Supplemental Digital Content is available in the text.
Key Words: medication titration, hypertension, meta-analysis
Abstract
Background:
Medication titration has been used in home blood pressure (BP) control, with the expectation of enabling patients with hypertension to better manage their BP.
Objective:
The study goal was to estimate the effects of medication titration intervention in lowering the systolic blood pressure and diastolic blood pressure of patients with hypertension.
Methods:
The meta-analysis included randomized controlled trials on adults diagnosed with hypertension and BP≧130/80 mm Hg, having a medication-titration intervention, and using a home BP measurement. We systematically searched PubMed, CINAHL, Ovid-Medline, and the Cochrane Library, for studies published from 1997 to 2017. The quality of the studies was evaluated by the Modified Jadad scale. Statistical heterogeneity among the trials was evaluated using Q statistics and I2. Publication bias was assessed with the funnel plot and Rosenthal’s fail-safe N.
Results:
The meta-analysis included 4 studies randomizing 1335 participants. Medication-titration intervention significantly assisted hypertensive patients to improve BP control; systolic blood pressure was reduced by 6.86 mm Hg [95% confidence interval (CI), 4.80-8.93, P<0.0001] and diastolic blood pressure by 3.03 mm Hg (95% CI, 2.07-3.99, P<0.0001), did not significantly affect EQ-5D scores (mean difference, 0.02; 95% CI, −0.01 to 0.04, P=0.13).
Conclusions:
Our findings suggest home medication titration of antihypertensive medication for hypertensive patients significantly improved home BP control. However, the strategy did not enhance quality of life in patients with hypertension.
Hypertension affects ~40% of the adult population worldwide and is one of the leading causes of disease-related death and disability.1,2 In the United States, 1 in every 3 adults has hypertension;3 in Canada, ~1 in 4 adults is affected.4 In Taiwan, hypertension has been one of the top 10 causes of death for more than 10 years. In 2015, the death rate from hypertension was 23.6 per 10,000 people, compared to 8.3 per 10,000 people in 2005, indicating a significant increase in death due to hypertension in the past 10 years.5 It is estimated that the percentage of the global population suffering from hypertension will increase to 29.2% in 2025.6 Effective control of blood pressure (BP) can lower the incident rate of cerebrovascular accidents by 35%–40%, myocardial infarctions by 20%–25%, and heart failures by 50%.7
Uncontrolled BP not only causes target organ damage,4 but also influences patients’ quality of life (QoL).8,9 Home BP monitoring can be used to assess the treatment responses in patients with hypertension.10 The findings of a meta-analysis showed that home BP monitoring combined with other strategies resulted in more effective and lasting impact on home BP control, and medication titration is one of these strategies.11
Medication titration is a novel strategy, which allows patients or medical professionals to adjust their medicine (additional, maintain, or decrease dose) depending on a medication titration plan.12 This strategy has been widely used to assist patients with asthma,13 diabetes,14 and those receiving long-term anticoagulant treatment to self-manage and adhere to their treatments.15 In recent years, medication titration has been used for BP control, with the expectation of enabling patients with hypertension to better manage their BP at home. The medication titration plan for hypertensive patients involves setting target BP, self-monitoring BP, and constructing a medication titration schedule.16 Each medication titration step is conducted based on the average home BP measurement readings.17 Several randomized controlled trials (RCTs) identified that medication titration strategy through a step-by-step approach can remind patients about their BP readings and target goals.16,18–20 The strategy filled the gap of patient’s insufficiency of the BP readings and target, which is one of the main causes of poor BP control.21 However, some studies has significantly decreased in systolic blood pressure (SBP) and diastolic blood pressure (DBP) between groups;16,19 some studies conversely.18,20
No meta-analysis has been conducted that examines the effects of medication titration on BP control. Therefore, the purpose of this systematic review and meta-analysis was to investigate the overall effectiveness of a medication titration strategy on lowering the SBP and DBP of patients with hypertension.
METHODS
This analysis followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).22
Search Strategy
We searched PubMed, CINAHL, Ovid-Medline, and the Cochrane Library, for studies published from 1997 to 2017. The keywords used were “blood pressure,” “hypertension,” “self-titration,” “medication-titration,” and “home-titration.” We also used Medical Subject Headings to identify the terminology of keywords.
Study Selection
Studies for review were included if they met the following criteria: (1) RCT; (2) subjects were adult patients with an existing diagnosis of hypertension by a physician, and BP≧130/80 mm Hg; (3) a medication-titration intervention was provided to the intervention group; (4) use of a home BP measurement; (5) written in English or Chinese; and (6) presented adequate data to calculate the effect size (eg, sample size, mean, SD, 95% confidence interval, and P-value).
Quality Assessment
The methodological quality of included studies was independently evaluated by 2 reviewers (C.W.K. and T.Y.C.) using the Modified Jadad scale.23 The scale includes 8 items: (1) Was the study designed as randomized? (2) Was the method of randomization appropriate? (3) Was the study designed as blind? (4) Was the method of blinding appropriate? (5) Was there a description of withdrawals and drop outs? (6) Was there a clear description of the inclusion and exclusion criteria? (7) Was the method used to assess adverse effects described? (8) Was the method of statistical analysis described? The questions are evaluated as yes (1-point) or no (0-point) for a maximum total score of 8. Scores higher than 4 points reflect favorable quality. Any disagreements between the 2 reviewers regarding the quality evaluation were resolved by discussion.
Data Extraction
C.W.K. and T.Y.C. independently reviewed full-text articles and extracted the data, which included authors, publication year, title of study, sample size of intervention and control groups, participants’ age, gender and body mass index, percentage of current smokers, comorbidity, baseline and post antihypertensive medicine dose, baseline and postintervention SBP and DBP, follow-up times and intervention context, and the scores of the State-Trait Anxiety Inventory (STAI-6) and the EuroQol 5 dimensions questionnaire (EQ-5D). The 2 reviewers discussed any inconsistency in the data they extracted to achieve consensus.
Data Analysis and Synthesis
This meta-analysis was conducted using Comprehensive Meta-Analysis version 2.0 software. The BP data were reported as the mean and SD in each original study. When necessary, we estimated SD from the 95% confidence intervals provided. Statistical heterogeneity among the trials was evaluated using Q statistics and I2. If I2>75%, high heterogeneity was indicated.24 On the basis of the findings of the heterogeneity analysis, we used a random-effects or fixed-effects model to pool data and estimate the overall effect.25 A fixed-effects model is based on the assumption that the sole source of variation in observed outcomes is that occurring within the study; that is, the effect expected from each study is the same. A random-effects model assume that each of the included trials may estimate a different treatment effect. Therefore, need to be taken into account the variance within trials and the variance between trials.
Potential publication bias was assessed with a funnel plot and Rosenthal’s fail-safe N. An asymmetrical funnel plot indicates publication bias.26 The Rosenthal’s method estimates the number of unpublished studies with a zero-effect size that would be needed to reduce the overall effect size to cause it become nonsignificant. If only a few studies are needed to negate the effect, publication bias should be considered. Conversely, if a large number of studies are needed to negate the effect, there is less reason for the consideration of publication bias.27
RESULTS
Characteristics of Included Trials
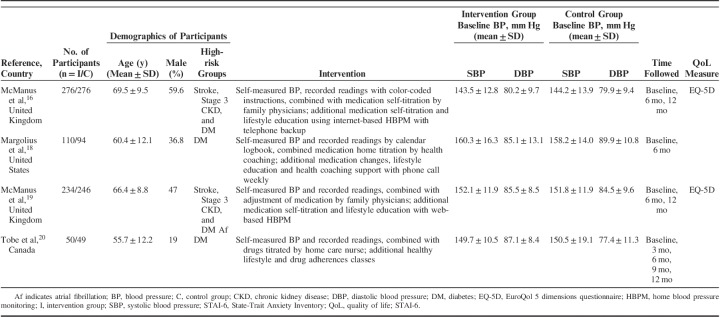
A PRISMA flow diagram (Fig. 1) illustrates the study selection process of clinical trials for the meta-analysis, based on the inclusion and exclusion criteria. In total, 50 titles and abstracts were identified through database screening, and 5 studies were found through hand searches. A total of 33 studies were removed due to duplication. Of the remaining 22 studies retrieved, we excluded 4 studies with a non-RCT design,17,28–30 4 due to study protocols, which were not present in the BP readings,31–34 1 study providing titration intervention for both arms,35 1 study recruiting patients with BP <130/80 mm Hg,36 1 study presenting an unclear titration plan,37 1 study reporting mean arterial pressure,15 and 6 commentary articles.38–43 Finally, we recruited 4 RCTs for meta-analysis (Table 1).16,18–20 These 4 studies included 1335 participants with hypertension; 670 and 665 patients were randomly assigned to the intervention and control groups, respectively. In the intervention group the pooled mean SBP at baseline was 149.72 (SD=12.99) mm Hg and DBP was 83.20 (SD=8.61) mm Hg. In the control group the pooled mean SBP at baseline was 149.45 (SD=13.67) mm Hg and DBP was 82.83 (SD=9.83) mm Hg.
FIGURE 1.
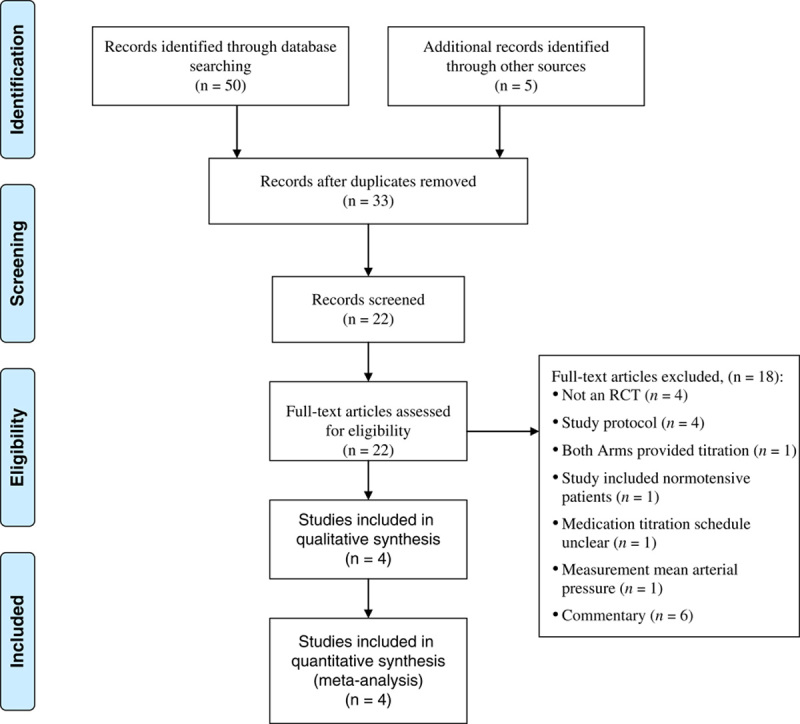
PRISMA flow diagram for the selection process of clinical trials for meta-analysis, showing inclusion and exclusion criteria, selection, and inclusion process. RCT indicates randomized controlled trial.
TABLE 1.
Characteristics of Participants and Interventions for Included Studies
We evaluated methodological quality of these 4 studies by using the 8-item Modified Jadad scale (eTable 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B700). The Jadad scores for these 4 studies were >4 points, which indicated favorable quality.23 Two studies evaluated received a score of 8.16,19 One study scored 5 points because it did not describe the double blinding, and did not report adverse effects.18 One study scored 6 points because it did not use the double-blind design.20
Effect on BP Control
We used a random-effects model for examining the effects of medication titration on SBP control because of the heterogeneity among trials (χ2=5.39, P=0.15; I2=44.29%). The pooled mean effect size of SBP was estimated as 6.86 [95% confidence interval (CI), 4.80-8.93; P<0.0001], a statistically significant difference between the intervention and control groups (Fig. 2). The results indicated that medication titration strategy significantly assisted hypertension patients to improve their SBP control.
FIGURE 2.
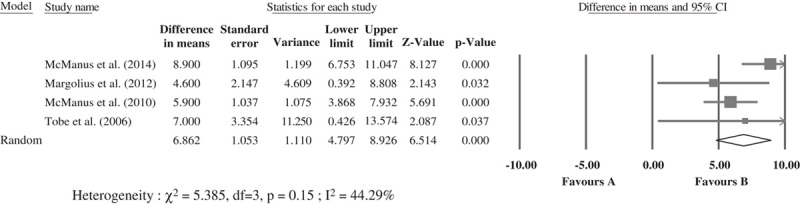
Forest plot of random-effects model for studies examining the effects of medication titration on systolic blood pressure between intervention and nonintervention groups: mean differences between groups. CI indicates confidence intervals.
Because no heterogeneity among trials in DBP was detected (χ2=1.24, P=0.74; I2=0%), we used a fixed-effects model to examine the effect of self-titration of medication on DBP control. The pooled mean effect size of DBP was estimated as 3.03 (95% CI, 2.07-3.99; P<0.0001), a statistically significant difference between the intervention and control groups (Fig. 3), indicating medication titration strategy also significantly improved DBP control in hypertensive patients.
FIGURE 3.
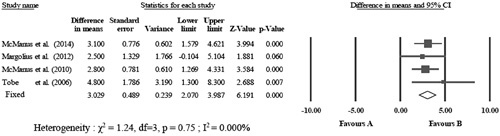
Forest plot of fixed-effects model on studies looking at the effect of self-titration of medication on diastolic blood pressure between intervention and nonintervention groups: mean differences between groups. CI indicates confidence intervals.
Effect on QoL
To examine the effect of medication titration strategy on improving QoL in patients with hypertension, we conducted a subgroup analysis of 2 RCTs that used the EQ-5D to evaluate QoL.16,19 We used the random-effects model to determine the effect of medication titration strategy on QoL because homogeneity was detected among trials (χ2=10.20, P=0.001; I2=90.19%). The pooled mean difference of EQ-5D scores was estimated as 0.02 (95% CI, −0.01 to 0.04; P=0.13) (Fig. 4), indicating no difference in improvement of QoL between hypertensive patients receiving or not receiving a medication-titration strategy.
FIGURE 4.
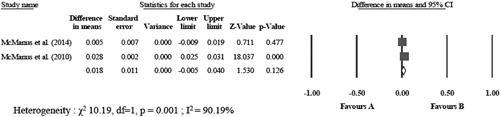
Forest plot of fixed-effects model for on studies looking at the effects of a medication titration strategy on quality of life. Mean differences in EQ-5D scores between intervention and nonintervention groups. CI indicates confidence intervals.
Publication Bias
The funnel plot of the 4 RCTs detected no severe publication bias (eFigure 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B700). The results of Rosenthal’s fail-safe N analysis showed that 91 studies with zero-effect would be needed to be published to render the mean effect size of SBP as nonsignificant. Visual inspection of the funnel plot for DBP also showed no severe publication bias and the findings of Rosenthal’s fail-safe N indicated that 34 studies with zero-effect would be needed to render the mean effect size of DBP as nonsignificant (eFigure 2, Supplemental Digital Content 1, http://links.lww.com/MLR/B700). These findings suggest that publication bias was unlikely to interfere with the explanation of the main results of this meta-analysis.
DISCUSSION
This meta-analysis contributes to knowledge about using a titration strategy for antihypertensive medication to improve home BP control in patients with hypertension. This the first meta-analysis to evaluate the effects of medication titration for home BP control. This meta-analysis provides evidence that using medication titration can significantly reduce SBP and DBP, but does not significantly improve QoL scores. These findings suggest that medication titration is beneficial for BP control in patients with hypertension; additionally, 3 studies reported no harmful events.16,19,20
The hypertensive patients in the 4 included studies were guided by a medication titration plan to control their home BP. The medication titration plan was comprised of setting home BP goals with medical professionals, measuring and monitoring home BP, and titrating antihypertensive medications according to their average home BP, either by the patient themselves16,19 or health care professionals.18,20 Both patients and medical professionals evaluated home BP readings and shared the decision-making for how to titrate the antihypertensive medications. The TASMINH2 trial compared with the control group, the intervention group had significantly more decreases in SBP by 3.7 mm Hg (95% CI, 0.8-6.6) and DBP by 1.3 mm Hg (95% CI, 0.3-2.6).19 The TASMIN-SR trial recruited high-risk patients compared with the control group, the intervention groups had significant differences in SBP 8.8 mm Hg (95% CI, 4.9-12.7) and DBP 3.1 mm Hg (95% CI, 0.7-5.5) at 12 months, respectively.
The patients who received the medication titration plan have to self-measure and report BP every day. The strategy of self-monitor BP increased reliability of BP values, absence of white-coat and masked hypertension, and a more accurate reflection of cardiovascular prognosis compared with BP readings completed at the clinic.33 Furthermore, a meta-analysis examining the effect of self-monitored BP at home on BP control reported that patients with self-monitoring BP at home had a significant decrease in both SBP and DBP at 6 months, compared with the patients without self-monitoring BP (weighted mean difference, 3.9 and 2.4 mm Hg, respectively). The authors suggested that home-based BP monitoring with co-intervention (eg, providing educational materials, tele-counseling, phone monitoring, or medication management with decision support) may achieve long-term efficacy on BP control.11 According to a previous qualitative study, the medication titration process can alert participants as to whether they are, or are not, on the right track.28 The researchers found when patients not only measured their own BP, but also understood the implications of the BP readings. Therefore, patients may engage in their disease management.16–20 The strategy of medication titration enhances patient motivation to take more responsibility to maintain better BP control.28 The medication titration strategy may also effectively influence patients’ behavior.44
In addition, all of the presented studies provided lifestyle modification education for the patients.16,18–20 The guidelines in American Heart Association for management of hypertension has identified lifestyle modification as a key to prevention and control of hypertension.45 Previous study suggested that the clinical professionals may provide the education through the internet for hypertension patients to modify their lifestyle and prevent long-term risk of cardiovascular diseases.46 The 4 studies also used internet-based system16,19 or telephone calls18,20 to follow-up patient safety and adherence.
There are some limitations to this meta-analysis. First, we found few recent RCTs which used medication titration for control of hypertension. Although we contacted many authors and conducted hand searches from the reference lists of all the collected articles, we were only able to include 4 RCTs, which fit the inclusion criteria and had adequate quality for this meta-analysis. Second, this meta-analysis showed no significant improvement in scores for QoL, which is most likely due to the small sample size resulting in low statistical power. One meta-analysis study indicated that patients with hypertension had a lower QoL for both physical and mental components (mean difference, −2.43; 95% CI, −4.77 to −0.08 and mean difference, −1.68; 95% CI, −2.14 to −1.23, respectively) compared with normotensive.47 Issues associated with how to improve QoL in patients with hypertension are important and, as such, require further investigation. Last, not all of the included studies had baseline data for anxiety status and medication dosages in hypertension patients, therefore, we cannot present subgroup analysis.
CONCLUSIONS
The results of this systematic review and meta-analysis provide evidence that medication titration could assist hypertension patients in controlling their SBP and DBP; however, there were no significant findings on QoL score. Medication titration is a novel home BP control strategy. We recommend that the health professionals be designated to assist hypertensive patients with managing their home BP through the use of medication titration in clinical practice.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
ACKNOWLEDGMENTS
The authors thank the Research Center for Testing and Assessment of the National Academy for Educational Research, Taiwan, and Associate Research Fellow Jin-Chang Hsieh for providing statistical consultation.
Footnotes
Present address: Ting-Yu Chen, MD and Chi-Wen Kao, PhD, No. 161, Section 6, Minquan East Road, Neihu District, Taipei City, Taiwan.
Present address: Shu-Meng Cheng, PhD, No. 325, Section 2, Chenggong Road, Neihu District, Taipei City, Taiwan.
Present address: Yue-Cune Chang, PhD, No. 151, Yingzhuan Road, Tamsui District, New Taipei City, Taiwan.
The authors declare no conflict of interest.
REFERENCES
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leung AA, Nerenberg K, Daskalopoulou SS, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension. Can J Cardiol. 2016;32:569–588. [DOI] [PubMed] [Google Scholar]
- 5.Ministry of Health and Welfare. 104 Annual cause of death statistic. Ministry of Health and Welfare. 2017. Available at: https://www.mohw.gov.tw/lp-3266-2.html. Accessed June 30, 2017.
- 6.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 7.Ogden LG, He J, Lydick E, et al. Long-term absolute benefit of lowering blood pressure in hypertensive patients according to the JNC VI risk stratification. Hypertension. 2000;35:539–543. [DOI] [PubMed] [Google Scholar]
- 8.Saleem F, Hassali MA, Shafie AA. A cross-sectional assessment of health-related quality of life (HRQoL) among hypertensive patients in Pakistan. Health Expect. 2014;17:388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y, Zhou Z, Gao J, et al. Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province, China. BMC Health Serv Res. 2016;16:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: Executive Summary. A joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Clin Hypertens (Greenwich). 2008;10:467–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uhlig K, Patel K, Ip S, et al. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–194. [DOI] [PubMed] [Google Scholar]
- 12.Zarnke KB, Feagan BG, Mahon JL, et al. A randomized study comparing a patient-directed hypertension management strategy with usual office-based care. Am J Hypertens. 1997;10:58–67. [DOI] [PubMed] [Google Scholar]
- 13.Powell H, Gibson PG. Options for self-management education for adults with asthma. Cochrane Database Syst Rev. 2003;1:CD004107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clar C, Barnard K, Cummins E, et al. Self-monitoring of blood glucose in type 2 diabetes: systematic review. Health Technol Assess. 2010;14:1–140. [DOI] [PubMed] [Google Scholar]
- 15.Levi M. Self-management of anticoagulation. Expert Rev Cardiovasc Ther. 2008;6:979–985. [DOI] [PubMed] [Google Scholar]
- 16.McManus RJ, Mant J, Haque MS, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312:799–808. [DOI] [PubMed] [Google Scholar]
- 17.Bobrie G, Postel-Vinay N, Delonca J, et al. Self-measurement and self-titration in hypertension: a pilot telemedicine study. Am J Hypertens. 2007;20:1314–1320. [DOI] [PubMed] [Google Scholar]
- 18.Margolius D, Bodenheimer T, Bennett H, et al. Health coaching to improve hypertension treatment in a low-income, minority population. Ann Fam Med. 2012;10:199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McManus RJ, Mant J, Bray EP, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376:163–172. [DOI] [PubMed] [Google Scholar]
- 20.Tobe SW, Pylypchuk G, Wentworthet J, et al. Effect of nurse-directed hypertension treatment among First Nations people with existing hypertension and diabetes mellitus: the Diabetes Risk Evaluation and Microalbuminuria (DREAM3) randomized controlled trial. CMAJ. 2006;174:1267–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Knight EL, Bohn RL, Wang PS, et al. Predictors of uncontrolled hypertension in ambulatory patients. Hypertension. 2001;38:809–814. [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oremus M, Wolfson C, Perrault A, et al. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement Geriatr Cogn Disord. 2001;12:232–236. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration, Version 5.1.0; 2011.
- 26.Littell JH, Corcoran J, Pillai V. Systematic Reviews and Meta-analysis. New York: Oxford University Press; 2008. [Google Scholar]
- 27.Rosenthal R. Meta-analytic Procedures for Social Research, Revised ed. London: Sage; 1991. [Google Scholar]
- 28.Grant RW, Pandiscio JC, Pajolek H, et al. Implementation of a web-based tool for patient medication self-management: the Medication Self-titration Evaluation Programme (Med-STEP) for blood pressure control. Inform Prim Care. 2012;20:57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor D, van der Merwe V, van der Merwe W. Nurse titration clinics to achieve rapid control of blood pressure. N Z Med J. 2012;125:31–40. [PubMed] [Google Scholar]
- 30.Kravetz JD, Walsh RF. Team-based hypertension management to improve blood pressure control. J Prim Care Community Health. 2016;7:272–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Brien C, Bray EP, Bryan S, et al. Targets and self-management for the control of blood pressure in stroke and at risk groups (TASMIN-SR): protocol for a randomised controlled trial. BMC Cardiovasc Disord [serial online]. 2013;13:21. Available at: BioMed Central. Accessed January 15, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McManus RJ, Bray EP, Mant J, et al. Protocol for a randomised controlled trial of telemonitoring and self-management in the control of hypertension: telemonitoring and self-management in hypertension. BMC Cardiovasc Disord [serial online]. 2009;9:6. Available at: BioMed Central. Accessed January 15, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Den Hond E, Staessen JA, Celis H, et al. Antihypertensive treatment based on home or office blood pressure--the THOP trial. Blood Press Monit. 2004;9:311–314. [DOI] [PubMed] [Google Scholar]
- 34.Bennett H, Laird K, Margolius D, et al. The effectiveness of health coaching, home blood pressure monitoring, and home-titration in controlling hypertension among low-income patients: protocol for a randomized controlled trial. BMC Public Health [serial online]. 2009;9:456. Available at: BioMed Central. Accessed January 15, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Staessen JA, Den Hond E, Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician’s office: a randomized controlled trial. JAMA. 2004;291:955–964. [DOI] [PubMed] [Google Scholar]
- 36.Watson AJ, Singh K, Myint-U K, et al. Evaluating a web-based self-management program for employees with hypertension and prehypertension: a randomized clinical trial. Am Heart J. 2012;164:625–631. [DOI] [PubMed] [Google Scholar]
- 37.Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy. 2000;2:1384–1389. [DOI] [PubMed] [Google Scholar]
- 38.Hill JR. Home blood pressure monitoring and self-titration of antihypertensive medications: proposed patient selection criteria. J Am Assoc Nurse Pract. 2016;28:277–281. [DOI] [PubMed] [Google Scholar]
- 39.Bosworth HB, Crowley MJ. Self-monitoring and self-titration of antihypertensive medication reduces systolic blood pressure compared with usual care. Evid Based Nurs. 2015;18:87. [DOI] [PubMed] [Google Scholar]
- 40.Steurer J. Arterial hypertension: blood pressure self-monitoring and self-titration of medications improves blood pressure readings. Praxis. 2014;103:1473–1474. [DOI] [PubMed] [Google Scholar]
- 41.Nilsson PM, Nystrom FH. Self-titration of antihypertensive therapy in high-risk patients: bringing it home. JAMA. 2014;312:795–796. [DOI] [PubMed] [Google Scholar]
- 42.Herrigel DJ, Willett LR. In hypertension with high CV risk, BP self-monitoring and medication self-titration reduced BP at 12 months. Ann Intern Med. 2015;162:JC7. [DOI] [PubMed] [Google Scholar]
- 43.Ogedegbe G. Self-titration for treatment of uncomplicated hypertension. Lancet. 2010;376:144–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fahey T, Schroeder K, Ebrahim S. Educational and organisational interventions used to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract. 2005;55:875–882. [PMC free article] [PubMed] [Google Scholar]
- 45.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 46.Kokubo Y. Prevention of hypertension and cardiovascular diseases: a comparison of lifestyle factors in Westerners and East Asians. Hypertension. 2014;63:655–660. [DOI] [PubMed] [Google Scholar]
- 47.Trevisol DJ, Moreira LB, Kerkhoff A, et al. Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens. 2011;29:179–188. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.