Sir,
Adamantinoma is a rare malignant tumor of the bone constituting 0.1%–0.5% of all primary bone tumors.[1] It has a predilection for long bone involvement, especially the tibia in 80%–85% of the cases.[2] Management requires early recognition and timely biopsy with wide local excision. Pulmonary metastasis is usually parenchymal, with few reports of pneumothorax and two instances of endobronchial metastasis reported in literature till date.[3,4] We describe an unusual case with extensive pulmonary involvement and respiratory failure. The patient had extensive endobronchial involvement with postobstructive pneumonia; this necessitated bronchoscopic debulking. The options were flexible bronchoscopy under sedation or rigid bronchoscopy under general anesthesia (GA). He was taken up for rigid bronchoscopic debulking due to respiratory failure for better control of airway.
A 31-year-old male patient presented to the emergency department with respiratory failure and fever. Evaluation revealed multiple cavitating pulmonary masses with right hydropneumothorax and extensive subcutaneous emphysema [Figure 1a]. The patient gave a history of surgery for adamantinoma of right tibia 7 years ago and had remained symptom free for 5 years thereafter. He had received six cycles of adriamycin with cyclophosphamide-based chemotherapy followed by oral everolimus for 4 months. He was managed with chest drain and taken up for right pleurodesis with povidone-iodine once air leak settled. The patient had room air SpO2 of 94%, and computed tomography (CT) chest [Figure 1b] and bronchoscopy revealed extensive endobronchial metastasis, causing total obstruction of the left upper lobe and partial obstruction of left lower lobe [Figure 2a]. At this point, the patient was afebrile and was comfortable at rest. The patient was explained that if he develops symptoms of postobstructive pneumonia or dyspnea, he will require management of endobronchial metastasis. The patient presented 15 days later to the emergency department in respiratory failure requiring noninvasive ventilation with high-grade fever, and CT revealed persistent air-fluid level on the left side [Figure 1c]. The patient was taken up for rigid bronchoscopy under GA, and sequential debulking of endobronchial lesions was done from both sides using cryoprobe [Figure 2b] for relieving the obstruction. The procedure included several cycles of cryoactivation with piecemeal extraction of multifocal disease, leading to relief of obstruction. The patient demonstrated improvement in oxygenation and was extubated on table. The histology was consistent with metastatic adamantinoma [Figure 3a and b]. Over the next couple of days, the patient became afebrile and was weaned off noninvasive ventilation and oxygen. He was discharged and remained ambulant without respiratory support for 126 days.
Figure 1.
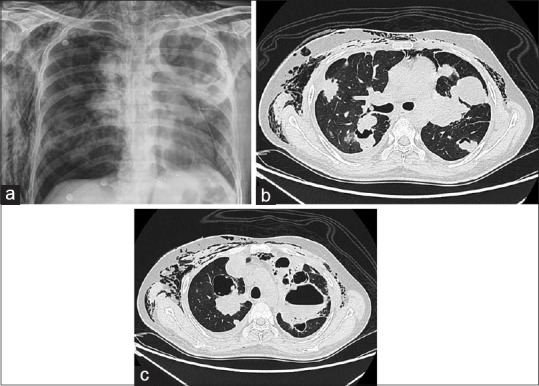
(a) Initial presentation with right pneumothorax and extensive subcutaneous emphysema. (b) Endobronchial, parenchymal metastasis with pleural extension. (c) Postobstructive pneumonia with air-fluid level in the left upper lobe
Figure 2.
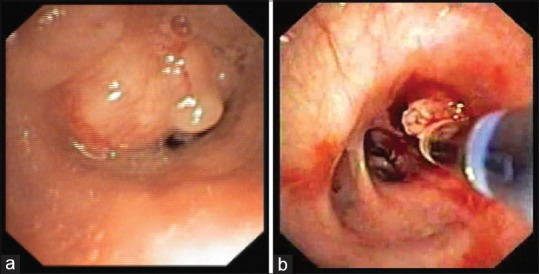
(a) Extensive endobronchial metastasis – bronchoscopic view. (b) Cryo debulking of endobronchial metastasis
Figure 3.
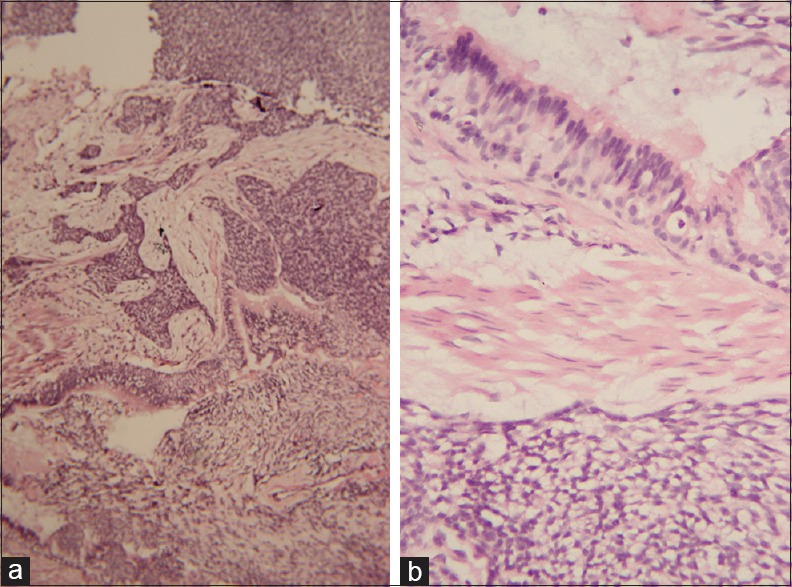
(a) Low power microscopic view of adamantinoma. (b) Adamantinoma – reversal of nuclear polarity
Commonly reported pulmonary metastasis of adamantinoma is parenchymal nodules/masses. Accepted treatment strategy is metastasectomy when feasible. Disease-free survival of up to 4 years and survival beyond 6 years with recurrence have been described after pulmonary metastasectomy.[5,6] In our case, the first presentation itself revealed extensive bilateral parenchymal involvement and hence metastasectomy with curative intent was not an option. There have been several reports of secondary spontaneous pneumothorax due to either pleural metastasis or rupture of a peripherally placed lung mass.[7] Management in the cases encountered had ranged from metastasectomy to chest tube drainage and pleurodesis.[7,8] In our case, pleurodesis was the only option feasible due to extensive nature of the pulmonary disease. Bronchoscopy of the two cases with suspected endobronchial metastasis had confirmed the same, and these patients subsequently succumbed to respiratory insufficiency.[3,4] Our patient had an extremely rare presentation consisting of symptomatic parenchymal, pleural, and endobronchial involvement. The presence of endobronchial obstruction with recurrent postobstructive pneumonia and the inherently slow-growing nature of disease allowed us to explore the possibility of endobronchial debulking.
Bronchoscopic debulking provides swift relief of symptoms as it improves ventilation. In our case, it also lead to drainage of secretions and helped control of infection. Options include flexible bronchoscopy or rigid bronchoscopy for a conduit. Rigid conduit was used as it provides better airway control as well as providing adequate space for using multiple accessories. Several tools exist for achieving debulking depending on the nature of tumor. In case of polypoid tumor with narrow base electrocautery snare is an ideal tool for excision and achieving hemostasis at the same time. For broad-based tumors, the bevel of rigid scope, blunt cautery probe, laser, rigid biopsy forceps, or cryobiopsy probe can be used to debulk. Cryo avulsion was chosen due to distal and multifocal nature of disease. This should be done with caution as avulsion can lead to significant bleeding from the tumor bed and the same should be handled by appropriate measures including tamponade and argon plasma coagulation.
Adamantinoma is a rare tumor of the bone for which early appropriate wide local excision remains the standard of care. Lung lesions are best managed by metastasectomy when feasible. In cases with extensive lung lesions like in ours, pleurodesis in case of pneumothorax and rigid bronchoscopic debulking of endobronchial metastasis can help in palliation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thankfully acknowledge the staff members of the bronchoscopy suite (Mrs. Sathya Janani, Mr. Uma Maheshwaran, Mrs. Anitha, and Miss. Kalpana) for assisting in interventional procedures and collecting reliable and meaningful information about our study subject. We thank Mrs. Sai Chandini Krishnamoorthy for editing the manuscript.
REFERENCES
- 1.Gebhardt MC, Lord FC, Rosenberg AE, Mankin HJ. The treatment of adamantinoma of the tibia by wide resection and allograft bone transplantation. J Bone Joint Surg Am. 1987;69:1177–88. [PubMed] [Google Scholar]
- 2.Keeney GL, Unni KK, Beabout JW, Pritchard DJ. Adamantinoma of long bones. A clinicopathologic study of 85 cases. Cancer. 1989;64:730–7. doi: 10.1002/1097-0142(19890801)64:3<730::aid-cncr2820640327>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 3.De Keyser F, Vansteenkiste J, Van Den Brande P, Demedts M, Van de Woestijne KP. Pulmonary metastases of a tibia adamantinoma. Case report and review of the literature. Acta Clin Belg. 1990;45:31–3. doi: 10.1080/17843286.1990.11718062. [DOI] [PubMed] [Google Scholar]
- 4.Van Schoor JX, Vallaeys JH, Joos GF, Roels HJ, Pauwels RA, Van Der Straeten ME, et al. Adamantinoma of the tibia with pulmonary metastases and hypercalcemia. Chest. 1991;100:279–81. doi: 10.1378/chest.100.1.279. [DOI] [PubMed] [Google Scholar]
- 5.Van Geel AN, Hazelbag HM, Slingerland R, Vermeulen MI. Disseminating adamantinoma of the tibia. Sarcoma. 1997;1:109–11. doi: 10.1080/13577149778399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flug JA, Scalcione LR, Hakima L, Ganson G, Mazzie JP, Katz DS, et al. Radiologic-pathologic findings of primary osseous adamantinoma with unusual metastasis to the posterior cul-de-sac in pregnancy. Clin Imaging. 2011;35:483–7. doi: 10.1016/j.clinimag.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Gonçalves R, Saad Junior R, Dorgan Neto V, Botter M. A rare case of pneumothorax: Metastatic adamantinoma. J Bras Pneumol. 2008;34:425–9. doi: 10.1590/s1806-37132008000600014. [DOI] [PubMed] [Google Scholar]
- 8.Winter WG., Jr Spontaneous pneumothorax heralding metastasis of admantinoma of the tibia. Report of two cases. J Bone Joint Surg Am. 1976;58:416–7. [PubMed] [Google Scholar]


