G, Boirie Y, Bosaeus I, Cederholm T, Costelli P, Fearon KC, Laviano A, Maggio M, Rossi Fanelli F, Schneider SM, Schols A, Sieber CC. Consensus definition of sarcopenia, cachexia and pre‐cachexia: joint document elaborated by special interest groups (SIG) ‘Cachexia–Anorexia in Chronic Wasting Diseases’ and ‘Nutrition in Geriatrics’. Clin Nutr 2010; 29: 154–159. [DOI] [PubMed] [Google Scholar]
- 19. Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, Abellan van Kan G, Andrieu S, Bauer J, Breuille D, Cederholm T, Chandler J, De Meynard C, Donini L, Harris T, Kannt A, Keime Guibert F, Onder G, Papanicolaou D, Rolland Y, Rooks D, Sieber C, Souhami E, Verlaan S, Zamboni M. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International Working Group on Sarcopenia. J Am Med Dir Assoc 2011; 12: 249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Haran PH, Rivas DA, Fielding RA. Role and potential mechanisms of anabolic resistance in sarcopenia. J Cachexia Sarcopenia Muscle 2012; 3: 157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fanzani A, Conraads VM, Penna F, Martinet W. Molecular and cellular mechanisms of skeletal muscle atrophy: an update. J Cachexia Sarcopenia Muscle 2012; 3: 163–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ferraro E, Molinari F, Berghella L. Molecular control of neuromuscular junction development. J Cachexia Sarcopenia Muscle 2012; 3: 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Malmstrom TK, Miller DK, Herning MM, Morley JE. Low appendicular skeletal muscle mass (ASM) with limited mobility and poor health outcomes in middle‐aged African Americans. J Cachexia Sarcopenia Muscle 2013; 4: 179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ling SM, Conwit RA, Ferrucci L, Metter EJ. Age‐associated changes in motor unit physiology: observations from the Baltimore Longitudinal Study of Aging. Arch Phys Med Rehabil 2009; 90: 1237–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Deschenes MR, Sherman EG, Roby MA, Glass EK, Harris MB. Effect of resistance training on neuromuscular junctions of young and aged muscles featuring different recruitment patterns. J Neurosci Res 2014, doi: 10.1002/jnr.23495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kang C, Chung E, Diffee G, Ji LL. Exercise training attenuates aging‐associated mitochondrial dysfunction in rat skeletal muscle: role of PGC‐1α. Exp Gerontol 2013; 48: 1343–1350. [DOI] [PubMed] [Google Scholar]
- 27. Vaughan VC, Martin P, Lewandowski PA. Cancer cachexia: impact, mechanisms and emerging treatments. J Cachexia Sarcopenia Muscle 2013; 4: 95–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tacke M, Ebner N, Boschmann M, Jarius A, Valentova M, Fülster S, Sandek A, Schomburg L, Anker SD, Doehner W, von Haehling S. Resting energy expenditure and the effects of muscle wasting in patients with chronic heart failure: results from the Studies Investigating Comorbidities Aggravating Heart Failure (SICA‐HF). J Am Med Dir Assoc 2013; 14: 837–841. [DOI] [PubMed] [Google Scholar]
- 29. Sandek A, Swidsinski A, Schroedl W, Watson A, Valentova M, Herrmann R, Scherbakov N, Cramer L, Rauchhaus M, Grosse‐Herrenthey A, Krueger M, von Haehling S, Doehner W, Anker SD, Bauditz J. Intestinal blood flow in patients with chronic heart failure—a link with bacterial growth, gastrointestinal symptoms and cachexia. J Am Coll Cardiol 2014; 64: 1092–1102. [DOI] [PubMed] [Google Scholar]
- 30. Arutyunov GP, Kostyukevich OI, Serov RA, Rylova NV, Bylova NA. Collagen accumulation and dysfunctional mucosal barrier of the small intestine in patients with chronic heart failure. Int J Cardiol 2008; 125: 240–245. [DOI] [PubMed] [Google Scholar]
- 31. Klein GL, Petschow BW, Shaw AL, Weaver E. Gut barrier dysfunction and microbial translocation in cancer cachexia: a new therapeutic target. Curr Opin Support Palliat Care 2013; 7: 361–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sandek A, Bjarnason I, Volk HD, Crane R, Meddings JB, Niebauer J, Kalra PR, Buhner S, Herrmann R, Springer J, Doehner W, von Haehling S, Anker SD, Rauchhaus M. Studies on bacterial endotoxin and intestinal absorption function in patients with chronic heart failure. Int J Cardiol 2012; 157: 80–85. [DOI] [PubMed] [Google Scholar]
- 33. Julienne CM, Dumas JF, Goupille C, Pinault M, Berri C, Collin A, Tesseraud S, Couet C, Servais S. Cancer cachexia is associated with a decrease in skeletal muscle mitochondrial oxidative capacities without alteration of ATP production efficiency. J Cachexia Sarcopenia Muscle 2012; 3: 265–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hinch EC, Sullivan‐Gunn MJ, Vaughan VC, McGlynn MA, Lewandowski PA. Disruption of pro‐oxidant and antioxidant systems with elevated expression of the ubiquitin proteosome system in the cachectic heart muscle of nude mice. J Cachexia Sarcopenia Muscle 2013; 4: 287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Palus S, von Haehling S, Springer J. Muscle wasting: an overview of recent developments in basic research. J Cachexia Sarcopenia Muscle 2014; 5: 193–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Penna F, Costamagna D, Pin F, Camperi A, Fanzani A, Chiarpotto EM, Cavallini G, Bonelli G, Baccino FM, Costelli P. Autophagic degradation contributes to muscle wasting in cancer cachexia. Am J Pathol 2013; 182: 1367–1378. [DOI] [PubMed] [Google Scholar]
- 37. Padrao AI, Oliveira P, Vitorino R, Colaço B, Pires MJ, Märquez M, Castellanos E, Neuparth MJ, Teixeira C, Costa C, Moreira‐Gonçalves D, Cabral S, Duarte JA, Santos LL, Amado F, Ferreira R. Bladder cancer‐induced skeletal muscle wasting: disclosing the role of mitochondria plasticity. Int J Biochem Cell Biol 2013; 45: 1399–1409. [DOI] [PubMed] [Google Scholar]
- 38. Lerner L, Guillory B, Chen J, Winston W, Weiler S, Gyuris J, Garcia J. Growth differentiating factor‐15 (GDF‐15) induces anorexia and cachexia in mice: a novel pathway for cachexia. J Cachexia Sarcopenia Muscle 2013; 4: 295–343. abstract 2‐02.24190182 [Google Scholar]
- 39. Tsai VW, Husaini Y, Manandhar R, Lee‐Ng KK, Zhang HP, Harriott K, Jiang L, Lin S, Sainsbury A, Brown DA, Breit SN. Anorexia/cachexia of chronic diseases: a role for the TGF‐β family cytokine MIC‐1/GDF15. J Cachexia Sarcopenia Muscle 2012; 3: 239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ebner N, Steinbeck L, Doehner W, Anker SD, von Haehling S. Highlights from the 7th Cachexia Conference: muscle wasting pathophysiological detection and novel treatment strategies. J Cachexia Sarcopenia Muscle 2014; 5: 27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Omlin A, Blum D, Wierecky J, Haile SR, Ottery FD, Strasser F. Nutrition impact symptoms in advanced cancer patients: frequency and specific interventions, a case‐control study. J Cachexia Sarcopenia Muscle 2013; 4: 55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. von Haehling S, Anker SD. Cachexia vs obesity: where is the real unmet clinical need? J Cachexia Sarcopenia Muscle 2013; 4: 245–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cesari M, Fielding RA, Pahor M, Goodpaster B, Hellerstein M, van Kan GA, Anker SD, Rutkove S, Vrijbloed JW, Isaac M, Rolland Y, M'rini C, Aubertin‐Leheudre M, Cedarbaum JM, Zamboni M, Sieber CC, Laurent D, Evans WJ, Roubenoff R, Morley JE, Vellas B, International Working Group on Sarcopenia . Biomarkers of sarcopenia in clinical trials—recommendations from the International Working Group on Sarcopenia. J Cachexia Sarcopenia Muscle 2012; 3: 181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Janssen I, Heymsfield SB, Baumgartner RN, Ross R. Estimation of skeletal muscle mass by bioelectrical impedance analysis. J Appl Physiol 2000; 89: 465–471. [DOI] [PubMed] [Google Scholar]
- 45. Norman K, Pirlich M, Sorensen J, Christensen P, Kemps M, Schütz T, Lochs H, Kondrup J. Bioimpedance vector analysis as a measure of muscle function. Clin Nutr 2009; 28: 78–82. [DOI] [PubMed] [Google Scholar]
- 46. Wilkinson DJ, Franchi MV, Brook MS, Narici MV, Williams JP, Mitchell WK, Szewczyk NJ, Greenhaff PL, Atherton PJ, Smith K. A validation of the application of D(2)O stable isotope tracer techniques for monitoring day‐to‐day changes in muscle protein subfraction synthesis in humans. Am J Physiol Endocrinol Metab 2014; 306: E571–E579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Clark RV, Walker AC, O'Connor‐Semmes RL, Leonard MS, Miller RR, Stimpson SA, Turner SM, Ravussin E, Cefalu WT, Hellerstein MK, Evans WJ. Total body skeletal muscle mass: estimation by creatine (methyl‐d3) dilution in humans. J Appl Physiol 2014; 116: 1605–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Stimpson SA, Leonard MS, Clifton LG, Poole JC, Turner SM, Shearer TW, Remlinger KS, Clark RV, Hellerstein MK, Evans WJ. Longitudinal changes in total body creatine pool size and skeletal muscle mass using the D3‐creatine dilution method. J Cachexia Sarcopenia Muscle 2013; 4: 217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Marzetti E, Calvani R, Cesari M, Buford TW, Lorenzi M, Behnke BJ, Leeuwenburgh C. Mitochondrial dysfunction and sarcopenia of aging: from signaling pathways to clinical trials. Int J Biochem Cell Biol 2013; 45: 2288–2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dideriksen K, Reitelseder S, Holm L. Influence of amino acids, dietary protein, and physical activity on muscle mass development in humans. Nutrients 2013; 5: 852–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Argilés JM, Busquets S, López‐Soriano FJ, Costelli P, Penna F. Are there any benefits of exercise training in cancer cachexia? J Cachexia Sarcopenia Muscle 2012; 3: 73–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Puppa MJ, White JP, Velázquez KT, Baltgalvis KA, Sato S, Baynes JW, Carson JA. The effect of exercise on IL‐6‐induced cachexia in the Apc (Min/+) mouse. J Cachexia Sarcopenia Muscle 2012; 3: 117–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Laoutaris ID, Adamopoulos S, Manginas A, Panagiotakos DB, Kallistratos MS, Doulaptsis C, Kouloubinis A, Voudris V, Pavlides G, Cokkinos DV, Dritsas A. Benefits of combined aerobic/resistance/inspiratory training in patients with chronic heart failure. A complete exercise model? A prospective randomised study. Int J Cardiol. 2013; 167: 1967–1972. [DOI] [PubMed] [Google Scholar]
- 54. Benavent‐Caballer V, Rosado‐Calatayud P, Segura‐Ortí E, Amer‐Cuenca JJ, Lisón JF. Effects of three different low‐intensity exercise interventions on physical performance, muscle CSA and activities of daily living: a randomized controlled trial. Exp Gerontol 2014; 58: 159–165. [DOI] [PubMed] [Google Scholar]
- 55. Rhee CM, Kalantar‐Zadeh K. Resistance exercise: an effective strategy to reverse muscle wasting in hemodialysis patients? J Cachexia Sarcopenia Muscle 2014; 5: 177–180, doi: 10.1007/s13539-014-0160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Habedank D, Meyer FJ, Hetzer R, Anker SD, Ewert R. Relation of respiratory muscle strength, cachexia and survival in severe chronic heart failure. J Cachexia Sarcopenia Muscle 2013; 4: 277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Laoutaris ID, Adamopoulos S, Manginas A, Kallistratos MS, Cokkinos DV, Voudris V, Pavlides G, Dritsas A. Inspiratory muscle work capacity is more severely depressed than inspiratory muscle strength in patients with chronic heart failure. Eur Heart J 2012; 33: 1056 [Abstract Supplement]. [Google Scholar]
- 58. Gallot YS, Durieux AC, Castells J, Desgeorges MM, Vernus B, Plantureux L, Rémond D, Jahnke VE, Lefai E, Dardevet D, Nemoz G, Schaeffer L, Bonnieu A, Freyssenet DG. Myostatin gene inactivation prevents skeletal muscle wasting cancer. Cancer Res 2014; Doi: pii: canres.0057.2014. [DOI] [PubMed] [Google Scholar]
- 59. Morley JE, Anker SD, von Haehling S. Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology‐update 2014. J Cachexia Sarcopenia Muscle 2014; 5: 253–259, doi: 10.1007/s13539-014-0161-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sandek A, von Haehling S, Anker SD. Muscle in heart disease: highlights from the European Society of Cardiology's Annual Meeting 2012. Int J Cardiol 2012; 161: 126–129. [DOI] [PubMed] [Google Scholar]
- 61. Wandrag L, Brett SJ, Frost G, Hickson M. Impact of supplementation with amino acids or their metabolites on muscle wasting in patients with critical illness or other muscle wasting illness: a systematic review. J Hum Nutr Diet. 2014; doi: 10.1111/jhn.12238. [DOI] [PubMed] [Google Scholar]
- 62. Quanjun Y, Genjin Y, Lili W, Bin L, Jin L, Qi Y, Yan L, Yonglong H, Cheng G, Junping Z. Serum metabolic profiles reveal the effect of formoterol on cachexia in tumor‐bearing mice. Mol Biosyst 2013; 9: 3015–3025. [DOI] [PubMed] [Google Scholar]
- 63. White HK, Petrie CD, Landschulz W, MacLean D, Taylor A, Lyles K, Wei JY, Hoffman AR, Salvatori R, Ettinger MP, Morey MC, Blackman MR, Merriam GR, Capromorelin Study Group . Effects of an oral growth hormone secretagogue in older adults. J Clin Endocrinol Metab 2009; 94: 1198–1206. [DOI] [PubMed] [Google Scholar]
- 64. Dalton JT, Barnette KG, Bohl CE, Hancock ML, Rodriguez D, Dodson ST, Morton RA, Steiner MS. The selective androgen receptor modulator GTx‐024 (enobosarm) improves lean body mass and physical function in healthy elderly men and postmenopausal women: results of a double‐blind, placebo‐controlled phase II trial. J Cachexia Sarcopenia Muscle 2011; 2: 153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Dobs AS, Boccia RV, Croot CC, Gabrail NY, Dalton JT, Hancock ML, Johnston MA, Steiner MS. Effects of enobosarm on muscle wasting and physical function in patients with cancer: a double‐blind, randomised controlled phase 2 trial. Lancet Oncol 2013; 14: 335–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Neelemaat F, Bosmans JE, Thijs A, Seidell JC, van Bokhorst‐de van der Schueren MA. Post‐discharge nutritional support in malnourished elderly individuals improves functional limitations. J Am Med Dir Assoc 2011; 12: 295–301. [DOI] [PubMed] [Google Scholar]
- 67. Russ DW, Gregg‐Cornell K, Conaway MJ, Clark BC. Evolving concepts on the age‐related changes in “muscle quality”. J Cachexia Sarcopenia Muscle 2012; 3: 95–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Sumukadas D, Witham MD, Struthers AD, McMurdo ME. Effect of perindopril on physical function in elderly people with functional impairment: a randomized controlled trial. CMAJ 2007; 177: 867–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Page ST, Amory JK, Bowman FD, Anawalt BD, Matsumoto AM, Bremner WJ, Tenover JL. Exogenous testosterone (T) alone or with finasteride increases physical performance, grip strength, and lean body mass in older men with low serum T. J Clin Endocrinol Metab 2005; 90: 1502–1510. [DOI] [PubMed] [Google Scholar]
- 70. Kwon J, Yoshida Y, Yoshida H, Kim H, Suzuki T, Lee Y. Effects of a combined physical training and nutrition intervention on physical performance and health‐related quality of life in prefrail older women living in the community: a randomized controlled trial. J Am Med Dir Assoc 2015, pii: S1525‐8610(14)00800‐7. [DOI] [PubMed] [Google Scholar]
- 71. Aquilani R, Opasich C, Gualco A, Verri M, Testa A, Pasini E, Viglio S, Iadarola P, Pastoris O, Dossena M, Boschi F. Adequate energy‐protein intake is not enough to improve nutritional and metabolic status in muscle‐depleted patients with chronic heart failure. Eur J Heart Fail 2008; 10: 1127–1135. [DOI] [PubMed] [Google Scholar]
- 72. Osterziel KJ, Strohm O, Schuler J, Friedrich M, Hänlein D, Willenbrock R, Anker SD, Poole‐Wilson PA, Ranke MB, Dietz R. Randomised, double‐blind, placebo‐controlled trial of human recombinant growth hormone in patients with chronic heart failure due to dilated cardiomyopathy. Lancet 1998; 351: 1233–1237. [DOI] [PubMed] [Google Scholar]
- 73. Caminiti G, Volterrani M, Marazzi G, Cerrito A, Massaro R, Sposato B, Arisi A, Rosano G. Hydrotherapy added to endurance training versus endurance training alone in elderly patients with chronic heart failure: a randomized pilot study. Int J Cardiol 2011; 148: 199–203 [DOI] [PubMed] [Google Scholar]
- 74. Lenk K, Erbs S, Höllriegel R, Beck E, Linke A, Gielen S, Winkler SM, Sandri M, Hambrecht R, Schuler G, Adams V. Exercise training leads to a reduction of elevated myostatin levels in patients with chronic heart failure. Eur J Prev Cardiol 2012; 19: 404–411. [DOI] [PubMed] [Google Scholar]
- 75. Harrington D, Chua TP, Coats AJ. The effect of salbutamol on skeletal muscle in chronic heart failure. Int J Cardiol 2000; 73: 257–265. [DOI] [PubMed] [Google Scholar]


