Abstract
Objective
Our aim was to assess the impact of comorbidities on existing COPD prognosis scores.
Patients and methods
A total of 543 patients with COPD (FEV1 <80% and FEV1/FVC <70%) were included between January 2003 and January 2004. Patients were stable for at least 6 weeks before inclusion and were followed for 5 years without any intervention by the research team. Comorbidities and causes of death were established from medical reports or information from primary care medical records. The GOLD system and the body mass index, obstruction, dyspnea and exercise (BODE) index were used for COPD classification. Patients were also classified into four clusters depending on the respiratory disease and comorbidities. Cluster analysis was performed by combining multiple correspondence analyses and automatic classification. Receiver operating characteristic curves and the area under the curve (AUC) were calculated for each model, and the DeLong test was used to evaluate differences between AUCs. Improvement in prediction ability was analyzed by the DeLong test, category-free net reclassification improvement and the integrated discrimination index.
Results
Among the 543 patients enrolled, 521 (96%) were male, with a mean age of 68 years, mean body mass index 28.3 and mean FEV1% 55%. A total of 167 patients died during the study follow-up. Comorbidities were prevalent in our cohort, with a mean Charlson index of 2.4. The most prevalent comorbidities were hypertension, diabetes mellitus and cardiovascular diseases. On comparing the BODE index, GOLDABCD, GOLD2017 and cluster analysis for predicting mortality, cluster system was found to be superior compared with GOLD2017 (0.654 vs 0.722, P=0.006), without significant differences between other classification models. When cardiovascular comorbidities and chronic renal failure were added to the existing scores, their prognostic capacity was statistically superior (P<0.001).
Conclusion
Comorbidities should be taken into account in COPD management scores due to their prevalence and impact on mortality.
Keywords: comorbidities, COPD, mortality, GOLD, cluster analysis, BODE index
Introduction
For many years, COPD has been categorized using the FEV1.1,2 However, because of the complexity, heterogeneity and multicomponent aspect of the disease, different indices and scores have been developed in recent years in an attempt to include different COPD outcomes such as mortality and hospitalization. Nevertheless, determining which variables should be included in these scores, or how these indices should be developed, has not yet been completely established.
In 2004, Celli et al developed a multidimensional index, the body mass index, obstruction, dyspnea and exercise (BODE) index,3 using four factors that predicted the risk of death: body mass index (BMI),4 airflow obstruction, dyspnea5 and exercise. This score has been extensively validated for predicting mortality, and has also shown an ability to predict hospitalization,6 response to lung volume reduction surgery7 and pulmonary rehabilitation.8
Some years later, in 2011, the Global Strategy for Diagnosis, Management and Prevention of COPD (GOLD)FEV1 system was modified by including exacerbations and symptoms in the GOLDABCD classification.2,9 Even though it was not designed to predict outcomes, GOLDABCD was found to be superior for predicting exacerbations and hospitalizations, with no differences in mortality compared with GOLD 2007, based on FEV1 alone.10–12 A new update of the GOLDABCD classification has recently been proposed. In GOLD2017, spirometry is required for the diagnosis, prognosis and disease progression, but is no longer included in the ABCD tool, which is now centered exclusively on symptoms and exacerbations.13
Another way to classify COPD patients is to create homogeneous groups considering multiple disease-related variables in a clustering analysis.14 Garcia-Aymerich et al identified three COPD phenotypes based on the respiratory and systemic components,15 and similar results were reported by Burgel et al.16 The first two clusters were predominantly based on the respiratory disease, while the latter had more systemic inflammation and comorbidities. Esteban et al had comparable outcomes, classifying COPD into four different clusters, with no differences found after 1 year of follow-up. Clusters were heavily impacted by comorbidities.17
Comorbidities are a major cause of death and hospitalization in COPD patients.18 The GOLDFEV1 executive summary in 2007 and its update in 2016 acknowledged the importance of comorbidities in all COPD stages, with a significant impact on prognosis, recommending that comorbidities be actively sought and treated, if present. However, they have not been included in COPD management in the GOLDABCD classification.19 Different indices have been proposed based on comorbidities in order to improve the prediction of mortality, namely, the COTE index (COPD specific comorbidity test) developed by Divo et al and the CODEX index (comorbidity, obstruction, dyspnea and previous severe exacerbations) developed by Almagro et al.20–22
Taking this into account, the aim of our study was to evaluate the impact of comorbidities on the GOLDABCD classification, GOLD2017, the BODE index and cluster-based subtypes for predicting mortality.
Patients and methods
Participants and data collection
Individuals were recruited when being treated for COPD between January 2003 and January 2004 at one of five outpatient respiratory clinics run by the Respiratory Service of Galdakao-Usansolo Hospital. Patients were consecutively included in the study if they had been diagnosed with COPD for at least 6 months and had been stable for 6 weeks before enrollment. Other inclusion criteria were FEV1 <80% of the predicted value and FEV1/FVC <70%. Patients diagnosed with asthma, extensive pulmonary tuberculosis or cancer, or who suffered from psychiatric or neurological problems that might prevent effective collaboration were not eligible. The protocol was approved by the Institutional Research Committee of OSI Galdakao-Barrualde (ethics approval number: 03/09062005) and according to the 1964 Helsinki declaration and its later amendments. All eligible patients were given detailed information about the study, and all those included provided written informed consent.
Study protocol
Sociodemographic and lifestyle variables were recorded. The level of dyspnea was established using the mMRC scale.23 Comorbidities were determined by reviewing patients’ medical records and were summarized in the Charlson comorbidity index.24 Health-related quality of life was assessed using the Spanish validated version of the St George’s Respiratory Questionnaire (SGRQ).25,26 Data on the level of physical activity, complete pulmonary function tests, muscle strength and 6-minute walk test (6MWT) were collected as defined in detail elsewhere, always following the Spanish Society of Respiratory Medicine and Thoracic Surgery guidelines and using well-established thresholds for theoretical values.27–29
The outcome variable was defined as all-cause mortality during the 5 years of follow-up.
Follow-up
Patients were followed up for 5 years after recruitment. No interventions were performed related to this study, and the research team did not take part in the patients’ routine treatment or the treatment of any exacerbations.
During this 5-year follow-up period, patient medical records and the hospital admissions database were reviewed. Vital status was established by reviewing the medical records and examining the hospital database and public death registries. Deaths were considered confirmed if the name, sex and date of birth on the record matched with those of the participant.
Statistical analyses
Variables were described using mean and SDs for continuous variables and the number of cases and percentages for categorical variables. Comparisons between groups were performed with the chi-squared test for categorical variables and the t-test for continuous variables. Fisher’s exact test and non-parametric Wilcoxon and Kruskal–Wallis tests were used when necessary and indicated in the text.
Cluster classification was performed by combining multiple correspondence analyses and automatic classification as explained in detail elsewhere.30 Patients were classified according to the GOLD criteria and the BODE index.3,9,13 The BODE index was classified into four categories as suggested by Celli et al for comparability purposes.3
Simple logistic regression was performed with 5-year mortality as the outcome and cluster classification, GOLD criteria and the BODE index as independent predictive variables. Multiple logistic regression was performed for each prediction rule (cluster, GOLD and BODE), adding the statistically significant comorbidities as predictors into the model. Alternatively, multiple logistic regression was performed for each prediction rule (cluster, GOLD and BODE), adding the Charlson comorbidity index as a predictor into the model. For each model, a receiver operating characteristic (ROC) curve, area under the curve (AUC) and the 95% CI of the AUC were calculated in order to measure discriminative ability. Goodness-of-fit was performed with the Hosmer–Lemeshow test. DeLong test was used to evaluate differences between AUCs. Improvement in prediction ability when comorbidities were included was measured by the category-free net reclassification improvement (NRI) and the integrated discrimination improvement (IDI), including 95% CIs. Statistical significance was stated at α=0.05. All statistical analyses were performed using R v2.13.0., including pROC and PredictABEL libraries.30–32
Ethics approval and informed consent
The protocol was approved by the Ethics and Research committees of Hospital Galdakao-Usansolo (03/09062005). All eligible patients were given detailed information about the study, and all those included provided written informed consent.
Results
A total of 543 patients were enrolled, of whom 96% were male, with the mean age being 68.3 (SD ±8.3) years, mean BMI 28.3 (SD ±4.4) kg/m2 and mean mMRC dyspnea score 2.4 (SD ±0.9). Mean post-bronchodilator FEV1% was 55% (SD ±13.3) of the predicted value and mean 6-minute walk distance was 408.9 m (SD ±92.4).
During the 5 years of follow-up, 167 patients died. The group that died was older, with worse FEV1%, dyspnea and 6MWT, more previous hospitalizations and worse SGRQ score. In relation to comorbidities, there was nearly 1 point of difference between groups in the Charlson index, with more comorbidities in the group of patients who died. Hypertension, diabetes mellitus and cardiovascular diseases (coronary artery disease, arrhythmia and valvular heart disease) were the most prevalent comorbidities in this group (Table 1).
Table 1.
General characteristics of the cohort at baseline by mortality
| Characteristics | Total (N=543) | Mortality
|
P-value | |
|---|---|---|---|---|
| Yes (n=167) | No (n=376) | |||
|
| ||||
| Gender (male) | 522 (96.1) | 165 (98.9) | 357 (94.9) | 0.032 |
|
| ||||
| Age (years): | 68.3 (8.3) | 72.3 (6.4) | 66.6 (8.5) | <0.001 |
|
| ||||
| BMI (kg/m): | 28.3 (4.4) | 27.9 (4.6) | 28.4 (4.4) | 0.252 |
|
| ||||
| Dyspnea (mMRC): | 24 (0.9) | 1.37 (1.0) | 2.2 (0.8) | <0.001 |
| 1 | 69 (12.7) | 13 (7.8) | 56 (14.9) | |
| 2 | 264 (48.6) | 60 (37.7) | 201 (53.5) | |
| 3 | 166 (30.6) | 60 (35.9) | 106 (28.2) | |
| 4–5 | 44 (8.1) | 31 (18.6) | 13 (3.5) | |
|
| ||||
| FEV1 (mL): | 1,464 (441.3) | 1,248 (368) | 1,560 (438) | <0.001 |
|
| ||||
| FEV1%: | 55.0 (13.3) | 50.1 (13.7) | 57.2 (12.6) | <0.001 |
|
| ||||
| Smoking status | ||||
| Current smoker | 114 (21.0) | 24 (14.4) | 90 (23.9) | 0.02 |
| Former smoker | 414 (76.2) | 140 (83.8) | 274 (72.9) | |
| No smoker | 15 (2.8) | 3 (1.8) | 12 (3.2) | |
|
| ||||
| Packs/year: | 46.8 (27.3) | 49.2 (27.5) | 45.8 (27.2) | 0.175 |
|
| ||||
| 6-minute walking test (m): | 408.9 (92.4) | 353.7 (99.8) | 433.4 (77.3) | <0.001 |
|
| ||||
| Hospital admission for COPD in the 2 previous years | ||||
| 0 | 402 (74.0) | 97 (58.1) | 305 (81.1) | <0.001 |
| 1 | 87 (16.0) | 40 (24.0) | 47 (12.5) | |
| ≥2 | 54 (10.0) | 30 (18.0) | 24 (6.4) | |
|
| ||||
| Charlson comorbidity index: | 2.4 (1.4) | 3.0 (1.7) | 2.1 (1.2) | <0.001 |
| 0–1 | 172 (31.7) | 33 (19.8) | 139 (37.0) | |
| 2–3 | 264 (48.6) | 77 (46.1) | 187 (49.7) | |
| >3 | 107 (19.7) | 57 (34.1) | 50 (13.3) | |
|
| ||||
| SGRQ (total): | 39.2 (20.1) | 43.5 (19.6) | 37.3 (20.0) | <0.001 |
|
| ||||
| Coronary artery disease | 32 (5.9) | 18 (10.8) | 14 (3.7) | 0.001 |
|
| ||||
| Congestive heart failure | 79 (14.6) | 50 (29.9) | 29 (7.7) | <0.001 |
|
| ||||
| Angine | 40 (7.4) | 15 (9.0) | 25 (6.6) | 0.337 |
|
| ||||
| Arrhythmia | 73 (13.4) | 40 (24.0) | 33 (8.8) | <0.001 |
|
| ||||
| Valvular heart disease | 17 (3.1) | 10 (6.0) | 7 (1.9) | 0.011 |
|
| ||||
| Hypertension | 211 (38.9) | 76 (45.5) | 135 (35.9) | 0.034 |
|
| ||||
| Peripheral artery disease | 49 (9.0) | 21 (12.6) | 28 (7.4) | 0.054 |
|
| ||||
| Cerebrovascular accident | 39 (7.2) | 13 (7.8) | 26 (6.9) | 0.717 |
|
| ||||
| Diabetes | 88 (16.2) | 36 (21.6) | 52 (13.8) | 0.024 |
|
| ||||
| Chronic renal failure | 8 (1.5) | 6 (3.6) | 2 (0.5) | 0.006 |
|
| ||||
| Liver disease | 36 (6.6) | 18 (10.8) | 18 (4.8) | 0.009 |
Abbreviations: BMI, body mass index; SGRQ, St George’s Respiratory Questionnaire.
We classified the 543 patients using the BODE index, GOLDABCD classification and cluster-based subtypes.
Using the BODE index, 47.9% had a score of 0–2, 35.5% a score of 3–4, 13.1% a score of 5%–6% and 3.5% had a score >6. The mean Charlson index for each group was 2.13 (SD ±1.19), 2.62 (SD ±1.54), 2.86 (SD ±1.74) and 2.26 (SD ±0.81), respectively.
When patients were stratified based on GOLDABCD criteria, 42.4% were classified as stage A, 15.6% as stage B, 19.0% as stage C and 23.0% as stage D. In this case, group A had the lowest score in the Charlson index, 2.14 (SD 1.24), and group B had the highest value, 2.91 (SD 1.64); the Charlson index for groups C and D was 2.42 (SD 1.51) and 2.55 (SD 1.39), respectively. After the update of GOLD2017, patients moved from C and D stages to A and B. Also, 54.8% and 28.4% were classified as stage A and B, respectively, whereas 6.5% and 10.3% were classified as stage C and D, respectively.
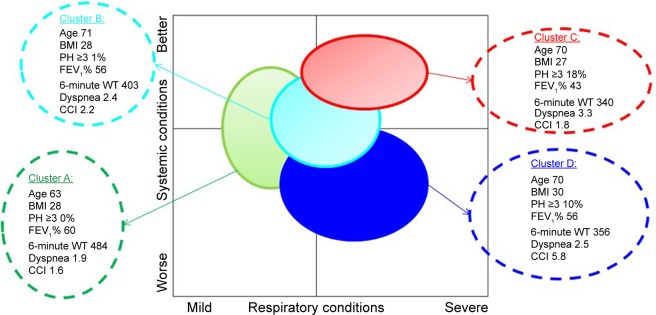
Finally, in relation to the cluster-based subtypes, patients were distributed into four different clusters: clusters A–C were appropriate for describing growing severity of the respiratory disease (mild to severe), while cluster D was more systemic, as previously described by Esteban et al17 (Figure 1).
Figure 1.
Grouping of patients given by cluster classification depending on respiratory conditions (horizontal axes) and systemic conditions (vertical axes) based on multiple correspondence analyses.
Note: Mean and SD were included in the bubbles for age, BMI, FEV1%, 6-minute WT, dyspnea and CCI, whereas the number of PH was described as the percentage of three or more.
Abbreviations: BMI, body mass index; CCI, Charlson comorbidity index; PH, previous hospitalizations; WT, walking test.
Patient distribution was as follows: 30.2% were included in cluster A, 35.9% in cluster B and 16.4% in cluster C, with Charlson indices of 1.6, 2.2 and 1.8, respectively. Among the patients, 17.5% were included in cluster D with similar respiratory characteristics to the intermediate group (cluster B), but more systemic disease, with a mean Charlson index of 5.8.
There were 167 deaths during follow-up (44.4%). Mortality was higher for patients included in stage D of the GOLDABCD and GOLD2017 classification, those with a BODE index higher than 6 and for patients included in clusters C (worse respiratory status) and D (high number of comorbidities). The prediction capacity for mortality was 0.678 for GOLDABCD, 0.689 for the BODE index and 0.722 for cluster-based subtypes, with no statistically significant differences among the three classification approaches. Using the updated GOLD2017, the prediction capacity seemed to be slightly worse (0.654 vs 0.678) compared with previous GOLDABCD, although differences were not statistically significant. However, compared with cluster-based subtype, GOLD2017 was worse for predicting mortality (0.654 vs 0.722, P<0.001), as shown in Table 2 and Figure 2.
Table 2.
Distribution of mortality by classification of patients based on different methods
| Classification | Total | Mortality | |
|---|---|---|---|
| No | Yes | ||
| GOLD, n (%) | |||
| A | 230 (42.4) | 190 (82.6) | 40 (17.4) |
| B | 85 (15.6) | 61 (71.8) | 24 (28.2) |
| C | 103 (19.0) | 67 (65.1) | 36 (34.9) |
| D | 125 (23.0) | 58 (46.4) | 67 (53.6) |
| AUC | 0.678 | ||
| GOLD2017, n (%) | |||
| A | 298 (54.8) | 237 (79.5) | 61 (20.5) |
| B | 154 (28.4) | 97 (63.0) | 57 (37.0) |
| C | 35 (6.5) | 20 (57.1) | 15 (42.9) |
| D | 56 (10.3) | 22 (39.3) | 34 (60.7) |
| AUC | 0.654 | ||
| Cluster, n (%) | |||
| A | 164 (30.2) | 150 (91.5) | 14 (8.5) |
| B | 195 (35.9) | 137 (70.3) | 58 (29.7) |
| C | 89 (16.4) | 44 (49.4) | 45 (50.6) |
| D | 95 (17.5) | 45 (47.4) | 50 (52.6) |
| AUC | 0.722 | ||
| BODE,a n (%) | |||
| 0–2 | 260 (47.9) | 213 (81.9) | 47 (18.1) |
| 3–4 | 193 (35.55) | 130 (67.4) | 63 (32.6) |
| 5–6 | 71 (13.1) | 31 (43.7) | 40 (56.3) |
| 7–10 | 19 (3.5) | 2 (10.5) | 17 (89.5) |
| AUC | 0.689 | ||
Note:
BODE score was categorized as proposed by Celli et al (2004).3
Abbreviations: AUC, area under the curve; BODE, body mass index, obstruction, dyspnea and exercise.
Figure 2.
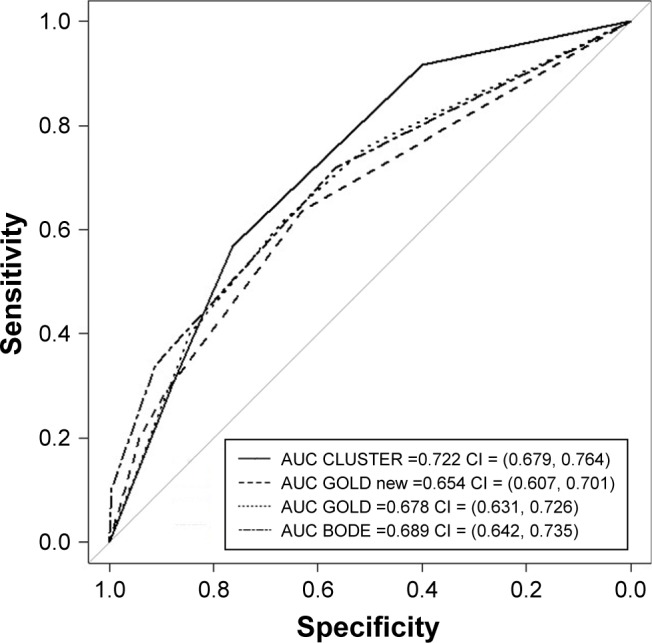
ROC curves for various mortality prediction rules: cluster classification, GOLDABCD, GOLD2017 and BODE.
Notes: GOLDABCD, GOLD2017 and cluster classification were included in the original four categories, and BODE score was categorized into four categories as proposed by Celli et al.3 AUC and 95% CI were included for each of the classification rules.
Abbreviations: AUC, area under the curve; BODE, body mass index, obstruction, dyspnea and exercise; ROC, receiver operating characteristic.
Comorbidities were frequent in our cohort, with a Charlson index of 2.4 (SD ±1.4). Cardiovascular comorbidities (coronary artery disease, congestive heart failure, arrhythmia and valvular heart disease) were associated with a major risk of death, with a >2- to 3-fold increased risk. Chronic renal failure had an even greater effect, increasing the mortality risk to 5.65 in the BODE index and 7.29 in GOLD (Table 3).
Table 3.
OR and its 95% CI obtained from a multiple logistic regression model including 5-year mortality as the outcome and various mortality prediction rules plus comorbidities as predictors
| Scores and comorbidities | OR | 95% CI | P-value |
|---|---|---|---|
| GOLD + comorbidities | |||
| GOLD | |||
| A | – | – | |
| B | 1.33 | 0.71, 2.48 | 0.37 |
| C | 1.95 | 1.11, 3.43 | 0.02 |
| D | 4.56 | 2.72, 7.62 | <0.001 |
| Coronary artery disease | |||
| No | – | – | |
| Yes | 2.70 | 1.23, 5.95 | 0.014 |
| Congestive heart failure | |||
| No | – | – | |
| Yes | 2.82 | 1.58, 5.03 | <0.001 |
| Arrhythmia | |||
| No | – | – | |
| Yes | 2.10 | 1.16, 3.82 | 0.014 |
| Chronic renal failure | |||
| No | – | – | |
| Yes | 7.29 | 1.23, 43.15 | 0.029 |
| BODE + comorbidities | |||
| BODEa | 1.59 | 1.40, 1.81 | <0.001 |
| Coronary artery disease | |||
| No | – | – | |
| Yes | 2.39 | 1.07, 5.37 | 0.034 |
| Congestive heart failure | |||
| No | – | – | |
| Yes | 2.41 | 1.33, 4.37 | 0.004 |
| Arrhythmia | |||
| No | – | – | |
| Yes | 2.32 | 1.27, 4.24 | 0.006 |
| Chronic renal failure | |||
| No | – | – | |
| Yes | 5.649 | 1.06, 43.99 | 0.042 |
Notes:
Raw BODE score, without any categorization. Only statistically significant comorbidities were maintained in the model.
Abbreviation: BODE, body mass index, obstruction, dyspnea and exercise.
Due to the absence of improvement in the prediction capacity with the updated GOLD2017, we used GOLDABCD for further analysis.
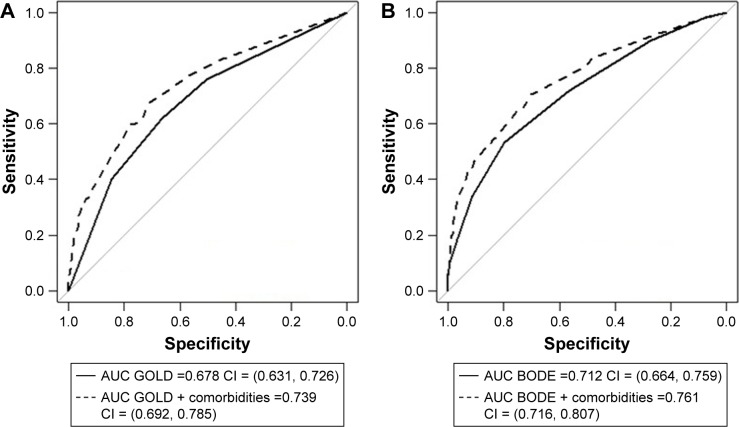
The prediction capacity of the BODE index and GOLDABCD after adding comorbidities was 0.761 and 0.739, respectively. There were no statistically significant differences between them (BODE index, GOLDABCD and cluster-based subtypes). However, the modified indices including comorbidities were better for predicting mortality compared with the original ones that did not include comoridities (P<0.001; Figure 3). Moreover, the values of the IDI were 0.082, 95% CI (0.054–0.110) and 0.073, 95% CI (0.046–0.100) for GOLDABCD and BODE, respectively, and the value of the NRI was 0.592, 95% CI (0.424–0.761) for both classification rules (all P<0.001).
Figure 3.
ROC curves for various mortality prediction rules plus comorbidities: (A) GOLD; (B) BODE.
Notes: BODE index was included as continuous, without any categorization. AUC and 95% CI were included for each of the classification rules, with and without including comorbidities. The comorbidities included were cardiac arrest, cardiac congestive disease, arrhythmias and kidney disease.
Abbreviations: AUC, area under the curve; BODE, body mass index, obstruction, dyspnea and exercise; ROC, receiver operating characteristic.
Discussion
This study shows the impact of comorbidities on the major COPD classification systems, the GOLDABCD and the BODE index. In general, the comorbidities that have more impact on mortality are cardiovascular diseases, including coronary artery disease, arrhythmia and valvular heart disease.
For many years, FEV1 has been the most important variable in the management of COPD. However, due to the heterogeneity of the disease, different COPD-related components are included nowadays in different scores: GOLDABCD, BODE index, ADO (age, dyspnea, airflow obstruction), DOSE (dyspnea, obstruction, smoking, exacerbation) and HADO (health status, physical activity, dyspnea, airway obstruction).3,9,33–35
Although GOLD is aimed at the management and classification of the disease, the way in which it was developed has resulted in many studies attempting to establish the prognostic capacity of both classification systems (GOLDFEV1 vs GOLDABCD). The Spanish multicenter COCOMICS study reported that the GOLDABCD score did not improve the prognostic capacity of the previous GOLDFEV1, based on spirometry alone.10 Similar results were found in a cohort of COPD patients, where GOLDABCD was a better predictor of exacerbations, with no differences between the two categories for predicting mortality.12
Continuing the multidimensional approach to the disease, the BODE index was developed and included four mortality-related risk factors (BMI, dyspnea, FEV1 and exercise capacity); it predicted the risk of death with an AUC of 0.74, better than using obstruction severity alone.3
Few studies have compared the GOLDABCD and BODE index for mortality. de Torres et al compared the ability of these two scores and found that the BODE index was superior for predicting short-term (24 months) and long-term (50 months) mortality (AUCGOLD-ABCD 0.68 vs AUCBODE 0.71).21 The way in which the BODE index was created and the inclusion of extra domains (BMI and 6MWT) related to exacerbations could explain the superiority of the BODE index.
In relation to the cluster-based subtypes, the four different clusters from our cohort were similar to those previously described.15,16 Subgroups A–C could be described as progressive worsening of the respiratory disease, while group D had moderate respiratory disease but with more systemic conditions.
Comparing GOLD 2017 (excluding FEV1 from the assessment tool) with the previous GOLD ABCD did not show any improvement for predicting mortality. It was also worse for predicting mortality when the new GOLD 2017 was compared with clusters.
Comorbidities are frequent in COPD and contribute to disease severity and mortality.36 The prevalence of at least one comorbidity in COPD patients is often reported to be >50%.37 Vanfleteren et al actively investigated the presence of comorbidities, finding that 97.7% of patients included in the study had one or more comorbidities, while 53.3% were diagnosed with four or more.38 The most prevalent comorbidities are similar in different studies. Divo et al found that hypertension, hyperlipidemia and coronary artery disease were the most prevalent, with a mean of six (SD =3) comorbidities.20 Almagro et al also described comorbidities in hospitalized COPD patients: hypertension, diabetes, dyslipemia and cardiovascular diseases were the most prevalent, with a mean Charlson index of 3.1.22 In our study, 68.3% of patients had at least one comorbidity, with a mean Charlson index of 2.4; the most prevalent diseases were hypertension, diabetes, heart failure and arrhythmia. The lower prevalence of comorbidities and lower Charlson index are likely due to patient recruitment, wherein outpatients were followed in five respiratory clinics.
Nonetheless, it is not clear how different comorbidities impact mortality in COPD patients and whether all underlying diseases should be taken into account. The ECLIPSE cohort and Divo et al identified a close relationship between specific comorbidities and mortality.20,39 In the ECLIPSE cohort, heart failure, ischemic heart disease and diabetes were associated with significantly increased mortality, independent of FEV1%, BODE index and exacerbations.39 Divo et al identified 12 comorbidities closely related to mortality, including cardiovascular disease (atrial fibrillation, heart failure and coronary artery disease) and anxiety, with an HR of 1.27–1.56 and 13.76, respectively, that were included in a 25-point score (COTE index).20 However, other authors have evaluated comorbidities as a group using the Charlson index: higher the Charlson Index score, higher is the risk of mortality.22
Among the comorbidities evaluated in our patients, coronary artery disease, congestive heart failure, arrhythmia and chronic renal failure were independently associated with 5-year mortality, with the ORs ranging from 2.10 (arrhythmia) to 7.29 (chronic renal failure). Despite its low prevalence (1.5%), chronic renal failure was strongly related with mortality (OR 7.29), probably due to the severity of the disease included in the Charlson index.
In recent years, different scores have been developed for the management and stratification of comorbidities. The COTE index was able to predict mortality, with a >26% increased risk of death with a score of ≥4 (HR 2.26–2.68; P<0.001 in all BODE quartiles), with an AUC of 0.62 (0.57–0.68).20 The CODEX index, including comorbidities from the Charlson index, was independently associated with short- and long-term mortality (HR 1.5 and 1.3, respectively).22
Despite the importance of comorbidities in COPD management, the effect of adding comorbidities to the existing scores is not clear. When the COTE index was combined with the original BODE, it was superior for predicting 24- and 50-month mortality (AUC 0.81) compared with the BODE index and GOLDABCD.21 The same occurred with CODEX, which was better for predicting short- and long-term mortality than BODE, GOLD, ADO or DOSE.22
Similar results were found in our cohort when the most relevant comorbidities were added. The prognostic capacity of the BODE index and GOLDABCD after adding cardiovascular comorbidities was superior compared with the original scores (0.712 vs 0.761, P<0.001 for the BODE index and 0.678 vs 0.739, P<0.001 for GOLD; Figure 3).
Our findings support the importance of comorbidities in the management of COPD, especially cardiovascular diseases, as a predictor of mortality, and perhaps should be considered in future severity scores. It is clear that neither all comorbidities nor their impact on mortality are similar. However, further studies are needed to clarify which comorbidities should be taken into account in future prognosis scores.
Limitations
This study has several limitations. First, comorbidities were determined by reviewing patient medical records, without investigating them actively; so, it might not represent the real “comorbidoma” of our COPD patients. Second, the findings may only be transferable to the type of patients included in the study. As the study was carried out in our patient respiratory clinics and the number of patients with FEV1 >80% has been really low, only the patients with FEV1 <80% have been included. Moreover, we only assessed all-cause mortality because of the difficulty to identify the real cause of death, as most of the them were out-of-hospital deaths. Finally, although the cluster analysis provides a lot of information about the patient, including multiple variables, it cannot currently be used for patient management and classification, as it is not possible to find out in which cluster might your patients be just using patients’ clinical variables/using clinical variables by themselves.
Conclusion
Our study confirms the importance of comorbidities in COPD patients that should be included in future management scores, due to their prevalence and impact on prognosis. However, further studies are needed to clarify which comorbidities should be taken into account.
Acknowledgments
This work was supported by Fondo de Investigación Sanitaria (grant number PI020510), Departamento de Sanidad del Gobierno Vasco (grant number 200111002), and Departamento de Educación, Cultura y Política Lingüística del Gobierno Vasco (grant numbers IT620-13 and Publibeca SEPAR 2016 [the latter grant paid for editing of the manuscript]).
Footnotes
Author contributions
All authors participated in the conception and design of the study. CE, IA and IB supervised the data collection. IA and IB analyzed and interpreted the data. AA wrote the first and all consecutive drafts of the manuscript. CE, JMQ, AGL and AU provided critical contributions to the drafts of the manuscript. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS, GOLD Scientific Committee Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–1276. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 2.Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 3.Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 4.Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1791–1797. doi: 10.1164/ajrccm.157.6.9705017. [DOI] [PubMed] [Google Scholar]
- 5.Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121(5):1434–1440. doi: 10.1378/chest.121.5.1434. [DOI] [PubMed] [Google Scholar]
- 6.Marín JM, Cote CG, Diaz O, et al. Prognostic assessment in COPD: health related quality of life and the BODE index. Respir Med. 2011;105(6):916–921. doi: 10.1016/j.rmed.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Martinez FJ, Foster G, Curtis JL, et al. Predictors of mortality in patients with emphysema and severe airflow obstruction. Am J Respir Crit Care Med. 2006;173(12):1326–1334. doi: 10.1164/rccm.200510-1677OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J. 2005;26(4):630–636. doi: 10.1183/09031936.05.00045505. [DOI] [PubMed] [Google Scholar]
- 9.Global Initiative for Chronic Obstructive Lung Disease (GOLD) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: revised 2011. [Accessed January 17, 2019]. Available: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2011_Jan21.pdf.
- 10.Soriano JB, Alfageme I, Almagro P, et al. Distribution and prognostic validity of the new Global Initiative for Chronic Obstructive Lung Disease grading classification. Chest. 2013;143(3):694–702. doi: 10.1378/chest.12-1053. [DOI] [PubMed] [Google Scholar]
- 11.Agusti A, Edwards LD, Celli B, et al. ECLIPSE Investigators Characteristics, stability and outcomes of the 2011 GOLD COPD groups in the ECLIPSE cohort. Eur Respir J. 2013;42(3):636–646. doi: 10.1183/09031936.00195212. [DOI] [PubMed] [Google Scholar]
- 12.Lange P, Marott JL, Vestbo J, et al. Prediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general population. Am J Respir Crit Care Med. 2012;186(10):975–981. doi: 10.1164/rccm.201207-1299OC. [DOI] [PubMed] [Google Scholar]
- 13.Vogelmeier CF, Criner GJ, Martínez FJ, et al. Global Strategy for the Diagnosis Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report GOLD Executive Summary. Eur Respir J. 2017;49(6):1700214. doi: 10.1183/13993003.00214-2017. [DOI] [PubMed] [Google Scholar]
- 14.Wardlaw AJ, Silverman M, Siva R, Pavord ID, Green R. Multidimensional phenotyping: towards a new taxonomy for airway disease. Clin Exp Allergy. 2005;35(10):1254–1262. doi: 10.1111/j.1365-2222.2005.02344.x. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Aymerich J, Gómez FP, Benet M, et al. Identification and prospective validation of clinically relevant chronic obstructive pulmonary disease (COPD) subtypes. Thorax. 2011;66(5):430–437. doi: 10.1136/thx.2010.154484. [DOI] [PubMed] [Google Scholar]
- 16.Burgel PR, Paillasseur JL, Caillaud D, et al. Clinical COPD phenotypes: a novel approach using principal component and cluster analyses. Eur Respir J. 2010;36(3):531–539. doi: 10.1183/09031936.00175109. [DOI] [PubMed] [Google Scholar]
- 17.Esteban C, Arostegui I, Aburto M, et al. Chronic obstructive pulmonary disease subtypes. Transitions over time. PLoS One. 2016;11(9):e0161710. doi: 10.1371/journal.pone.0161710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almagro P, Cabrera FJ, Diez J, et al. Comorbidities and short-term prognosis in patients hospitalized for acute exacerbation of COPD: the EPOC en Servicios de medicina interna (ESMI) study. Chest. 2012;142(5):1126–1133. doi: 10.1378/chest.11-2413. [DOI] [PubMed] [Google Scholar]
- 19.The Global Initiative for Chronic Obstructive Lung Disease (GOLD) Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. Report. 2017. 2017. [Accessed March 25, 2018]. Available from: http://goldcopd.org/gold2017-global-strategy-diagnosis-manage-mentprevention-copd.
- 20.Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. doi: 10.1164/rccm.201201-0034OC. [DOI] [PubMed] [Google Scholar]
- 21.de Torres JP, Casanova C, Marín JM, et al. Prognostic evaluation of COPD patients: GOLD 2011 versus BODE and the COPD comorbidity index COTE. Thorax. 2014;69(9):799–804. doi: 10.1136/thoraxjnl-2014-205770. [DOI] [PubMed] [Google Scholar]
- 22.Almagro A, Soriano JB, Cabrera FJ, et al. Short- and medium-term prognosis in patients hospitalized for COPD exacerbation the CODEX index. Chest. 2014;154:972–980. doi: 10.1378/chest.13-1328. [DOI] [PubMed] [Google Scholar]
- 23.Mahler DA, Ward J, Waterman LA, et al. Patient-reported dyspnea in COPD reliability and association with stage of disease. Chest. 2009;136(6):1473–1479. doi: 10.1378/chest.09-0934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 25.Jones PW, Quirk FH, Baveystock CM. The St George’s Respiratory Questionnaire. Respir Med. 1991;85(Suppl B):25–31. doi: 10.1016/s0954-6111(06)80166-6. [DOI] [PubMed] [Google Scholar]
- 26.Ferrer M, Alonso J, Prieto L, et al. Validity and reliability of the St George’s Respiratory Questionnaire after adaptation to a different language and culture: the Spanish example. Eur Respir J. 1996;9(6):1160–1166. doi: 10.1183/09031936.96.09061160. [DOI] [PubMed] [Google Scholar]
- 27.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 28.Manual SEPAR de Procedimientos . Procedimientos de evaluación de la función pulmonar [SEPAR Manual of Procedures. Pulmonary function evaluation procedures] Barcelona, Spain: Publicaciones Permanyer; 2002. Available from: https://issuu.com/separ/docs/procedimientos3?mode=window&backgroundColor=%23222222. Spanish. [Google Scholar]
- 29.Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Eur Respir J. 1993;6(Suppl 16):5–40. doi: 10.1183/09041950.005s1693. [DOI] [PubMed] [Google Scholar]
- 30.R development Core Team . A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2010. 2010. [Accessed January 12, 2019]. Software available from: http://cran.r-project.org. [Google Scholar]
- 31.Pencina MJ, D’Agostino RB, D’Agostino RB, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–172. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 32.Pencina MJ, D’Agostino RB, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30(1):11–21. doi: 10.1002/sim.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Puhan MA, Hansel NN, Sobradillo P, et al. Large-scale international validation of the ADO index in subjects with COPD: an individual subject data analysis of 10 cohorts. BMJ Open. 2012;2(6):e002152. doi: 10.1136/bmjopen-2012-002152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jones RC, Donaldson GC, Chavannes NH, et al. Derivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE index. Am J Respir Crit Care Med. 2009;180(12):1189–1195. doi: 10.1164/rccm.200902-0271OC. [DOI] [PubMed] [Google Scholar]
- 35.Esteban C, Quintana JM, Aburto M, et al. The health, activity, dyspnea, obstruction, age, and hospitalization: prognostic score for stable COPD patients. Respir Med. 2011;105(11):1662–1670. doi: 10.1016/j.rmed.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 36.Putcha N, Puhan MA, Hansel NN, Drummond MB, Boyd CM. Impact of co-morbidities on self-rated health in self-reported COPD: an analysis of NHANES 2001–2008. COPD. 2013;10(3):324–332. doi: 10.3109/15412555.2012.744963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frei A, Muggensturm P, Putcha N, et al. Five comorbidities reflected the health status in patients with chronic obstructive pulmonary disease: the newly developed COMCOLD index. J Clin Epidemiol. 2014;67(8):904–911. doi: 10.1016/j.jclinepi.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 38.Vanfleteren LE, Spruit MA, Groenen M, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(7):728–735. doi: 10.1164/rccm.201209-1665OC. [DOI] [PubMed] [Google Scholar]
- 39.Miller J, Edwards LD, Agustí A, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med. 2013;107(9):1376–1384. doi: 10.1016/j.rmed.2013.05.001. [DOI] [PubMed] [Google Scholar]