ABSTRACT
This review examined the evidence behind dietary guidelines for dairy. Most countries recommend consumption of dairy products; and when amounts are specified, recommendations are typically for 2 or 3 servings per day. Specific recommendations for dairy products are based partly on culture and availability but primarily on meeting nutrient requirements. Dairy products are a rich source of many minerals and vitamins as well as high-quality protein. Thus, dairy consumption is a marker for diet quality. A recent report found that yogurt specifically is a good marker of diet quality. The food patterns recommended by the 2010 Dietary Guidelines for Americans Advisory Committee (DGAC) include 3 cups of low-fat milk and milk products. Few people achieve their recommended intakes of several shortfall nutrients without meeting their recommendations for dairy. The evidence for a benefit of dairy consumption is moderate for bone health in children but limited in adults and moderate for cardiovascular disease, blood pressure, and diabetes and limited for metabolic syndrome. Newer data since the recommendations of the 2010 DGAC are presented. However, the strength of the evidence for dairy consumption and health is limited by the lack of appropriately powered randomized controlled trials.
WHAT ARE THE DIETARY RECOMMENDATIONS FOR DAIRY?
Dairy foods play a central role in most dietary guidance recommendations. They provide a package of essential nutrients and bioactive constituents for health that are difficult to obtain in diets with no or limited use of dairy products. The contribution of dairy products to providing recommended calcium intakes has largely driven the recommendation for dairy. Since the agricultural revolution when energy sources shifted from plant foods relatively high in calcium in the diets of hunter-gatherers to cereal crops with low calcium content, the major source of dietary calcium has been milk.
In addition to calcium, dairy products provide many other nutrients (Table 1) (1). They are a good source of high-quality protein, potassium, magnesium, phosphorus, zinc, selenium, vitamin A, riboflavin, thiamine, vitamin B-12, and vitamin D (when fortified) (2). Not all dairy products are equal sources of nutrients. The calcium content of soft cheeses, in which the curd is formed with acid, is reduced because some calcium is lost in the whey. Nutrients are diluted in the making of ice cream by the addition of fat and sugar. Cheeses are typically salted, which contributes to high sodium intakes. The fat content varies widely depending on the degree of removal of dairy fat. Not indicated in Table 1 is the reduced lactose content in yogurt and cheese, making those products popular in lactose-maldigesting cultures.
TABLE 1.
Nutrient composition per 100 g of selected dairy foods1
| USDA food name and food code | |||||||
| Cow milk, producer fluid, 3.7% milk fat (01078) | Milk, nonfat, fluid (skim) (01151) | Yogurt, plain, low fat (01117) | Yogurt, fruit, low fat (01122) | Cheese, cheddar (01009) | Cheese, cottage, nonfat, uncreamed, dry large or small curd (01014) | Ice cream, vanilla (19095) | |
| Energy (kcal) | 64 | 34 | 63 | 105 | 403 | 72 | 2.07 |
| Protein (g) | 3.3 | 3.37 | 5.3 | 4.9 | 24.9 | 10.3 | 3.5 |
| Total fat (g) | 3.7 | 0.08 | 1.6 | 1.4 | 33.1 | 0.3 | 11 |
| SFAs (g) | 2.3 | 0.1 | 1.0 | 0.9 | 21.1 | 0.2 | 6.8 |
| MUFAs (g) | 1.1 | 0 | 0.4 | 0.4 | 9.4 | 0.1 | 3.0 |
| PUFAs (g) | 0.1 | 0 | 0 | 0 | 0.9 | 0 | 0.5 |
| Cholesterol (mg) | 14 | 2 | 6 | 6 | 105 | 7 | 44 |
| Carbohydrate (g) | 4.7 | 4.96 | 7.0 | 18.6 | 1.3 | 6.7 | 23.6 |
| Calcium (mg) | 119 | 122 | 183 | 169 | 721 | 86 | 128 |
| Iron (mg) | 0.05 | 0.03 | 0.08 | 0.07 | 0.68 | 0.15 | 0.09 |
| Magnesium (mg) | 13 | 11 | 17 | 16 | 28 | 11 | 14 |
| Phosphorus (mg) | 93 | 101 | 144 | 133 | 512 | 190 | 105 |
| Potassium (mg) | 151 | 156 | 234 | 216 | 98 | 137 | 199 |
| Sodium (mg) | 49 | 42 | 70 | 65 | 621 | 330 | 80 |
| Zinc (mg) | 0.38 | 0.42 | 0.89 | 0.82 | 3.11 | 0.47 | 0.69 |
| Thiamine (mg) | 0.038 | 0.045 | 0.044 | 0.041 | 0.027 | 0.023 | 0.041 |
| Riboflavin (mg) | 0.161 | 0.182 | 0.214 | 0.198 | 0.375 | 0.226 | 0.240 |
Data are from reference 1.
Dairy intake recommendations vary from region to region. Some countries, such as the United Kingdom, provide general recommendations to consume milk and other dairy products daily, but most countries have quantitative recommendations that usually range from 2 to 3 servings or cups of milk or yogurt or sometimes the equivalent serving of cheese (Table 2). The 2010 Dietary Guidelines for Americans specify low-fat dairy products because of concern over the high prevalence of obesity (3).
TABLE 2.
Selected dietary recommendations for dairy by country
| Country and population group | Daily recommendation |
| Australia | |
| 12–18 y | 3 servings of milk, yogurt, cheese, or custard |
| All others >4 y | 2 servings of milk, yogurt, cheese, or custard |
| Canada | |
| 9–18 y | 3–4 servings of milk, yogurt, kefir, or cheese |
| 2–8 y, 19–50 y | 2 servings of milk, yogurt, kefir, or cheese |
| ≥51 y | 3 servings of milk, yogurt, kefir, or cheese |
| Chile | |
| 2–5 y | 3 cups milk or yogurt or one piece of cheese |
| 10–18 y | 3–4 cups milk or yogurt or one piece of cheese |
| 19–59 y | 3 cups milk or yogurt or one piece of cheese |
| ≥60 y | 2–3 cups milk or yogurt or one piece of cheese |
| China | |
| General | 300 g dairy milk or dairy products |
| Breastfeeding women | 500 mL dairy milk or dairy products |
| Finland | |
| All | 500 mL milk or liquid yogurt |
| France | |
| General >3 y | 3 servings of milk, cheese, or yogurt |
| India | |
| 1–18 y, pregnant and lactating women | 5 portions of milk |
| Adults | 3 portions of milk |
| Japan | |
| General | 2 servings of milk/milk products |
| South Africa | |
| 7–13 y | 2–3 cups milk, maas, yogurt, sour milk, or cheese |
| 14–25 y | 1–2 cups milk, maas, yogurt, sour milk, or cheese |
| >25 y | 1 cup milk, maas, yogurt, sour milk, or cheese |
| Switzerland | |
| General | 3 portions of milk, yogurt, or cheese |
| Elderly | 3–4 portions of milk, yogurt, or cheese |
| United Kingdom | |
| General | Eat some milk and dairy foods every day |
| Turkey | |
| Adults | 2 servings of milk, yogurt, or cheese |
| Children, adolescents, pregnant and lactating women | 3–4 servings of milk, yogurt, or cheese |
| United States | |
| 2–3 y | 2 cups of low-fat milk, yogurt, or fortified beverage |
| 4–8 y | 2.5 cups of low-fat milk, yogurt, or fortified beverage |
| >9 y | 3 cups of low-fat milk, yogurt, or fortified beverage |
HOW DAIRY RECOMMENDATIONS ARE SET BY THE DIETARY GUIDELINES FOR AMERICANS
Milk has had a major role in one of the food groups since the USDA published the first food guide in 1917. In that first food guide there were only 5 groups; milk was combined with meat. In 1933, 12 food groups were recommended, and milk was expanded to include milk products, which comprised a single major food group. Milk and milk products remained as an independent group in the 1940s with the Basic Seven guide, in the Basic Four guide from the 1950s to the 1970s, in the Pyramid/MyPyramid guides of the 1980s to 2010, and in the current 2011 MyPlate (4, 5). The food groups of MyPlate include protein, fruit, vegetables, low-fat milk and milk products, and whole grains.
The amount of milk and milk products (and other food groups) is determined by the Dietary Guidelines for Americans Advisory Committee (DGAC)5 (6) on the basis of 1) intakes of the food groups needed to achieve the Dietary Reference Intakes (DRIs) for essential nutrients without exceeding energy needs and 2) the evidence for the relation of intake of food groups and relevant health outcomes. In an iterative process, food intake pattern modeling and interpretation of the evidence on the relation to health developed the food intake patterns for MyPyramid/MyPlate (6, 7). The 12 patterns developed for various energy and nutrient needs of different age and sex groups were created to meet the DRIs for that subpopulation and guidance from evidence-based reviews. For some nutrients, the Recommended Dietary Allowance was used, and for others with insufficient evidence to determine the Recommended Dietary Allowance, the Adequate Intake for a healthy population was used. However, when the review of the literature led to a decision by the DGAC to increase or decrease the amount of a food group to recommend, food modeling was again used to adjust the intake recommendations of other food groups to meet the DRIs for the essential nutrients within each energy pattern.
The intent of food guidance is to be flexible to accommodate the diversity of culture and preferences of the population. For most food groups, there is a large choice of items within the category. However, for the milk and milk products food group, most foods within the category stem from a similar raw ingredient, ie, milk from a domesticated animal supply. The food guides include alternative sources of protein and calcium and guidance for those with milk protein allergy or lactose intolerance. However, few people who avoid dairy products achieve recommended intakes of several shortfall nutrients, such as calcium, potassium, magnesium, riboflavin, and vitamin D.
DAIRY PRODUCTS AND DIET QUALITY
Milk products, along with fruit, vegetables, and whole grains, were identified by the 2005 and 2010 DGAC as foods that need to be increased to meet nutrient needs and for improved health (3, 8). The role of milk products in meeting 3 shortfall nutrients for various age groups is shown in Table 3 (9).The best and most economical source of the limiting nutrients is dairy (10). Supplements typically do not fill the gap of all these nutrients for those who do not consume recommended intakes of dairy products. By using NHANES 2001–2002 data, Gao et al (11) determined that it is impossible to meet calcium recommendations while meeting other nutrient recommendations with a dairy-free diet within the current US dietary pattern. Fulgoni et al (12) identified calcium-rich foods that could provide as much calcium as a serving of dairy (eg, 1.1 servings of fortified soy beverage, 0.5 servings of fortified orange juice, 1.2 servings of bony fish, or 2.2 servings of leafy greens), but these foods did not provide the equivalent profile of other nutrients and the amounts needed are unrealistic in some cases. By using the 1999–2004 NHANES data, Nicklas et al (13) determined that <3% of the US population met potassium recommendations and 55% did not meet their Estimated Average Requirement for magnesium. This group recently reported the following major barriers to meeting the Dietary Guidelines recommendations: 1) inadequate meal preparation skills, 2) difficulty in changing eating habits, 3) lack of understanding the specific recommendations, and 4) taste preference (13).
TABLE 3.
Role of milk products in food patterns1
| 2–8 y | 9–18 y | 19–50 y | ≥51 y | |||||
| Without dairy | With dairy | Without dairy | With dairy | Without dairy | With dairy | Without dairy | With dairy | |
| % of recommendation | % of recommendation | % of recommendation | % of recommendation | |||||
| Calcium | 146 | 54 | 97 | 32 | 134 | 47 | 107 | 38 |
| Potassium | 70 | 43 | 59 | 38 | 68 | 48 | 71 | 49 |
| Magnesium | 254 | 160 | 114 | 69 | 112 | 79 | 109 | 75 |
Adequate Intakes for calcium and potassium and Estimated Average Requirements for magnesium are shown. Data are from reference 9. With dairy = 2.5–3.5 servings/d; Without dairy = <1 serving/d.
A number of studies have indicated that milk intake is a marker for dietary quality because of its nutrient contributions (10, 14–16). Recently, the Framingham Heart Study offspring cohort, involving 6526 adults, found that yogurt is also a marker of dietary quality (17). Yogurt consumers compared with nonconsumers had improved diet quality scores (according to the Dietary Guidelines Adherence Index with a maximum score of 20) of 9.4 compared with 8.05. The prevalence of nutrient inadequacy was also much lower in the 64% of women and 41% of men in the cohort who consumed yogurt (Figure 1). Yogurt consumption also increased the percentage of individuals exceeding the Adequate Intake for potassium (11.4% compared with 4.7%) and fiber (22.4% compared with 10.0%). Unfortunately, milk or dairy products other than yogurt were not evaluated so it is not possible to compare which of the dairy products is the best marker of diet quality.
FIGURE 1.
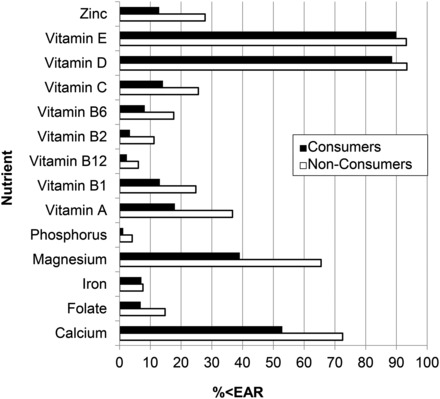
Yogurt consumption is associated with better diet quality compared with nonconsumers for all nutrients in generalized estimating equation models (P < 0.001). Data are from reference 14. EAR, Estimated Average Requirement.
The nutrient concentration on a weight basis is greater in yogurt and cheese than in milk, but serving sizes are typically less for these products than for milk. Calcium bioavailability was not significantly different among various dairy products prepared from milk endogenously labeled with stable calcium isotopes and tested in women aged 24–42 y (18) (Figure 2). Little is known about the bioavailability of most of the other nutrients provided by dairy products.
FIGURE 2.
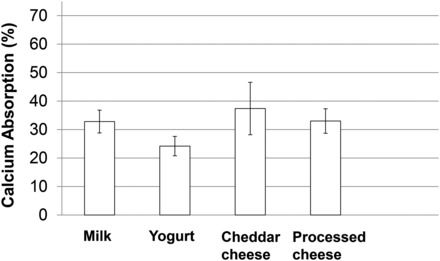
Mean (±SEM) calcium bioavailability from dairy products endogenously labeled with a stable calcium isotope in 7 adult women. There were no significant differences by ANOVA. Data are from reference 18.
EVIDENCE FOR A RELATION BETWEEN MILK INTAKE AND HEALTH OUTCOMES
The 2010 DGAC concluded that the evidence for intake of milk and milk products was moderate for a positive relation with bone health in children but limited in adults; moderate for an inverse relation with cardiovascular disease, blood pressure, and type 2 diabetes in adults; limited for an inverse relation with metabolic syndrome; insufficient to assess the relation with serum cholesterol; and strong for no unique relation to weight control (8). The long latency period for chronic disease outcomes make randomized controlled trials (RCTs) with food impractical, except in some cases in vulnerable populations. Consequently, meta-analyses and systematic reviews on the relation between milk and milk product intake and health tend to use RCTs of biomarkers or on prospective or observational studies. This is reasonable for health impacts related to nutrition.
Bone
The consequences of excluding dairy in the diet are most associated with compromised bone health. Effects apparently can begin in utero as evidenced by a study that showed increased consumption of milk and milk products by pregnant women at 28 wk gestation significantly (P < 0.05) predicted total body and bone mineral content (BMC) of children at age 6 y (19). Nutrition in the first 2–3 y of life is important for growth. The addition of milk and milk products to the diet is associated with improved linear growth as shown by observational and interventional studies, especially in developing countries (20, 21). The increased growth with milk/milk product intake is attributed to the essential nutrients provided, especially the limiting minerals for bone mineral acquisition, and to stimulation of serum insulin-like growth factor I. Bone accretion is high during the first year of life, but cow milk is not recommended before 1 y of age. Infants rely on breast milk or formula and, on average, they meet their nutrient needs. The pubertal growth spurt is a critical time for building peak bone mass to protect against fracture risk as a child and later in life. Almost half of adult peak bone mass is acquired during adolescence (22). Approximately 95% of adult peak bone mass is acquired by the age of 16.2 y (23), emphasizing that nutrition can only influence peak bone mass appreciably before the end of adolescence. Thereafter, any benefits are to minimizing loss of peak bone mass, a much lower return on investment approach.
A meta-analysis of trials of dairy products and dietary calcium on BMC in children showed significantly higher total body and lumbar spine BMC with higher intakes when the comparison group had low calcium intakes (24). Benefits to growing bone by milk consumption appear to be more than merely providing required nutrients that are important to growing bone. In a growing rat model, when adequate dietary calcium was given as nonfat dry milk, bones were larger and stronger than when calcium was supplied as calcium carbonate (25). Moreover, when rats were switched to the same low-calcium diet during adulthood, rats fed nonfat dry milk during growth retained many of the advantages compared with rats fed calcium carbonate. In a retrospective study in postmenopausal women in NHANES III, low milk intake during childhood was associated with twice the risk of fracture (26). Studies of milk avoiders compared with age-matched cohorts in the same population with the same geographic and cultural environment are the strongest type of observational studies because they are the least confounded by factors such as other dietary constituents, race, sunlight, physical activity, etc. Studies of this type show an advantage to milk drinking in both children and adults. Milk avoiders in New Zealand children had a fracture risk of 34.8% compared with 13.0% for the matched cohort (27). In early pubertal girls in California and Indiana, perceived milk intolerance was inversely related to BMC for several bone sites (P = 0.009 for the lumbar spine and trends for total hip, femoral neck, and total body) (28). In contrast, lactose maldigestion, as measured by hydrogen breath analysis, was not related to bone measures.
There are no meta-analyses of RCTs of milk/milk product consumption and fracture outcomes or incidence of osteoporosis; however, there are meta-analyses and systematic reviews of calcium supplementation and fracture and meta-analyses of prospective studies of dairy intake and fracture (29, 30). A meta-analysis of prospective cohort studies concluded that there is no overall association between milk intake and hip fracture risk in women, whereas, in men, evidence was suggestive of a benefit of higher milk intake (31).
There are also matched-cohort studies in milk avoiders and milk consumers. In Finnish women aged 38–57 y, women who were lactose intolerant consumed 570 mg calcium daily compared with 850 mg daily in the lactose-tolerant group, and had double the risk of lower body fracture (OR: 2.15; 95% CI: 1.53, 3.04) (32).
Cardiovascular disease and blood pressure
As for bone, there is a lack of adequately powered RCTs on cardiovascular disease and blood pressure; the evidence used by the 2010 DGAC for a benefit of dairy is based on systematic reviews and meta-analyses of prospective and cohort studies (7). A systematic review and meta-analysis (32) showed a reduction in risk of myocardial infarction, ischemic heart disease, hypertension, and stroke in those consuming the highest amount of milk compared with those consuming the lowest amount. This was consistent with another systematic review (29) and a case-control study (34). It is also consistent with large prospective cohort studies published since the 2010 DGAC report (35–38). Also, published after the 2012 DGAC report was a meta-analysis reporting a 13% reduction in risk of all-cause mortality, an 8% reduction in risk of ischemic heart disease, and a 21% reduction in risk of stroke in those with the highest compared with the lowest intake of dairy (39). This contrasts with another meta-analysis of 6 prospective cohort studies that reported no association with milk and risk of coronary heart disease or stroke but a possible inverse relation to overall cardiovascular disease risk (40).
The DASH (Dietary Approaches to Stop Hypertension)-style diet includes low-fat dairy products (41). Because of the reduction in blood pressure associated with this dietary pattern, a diet high in potassium, calcium, and magnesium, which can be accomplished with a diet rich in fruit, vegetables and diary, is promoted in clinical and dietary guidelines.
Little evidence exists for individual dairy foods, although yogurt was associated with better systolic blood pressure, and fluid milk was associated with reduced systolic and diastolic blood pressure (42).
Type 2 diabetes and metabolic syndrome
One meta-analysis of 4 prospective studies constituted the evidence used by the 2010 DGAC to determine the benefit of dairy in reducing risk of diabetes. Those with the highest milk consumption compared with those with the lowest milk consumption had a 15% reduction in risk of type 2 diabetes (18). In a more recent meta-analysis of 7 cohort studies, there was a reduction of 18% in the risk of type 2 diabetes associated with low-fat dairy and a reduction of 17% with yogurt (43). The benefit of dairy on reduced risk of metabolic syndrome was based on 1 systematic review with meta-analysis, 1 prospective cohort study, and 3 cross-sectional cohort studies (8). The systematic review and meta-analysis reported a 26% reduction in risk of metabolic syndrome in those consuming the highest amounts of milk compared with those consuming the lowest amounts (33).
Subsequent to the DGAC report, Nicklas et al (44) reported that perceived lactose intolerance was associated with higher rates of diagnosis of diabetes and hypertension in the national sample of 3452 adults. The authors speculated that reduced dairy intake would reduce diet quality, ie, lower intakes of calcium, magnesium, vitamin D, and other nutrients that may predispose these individuals to higher risk of diseases.
CONCLUSIONS
This review examined the evidence for dietary guidelines for dairy. The evidence is strong for the role of dairy in meeting daily nutrient recommendations. Because milk and other dairy products are concentrated sources of so many essential nutrients, it is difficult to achieve recommended intakes with dietary patterns that contain little or no dairy products. This type of evidence is not from RCTs or prospective studies but from food intake analysis comparing nutrient composition associated with a range of intakes of dairy products to nutrient recommendations. The role of dairy in meeting nutrient recommendations has been shown largely for milk and recently for yogurt. Meeting nutrient recommendations has little to do with fat content or flavorings in the dairy products. The recommendation for low-fat dairy is more of a philosophical argument to reduce energy intake from fat and added sugar than from evidence of health concerns. Milk and cheese contribute 9.2% of intake of energy, 10.9% of fat, and 8.3% of carbohydrate in the diet of Americans, but these products also contribute 46.3% of calcium, 11.6% of potassium, and 7.9% of magnesium in the American diet, which may provide overriding benefits to health (45).
The evidence for a relation between dairy consumption and health is less strong because there are few adequately powered RCTs of sufficient duration to affect health outcomes of long latency periods relevant to milk. Evidence for a benefit is stronger in children for calcium balance and bone mineral density and in adults for blood pressure because these biomarkers of health outcomes can be studied in shorter RCTs. These types of studies are needed to compare the benefit of various dairy products. Because weight change can also be measured over a practical study duration of an RCT, the evidence for concluding that milk has no unique role in weight control was also considered strong by the 2010 DGAC. The evidence for disease outcome measures derives primarily from systematic reviews and meta-analyses of prospective cohort studies. Thus, there is limited to moderate evidence for a benefit of dairy intake on cardiovascular disease, metabolic syndrome, and type 2 diabetes.
The most productive path forward for strengthening our understanding of a health benefit specifically for yogurt or any other dairy product is with RCTs that use biomarkers of health. Yogurt and milk could be compared in balance studies measuring calcium, magnesium, and potassium absorption and retention, as well as blood pressure or other markers of metabolic syndrome.
Acknowledgments
Editorial assistance was provided by Chill Pill Media LLP, which was contracted and funded by Danone Institute International.
CMW received financial reimbursement for travel expenses and an honorarium from the Danone Institute International for her participation in the conference. She is a member of the Yogurt in Nutrition Initiative Advisory Board and has received grant funding from the Dairy Research Institute.
ABBREVIATIONS
- BMC
bone mineral content
- DGAC
Dietary Guidelines for Americans Advisory Committee
- DRI
Dietary Reference Intake
- RCT
randomized controlled trial
FOOTNOTES
Presented at the satellite symposium “First Global Summit on the Health Effects of Yogurt,” held in Boston, MA, at ASN’s Scientific Sessions at Experimental Biology 2013, 24 April 2013. The conference was organized by the ASN, the Nutrition Society, Danone Institute International, and the Dairy Research Institute. The supplement scientific guest editors were Sharon M Donovan, University of Illinois, Urbana, IL, and Raanan Shamir, Schneider Children’s Medical Center and Tel Aviv University, Israel.
Supported by NIH grant H0061908.
REFERENCES
- 1. USDA. USDA National Nutrient Database for Standard Reference. 2009. Available from: http://ndb.nal.usda.gov/ndb/search/list (cited 17 March 2014).
- 2. Gaucheron F.. Milk and dairy products: a unique micronutrient combination. J Am Coll Nutr 2011;30:400S–9S. [DOI] [PubMed] [Google Scholar]
- 3. US Department of Health and Human Services; USDA. Dietary guidelines for Americans, 2005. 6th ed. Washington, DC: US Government Printing Office, 2005. [Google Scholar]
- 4. Davis C, Saltos E.. Dietary recommendations and how they have changed over time In: America’s eating habits: changes and consequences. Agriculture Information Bulletin NO (AIB-750), pp 449 Washington, DC: USDA, Economics Research Service, 1999. [Google Scholar]
- 5. Post RC, Maniscalco S, Herrup M, Chang S.. What’s new on MyPlate? A new message, redesigned web site, and SuperTracker debut. J Acad Nutr Diet 2012;112:18–22. [DOI] [PubMed] [Google Scholar]
- 6. Britten P, Lyon J, Weaver CM, Kris-Etherton P, Nicklas T, Weber J, Davis C.. MyPyramid food intake pattern modeling for the Dietary Guidelines Advisory Committee. J Nutr Educ Behav 2006;38:S143. [DOI] [PubMed] [Google Scholar]
- 7. Weaver C, Nicklas T, Britten P.. The 2005 Dietary Guidelines Advisory Committee report. Nutr Today 2005;40:102–7. [Google Scholar]
- 8. The Dietary Guidelines Advisory Committee. Report of the Dietary Guidelines Advisory Committee on the Dietary guidelines for Americans, 2010. Washington DC: U.S. Department of Agriculture Research Service, 2011. [Google Scholar]
- 9. Nicklas TA, O’Neil CE, Fulgoni VL.. The role of dairy in meeting the recommendations for shortfall nutrients in the American Diet. J Am Coll Nutr 2009;28:73S–81S. [DOI] [PubMed] [Google Scholar]
- 10. Fulgoni V III, Nichols J, Reed A, Buckley R, Kafer K, Huth P, DiRienzo D, Miller GD.. Dietary consumption and related nutrient intake in African-American adults and children in the United States: Continuing Survey of Food Intakes by Individuals 1994–1996, 1998, and the National Health and Nutrition Examination Survey 1999–2000. J Am Diet Assoc 2007;107:256–64. [DOI] [PubMed] [Google Scholar]
- 11. Gao X, Wilde PE, Lichtenstein AH, Tucker KL.. Meeting adequate intake for dietary calcium without dairy foods in adolescents aged 9 to 18 years (National Health and Nutrition Examination Survey 2001–2002). J Am Diet Assoc 2006;106:1759–65. [DOI] [PubMed] [Google Scholar]
- 12. Fulgoni VL III, Keast DR, Auestad N, Quann EE.. Nutrients from dairy foods are difficult to replace in diets of Americans: food pattern modeling and an analyses of the National Health and Nutrition Examination Survey 2003–2006. Nutr Res 2011;31:759–65. [DOI] [PubMed] [Google Scholar]
- 13. Nicklas TA, Jahns L, Bogle ML, Chester DN, Giovanni M, Klurfeld DM, Laugero K, Liu Y, Lopez S, Tucker KL.. Barriers and facilitators for consumer adherence to the Dietary Guidelines for Americans: the HEALTH Study. J Acad Nutr Diet 2013;113:1317–31. [DOI] [PubMed] [Google Scholar]
- 14. Barger-Lux MJ, Heany RP, Pakard PT, Lappe JM, Recker RR.. Nutritional correlations of low calcium intake. Clin Appl Nutr 1992;2:39–44. [Google Scholar]
- 15. Ranganathan R, Nicklas TA, Yang SJ, Berenson GS.. The nutritional impact of dairy product consumption on dietary intakes of adults (1995–1996): the Bogalusa Heart Study. J Am Diet Assoc 2005;105:1391–400. [DOI] [PubMed] [Google Scholar]
- 16. Coudray B.. The contribution of dairy products to micronutrient intakes in France. J Am Coll Nutr 2011;30:410S–4S. [DOI] [PubMed] [Google Scholar]
- 17. Wang H, Livingston KA, Fox CS, Meigs JB, Jacques PF.. Yogurt consumption is associated with better diet quality and metabolic profile in American men and women. Nutr Res 2013;33:18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nickel KP, Martin BR, Smith DL, Smith JB, Miller GD, Weaver CM.. Calcium bioavailability from bovine milk and dairy products in premenopausal women using intrinsic and extrinsic labeling techniques. J Nutr 1996;126:1406–11. [DOI] [PubMed] [Google Scholar]
- 19. Ganpule A, Yajnik CS, Fall CHD, Rao S, Fisher DJ, Kanade A, Cooper C, Naik S, Joshi N, Lubree H et al. Bone mass in Indian children—relationships to maternal nutritional status and diet during pregnancy: the Pune Maternal Nutrition Study. J Clin Endocrinol Metab 2006;91:2994–3001. [DOI] [PubMed] [Google Scholar]
- 20. Allen LH, Dror DK.. Effects of animal source foods, with emphasis on milk, in the diet of children in low-income countries. Nestle Nutr Workshop Ser Pediatr Program 2011;67:113–30. [DOI] [PubMed] [Google Scholar]
- 21. Hoppe C, Mølgaard C, Juul A, Michaelsen MK.. High intakes of skimmed milk, but not meat, increase serum IGF-I and IGF BP-3 in eight year old boys. Eur J Clin Nutr 2004;58:1211–6. [DOI] [PubMed] [Google Scholar]
- 22. Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, Weaver CM.. Peak bone mass. Osteoporos Int 2000;11:985–1009. [DOI] [PubMed] [Google Scholar]
- 23. Teegarden D, Proulx WR, Martin BR, Zhao J, McCabe GP, Lyle RM, Peacock M, Slemenda C, Johnston CC, Weaver CM.. Peak bone mass in young women. J Bone Miner Res 1995;10:711–5. [DOI] [PubMed] [Google Scholar]
- 24. Huncharek M, Muscat J, Kupelnick B.. Impact of dairy products and dietary calcium on bone-mineral content in children: results of a meta-analysis. Bone 2008;43:312–21. [DOI] [PubMed] [Google Scholar]
- 25. Weaver CM, Janle E, Martin B, Browne S, Guiden H, Lachick P, Lee W-H.. Dairy versus calcium carbonate in promoting peak bone mass and bone maintenance during subsequent calcium deficiency. J Bone Miner Res 2009;24:1411–9. [DOI] [PubMed] [Google Scholar]
- 26. Kalkwarf HJ, Khoury JC, Lamphear BP.. Milk intake during childhood and adolescence, adult bone density, and osteoporotic fractures in U.S. women. Am J Clin Nutr 2003;77:257–65. [DOI] [PubMed] [Google Scholar]
- 27. Goulding A, Rockell JE, Black RE, Grant AM, Jones IE, Williams SM.. Children who avoid drinking cow’s milk are at increased risk for prepubertal bone fractures. J Am Diet Assoc 2004;104:250–3. [DOI] [PubMed] [Google Scholar]
- 28. Matlik L, Savaiano D, McCabe G, VanLoan M, Blue CL, Boushey CJ.. Perceived milk intolerance is related to bone mineral content in 10- to 13-year-old female adolescents. Pediatrics 2007;120:e669–77. [DOI] [PubMed] [Google Scholar]
- 29. Alvarez-León EE, Roman-Viñas B, Serra-Majem L.. Dairy products and health: a review of the epidemiological evidence. Br J Nutr 2006;96:S94–9. [DOI] [PubMed] [Google Scholar]
- 30. Kanis JA, Johansson H, Oden A, De Laet C, Johnell O, Eisman JA, McCloskey E, Mellstrong D, Pols H, Reeve J et al. A meta-analysis of milk intake and fracture risk: low utility for case finding. Osteoporos Int 2005;16:799–804. [DOI] [PubMed] [Google Scholar]
- 31. Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA, Kanis JA, Orav EJ, Staehelin HB, Kiel DP, Burckhardt P, Henschkowski J, Spiegelman D et al. Milk intake and risk of hip fracture in men and women: a meta-analysis of prospective cohort studies. J Bone Miner Res 2011;26:833–9. [DOI] [PubMed] [Google Scholar]
- 32. Honkanen R, Kröger H, Alhava E, Turpeinen P, Tuppurainen M, Saarikoski S.. Lactose intolerance associated with fractures of weight-bearing bone in Finnish women aged 38-57 years. Bone 1997;21:473–7. [DOI] [PubMed] [Google Scholar]
- 33. Elwood PC, Givens DI, Beswick AD, Fehily AM, Pickering JE, Gallacher J.. The survival advantage of milk and dairy consumption: an overview of evidence from cohort studies of vascular diseases, diabetes and cancer. J Am Coll Nutr 2008;27:723S–34S. [DOI] [PubMed] [Google Scholar]
- 34. Kontogianni MD, Panagiotakos DB, Chrysohoou C, Pitsavos C, Stefanadis C.. Modelling dairy intake on the development of acute coronary syndromes: the CARDIO2000 study. Eur J Cardiovasc Prev Rehabil 2006;13:791–7. [DOI] [PubMed] [Google Scholar]
- 35. Larsson SC, Virtamo J, Wolk A.. Dairy consumption and risk of stroke in Swedish women and men. Stroke 2012;43:1775–80. [DOI] [PubMed] [Google Scholar]
- 36. Bernstein AM, Pan A, Rexrode KM, Stampfer M, Hu FB, Mozaffarian D, Willett WC.. Dietary protein sources and the risk of stroke in men and women. Stroke 2012;43:637–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Patterson E, Larsson SC, Wolk A, Åkesson A.. Association between dairy food consumption and risk of myocardial infarction in women differs by type of dairy food. J Nutr 2013;143:74–9. [DOI] [PubMed] [Google Scholar]
- 38. Larsson SC, Orsini N, Wolk A.. Dietary calcium intake and risk of stroke: a dose-response meta-analysis. Am J Clin Nutr 2013;97:951–7. [DOI] [PubMed] [Google Scholar]
- 39. Elwood PC, Pickering JE, Givens I, Gallacher JE.. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids 2010;45:925–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Soedamah-Muthu SS, Ding El, Al-Delaimy Wk, Hu FB, Engberink MF, Willett WC, Geleijnse JM.. Milk and dairy consumption and incidence of cardiovascular disease and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr 2011;93:158–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Appel LJ, Moore TJ, Obarzanek E, Vallmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA.. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 42. Beydoun MA, Gary TL, Caballero BH, Lawrence RS, Cheskin LJ, Wang Y.. Ethnic differences in dairy and related nutrient consumption among US adults and their association with obesity, central obesity, and the metabolic syndrome. Am J Clin Nutr 2008;87:1914–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tong X, Dong JY, Wu ZW, Li W, Qin LQ.. Dairy consumption of risk of type 2 diabetes mellitus: a meta-analysis of cohort studies. Eur J Clin Nutr 2011;65:1027–31. [DOI] [PubMed] [Google Scholar]
- 44. Nicklas TA, Qu H, Hughes SO, He M, Wagner SE, Foushee HR, Shewchuk RM.. Self-perceived lactose intolerance results in lower intakes of calcium and dairy foods and is associated with hypertension and diabetes in adults. Am J Clin Nutr 2011;94:191–8. [DOI] [PubMed] [Google Scholar]
- 45. Huth PJ, Fulgoni VL III, Keast DR, Park K, Auestad N.. Major food sources of calories, added sugars, and saturated fat and their contribution to essential nutrient intake in the U.S. diet: data from the national health and nutrition examination survey (2003–2006). Nutr J 2013;12:116. [DOI] [PMC free article] [PubMed] [Google Scholar]


