Abstract
BACKGROUND AND OBJECTIVES:
Student-Run Free Clinics (SRFCs) play a significant role in medical education yet there is minimal information about patient outcomes over time in this setting. The purpose of this study was to assess longitudinal outcomes of hypertension management during routine care at four SRFC sites, while comparing control rates with national standards, and examining for characteristics independently associated with uncontrolled hypertension.
METHODS:
The authors conducted a retrospective medical record review of visits from January 2004 through April 2016 with an initial visit for hypertension and a follow-up visit 9 to 15 months later. Hypertension control was analyzed using descriptive statistics, paired t tests, logistic regression, and a longitudinal linear mixedeffects model.
RESULTS:
This study included 496 patients and 4,798 visits. The mean age was 50.9 (SD 10.8) years old, 71.2% (346) were Latinos, 63.3% (314) were Spanish speaking, and 15.5% (72) were homeless. Mean blood pressure was reduced from 141.6 (SD 21.8)/85.1 (SD 13.2) to 132.1 (SD 17.3)/79.4 (SD10.8), a decrease of 9.5 (CI 7.4, 11.5)/5.7 (CI 4.4, 7.0) mmHg. Blood pressure was significantly reduced within the first month of treatment, and this reduction was sustained throughout the follow-up period. Using the National Health and Nutrition Examination Survey (NHANES) definition (<140/<90), blood pressure was controlled in 59.7% (296/496) of patients. No significant differences in control were noted based on gender, ethnicity, language, housing status, or clinic site.
CONCLUSIONS:
SRFCs can provide effective long-term hypertension management and achieve rates of control that exceed national averages despite serving those least likely to be controlled.
Cardiovascular disease is the leading cause of death in the United States, and hypertension is the most significant modifiable risk factor for this disease.1 Hypertension affects approximately one third of the adult population in the United States, or 80 million people.1–3 It is estimated that 46,000 deaths could be prevented each year if hypertension was adequately treated.3 However, National Health and Nutrition Examination Survey (NHANES) data demonstrated that over half (53.5%) of hypertensive patients had uncontrolled blood pressure.4 Those with the lowest rates of blood pressure control nationally include Mexican-Americans (36.9%), the uninsured (29.0%), and those without a usual source of care (12.1%).5
Over 75% of Association of American Medical Colleges (AAMC) institutions now have Student-Run Free Clinics (SRFCs).6 The AAMC Graduation Questionnaire demonstrates that free clinics are a core part of medical education, as each year over 70% of fourth-year medical students have been involved in a free clinic for the underserved.7 The University of California, San Diego (UCSD) School of Medicine Student-Run Free Clinic Project (SRFCP) has been previously described in the literature and now operates at four clinical sites.8–12
Hypertension is one of the most common medical conditions treated at SRFCs.6 Two SRFCs have published data documenting that their rates of control were comparable to national standards.13,14 Based on data from long-term clinical trials and cohort studies, the full effect of blood pressure reduction is achieved within one year.15 Therefore, we aimed to assess blood pressure control in our patient population after approximately 1 year of treatment in our setting.
The purpose of this study was to assess longitudinal outcomes of hypertension management during routine care at four SRFC sites, while comparing blood pressure control rates with national standards and examining for characteristics independently associated with uncontrolled hypertension within this patient population.
Methods
Data Collection
This was a retrospective medical record review of clinic visits from January 2004 through April 2016. A Microsoft Access (Redmond, WA) database and EPIC (Verona, WI) Electronic Health Records were used to record patient demographics, diagnoses, and vitals signs. We queried this database for new patients 18 years of age and over with a diagnosis of hypertension and at least one followup visit between 9 and 15 months from the initial visit for inclusion in this study.
Outcomes
Baseline blood pressure measurements were recorded at the initial visit for hypertension. The blood pressure recorded at the visit closest to 1 year from the initial diagnostic visit was considered the outcome blood pressure. To allow for usual variation in clinical practice, we included visits up to 3 months before or after the 1-year time frame in this study (9 to 15 months). We defined a dichotomous blood pressure control variable as controlled or uncontrolled, with control defined as the systolic blood pressure (SBP) <140 mm Hg and the diastolic blood pressure (DBP) <90 mm Hg. This allows our data to be compared to national datasets as NHANES classifies SBP of <140 mm Hg and DBP <90 mm Hg as controlled based on an average of up to three blood pressure readings during a single examination at a mobile examination center.4 The study timeframe overlaps with two blood pressure guidelines, The Seventh16 and Eighth17 Report and of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7: 2003–2013) and (JNC 8: 2014–present). Both guidelines are consistent with NHANES as they also set blood pressure goals as <140/<90. However, JNC 8 now allows for a more lenient blood pressure goal of <150/<90 for people over 60 years of age. To allow for comparisons with national data sets, the more lenient blood pressure goal for individuals over 60 years of age was not considered in this study. NHANES and JNC8 do not include a lower blood pressure goal for diabetic patients.
Statistical Analysis
Participant demographics were summarized overall and for each of the four enrollment sites using numbers and percentage for categorical variables (age, gender, ethnicity, housing status, primary language, and diabetes status) and mean and standard deviation for continuous variables (age). Ethnicities considered include Hispanic, White, Black, Asian, and Other. Primary language included English, Spanish, and other language. Housing status was dichotomized into two variables, housed and homeless. The comparison between sites used Fisher’s exact test for categorical variables and F-test for continuous variables. The baseline and 12-month follow-up values for SBP and DBP were summarized using mean and standard deviation, overall, by diabetes status, and by enrollment site. The changes from baseline to 12-months in SBP and DBP used the paired t test. Hypertension control (defined as SBP <140 and DBP <90 at 12 months) was reported using numbers and percentages, overall and by site and demographic covariates (age, gender, ethnicity, housing status, primary language, and diabetes status). Unadjusted odds ratios and 95% confidence intervals were computed using single-predictor logistic regression models. The P value of the association of each of these factors with hypertension control at 12 months used Fisher’s exact test for categorical predictors and the likelihood ratio test of logistic regression for continuous predictors (baseline SBP and DBP). An adjusted analysis used multiple logistic regression, with the final model chosen based on the Akaike information criterion (AIC), which emphasizes accurate prediction of the outcome (hypertension control). The P values of the adjusted analysis used the likelihood ratio of the multiple logistic regression. The longitudinal blood pressure reduction in 1-month intervals over 12 months was evaluated using a linear mixed-effects model with a random subject effect. All P values were two-tailed with a .05 significance threshold. Statistical analyses were performed using the R statistical language.18 The Institutional Review Board at UCSD approved this study.
Results
Study Population
Demographics of the study population are summarized in Table 1. Overall, including all four sites, the mean age was 50.8 years (SD=10.8), and the study population included a significant percentage of underserved minorities including Hispanics (71.2%), Spanish speakers (63.3%), and homeless patients (15.5%).
Table 1:
Demographics of Hypertensive Study Participants at Four University of California San Diego Student-Run Free Clinic Project Sites From January 2004 Through April 2016
| Characteristic | All | Downtown | Pacific Beach |
Mountain View |
Lemon Grove |
P Value |
|---|---|---|---|---|---|---|
| Number of subjects | 496 | 210 | 149 | 123 | 14 | |
| Age, n (%) | .47 | |||||
| 18–39 | 75 (15.1) | 28 (13.3) | 21 (14.1) | 23 (18.7) | 3 (21.4) | |
| 40–59 | 320 (64.5) | 136 (64.8) | 102 (68.5) | 72 (58.5) | 10 (71.4) | |
| 60+ | 101 (20.4) | 46 (21.9) | 26 (17.4) | 28 (22.8) | 1 (7.1) | |
| Age, mean (SD) | 50.9 (10.8) | 51.5 (10.8) | 50.0 (10.3) | 51.6 (11.8) | 46.4 (7.7) | |
| Gender, n (%) | <.0001 | |||||
| Female | 294 (59.3) | 128 (61) | 68 (45.6) | 89 (72.4) | 9 (64.3) | |
| Male | 202 (40.7) | 82 (39) | 81 (54.4) | 34 (27.6) | 5 (35.7) | |
| Ethnicity, n (%) | <.0001 | |||||
| White | 92 (18.9) | 46 (22.1) | 45 (31.2) | 1 (0.8) | 0 (0) | |
| Hispanic | 346 (71.2) | 134 (64.4) | 85 (59) | 113 (94.2) | 14 (100) | |
| Black | 15 (3.1) | 7 (3.4) | 3 (2.1) | 5 (4.2) | 0 (0) | |
| Asian | 21 (4.3) | 14 (6.7) | 6 (4.2) | 1 (0.8) | 0 (0) | |
| Other | 12 (2.5) | 7 (3.4) | 5 (3.5) | 0 (0) | 0 (0) | |
| Housing status, n (%) | <.0001 | |||||
| Housed | 392 (84.5) | 167 (85.2) | 103 (72.5) | 109 (96.5) | 13 (100) | |
| Homeless | 72 (15.5) | 29 (14.8) | 39 (27.5) | 4 (3.5) | 0 (0) | |
| Primary language, n (%) | <.0001 | |||||
| English | 159 (32.1) | 78 (37.1) | 69 (46.3) | 11 (8.9) | 1 (7.1) | |
| Other | 23 (4.6) | 11 (5.2) | 6 (4) | 4 (3.3) | 2 (14.3) | |
| Spanish | 314 (63.3) | 121 (57.6) | 74 (49.7) | 108 (87.8) | 11 (78.6) | |
| Diabetes, n (%) | .0013 | |||||
| No | 169 (34.1) | 69 (32.9) | 62 (41.6) | 29 (23.6) | 9 (64.3) | |
| Yes | 327 (65.9) | 141 (67.1) | 87 (58.4) | 94 (76.4) | 5 (35.7) |
Demographic information is queried from a database populated by information on initial intake forms filled out by patients. If a patient leaves a section blank on their initial intake form, no information is recorded in the database for that demographic variable.
Diagnoses, including diabetes, are recorded in the database and Electronic Health Record by health care providers including medical students and faculty physicians at each visit.
Blood Pressure Results
A total of 4,798 visits for hypertension were included in this study. Mean blood pressure from the initial visit was 141.6 mm Hg (SD=21.8) systolic and 85.1 mm Hg (SD=13.2) diastolic (Table 2). Overall, the mean outcome blood pressure measurement was 132.1mm Hg (SD=17.3) systolic and 79.4 mm Hg (SD=10.8) diastolic, a reduction of 9.5 mmHg (CI 7.4, 11.5) and 5.7 mmHg (CI 4.4, 7.0) respectively (P<.0001 for both). The SBP rate of control was 66.9% (332/496), and the DBP rate of control was 78.2% (388/496). The overall percentage of patients who met both the SBP goal of <140 and DBP goal of <90 was 59.7% (296/496). The percent of patients reaching blood pressure control by age, gender, ethnicity, primary language, and homeless status are listed in Table 3. We found no significant differences in hypertension control by clinic site (P=.14), housing status (P=.70), gender (P=.85), ethnicity (P=.70), or primary language (P=.17) (Table 3). However, patients 60 years of age and older were less likely to have reached their blood pressure goal (54/101; 53.5%) than those aged 18–39 (52/75; 69.3%) or 40–59 (190/320; 59.4%) (P=.033). SBP and DBP decreased on average by 6.1(CI 4.4–7.8) mmHg and 3.2 (CI 2.1–4.2) mmHg within the first month and stayed significantly lower than baseline throughout the 12-month follow up period (P<.0001) (Figure 1).
Table 2:
Mean Baseline Blood Pressure (in mm Hg) Compared With Outcome Blood Pressure in Hypertensive Patients. Four University of California San Diego Student-Run Free Clinic Project Sites From January 2004 Through April 2016, n=496
| Systolic Blood Pressure | Diastolic Blood Pressure | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) |
Follow-Up Mean (SD) |
Change Mean (95% CI) |
P Value | Baseline Mean (SD) |
Follow-up Mean (SD) |
Change Mean (95% CI) |
P Value | |
| All Participants | 141.6(21.8) | 132.1(17.3) | 9.5(7.4, 11.5) | <.0001 | 85.1(13.2) | 79.4(10.8) | 5.7(4.4, 7.0) | <.0001 |
| Diabetes | ||||||||
| No | 143.0(21.5) | 133.1(15.6) | 9.9(6.5, 13.4) | <.0001 | 86.5(13.5) | 82.3(10.4) | 4.3(2.2, 6.4) | .0001 |
| Yes | 140.8(21.9) | 131.6(18.2) | 9.2(6.7, 11.8) | <.0001 | 84.4(12.9) | 78.0(10.7) | 6.4(4.9, 8.0) | <.0001 |
| Site | ||||||||
| Mountain View | 136.6(21.7) | 127.7(19.9) | 8.9(4.1, 13.6) | .0003 | 81.0(13.1) | 76.3(10.4) | 4.7(2.1, 7.3) | .0005 |
| Downtown | 143.1(23.2) | 133.3(17.2) | 9.7(6.6, 12.9) | <.0001 | 86.0(13.5) | 79.8(11.1) | 6.2(4.2, 8.2) | <.0001 |
| Lemon Grove | 137.9(15.5) | 134.1(11.0) | 3.8(−5.8, 13.3) | .41 | 88.2(12.2) | 84.1(9.1) | 4.1(−4.1, 16.1) | .33 |
| Pacific Beach | 143.8(19.6) | 133.7(15.0) | 10.1(6.8, 13.4) | <.0001 | 87.1(11.8) | 81.1(10.4) | 6.0(3.8, 8.1) | <.0001 |
Table 3:
Predictors of Hypertension Control (Systolic Blood Pressure <140 and Diastolic Blood Pressure <90) at Outcome in Hypertensive Patients and Characteristics Associated With Hypertension Control: Unadjusted and Adjusted Analyses. Adjusted Analyses Uses the Akaike Information Criterion. Four University of California San Diego Student-Run Free Clinic Project Sites From January 2004 Through April 2016, n=496
| Hypertension Control |
Unadjusted Analysis |
Adjusted Analysis |
|||
|---|---|---|---|---|---|
| Participant Characteristic | All, n/N (%) | P Value | Unadjusted OR | Adjusted OR | P Value |
| Overall | 296/496 (59.7) | ||||
| Baseline SBP (per mm Hg) |
0.97 (0.96, 0.98) | 0.81 (0.71, 0.91) | .0008 | ||
| Baseline DBP (per mm Hg) |
0.96 (0.94, 0.97) | 0.84 (0.68, 1.02) | .083 | ||
| Age | .033 | ||||
| 18–39 | 52/75 (69.3) | 1 | |||
| 40–59 | 190/320 (59.4) | 0.65 (0.37, 1.10) | |||
| 60+ | 54/101 (53.5) | 0.51 (0.27, 0.95) | |||
| Gender | .85 | ||||
| Female | 174/294 (59.2) | 1 | |||
| Male | 122/202 (60.4) | 1.05 (0.73, 1.52) | |||
| Ethnicity | .70 | ||||
| White | 50/92 (54.3) | 1 | |||
| Hispanic | 211/346 (61) | 1.31 (0.82, 2.09) | |||
| Black | 8/15 (53.3) | 0.96 (0.32, 2.95) | |||
| Asian | 13/21 (61.9) | 1.36 (0.52, 3.74) | |||
| Other | 6/12 (50) | 0.84 (0.25, 2.87) | |||
| Site | .14 | ||||
| Mountain View | 120/210 (57.1) | 1.62 (1.02, 2.59) | |||
| Downtown | 7/14 (50) | 1 | |||
| GA | 84/123 (68.3) | 0.75 (0.25, 2.26) | |||
| Pacific Beach | 85/149 (57) | 1.00 (0.65, 1.52) | |||
| Housing status | .70 | ||||
| Housed | 233/392 (59.4) | 1 | |||
| Homeless | 45/72 (62.5) | 1.14 (0.68, 1.93) | |||
| Primary language | .17 | ||||
| English | 86/159 (54.1) | 1 | |||
| Other | 16/23 (69.6) | 1.37 (0.93, 2.02) | |||
| Spanish | 194/314 (61.8) | 1.94 (0.78, 5.28) | |||
| Diabetes | .15 | ||||
| No | 93/169 (55) | 1 | |||
| Yes | 203/327 (62.1) | 1.34 (0.92, 1.95) | |||
Age groups compared to patients 18–39 years old.
Spanish and “Other” speakers compared to English speakers.
Ethnic groups compared to Caucasian reference group.
Figure 1:
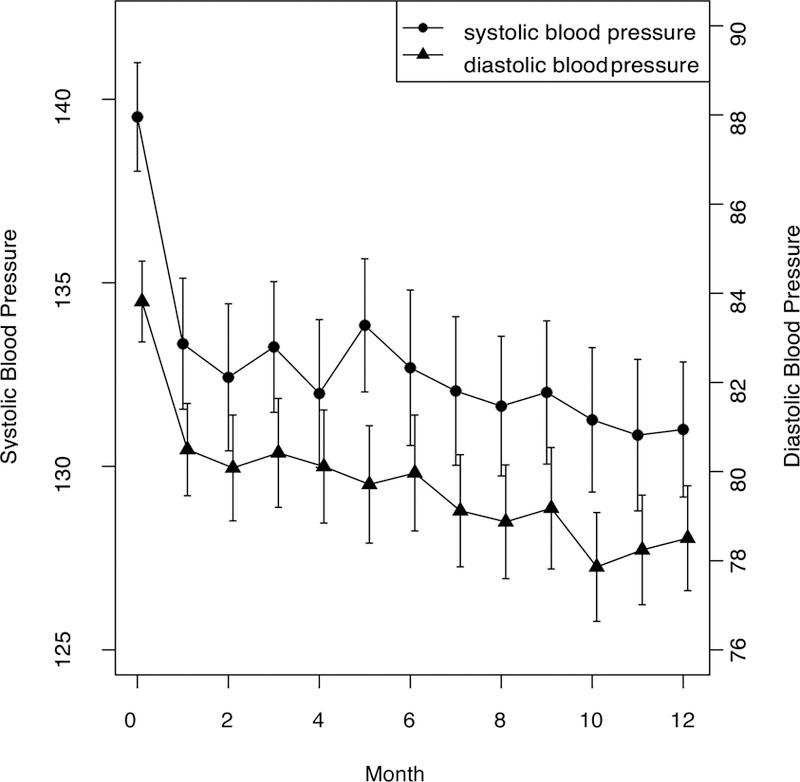
Mean Systolic and Diastolic Blood Pressure Change in Hypertensive Patients, Recorded in Monthly Intervals From Baseline, With 95% Confidence Intervals. University of California San Diego Student-Run Free Clinic Project From January 2004 Through April 2016, n=496
Discussion
Patients with hypertension receiving treatment at four sites of the UCSD SRFCP had a significant reduction in SBP and DBP over time. In addition to these reductions reaching statistical significance (P<.0001), they also have clinical significance. In the largest meta-analysis of randomized trials of blood pressure analysis to date (147 trials), lowering blood pressure by 10 mm Hg systolic and 5 mm Hg diastolic was found to reduce cardiac events by one-quarter and stroke by a third.15 Our patients had a similar size decrease of 9.5 mm Hg SBP and 5.7 mm Hg DBP, therefore it is reasonable to expect a similar decrease in cardiac events and stroke as a result of the treatment patients received at the SR-FCs. There is a positive, continuous, independent association of lowering blood pressure with coronary heart disease and stroke, even in those with mild hypertension.19,20 The benefit of blood pressure control may be even more than blood glucose control in diabetic patients.21–23 The UK Prospective Studies Diabetes Group demonstrated that by lowering the blood pressure by 10 mm Hg/5 mm Hg for 10 years, the number needed to treat (NNT) to prevent one death was 15.21
In addition to reducing the mean SBP and DBP over time, overall rates of blood pressure control in our SRFC patient population compared favorably with national data sets. NHANES reported the rate of blood pressure control as 45.8% overall, 36.9% in Mexican-Americans, and 29.0% in uninsured patients.5 The overall rate of control in our multisite SRFC study using the same definition was 59.7% (296/496) and 61.0 % (211/346) in Latinos. Our results suggest that SRFCs can meet or exceed national averages for blood pressure control and that SRFCs can provide effective chronic disease management for hypertensive patients over time.
SRFCs provide quality care in resource limited settings despite serving patients whose demographics reflect those who are the least likely to be controlled nationally. At the UCSD SRFCP sites, some explanations for this may include that although our patients are uninsured, we provide them with medical consultations, laboratory services, and provide medication on-site, same-day, free of charge. Employed and volunteer faculty attending physicians who have been chosen for their dedication to student education, excellence in clinical care, and humanism in medicine provide continuity of care. Despite the preconceived notion that SRFCs provide walk-in or acute care to a transient population, over 90% of our visits are follow-up visits. Our clinic sites are based in the community where these populations are likely to return, including churches who serve meals to the homeless and local public elementary schools.
Using NHANES criteria, patients 60 years of age and older met blood pressure goals at a lower rate than younger patients. However, using the newer JNC8 guidelines, released during the latter part of this study time frame, patients 60 years of age or older now have a more lenient blood pressure goal of <150/<90. It is likely that this change would eliminate the age-based disparity in blood pressure control noted in our setting.
While the blood pressure control documented in this study exceeds national standards, there is still room for improvement as approximately 40% of patients remain uncontrolled. Medical students are, by definition, in charge of the day-today administration of SRFCs.24,25 As health care moves toward more population-based management and routinely assessing quality assurance, it seems prudent and timely for SRFCs to regularly assess their quality of care, particularly for chronic disease management.24
This study has several limitations. First, it is a retrospective medical record review. Prospective studies could be considered, particularly to assess the outcomes from targeted interventions to improve hypertension control. Second, all clinic sites are affiliated with a single institution in San Diego, CA. However, this study included patients from four clinic sites, each in a different area of the city. Third, we assessed control of patients after 1 year of treatment, biasing the data toward patients with compliance and follow up. However, additional analysis for patients with any follow-up visit between 30 days to 5 years after their baseline revealed similar results that were consistent with these findings (data not shown). Finally, blood pressure measurements were taken with a manual sphygmomanometer, which may result in some level of reporter bias. Further areas of inquiry include prospective multi-institutional studies of chronic disease management at SRFCs.
Conclusions
This study adds to the growing body of literature suggesting that SRFCs are providing not only a service-learning opportunity for their students but also quality medical care that meets or exceeds national standards.
ACKNOWLEDGMENTS:
The authors would like to thank the dedicated students, staff, and volunteers of the UCSD SRFCP, including Carol Eames for querying this data, Michelle Johnson, MD, and Natalie Rodriguez, MD, for their outstanding ongoing clinical care, mentoring, and role modeling at the UCSD SRFCP, and Ellen Beck, MD, for creating and sustaining this project for 20 years.
Previous versions of data regarding hypertension control at the UCSD SRFCP were presented at the 2012 Society of Teachers of Family Medicine (STFM) Conference on Medical Student Education in Long Beach, CA, and at the 2013 STFM Conference on Medical Student Education in San Antonio, TX.
Ethical approval: The University of California, San Diego Institutional Review Board approved this project # 101845X.
Dr Steven Rojas was a medical student at UC San Diego School of Medicine when this project began.
Contributor Information
Sunny D. Smith, Department of Family Medicine and Public Health, University of California San Diego.
Steven M. Rojas, Family Health Center of San Diego.
Junwen Huang, Department of Mathematics.
Kuangyi Yang, Department of Mathematics.
Florin Vaida, Department of Family Medicine and Public Health.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation 2015. January;131:e29–e322. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PB, Trogdon JG, Khajou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011. March;123:933–4. [DOI] [PubMed] [Google Scholar]
- 3.Farley TA, Dalal MA, Mostashari F, et al. Deaths preventable in the US by improvements in use of clinical preventive services. Am J Prev Med 2010. June;38(6):600–9. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC). Vital signs: awareness and treatment of uncontrolled hypertension among adults— United States, 2003–2010. MMWR Morb Mortal Wkly Rep 2012. September;61:703–9. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Vital signs: prevalence, treatment, and control of hypertension—United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep 2011. February;60:103–8. [PubMed] [Google Scholar]
- 6.Smith S, Thomas R 3rd, Cruz M, et al. Presence and characteristics of student-run free clinics in medical schools. JAMA 2014. December;321:2407–10. [DOI] [PubMed] [Google Scholar]
- 7.Association of American Medical Colleges. Medical School Graduation Questionnaire 2015 All Schools Summary Report Washington, DC: Association of American Medical Colleges, 2015. https://www.aamc.org/download/440552/data/2015gqallschoolssummaryreport.pdf. Accessed May 2, 2016. [Google Scholar]
- 8.Smith SD, Yoon R, Johnson ML, et al. Effect of involvement in a student-run free clinic project on attitudes toward the underserved and interest in primary care. J Health Care Poor Underserved 2014. May;25:877–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rojas S, Smith SD, Rojas S, et al. Longitudinal hyperlipidemia outcomes at three student-run free clinic sites. Fam Med 2015;47:309–14. [PMC free article] [PubMed] [Google Scholar]
- 10.Soltani M, Smith S, Beck E, et al. Universal depression screening, diagnosis, management, and outcomes at a student-run free clinic. Acad Psychiatry 2015;39:259–66. [DOI] [PubMed] [Google Scholar]
- 11.Smith SD, Johnson ML, Rodriguez N, et al. Medical student perceptions of the educational value of a student-run free clinic. Fam Med 2012;44:646–9. [PubMed] [Google Scholar]
- 12.Zucker J, Gillen J, Ackrivo J, et al. Hypertension management in a student-run free clinic: meeting national standards? Acad Med 2011. February;86:239–45. [DOI] [PubMed] [Google Scholar]
- 13.Taylor J, Thomas D, Torhneim M, et al. Hypertension outcomes at a student-run clinic for the uninsured. Journal of Student-run Clinics 2015. June;1:1–9. [Google Scholar]
- 14.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. Br Med J 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003. May;289:2560–72. [DOI] [PubMed] [Google Scholar]
- 16.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC8). JAMA 2014. February;311(5):507–20. [DOI] [PubMed] [Google Scholar]
- 17.R Core Team. R: a language and environment for statistical computing R Foundation for Statistical Computing; (http://www.R-project.org), Austria, Vienna, 2014. [Google Scholar]
- 18.MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease, part 1: prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990;335:765–74. [DOI] [PubMed] [Google Scholar]
- 19.Edmin CA, Rahimi K, Neal B, et al. Blood pressure lowering in Type 2 diabetes: a systematic review and meta-analysis. JAMA 2015;313:603–15. [DOI] [PubMed] [Google Scholar]
- 20.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 21.UK Prospective Diabetes Study Group. Intensive blood glucose control with sulfonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352: 837–53. [PubMed] [Google Scholar]
- 22.Ogden LG, He J, Lydick E, Whelton PK. Long-term absolute benefit of lowering blood pressure in hypertensive patients according to JNC VI risk stratification. Hypertension 2000;35:539–43. [DOI] [PubMed] [Google Scholar]
- 23.Meah YS, Smith EL, Thomas DC. Student-run health clinic: novel arena to educate medical students on systems-based practice. Mt Sinai J Med 2009;76:344–56. [DOI] [PubMed] [Google Scholar]


