Dear Sir:
The letter from Burton addresses an important issue regarding the use of a fat mass index (FMI). Similar to BMI, the goal of expressing fat mass relative to height is to have an index of body fat that is independent of overall body size. Burton proposes that (fat mass)/height3 is a more appropriate formulation for FMI compared with (fat mass)/height2. The changes in body proportions and body composition during childhood and adolescence are indeed complex, so the task of identifying the optimal index across the entire age range is challenging. There were multiple considerations in our selection of (fat mass)/height2 rather than other indexes such as the one proposed by Burton.
The primary rationale for expressing fat mass relative to height squared in our article (1) was to generate reference data for fatness that could be readily compared with existing means of assessing adiposity in the pediatric population. BMI, calculated as (body mass)/height2, is the most widely used method to screen for excess adiposity in children and adults. Because of the familiarity with BMI as a frame of reference across the research, clinical care, and public health spectrums, FMI is a meaningful measure.
It is important to note that BMI is a measure of body mass that is independent of height in adults (2), but this is not the case in the pediatric population in whom a positive correlation between height and BMI is generally seen (3, 4). The same is true for fat mass. The true value of p [as in the equation FMI = (fat mass)/heightp] necessary to eliminate the correlation between height and FMI and BMI has been investigated previously and found to vary across the pediatric age range (5, 6). Cross-sectional correlations between height and measures of adiposity including BMI, FMI [(fat mass)/height2], and FMI3 [(fat mass)/height3] at each age for children aged 8–20 y in our NHANES sample are shown in Figure 1. For all 3 measures, the correlations with height tend to be highest around the ages of the adolescent growth spurt and are lower at older ages. Although the correlation with height was lower for (fat mass)/height3, the use of (fat mass)/height3 did not eliminate the positive correlation with height seen among younger children and resulted in a larger negative correlation among older children.
FIGURE 1.
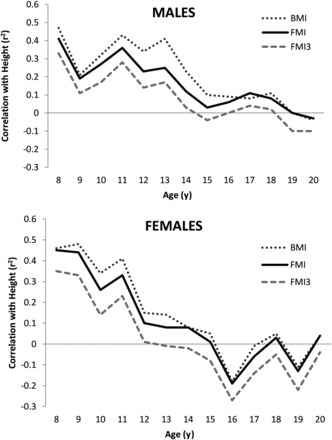
Cross-sectional correlations between height and BMI, FMI [(fat mass)/height2], and FMI3 [(fat mass)/height3] among 7336 NHANES participants aged 8–20 y. Pearson’s correlation coefficients are shown. FMI, fat mass index.
Most important, it is unclear whether the ideal index of adiposity should be independent of height because this may mask biological associations between adiposity and height (7). Studies have found that height-independent formulations of body mass and fat mass may be inferior for the detection of cardiometabolic risk factors compared with traditional formulations of BMI and FMI (6, 8). To our knowledge, there are no studies that show that (fat mass)/height3 is superior to FMI or BMI in identifying children at increased cardiometabolic risk.
Burton also maintains that curves for (fat mass)/height3 are preferable to FMI because they more closely resemble those for percentage body fat (%BF). The rationale for using %BF as the gold standard comparator is unclear, because he acknowledges that %BF fails to take into account the independent contributions of fat and lean body mass. The decrease in the median %BF for boys aged 11–17 y is likely a result of the rapid accumulation of lean body mass during puberty. The use of FMI and lean body mass index allows for the independent evaluation of fat and lean body mass, and thereby would allow for an individual who has accumulated excessive fat mass in addition to lean mass to be identified for screening. That same individual with high fat and lean body mass would be missed if %BF were used as the screening tool.
In summary, the letter by Burton underscores many of the challenges in analyzing body composition in children. Reference curves for lean body mass index and FMI for children and adolescents are now available, so that future body composition studies have a frame of reference with which to evaluate lean and fat mass relative to height and age. Interested clinicians and researchers may use an online calculator to convert dual-energy X-ray absorptiometry measures of whole-body fat and lean body mass into age- and sex-specific z scores (http://www.research.chop.edu/web/zscore/). It is our hope that the scientific community will use this reference data in future studies aimed at the assessment of body composition in diverse patient populations and its relation to health outcomes.
Acknowledgments
The authors had no conflicts of interest to disclose.
REFERENCES
- 1. Weber DR, Moore RH, Leonard MB, Zemel BS.. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am J Clin Nutr 2013;98:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Heymsfield SB, Heo M, Thomas D, Pietrobelli A.. Scaling of body composition to height: relevance to height-normalized indexes. Am J Clin Nutr 2011;93:736–40. [DOI] [PubMed] [Google Scholar]
- 3. Franklin M.. Comparison of weight and height relations in boys from 4 countries. Am J Clin Nutr 1999;70:157S–62S. [DOI] [PubMed] [Google Scholar]
- 4. Maynard LM, Wisemandle W, Roche AF, Chumlea WC, Guo SS, Siervogel RM.. Childhood body composition in relation to body mass index. Pediatrics 2001;107:344–50. [DOI] [PubMed] [Google Scholar]
- 5. Cole TJ.. Weight/heightp compared to weight/height2 for assessing adiposity in childhood: influence of age and bone age on p during puberty. Ann Hum Biol 1986;13:433–51. [DOI] [PubMed] [Google Scholar]
- 6. Metcalf BS, Hosking J, Fremeaux AE, Jeffery AN, Voss LD, Wilkin TJ.. BMI was right all along: taller children really are fatter (implications of making childhood BMI independent of height) EarlyBird 48. Int J Obes (Lond) 2011;35:541–7. [DOI] [PubMed] [Google Scholar]
- 7. Flegal KM.. Commentary: is there a best index of weight for height? Int J Epidemiol 2011;40:44–6. [DOI] [PubMed] [Google Scholar]
- 8. Frontini MG, Bao W, Elkasabany A, Srinivasan SR, Berenson G.. Comparison of weight-for-height indices as a measure of adiposity and cardiovascular risk from childhood to young adulthood: the Bogalusa heart study. J Clin Epidemiol 2001;54:817–22. [DOI] [PubMed] [Google Scholar]


