Abstract
Injuries of the posterolateral corner (PLC) of the knee lead to chronic lateral and external rotational instability. Successful treatment of PLC injuries requires an understanding of the complex anatomy and biomechanics of the PLC. Several open PLC reconstruction techniques have been published. It is understood that anatomic reconstruction is superior to extra-anatomic techniques, leading to better clinical results. An open, anatomic, fibula-based technique for reconstruction to address lateral and rotational instability has been described. However, when an open technique is used, surgeon and patient are faced with disadvantages, such as soft tissue damage or exposure of vulnerable structures. Few arthroscopic techniques for tibia- or fibula-based reconstruction of rotational posterolateral instability have been described. A complete arthroscopic stabilization of the combined lateral and posterolateral rotational instability of the knee has not yet been described. We therefore present the first all-arthroscopic technique for complete PLC reconstruction, based on an open technique described previously. All relevant landmarks of the PLC can be arthroscopically visualized in detail, allowing safe and effective treatment of PLC injuries.
The posterolateral corner (PLC) consists primarily of the lateral collateral ligament (LCL) and the popliteus complex (PTC), which includes the popliteus muscle tendon (PLT) unit and the arcuate complex.1, 2 The arcuate complex contains the popliteofibular ligament, the fabellofibular ligament, and the popliteomeniscal fibers.2, 3 Functionally, the arcuate complex acts as a static stabilizer of the tibia against external rotation and, in synergy with the PLT, against posterior translation.1, 2, 3
Depending on the involvement of injured structures, PLC injury may lead to posterolateral rotational instability (Fanelli A) or posterolateral rotational instability and lateral instability (Fanelli B/C).4 For Fanelli A, the popliteus bypass technique leads to effective stabilization of the PLC.2, 5 However, if a concomitant lateral instability is observed (Fanelli B/C), an additional reconstruction of the LCL is necessary to stabilize the PLC effectively, as described by LaPrade et al.1 and other investigators.2, 5, 6
Despite their frequent association with injuries of the posterior cruciate ligament (PCL), PLC injuries are often underdiagnosed and therefore remain untreated, resulting in chronic posterolateral rotational instability and insufficiency of cruciate ligament reconstructions.4, 7, 8, 9
Several open surgical techniques for PLC reconstruction have been previously described.6, 8, 10, 11, 12 Extra-anatomic procedures, such as the modified Larson technique, lack sufficient dorsal stabilization.2, 6, 11, 12, 13 Therefore, more anatomic procedures have been developed.10, 14, 15 Strict consideration of anatomic landmarks and precise placement of femoral and fibular attachments are crucial for effective posterolateral stabilization.2, 6
Arciero14 introduced a fibula-based technique with an anatomic transfibular tunnel placement, from anterolateral to posteromedial, in accordance with the native functional anatomy of the LCL and PTC (Fig 1).6 This technique is indicated in cases of LCL and PTC injury with subsequent posterolateral rotational instability.6, 14 Most recently, arthroscopic techniques for PTC reconstruction, which combine the less invasive approach of arthroscopy with the precise localization of anatomic landmarks, have evolved.9, 16 Herein, we introduce the first all-arthroscopic technique for posterolateral stabilization in accordance with the procedure devised by Arciero,14 using a free tendon graft.
Fig 1.
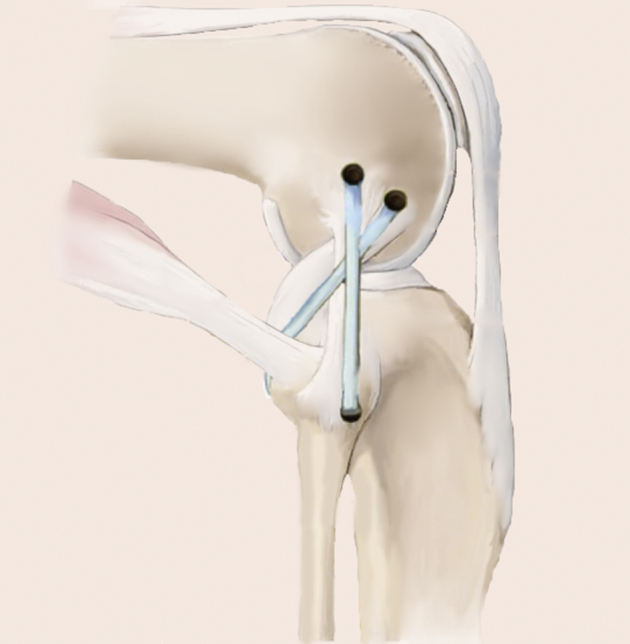
A fibula-based technique, as described by Arciero,14 can be used for anatomic reconstruction of the posterolateral corner. The graft is fixed precisely at the anatomic femoral footprints of the LCL and PLT, and the fibular tunnel is drilled in an anterolateral-to-posteromedial direction, to anatomically reconstruct the LCL and PLT footprints. (LCL, lateral collateral ligament; PLT, popliteus muscle tendon.)
This technique is indicated for posterolateral instabilities, Fanelli grades B and C.4
With the technique described in this Technical Note, the lateral (varus) instability and the external rotational instability can be addressed. In most patients, an additional posterior instability is present, which is treated by additional PCL reconstruction. The arthroscopic approach may be used in any case of posterolateral reconstruction; it has the advantages of smaller skin incisions, potentially lower infection rates, and more precise localization of anatomic landmarks for graft positioning. Furthermore, it may be indicated for complex injuries of the knee, which are often associated with compromised soft tissue, leaving little space for large surgical approaches.
Surgical Technique
Step 1: Portal Development
Arthroscopic posterolateral stabilization requires 5 portals: high anterolateral, high anteromedial, posteromedial, posterolateral, and parapatellar lateral. First, the high anterolateral and anteromedial portals are developed in the standard manner, and an anteromedial portal is added by introducing a needle and then making a stab incision. After the high anterolateral and anteromedial portals are developed, the arthroscope is placed in the anteromedial portal, advanced below the PCL and into the posteromedial recessus. To develop the posteromedial portal, a needle should be used to localize the correct placement under arthroscopic vision before the stab incision is made. A shaver (Excalibur; Arthrex, Naples, FL) is introduced through the posteromedial portal, and the dorsal septum is carefully resected (transseptal approach), while the popliteal nerves and vessels are protected meticulously. Next, the arthroscope is switched to the posteromedial portal, and a posterolateral portal is developed, again beginning with a needle, which should be inserted anterior to the biceps femoris tendon to protect the peroneal nerve. To facilitate the following steps, the posterolateral portal must not be placed far posterior.
Step 2: Preparing the PLC
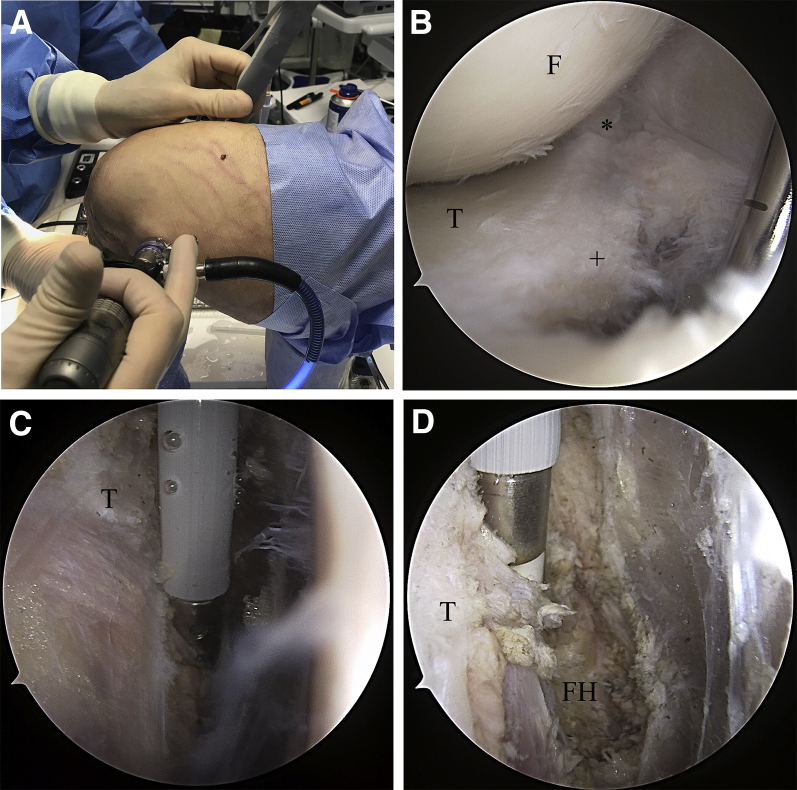
Through the posterolateral portal, capsular fibers dorsal to the popliteus tendon are resected with either a shaver or a radiofrequency electrode to expose the popliteus tendon. Directly lateral and distal to the popliteus tendon, the fibular head can be palpated and subsequently exposed by gentle preparation of the surrounding soft tissue17 (Fig 2). During preparation of the fibular head, the risk of injuring the peroneal nerve can be minimized by continuous visualization and avoidance of preparation past its posterior edge.
Fig 2.
For arthroscopic preparation and exposure of the FH (right knee), the patient is placed in the supine position, with the knee secured in an electric leg holder. (A) The dorsolateral recessus can be observed through the posteromedial portal. (B) The posterolateral portal provides access to the capsular fibers (+) posterior to the PLT; these fibers are resected with a shaver (Excalibur, Arthrex) to expose the PLT (*) and the FH. (C) A radiofrequency electrode is used to carefully resect soft tissue until the FH is exposed. (D) Care should be taken to protect the peroneal nerve, which is located an additional 2 to 3 cm distally, as well as the popliteal nerves and vessels. (F, femur; FH, fibular head; PLT, popliteus muscle tendon; T, tibia.)
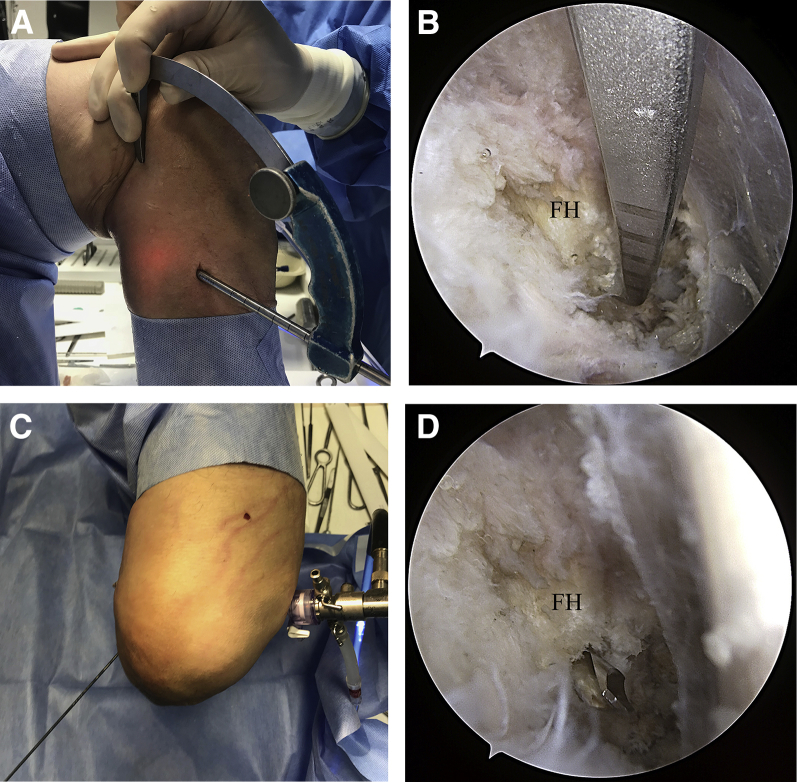
Step 3: Fibular Tunnel Placement
With the arthroscope placed in the posteromedial portal, a drill guide (AR-1510F; Arthrex) is inserted through the posterolateral portal and placed on the dorsomedial surface of the fibular head. A small stab incision is made on the anterolateral portion of the fibular head, and a guidewire is inserted in the anterolateral-to-posteromedial direction under arthroscopic visualization. It is then overdrilled with a 5- or 6-mm cannulated drill (Fig 3). Care must be taken to avoid placing the tunnel too proximal in the fibular head to ensure safe fixation of the graft.
Fig 3.
For preparation of the fibular tunnel (right knee, supine position, arthroscope in posteromedial portal), a tibial drill guide (AR-1510F; Arthrex) is introduced through the posterolateral portal. (A) A small incision is made anteroposterior to the FH, which can be easily palpated. (B) The tip of the drill guide is placed on the dorsomedial surface of the FH, which is visualized arthroscopically through the posteromedial portal. (C) A guidewire is then introduced in an anterolateral-to-posteromedial direction under arthroscopic visualization. (D) The fibular tunnel is drilled with a 5- or 6-mm drill, depending on the diameter of the tendon graft. (FH, fibular head.)
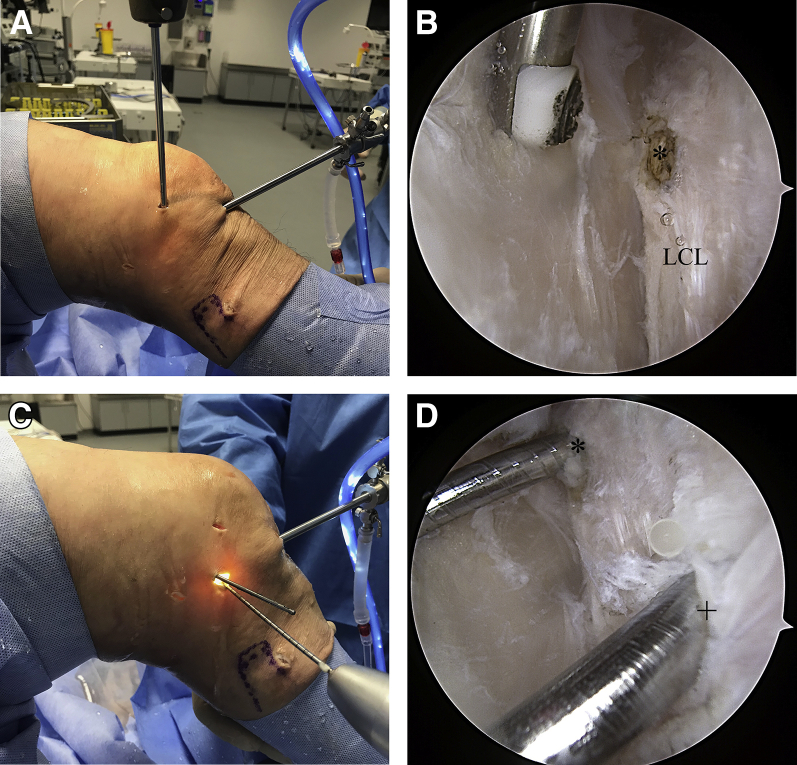
Step 4: Femoral Footprint Preparation and Tunnel Placement
The arthroscope is advanced through the high anterolateral portal to the lateral femoral epicondyle, and a lateral parapatellar portal is developed. The lateral joint capsule is carefully resected with the shaver (Torpedo; Arthrex) to expose the femoral attachments of the LCL and PLT, as previously described.2 At this point, addition of a stay suture can be helpful to retract the iliotibial band, providing better visualization. Eyelet wires are then drilled through a lateral stab incision into the femoral footprints of the LCL and PLT, which are then overdrilled with a 5- or 6-mm cannulated drill (Fig 4).
Fig 4.
To prepare the femoral tunnels (right knee, supine position, slightly flexed angle), the arthroscope is introduced through the high anterolateral portal, and a parapatellar portal is developed for the shaver. (A) The lateral joint capsule is carefully resected with the shaver (Torpedo; Arthrex) to expose the femoral attachments of the LCL (*) and PLT. The femoral footprints can be marked with a radiofrequency electrode for better orientation. A stab incision is made directly over the femoral attachments. (C) Two guidewires are introduced into the native origins of the LCL (*) and PLT (+). (D) The femoral tunnels are then drilled with a 5- or 6-mm drill, depending on the strength of the graft. The PLT tunnel should have a length of approximately 3 cm, and the LCL tunnel should be of greater depth to allow full graft tensioning. (LCL, lateral collateral ligament; PLT, popliteus muscle tendon.)
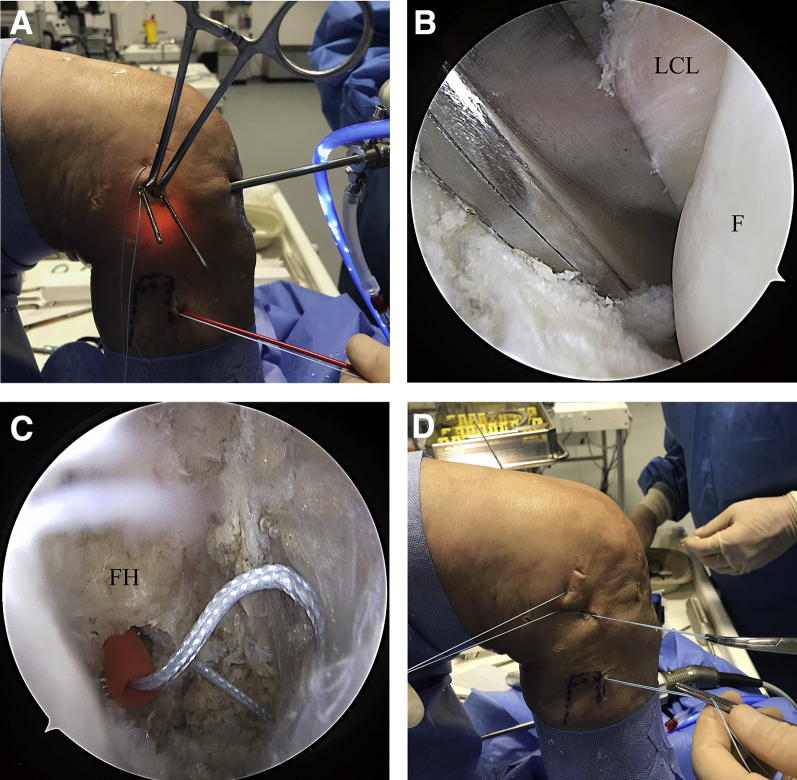
Step 5: Graft Positioning
We recommend an armed gracilis or semitendinosus tendon graft, with a length of at least 20 cm. First, the graft is pulled into the femoral PLT tunnel and fixed with a bioabsorbable screw under arthroscopic visualization through the anterolateral portal. A bent clamp is introduced through the lateral stab incision; the clamp is passed along the original path of the native popliteus tendon and down to the posterior end of the fibular tunnel. The arthroscope is then placed in the posteromedial portal, and a FiberStick (Arthrex) is introduced through the fibular tunnel in an anterior-to-posterior direction to implement a shuttling suture, which is then retrieved with the clamp and pulled back to the lateral epicondyle. The graft is then shuttled into the knee, along the native popliteus tendon, and through the fibular tunnel in the posterior-to-anterior direction (Fig 5). It is then fixed in the fibular tunnel with another bioabsorbable screw, with the knee at 80° to 90° of flexion (Fig 6). Arthroscopic observation is required during this step to ensure anatomic placement of the graft, analogous to the course of the native PLT (Video 1). Finally, the graft is pulled into the LCL tunnel and fixed with a bioabsorbable screw, at 20° to 30° of flexion (Fig 7).
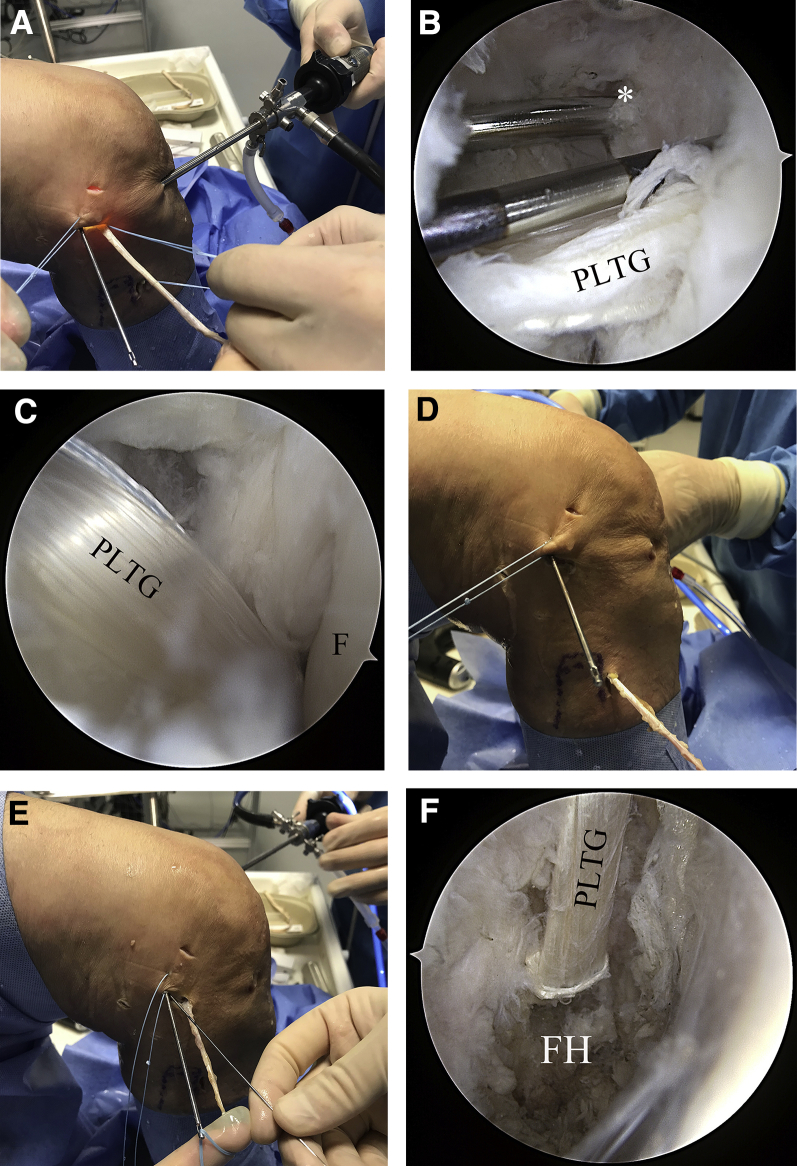
Fig 5.
Anatomic graft positioning requires an exact implementation of the shuttling sutures, following the course of the native PLT (right knee, supine position). (A) To obtain a better overview, stay sutures can be used to retract the iliotibial band. (B) A bent clamp is introduced through the lateral stab incision and is then passed down along the popliteus tendon. This step should be observed arthroscopically to ensure correct placement. (C) A FiberStick is inserted through the fibular tunnel, and the FiberWire is passed into the posterolateral recessus, where it is grasped with the bent clamp. (D) The FiberWire is then shuttled through the lateral stab incision and the fibular tunnel. To provide more space for the clamp, the femoral guidewires may be retracted so that the tips slightly overtop the lateral cortex. (PLT, popliteus muscle tendon.)
Fig 6.
We recommend using a gracilis or semitendinosus tendon graft, with a length of at least 20 cm. (A) The armed graft is shuttled into the femoral PLT tunnel and fixed with a bioabsorbable interference screw. (B) Again, a nitinol wire may be of use for retaining the tunnel position while the PLTG is fixed; the LCL (*) drill channel can be seen posterior to the PLT tunnel. (C) The PLTG is then shuttled into the posterolateral recessus, along the native PLT. At this point, precise anatomic placement of the graft is crucial. Interposition of soft tissue must be meticulously avoided. (D) The graft is further shuttled through the fibular tunnel in the posteromedial-to-anterolateral direction. (E) The graft is then shuttled to the lateral stab incision and into the femoral LCL tunnel. (F) The implanted PLTG can be observed though the posteromedial portal. (LCL, lateral collateral ligament; PLT, popliteus muscle tendon; PLTG, popliteus tendon graft.)
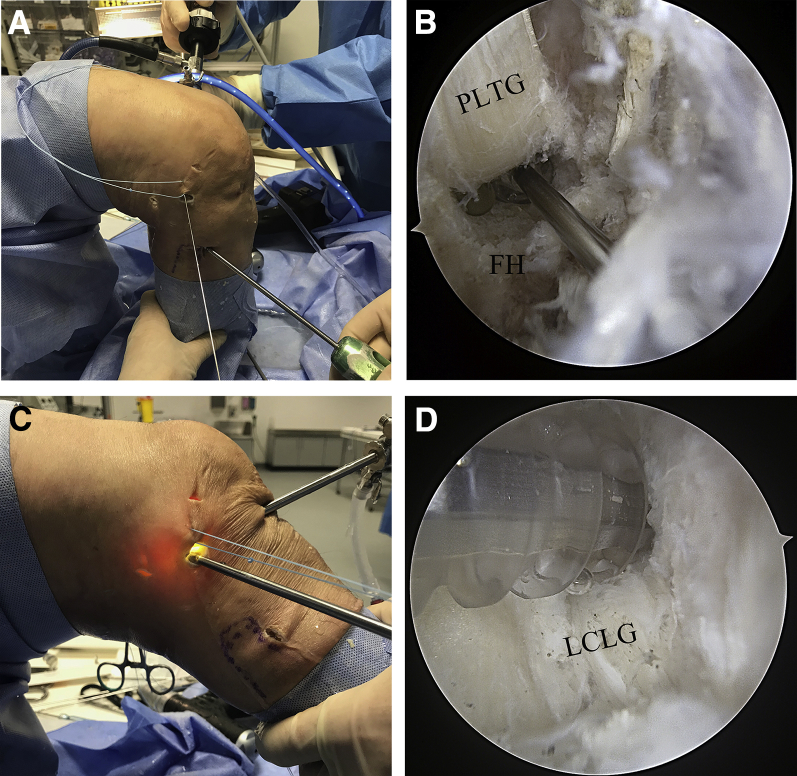
Fig 7.
(A) During fibular graft fixation (right knee, supine position), the knee is bent to 90°, and the graft is carefully tightened. (B) A bioabsorbable interference screw is introduced along a nitinol wire into the fibular tunnel. Correct screw placement can be verified under arthroscopic visualization. (C) After PLT fixation, the graft is fixed in the LCL tunnel while the knee is bent to 20° to 30° of flexion. (D) During fixation with a bioabsorbable interference screw, overtopping of the screws must be prevented by means of arthroscopic visualization to avoid painful soft tissue irritation. (LCL, lateral collateral ligament; PLT, popliteus muscle tendon.)
Rehabilitation
Isolated injuries of the PLC are rare, which is why there is no standardized rehabilitation protocol after PLC reconstruction.4 Therefore, postoperative treatment should be planned individually, depending on the combination of accompanying injuries.
For example, in combination with a surgically treated tear of the PCL, the rehabilitation protocol for PCL reconstruction may be modified in favor of the PLC. A hard-frame orthotic with posterior tibial support is recommended to protect the knee from varus stress. Mobilization should be restricted to partial weight bearing for 6 weeks, and joint mobilization should be limited to passive motion with limited flexion for about 6 weeks, depending on the injury pattern.
Discussion
Posterolateral injuries cause severe disruption of normal knee function.10 Posterolateral reconstruction becomes imperative in successful restoration of dorsal and external rotational stability and determines the durability of anterior cruciate ligament and PCL reconstructions, especially against the background of the synergistic function of the PCL and PLC.7, 8 However, precise knowledge of and compliance with anatomic landmarks are essential.1, 2, 6
Open anatomic techniques have refined posterolateral reconstruction with respect to native anatomy; however, detailed exposure inevitably compromises the surrounding soft tissue.2, 10, 14 All-arthroscopic anatomic PLC reconstruction combines the less invasive approach of arthroscopy with the maximized precision of anatomic tunnel placement and graft positioning in accordance with previously described techniques.2, 6, 9, 14 In contrast to the technique described by LaPrade et al.,1 only 1 tendon graft is required to reconstruct the PLC. Furthermore, anatomic landmarks can be visualized in detail and without destruction of surrounding structures. Moreover, vulnerable structures, such as the peroneal nerve, are not exposed, thus reducing the risk of nerve injury. Other procedures, such as PCL or anterior cruciate ligament reconstruction, can be performed simultaneously without extended or additional surgical approaches.
The arthroscopic popliteus bypass technique, described by Frosch et al.,2 was the first arthroscopic approach to posterolateral reconstruction. The authors demonstrated a high level of accuracy and reproducibility, based on detailed visualization of all substantial anatomic landmarks.2 Hermanowicz et al.9 used a similar approach to develop the arthroscopic popliteus tenodesis technique. However, in the presence of additional lateral instability (Fanelli B), a popliteus bypass graft does not provide sufficient lateral stabilization, and alternative techniques, as described by Rios et al.6 or LaPrade et al.,1 are necessary.
Certainly, arthroscopic posterolateral reconstruction requires significant experience in the field of arthroscopic surgery. Furthermore, the surgeon must be aware of the complex anatomy and kinematic properties of the PLC. Important key steps of the procedure described in this article must be meticulously considered because they are crucial for the success of the technique (Table 1). In addition, injured knees may present altered anatomy, in contrast to uninjured human cadaver knees, subsequently limiting intraoperative orientation.2
Table 1.
Key Steps, Perils, and Pitfalls in All-Arthroscopic Posterolateral Reconstruction
| Portal development | The posterolateral portal should be placed close to the femoral condyle to gain full access to the fibular head. A posterolateral portal positioned too posteriorly may limit the exposure. |
| Preparation of the PLT and fibular head | Preparation of the fibular head should be performed close to and directly posterior to the popliteus tendon. A more dorsal preparation must be avoided to protect the peroneal nerve and the popliteal nerves and vessels. The peroneal nerve is located 2 to 3 cm distal to the popliteus tendon. Sudden muscle contraction may indicate proximity to the peroneal nerve. |
| Fibular tunnel placement | For better orientation, the fibular head can be palpated through the skin before the stab incision is created. The direction of tunnel placement should be from anterolateral to posteromedial. |
| Preparation of the femoral attachments of LCL and PLT | A stay suture may be used to retract the iliotibial band, to provide more space and better visualization, during preparation. During gentle resecting, the lateral joint capsule and the lateral distal femur can be exposed. For better orientation, the femoral footprints of the LCL and PLT can be marked with a radiofrequency electrode (Fig 3B). |
| Femoral tunnel placement | The drilled LCL tunnel should be sufficiently long to provide space for the tendon graft, and the PLT tunnel should be approximately 3 cm long. |
| Graft fixation and implantation | For anatomic reconstruction, it is essential to first fix the graft to the femoral PLT footprint. During reconstruction of the PLT, the graft must be shuttled along the course of the native PLT and underneath the native LCL. Fibular graft fixation must be performed before LCL fixation. A nitinol wire is helpful to ensure correct placement of the interference screw in the tunnel (Fig 5B). |
LCL, lateral collateral ligament; PLT, popliteus muscle tendon.
In the presence of accompanying tibial head fractures, an increased risk for development of a compartment syndrome may further limit the field of application. Finally, the treatment of extremely overweight patients may pose a limitation to any arthroscopic technique because of a massive layer of surrounding soft tissue (Table 2). However, in experienced hands, this procedure is a safe, fast, and anatomic method for posterolateral stabilization, suitable for clinical application (Table 2).
Table 2.
Advantages and Disadvantages of the Technique
| Advantages | Risks, Disadvantages, and Limitations |
|---|---|
| Less invasive approach with little trauma to surrounding soft tissue | Requires profound knowledge of the complex anatomy of the posterolateral corner |
| Protection of the peroneal nerve | Advanced arthroscopic skills required |
| Exact location of anatomic landmarks | Increased risk of compartment syndrome in cases of accompanying tibial head fractures |
| Precise tunnel placement and anatomic graft positioning | Potentially limited by extremely thick soft tissue layer and extreme obesity |
| No prolonged surgery time in comparison with open techniques | |
| Simultaneous treatment of concomitant injuries |
Footnotes
This study was funded by Arthrex (Naples, FL, USA). J. Frings, J. Kolb, and K.-H. Frosch have been compensated in terms of travel expenses to Arthrex facilities. ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The posterolateral corner consists of the lateral collateral ligament (LCL) and the popliteus complex, which comprises the popliteus muscle tendon unit and the arcuate complex. The popliteus complex, especially the arcuate complex, stabilizes the knee against external rotation and, together with the posterior cruciate ligament, against posterior translation. The LCL acts as the main stabilizer against varus stress.
For surgical stabilization, anatomic reconstruction techniques, as described by Arciero14 or LaPrade et al.1, have been shown to be superior to extra-anatomic techniques. In this video, we present the all-arthroscopic reconstruction of the posterolateral corner in accordance with the technique described by Arciero.14
For this technique, 5 arthroscopic portals are required: a high anterolateral, a high anteromedial, a posteromedial, a posterolateral, and a lateral parapatellar portal.
After the posteromedial and posterolateral portals are developed, the popliteocapsular fibers are carefully resected with a shaver to visualize the popliteus tendon. It should be noted that preparation is started directly dorsal to the visible popliteus tendon, which is highlighted in the video by a green arrow.
A radiofrequency electrode can be used to prepare the fibular head. During preparation of the fibular head, it is important to stay close to the tibia to prevent injury to important popliteal structures. As demonstrated in the video, the fibular head can be identified nicely under arthroscopic vision by gently palpating it from the outside.
For preparation of the fibular tunnel, a tibial popliteus drill guide is introduced through the posterolateral portal and placed on the fibular head. After the anterior edge of the fibular head has been palpated, a small skin incision is made to position the drill guide. A guidewire is then inserted in an anterolateral-to-posteromedial direction under arthroscopic vision. It is then overdrilled with a 5- or 6-mm drill, depending on the diameter of the tendon graft. The risk of injury of the peroneal nerve can be minimized by continuous visualization of the fibular head during this step.
In the following step, the femoral tunnels are prepared. The arthroscope is placed in the anterolateral portal to visualize the lateral epicondyle, and a parapatellar portal is developed. To visualize the femoral footprints of the LCL and the popliteus tendon, the lateral joint capsule must be gently removed, for which we recommend using a shaver (Torpedo, Arthrex, Naples, FL). For better orientation, it can be helpful to mark the footprints.
Eyelet wires are drilled into the footprints of the LCL and popliteus tendon. They are then overdrilled again with 5- or 6-mm drills, depending on the graft diameter. The popliteus tunnel should be about 3 cm long. The LCL tunnel must be drilled to a greater depth to ensure proper tensioning of the graft when it is pulled into the tunnel.
To prepare a shuttling suture for graft positioning, a bent clamp is inserted through a lateral stab incision, which is made directly over the femoral footprints. It is advanced through the popliteus slot, following the original path of the popliteus tendon. For this step, it is helpful to retract the eyelet wires far enough, so the clamp can be maneuvered more easily.
Now, a FiberStick (Arthrex) is inserted through the fibular tunnel and subsequently grasped with the clamp to shuttle the fiber wire to the lateral epicondyle. An additional suture may be used, which is helpful in retracting the iliotibial tract and soft tissue from the joint, which allows for the creation of more space and overview.
After tunnel preparation, the graft is first pulled into the femoral popliteus tunnel, where it is fixed with a bioabsorbable screw. We recommend using a gracilis or semitendinosus tendon with a length of at least 20 cm for the graft,. The graft is then shuttled into the joint with the prepared fiber wire and through the fibular tunnel.
After the graft has been shuttled back to the lateral epicondyle, fibular fixation is performed. For this step, the knee should be bent to about 90°. We recommend use of a nitinol wire for all fixations for an exact location of the tunnel. The correct positioning of the screw can be checked arthroscopically to avoid overtopping of the implant. Finally, the graft is fixed inside the femoral LCL tunnel with another bioabsorbable interference screw. At this point, the knee is bent to 20° to 30° of flexion.
References
- 1.LaPrade R.F., Griffith C.J., Coobs B.R., Geeslin A.G., Johansen S., Engebretsen L. Improving outcomes for posterolateral knee injuries. J Orthop Res. 2014;32:485–491. doi: 10.1002/jor.22572. [DOI] [PubMed] [Google Scholar]
- 2.Frosch K.-H., Akoto R., Heitmann M., Enderle E., Giannakos A., Preiss A. Arthroscopic reconstruction of the popliteus complex: Accuracy and reproducibility of a new surgical technique. Knee Surg Sports Traumatol Arthrosc. 2015;23:3114–3120. doi: 10.1007/s00167-014-3000-y. [DOI] [PubMed] [Google Scholar]
- 3.Thaunat M., Pioger C., Chatellard R., Conteduca J., Khaleel A., Sonnery-Cottet B. The arcuate ligament revisited: Role of the posterolateral structures in providing static stability in the knee joint. Knee Surg Sports Traumatol Arthrosc. 2014;22:2121–2127. doi: 10.1007/s00167-013-2643-4. [DOI] [PubMed] [Google Scholar]
- 4.Shon O.-J., Park J.-W., Kim B.-J. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017;29:256. doi: 10.5792/ksrr.16.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Domnick C., Frosch K.H., Raschke M.J. Kinematics of different components of the posterolateral corner of the knee in the lateral collateral ligament-intact state: A human cadaveric study. Arthroscopy. 2017;33:1821–1830. doi: 10.1016/j.arthro.2017.03.035. [DOI] [PubMed] [Google Scholar]
- 6.Rios C.G., Leger R.R., Cote M.P., Yang C., Arciero R.A. Posterolateral corner reconstruction of the knee: Evaluation of a technique with clinical outcomes and stress radiography. Am J Sports Med. 2010;38:1564–1574. doi: 10.1177/0363546510363462. [DOI] [PubMed] [Google Scholar]
- 7.Sekiya J.K., Whiddon D.R., Zehms C.T., Miller M.D. A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries: Evaluation of isolated and combined deficiency. J Bone Joint Surg Am. 2008;90:1621–1627. doi: 10.2106/JBJS.G.01365. [DOI] [PubMed] [Google Scholar]
- 8.Crespo B., James E.W., Metsavaht L., LaPrade R.F. Injuries to posterolateral corner of the knee: A comprehensive review from anatomy to surgical treatment. Rev Bras Ortop. 2015;50:363–370. doi: 10.1016/j.rboe.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hermanowicz K., Góralczyk A., Malinowski K., Jancewicz P. Arthroscopic posterolateral corner stabilization with popliteus tenodesis. Arthrosc Techn. 2018;7:e669–e674. doi: 10.1016/j.eats.2018.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stannard J.P., Brown S.L., Robinson J.T., McGwin G., Volgas D.A. Reconstruction of the posterolateral corner of the knee. Arthroscopy. 2005;21:1051–1059. doi: 10.1016/j.arthro.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Khanduja V., Somayaji H., Harnett P., Utukuri M., Dowd G. Combined reconstruction of chronic posterior cruciate ligament and posterolateral corner deficiency: A two-to nine-year follow-up study. Bone Joint J. 2006;88:1169–1172. doi: 10.1302/0301-620X.88B9.17591. [DOI] [PubMed] [Google Scholar]
- 12.Strobel M.J., Schulz M.S., Petersen W.J., Eichhorn H.J. Combined anterior cruciate ligament, posterior cruciate ligament, and posterolateral corner reconstruction with autogenous hamstring grafts in chronic instabilities. Arthroscopy. 2006;22:182–192. doi: 10.1016/j.arthro.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Wajsfisz A., Christel P., Djian P. Does combined posterior cruciate ligament and posterolateral corner reconstruction for chronic posterior and posterolateral instability restore normal knee function? Orthop Traumatol Surg Res. 2010;96:394–399. doi: 10.1016/j.otsr.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Arciero R.A. Anatomic posterolateral corner knee reconstruction. Arthroscopy. 2005;21:1147. doi: 10.1016/j.arthro.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomical posterolateral knee reconstruction: An in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 16.Frosch K.-H., Drenck T., Akoto R., Krause M., Heitmann M., Preiss A. Arthroscopic popliteal bypass graft for combined posterolateral rotational instability of the knee. Arthroskopie. 2017;30:55–59. [Google Scholar]
- 17.Krause M., Akoto R., Drenck T.C., Frosch K.H., Preiss A. Posterolateral rotatory knee instability-MRI evaluation of anatomic landmarks for tibial drill tunnel placement in open and arthroscopic popliteus tendon reconstruction. J Knee Surg. July 6 2018 doi: 10.1055/s-0038-1666832. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The posterolateral corner consists of the lateral collateral ligament (LCL) and the popliteus complex, which comprises the popliteus muscle tendon unit and the arcuate complex. The popliteus complex, especially the arcuate complex, stabilizes the knee against external rotation and, together with the posterior cruciate ligament, against posterior translation. The LCL acts as the main stabilizer against varus stress.
For surgical stabilization, anatomic reconstruction techniques, as described by Arciero14 or LaPrade et al.1, have been shown to be superior to extra-anatomic techniques. In this video, we present the all-arthroscopic reconstruction of the posterolateral corner in accordance with the technique described by Arciero.14
For this technique, 5 arthroscopic portals are required: a high anterolateral, a high anteromedial, a posteromedial, a posterolateral, and a lateral parapatellar portal.
After the posteromedial and posterolateral portals are developed, the popliteocapsular fibers are carefully resected with a shaver to visualize the popliteus tendon. It should be noted that preparation is started directly dorsal to the visible popliteus tendon, which is highlighted in the video by a green arrow.
A radiofrequency electrode can be used to prepare the fibular head. During preparation of the fibular head, it is important to stay close to the tibia to prevent injury to important popliteal structures. As demonstrated in the video, the fibular head can be identified nicely under arthroscopic vision by gently palpating it from the outside.
For preparation of the fibular tunnel, a tibial popliteus drill guide is introduced through the posterolateral portal and placed on the fibular head. After the anterior edge of the fibular head has been palpated, a small skin incision is made to position the drill guide. A guidewire is then inserted in an anterolateral-to-posteromedial direction under arthroscopic vision. It is then overdrilled with a 5- or 6-mm drill, depending on the diameter of the tendon graft. The risk of injury of the peroneal nerve can be minimized by continuous visualization of the fibular head during this step.
In the following step, the femoral tunnels are prepared. The arthroscope is placed in the anterolateral portal to visualize the lateral epicondyle, and a parapatellar portal is developed. To visualize the femoral footprints of the LCL and the popliteus tendon, the lateral joint capsule must be gently removed, for which we recommend using a shaver (Torpedo, Arthrex, Naples, FL). For better orientation, it can be helpful to mark the footprints.
Eyelet wires are drilled into the footprints of the LCL and popliteus tendon. They are then overdrilled again with 5- or 6-mm drills, depending on the graft diameter. The popliteus tunnel should be about 3 cm long. The LCL tunnel must be drilled to a greater depth to ensure proper tensioning of the graft when it is pulled into the tunnel.
To prepare a shuttling suture for graft positioning, a bent clamp is inserted through a lateral stab incision, which is made directly over the femoral footprints. It is advanced through the popliteus slot, following the original path of the popliteus tendon. For this step, it is helpful to retract the eyelet wires far enough, so the clamp can be maneuvered more easily.
Now, a FiberStick (Arthrex) is inserted through the fibular tunnel and subsequently grasped with the clamp to shuttle the fiber wire to the lateral epicondyle. An additional suture may be used, which is helpful in retracting the iliotibial tract and soft tissue from the joint, which allows for the creation of more space and overview.
After tunnel preparation, the graft is first pulled into the femoral popliteus tunnel, where it is fixed with a bioabsorbable screw. We recommend using a gracilis or semitendinosus tendon with a length of at least 20 cm for the graft,. The graft is then shuttled into the joint with the prepared fiber wire and through the fibular tunnel.
After the graft has been shuttled back to the lateral epicondyle, fibular fixation is performed. For this step, the knee should be bent to about 90°. We recommend use of a nitinol wire for all fixations for an exact location of the tunnel. The correct positioning of the screw can be checked arthroscopically to avoid overtopping of the implant. Finally, the graft is fixed inside the femoral LCL tunnel with another bioabsorbable interference screw. At this point, the knee is bent to 20° to 30° of flexion.