Abstract
Context
Exertional heat illnesses (EHIs) among football athletes have been widely researched, but data examining all collegiate sports are limited.
Objective
To describe the epidemiology of EHI in 25 National Collegiate Athletic Association (NCAA) sports.
Design
Descriptive epidemiology study.
Setting
The NCAA Injury Surveillance Program during the 2009–2010 through 2014–2015 academic years.
Patients or Other Participants
A voluntary sample of 166 NCAA institutions over 2048 team-seasons.
Main Outcome Measure(s)
Athletic trainers reported EHIs to the NCAA Injury Surveillance Program. Only EHIs sustained during a sanctioned practice or competition were included. The EHI rate, specific diagnoses, and number of emergency transports were measured.
Results
Overall, 232 EHI events were reported (0.47/10 000 athlete-exposures [AEs]; 95% confidence interval [CI] = 0.41, 0.53). Football comprised 75% of all EHI events and had the largest rate (1.55/10 000 AEs; 95% CI = 1.32, 1.78). The overall EHI rate was higher in preseason practices (1.16/10 000 AEs) than all other time periods (regular and postseason practices and all competitions; 0.23/10 000 AEs, injury rate ratio [IRR] = 4.96; 95% CI = 3.79, 6.50). This result was retained when examining the individual sports of football (3.65/10 000 versus 0.63/10 000 AEs, IRR = 5.82; 95% CI = 4.18, 8.10), men's soccer (1.11/10 000 versus 0.07/10 000 AEs, IRR = 16.819; 95% CI = 1.89, 138.55), and women's soccer (1.10/10 000 versus 0.05/10 000 AEs, IRR = 22.52; 95% CI = 2.77, 183.05). The EHI rates were highest in states with elevated annual temperatures (1.05/10 000 AEs). Heat cramps (39%), heat exhaustion (27%), and dehydration (29%) were the most common types of EHI. Nineteen athletes with EHI (8%) required emergency transport.
Conclusions
Football players continue to experience the most EHIs; however, EHIs can potentially occur in all NCAA sports. Continued emphasis on preseason EHI policies and institution-specific environmental guidelines is needed to address EHI rates.
Keywords: heat stroke, heat exhaustion, hyponatremia, exercise-associated muscle cramps, American football, emergency transport
Key Points
Football players experienced the most exertional heat illness (EHI) events compared with athletes in all other sports combined.
Exertional heat illnesses occurred in almost all National Collegiate Athletic Association sports.
The majority of EHI cases occurred during preseason practices. The states with the hottest average temperatures had the highest EHI rates.
The term exertional heat illness (EHI) encompasses a variety of distinct conditions, including exercise-associated muscle cramps (also known as heat cramps), heat exhaustion, heat syncope, and exertional heat stroke (EHS). Also included in this category are clinical concerns involving a variety of hydration levels, such as hypohydration and hyperhydration (ie, hyponatremia). Several groups1–6 have examined the epidemiology of EHI, with several providing EHI diagnoses. In these studies, exercise-associated muscle cramps accounted for 15% to 74% of EHIs, and exertional heat exhaustion, for 16% to 26% of cases.3–6 Exertional heat stroke had a lower prevalence in the epidemiology literature but was responsible for approximately 2% of all sport-related deaths7 and approximately 15% of all football deaths annually.8 A total of 61 football players died from EHS between 1995 and 2016, of whom 11 were collegiate athletes.9 Hypohydration is prevalent, especially in team sports.10 Clinical hyponatremia is predominantly reported in marathons or similar events but also exists in team sports.11 Each EHI has associated concerns involving participation-restriction time from sport, morbidity, and mortality, supporting the need for updated epidemiologic research to determine patterns and trends.
To address EHI incidence and predisposing factors, the National Collegiate Athletic Association (NCAA) mandated heat-acclimatization guidelines starting in 2003 and practice changes in 2017. In addition, EHI-prevention recommendations12,13 and hydration guidelines11,14 are available that teams and support staffs can implement. Despite guidelines and recommendations, the majority of EHIs occurred in the preseason1–6 and during practices.1,2 Few authors have directly compared practice and competition rates,1,2,4 with one group4 finding different results depending on the competition level.
Investigations of EHI have predominantly focused on football.3–6 Of these, Yeargin et al4 examined football at different competitive levels and found that collegiate players had the highest EHI risk, but not rate, as compared with youth and high school athletes. Yet when high school football was compared with other sports, the rate of EHI was approximately 11 times that of all other sports combined.2 Whether this holds true in the collegiate setting has not yet been determined. Studies analyzing EHI patterns across all organized sports have been conducted at the high school level or have been based on extrapolated emergency room data.1,2,15 Other than football, sports with the highest EHI rates were soccer, wrestling, basketball, track, and lacrosse.1,2,15 However, the EHI injury rate at the collegiate level is underexplored.
The epidemiology of EHI among adolescent sports and football athletes has been widely researched. However, data examining all collegiate sports do not exist. Therefore, the primary purpose of our study was to describe the epidemiology of EHI in 25 NCAA sports. The secondary purpose was to determine whether differences existed by sport, event, time in season, or temperate-state group.
METHODS
Research Design and Study Sample
A descriptive epidemiology design was used to examine EHIs across NCAA sports. Exposures of interest were event (ie, practices, competitions), time in season (ie, preseason, regular season, postseason), sport (ie, football, all others), and temperate-state groupings. Outcomes of interest were frequency of EHI, injury rate, type of EHI, participation-restriction time, and need for emergency transport.
The NCAA Injury Surveillance Program (NCAA-ISP) collected data from a convenience sample of member institutions across all 3 divisions (Football Bowl Subdivision and Football Championship Subdivision programs included). All 25 sports of the NCAA are represented in the surveillance program, and athletes, in general, were aged 18 to 23 years. The number of programs providing data varied by year and sport, but 166 institutions provided 2048 team-seasons.
Procedures and Outcome Measures
The NCAA-ISP prospectively collects data from institutions that voluntarily participate across all sports. Our data originated in the 2009–2010 through 2014–2015 academic years. The study was approved by the research review board of the NCAA. The methods using NCAA-ISP data have been described in detail previously16 but are also summarized below.
Athletic trainers (ATs) attended practices and competitions and collected data on athlete-exposures (AEs) and EHI incidents. An athlete-exposure was defined as 1 athlete participating in 1 NCAA-sanctioned competition or practice. Injuries were recorded in real time through the school's chosen electronic health-documentation system. Deidentified injury and exposure information were reported using an export application that extracts common data elements that are then aggregated for the NCAA-ISP.16 Exported data were verified by the application and flagged if inconsistencies were identified. Data were then reviewed by quality-assurance staff who worked with the ATs to resolve inconsistencies. Verified data were downloaded into the aggregate data set.
A reportable EHI had to have occurred as a result of participation in a school-sanctioned practice or competition. The AT provided a report on the EHI including the diagnosis, related circumstances, event type (practice or competition), time in season (preseason, regular season, postseason), and emergency transportation (needed, not needed). Exertional heat illnesses were also categorized by participation-restriction time (<24 hours, 1–6 days, 7–21 days, >21 days), the period during which the athlete was restricted from participation (ie, date of injury subtracted from the date of return). Non–time-loss (NTL) injuries were defined as restricting participation for <24 hours, and severe injuries were defined as those requiring >21 days of participation-restriction time or causing a premature end to the season (eg, medical disqualification). We included only EHI diagnoses as determined by the ATs or team physicians and categorized as (1) dehydration, (2) heat cramps, (3) heat syncope, (4) hyponatremia, (5) exertional heat exhaustion, or (6) EHS.
Because of the deidentified nature of the data provided to the research team, we were unable to compute state-specific EHI rates. However, with the assistance of the Datalys Center for Sports Injury and Prevention, Inc (Indianapolis, IN), which maintains the data, we obtained data that classified injuries and exposures into 3 categories based on state-specific average temperatures during the study period. Temperature data originated from the National Oceanic and Atmospheric Administration's National Centers for Environmental Information (Asheville, NC).17
Statistical Analysis
Exertional heat illness injury rates were calculated overall, by event type (practice, competition), by time in season (preseason, regular season, and postseason), by sport (football, all other sports), and by temperate-state tertiles (with tertile 1 being those states with the highest average annual temperatures during the study period). Descriptive analyses provided the injury frequencies and rates per 10 000 AEs. Injury rate ratios (IRRs) compared rates within sports by event type, time in season, and temperate-state grouping. Injury proportion ratios (IPRs) were used to compare proportions among groups. A priori, we focused such comparisons on proportions in (1) football preseason practices versus all other football time periods, (2) football preseason practices versus preseason practices in all other sports, and (3) preseason practices in all other sports versus all other time periods in all other sports. All other time periods were defined as regular season practices, postseason practices, preseason competitions, regular season competitions, and postseason competitions. Dehydration, heat syncope, and heat cramps were grouped as mild EHI; and heat exhaustion, hyponatremia, and EHS were grouped for statistical comparisons only. All 95% confidence intervals (CIs) not including 1.00 were considered significant. Data were analyzed using SAS-Enterprise Guide software (version 5.4; SAS Institute Inc, Cary, NC).
RESULTS
Overall Injury Rate and Rates by Sport
During the 2009–2010 through 2014–2015 academic years, a total of 232 EHI events occurred during 4 908 478 AEs recorded, resulting in an overall EHI rate of 0.47/10 000 AEs. No EHI events occurred in men's indoor track, lacrosse, outdoor track, swimming and diving, and tennis and women's gymnastics. The majority of EHIs were NTL (n = 82, 35%) or had participation-restriction time of 1 to 6 days (n = 141, 61%). The remaining EHI cases involved participation-restriction time of 7 to 21 days (n = 3, 1%) or were severe (n = 4, 2%). Football accounted for 75% of all EHIs reported and had a higher EHI rate than all other sports combined (IRR = 10.12; 95% CI = 7.52, 13.62).
Event Type, Time in Season, and Temperate-State Grouping
Most EHI events occurred during practices (72.8%, n = 169). However, the competition rate (0.70/10 000 AEs) was higher than the practice rate (0.42/10 000 AEs, IRR = 1.65; 95% CI = 1.23, 2.20; Table 1). Men's sports had a higher competition EHI rate, particularly in football, wrestling, basketball, and cross-country. Women's sports EHI rates did not differ between practices and competitions, but the majority of events occurred during practices (68%, n = 17). Among both men's and women's soccer players, EHI events occurred more often during practices. Football's EHI rate during practices was higher than that in all other sports combined (IRR = 12.16; 95% CI = 8.31, 17.79).
Table 1.
Exertional Heat Illness Counts and Rates Among Student-Athletes in 25 Sports by Event Type: National Collegiate Athletic Association Injury Surveillance Program, 2009–2010 Through 2014–2015
| Sport |
Count |
Rate per 10 000 Athlete-Exposuresa (95% CI) |
Injury Rate Ratio (95% CI): Practices Versus Competitions |
||||
| Practices |
Competitions |
Total |
Practices |
Competitions |
Total |
||
| Men's football | 136 | 38 | 174 | 1.34 (1.12, 1.57) | 3.47 (2.37, 4.58) | 1.55 (1.32, 1.78) | 2.59 (1.81, 3.71) |
| Men's wrestling | 1 | 2 | 3 | 0.11 (0.00, 0.32) | 1.83 (0.00, 4.36) | 0.29 (0.00, 0.61) | 17.14 (1.55, 189.08) |
| Women's field hockey | 0 | 1 | 1 | 0.00 | 0.85 (0.00, 2.51) | 0.20 (0.00, 0.60) | NA |
| Women's indoor track | 1 | 0 | 1 | 0.07 (0.00, 0.21) | 0.00 | 0.07 (0.00, 0.19) | NA |
| Women's lacrosse | 1 | 0 | 1 | 0.08 (0.00, 0.25) | 0.00 | 0.07 (0.00, 0.20) | NA |
| Women's outdoor track | 3 | 3 | 6 | 0.36 (0.00, 0.76) | 1.79 (0.00, 3.82) | 0.59 (0.12, 1.07) | 5.04 (1.02, 24.97) |
| Women's swimming and diving | 1 | 0 | 1 | 0.07 (0.00, 0.20) | 0.00 | 0.06 (0.00, 0.18) | NA |
| Women's tennis | 1 | 1 | 2 | 0.28 (0.00, 0.82) | 0.94 (0.00, 2.79) | 0.43 (0.00, 1.03) | 3.39 (0.21, 54.17) |
| Women's volleyball | 1 | 0 | 1 | 0.07 (0.00, 0.20) | 0.00 | 0.05 (0.00, 0.15) | NA |
| Men's baseball | 2 | 3 | 5 | 0.14 (0.00, 0.33) | 0.36 (0.00, 0.76) | 0.22 (0.03, 0.41) | 2.55 (0.43, 15.25) |
| Women's softball | 0 | 1 | 1 | 0.00 | 0.12 (0.00, 0.37) | 0.05 (0.00, 0.14) | NA |
| Men's basketball | 6 | 6 | 12 | 0.26 (0.05, 0.48) | 0.96 (0.19, 1.72) | 0.41 (0.18, 0.65) | 3.61 (1.16, 11.20) |
| Women's basketball | 2 | 0 | 2 | 0.10 (0.00, 0.25) | 0.00 | 0.08 (0.00, 0.19) | NA |
| Men's cross-country | 1 | 2 | 3 | 0.17 (0.00, 0.52) | 3.69 (0.00, 8.81) | 0.48 (0.00, 1.02) | 21.12 (1.92, 232.95) |
| Women's cross-country | 0 | 2 | 2 | 0.00 | 4.01 (0.00, 9.57) | 0.35 (0.00, 0.84) | NA |
| Men's ice hockey | 0 | 2 | 2 | 0.00 | 0.20 (0.00, 0.48) | 0.05 (0.00, 0.12) | NA |
| Women's ice hockey | 1 | 0 | 1 | 0.09 (0.00, 0.28) | 0.00 | 0.07 (0.00, 0.20) | NA |
| Men's soccer | 5 | 1 | 6 | 0.33 (0.04, 0.62) | 0.24 (0.00, 0.71) | 0.31 (0.06, 0.56) | 0.73 (0.09, 6.24) |
| Women's soccer | 7 | 1 | 8 | 0.34 (0.09, 0.60) | 0.15 (0.00, 0.45) | 0.30 (0.09, 0.50) | 0.45 (0.06, 3.64) |
| Men's sports overallb | 14 | 14 | 28 | 0.10 (0.05, 0.15) | 0.37 (0.18, 0.56) | 0.15 (0.10, 0.21) | 3.83 (1.83, 8.04) |
| Women's sports overallb | 17 | 8 | 25 | 0.14 (0.07, 0.21) | 0.24 (0.07, 0.41) | 0.16 (0.10, 0.23) | 1.72 (0.74, 3.99) |
| Overall totalc | 169 | 63 | 232 | 0.42 (0.36, 0.49) | 0.70 (0.52, 0.87) | 0.47 (0.41, 0.53) | 1.65 (1.23, 2.20) |
Abbreviations: CI, confidence interval; NA, not applicable.
One student-athlete participating in 1 practice or 1 competition.
Includes only sex-comparable sports (baseball and softball, basketball, cross-country, ice hockey, indoor track, lacrosse, outdoor track, soccer, swimming and diving, and tennis).
No exertional heat illnesses were reported in men's indoor track, lacrosse, outdoor track, swimming and diving, and tennis and women's gymnastics.
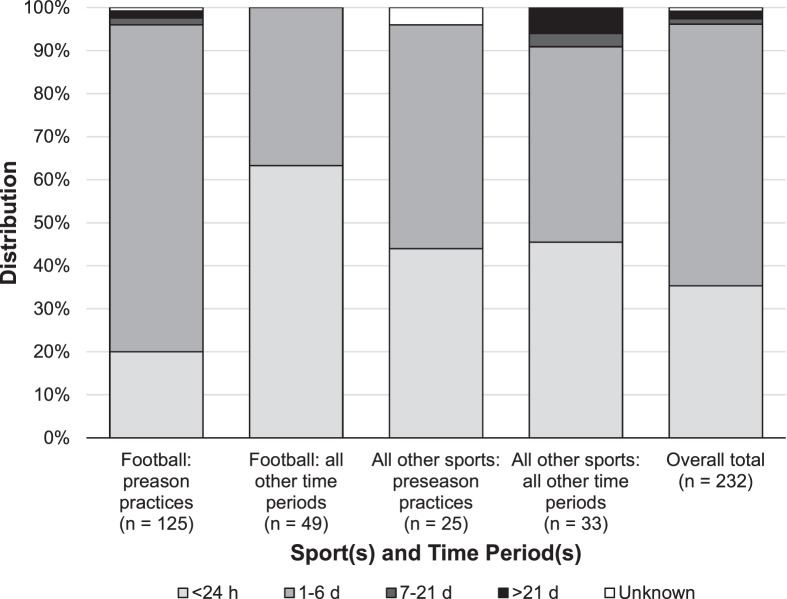
Most EHIs were reported in the preseason (64.7%, n = 150); half that number were reported in the regular season (32.3%, n = 75). The overall EHI rate was higher during preseason practices (1.16/10 000 AEs) than during all other time periods (0.23/10 000 AEs, IRR = 4.96; 95% CI = 3.79, 6.50; Table 2). This result was retained when we examined the individual sports of football and men's and women's soccer. Postseason rates were low (0.03/10 000 AEs; 95% CI = 0.01, 0.05) for all sports. The proportion of EHIs that resulted in NTL injuries (20.0%) during football preseason practices was lower than the proportion of EHI that resulted in NTL injuries during all other time periods in football (63.3%; IPR = 0.32; 95% CI = 0.21, 0.48) and during preseason practices in all other sports (44.0%; IPR = 0.45; 95% CI = 0.26, 0.80; Figure 1). Among all non-football sports, the proportion of EHIs that resulted in NTL injuries did not differ between preseason practices and all other time periods (IPR = 0.97; 95% CI = 0.54, 1.73). A total of 4 severe cases (ie, >21 days of participation restriction) of EHI were reported in the sample; 2 occurred during football preseason practices and 2 during the regular season in men's wrestling and women's outdoor track.
Table 2.
Exertional Heat Illness Counts and Rates Among Student-Athletes in 25 Sports by Time in Season: National Collegiate Athletic Association Injury Surveillance Program, 2009–2010 Through 2014–2015
| Sport |
Count |
Rate per 10 000 Athlete-Exposuresa (95% CI) |
Injury Rate Ratio (95% CI): Preseason Practice Versus All Other Time Periods |
||||||
| Practice |
Competition |
Preseason Practice |
All Other Time Periodsb |
||||||
| Pre |
Regular |
Post |
Pre |
Regular |
Post |
||||
| Men's football | 125 | 11 | 0 | 0 | 37 | 1 | 3.65 (3.01, 4.29) | 0.63 (0.45, 0.80) | 5.82 (4.18, 8.10) |
| Men's wrestling | 1 | 0 | 0 | 0 | 1 | 1 | 0.35 (0.00, 1.04) | 0.28 (0.00, 0.67) | 1.25 (0.11, 13.76) |
| Women's field hockey | 0 | 0 | 0 | 0 | 1 | 0 | 0.00 | 0.28 (0.00, 0.82) | NA |
| Women's indoor track | 1 | 0 | 0 | 0 | 0 | 0 | 0.14 (0.00, 0.40) | 0.00 | NA |
| Women's lacrosse | 0 | 1 | 0 | 0 | 0 | 0 | 0.00 | 0.10 (0.00, 0.30) | NA |
| Women's outdoor track | 1 | 1 | 1 | 0 | 2 | 1 | 0.42 (0.00, 1.24) | 0.74 (0.09, 1.39) | 0.56 (0.07, 4.83) |
| Women's swimming and diving | 0 | 1 | 0 | 0 | 0 | 0 | 0.00 | 0.09 (0.00, 0.26) | NA |
| Women's tennis | 1 | 0 | 0 | 0 | 1 | 0 | 0.96 (0.00, 2.84) | 0.29 (0.00, 0.84) | 3.36 (0.21, 53.79) |
| Women's volleyball | 1 | 0 | 0 | 0 | 0 | 0 | 0.21 (0.00, 0.63) | 0.00 | NA |
| Men's baseball | 0 | 1 | 1 | 0 | 2 | 1 | 0.00 | 0.33 (0.04, 0.63) | NA |
| Women's softball | 0 | 0 | 0 | 0 | 1 | 0 | 0.00 | 0.07 (0.00, 0.21) | NA |
| Men's basketball | 5 | 1 | 0 | 0 | 6 | 0 | 0.80 (0.10, 1.51) | 0.32 (0.08, 0.55) | 2.54 (0.80, 7.99) |
| Women's basketball | 1 | 1 | 0 | 0 | 0 | 0 | 0.19 (0.00, 0.56) | 0.05 (0.00, 0.16) | 3.56 (0.22, 56.95) |
| Men's cross-county | 1 | 0 | 0 | 0 | 1 | 1 | 0.87 (0.00, 2.57) | 0.43 (0.00, 1.03) | 2.02 (0.18, 22.25) |
| Women's cross-country | 0 | 0 | 0 | 0 | 2 | 0 | 0.00 | 0.46 (0.00, 1.10) | NA |
| Men's ice hockey | 0 | 0 | 0 | 0 | 2 | 0 | 0.00 | 0.05 (0.00, 0.13) | NA |
| Women's ice hockey | 1 | 0 | 0 | 0 | 0 | 0 | 0.55 (0.00, 1.64) | 0.00 | NA |
| Men's soccer | 5 | 0 | 0 | 0 | 1 | 0 | 1.11 (0.14, 2.08) | 0.07 (0.00, 0.20) | 16.19 (1.89, 138.55) |
| Women's soccer | 7 | 0 | 0 | 0 | 1 | 0 | 1.10 (0.29, 1.92) | 0.05 (0.00, 0.15) | 22.52 (2.77, 183.05) |
| Men's sports overallc | 11 | 2 | 1 | 0 | 12 | 2 | 0.25 (0.10, 0.40) | 0.13 (0.07, 0.19) | 2.02 (0.95, 4.31) |
| Women's sports overallc | 12 | 4 | 1 | 0 | 7 | 1 | 0.30 (0.13, 0.46) | 0.12 (0.05, 0.18) | 2.53 (1.15, 5.54) |
| Overall totald | 150 | 17 | 2 | 0 | 58 | 5 | 1.16 (0.97, 1.34) | 0.23 (0.18, 0.28) | 4.96 (3.79, 6.50) |
Abbreviations: CI, confidence interval; NA, not applicable; Post, postseason; Pre, preseason.
One student-athlete participating in 1 practice or 1 competition.
All other time periods include regular season practices, postseason practices, preseason competitions, regular season competitions, and postseason competitions.
Includes only sex-comparable sports (baseball and softball, basketball, cross-country, ice hockey, indoor track, lacrosse, outdoor track, soccer, swimming and diving, and tennis).
No exertional heat illnesses were reported in men's indoor track, lacrosse, outdoor track, swimming and diving, and tennis and women's gymnastics.
Figure 1.
Distribution of participation-restriction time for exertional heat illnesses among student-athletes in 25 sports: National Collegiate Athletic Association Injury Surveillance Program, 2009–2010 through 2014–2015. Note: All other time periods consists of regular season practices, postseason practices, preseason competitions, regular season competitions, and postseason competitions.
Most EHIs were reported in the temperate-state grouping with the highest average temperatures (45.7%, n = 106). The overall EHI rate was higher in temperate-state group 1 (1.05/10 000 AEs) than in temperate-state groups 2 and 3 combined (0.33/10 000 AEs, IRR = 3.16; 95% CI = 2.44, 4.10; Table 3). Findings were similar when stratified by sport and time in season.
Table 3.
Exertional Heat Illness Rates Among Student-Athletes in 25 Sports by Temperate-State Group: National Collegiate Athletic Association Injury Surveillance Program, 2009–2010 Through 2014–2015
| Temperate-State Groupa |
Rate per 10 000 Athlete-Exposuresb (95% Confidence Interval) |
||||
| Football Preseason Practices |
Football - All Other Time Periodsc |
All Other Sports - Preseason Practices |
All Other Sports - All Other Time Periodsc |
Total |
|
| 1 | 9.21 (6.93, 11.48) | 1.23 (0.70, 1.75) | 0.46 (0.17, 0.74) | 0.22 (0.09, 0.34) | 1.05 (0.85, 1.25) |
| 2 | 3.75 (2.60, 4.89) | 0.51 (0.22, 0.8) | 0.19 (0.04, 0.33) | 0.08 (0.02, 0.14) | 0.43 (0.33, 0.54) |
| 3 | 1.28 (0.73, 1.82) | 0.43 (0.22, 0.64) | 0.21 (0.07, 0.35) | 0.11 (0.05, 0.16) | 0.26 (0.20, 0.33) |
Temperate region: 1 (AR, AZ, DC, DE, FL, GA, HI, KS, KY, LA, MO, MS, NC, OK, SC, TN, TX), 2 (AL, CA, CT, IA, IL, IN, MD, NE, NJ, NM, NV, OH, RI, SD, UT, VA, WV), 3 (AK, CO, ID, MA, ME, MI, MN, MT, ND, NY, NH, OR, PA, VT, WA, WI, WY).
One student-athlete participating in 1 practice or 1 competition.
All other time periods included regular season practices, postseason practices, preseason competitions, regular season competitions, and postseason competitions.
Type of EHI and Emergency Transportation
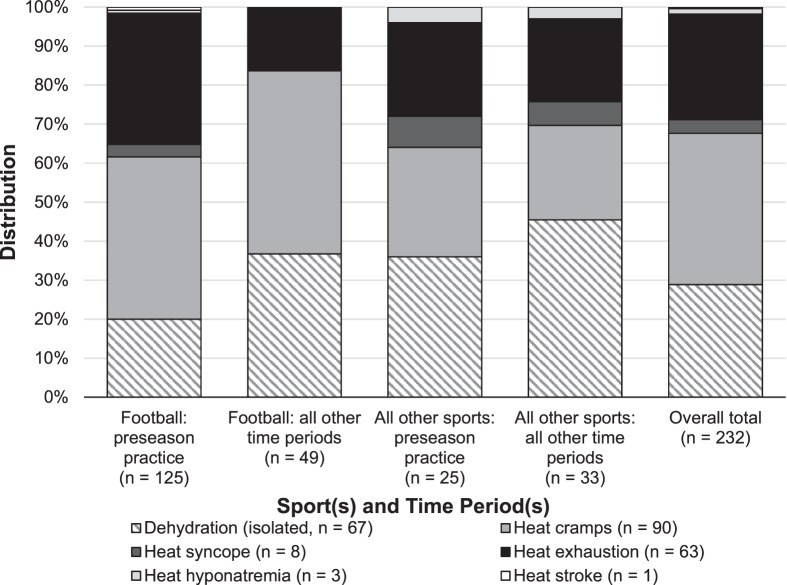
Heat cramps (38.8%), heat exhaustion (27.2%), and dehydration (28.9%) were the most common EHI types reported (Table 4). The proportion of heat exhaustion, EHS, and hyponatremia cases (35.2%) during football preseason practices was higher than that during all other time periods in football (16.3%; IPR = 2.16; 95% CI = 1.10, 4.24; Figure 2) but did not differ from that during preseason practices in all other sports (28.0%; IPR = 1.26; 95% CI = 0.64, 2.46). Among all non-football sports, the proportions of heat exhaustion, EHS, and hyponatremia cases did not differ between preseason practices and all other time periods (IPR = 1.16; 95% CI = 0.48, 2.76).
Table 4.
Exertional Heat Illness Diagnosis and Emergency Transports Among Student-Athletes in 25 Sports: National Collegiate Athletic Association Injury Surveillance Program, 2009–2010 Through 2014–2015, n (%)
| Sport |
Exertional Heat Illness Cases |
Cases Requiring Emergency Transport |
|||||
| Dehydration (Isolated) |
Heat Cramps |
Heat Syncope |
Heat Exhaustion |
Hyponatremia |
Heat Stroke |
||
| Men's football | 43 (24.7) | 75 (43.1) | 4 (2.3) | 50 (28.7) | 1 (0.6) | 1 (0.6) | 9 (5.2) |
| Men's wrestling | 2 (66.7) | 0 | 0 | 1 (33.3) | 0 | 0 | 1 (33.3) |
| Women's field hockey | 0 | 0 | 0 | 1 (100.0) | 0 | 0 | 0 |
| Women's indoor track | 0 | 0 | 0 | 1 (100.0) | 0 | 0 | 0 |
| Women's lacrosse | 0 | 0 | 1 (100.0) | 0 | 0 | 0 | 0 |
| Women's outdoor track | 3 (50.0) | 1 (16.7) | 0 | 2 (33.3) | 0 | 0 | 2 (33.3) |
| Women's swimming and diving | 1 (100.0) | 0 | 0 | 0 | 0 | 0 | 0 |
| Women's tennis | 0 | 1 (50.0) | 0 | 1 (50.0) | 0 | 0 | 0 |
| Women's volleyball | 0 | 1 (100.0) | 0 | 0 | 0 | 0 | 0 |
| Men's baseball | 0 | 2 (40.0) | 1 (20.0) | 1 (20.0) | 1 (20.0) | 0 | 1 (20.0) |
| Women's softball | 1 (100.0) | 0 | 0 | 0 | 0 | 0 | 0 |
| Men's basketball | 9 (75.0) | 3 (25.0) | 0 | 0 | 0 | 0 | 0 |
| Women's basketball | 1 (50.0) | 0 | 1 (50.0) | 0 | 0 | 0 | 0 |
| Men's cross-country | 1 (33.3) | 1 (33.3) | 0 | 0 | 1 (33.3) | 0 | 2 (66.7) |
| Women's cross-country | 1 (50.0) | 0 | 0 | 1 (50.0) | 0 | 0 | 1 (50.0) |
| Men's ice hockey | 1 (50.0) | 1 (50.0) | 0 | 0 | 0 | 0 | 1 (50.0) |
| Women's ice hockey | 1 (100.0) | 0 | 0 | 0 | 0 | 0 | 0 |
| Men's soccer | 1 (16.7) | 4 (66.7) | 0 | 1 (16.7) | 0 | 0 | 1 (16.7) |
| Women's soccer | 2 (25.0) | 1 (12.5) | 1 (12.5) | 4 (50.0) | 0 | 0 | 1 (12.5) |
| Total (% of total)a | 67 (28.9) | 90 (38.8) | 8 (3.4) | 63 (27.2) | 3 (1.3) | 1 (0.4) | 19 (8.2) |
% of total was calculated from 232 exertional heat illness events. Sports included in the analyses but with no reported cases of exertional heat illness were men's indoor track, lacrosse, outdoor track, swimming and diving, and tennis and women's gymnastics.
Figure 2.
Distribution of diagnoses for exertional heat illnesses among student-athletes in 25 sport-by-sport comparisons: National Collegiate Athletic Association Injury Surveillance Program, 2009–2010 through 2014–2015. Note: All other time periods consists of regular season practices, postseason practices, preseason competitions, regular season competitions, and postseason competitions.
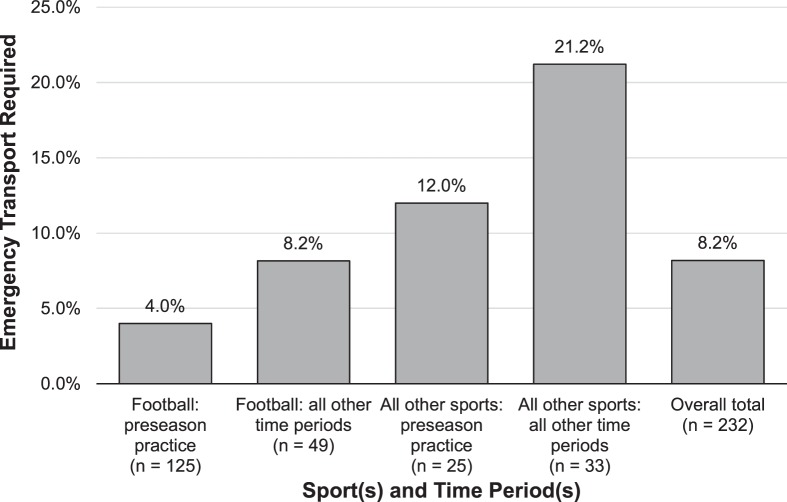
Nineteen patients with EHI (8%) required emergency transport: 9 in football and 2 each in men's cross-country and women's outdoor track and field. The diagnoses for those requiring emergency transport were dehydration (n = 7), heat cramps (n = 6), heat exhaustion (n = 5), heat syncope (n = 1), and hyponatremia (n = 1). The percentage of EHI patients requiring emergency transport varied during preseason football practices and for all other sports and all other time periods (Figure 3).
Figure 3.
Percentage of patients with exertional heat illnesses requiring emergency transport among student-athletes in 25 sport-by-sport comparisons: National Collegiate Athletic Association Injury Surveillance Program, 2009–2010 through 2014–2015. Note: All other time periods consists of regular season practices, postseason practices, preseason competitions, regular season competitions, and postseason competitions.
DISCUSSION
Overall Injury Rate and Sport
Although the overall rate of EHIs was low when compared with other injuries in collegiate athletes, EHS remained in the top 4 causes of death in this population,18 justifying the need to determine compliance with current policies and consider developing more policies based on injury-rate trends for EHI. Our data demonstrated higher rates of EHI in football than in all other sports, consistent with the high school level of play.2 Coupled with previous findings,4 continued concern and additional policies for this level of sport are recommended.
Most non-football sports (75%, n = 18) experienced an EHI event. Sports with relatively higher EHI rates were women's outdoor track, men's basketball, and men's and women's soccer. This is in contrast to sports at the secondary school level (ie, field hockey, lacrosse, volleyball, and wrestling).2 Soccer's sport dynamics—endurance play mixed with anaerobic spurts on large fields—could be a primary contributor. The basketball findings were surprising for an indoor sport given air conditioning and small courts. On further evaluation, the majority of basketball EHIs were isolated incidences of dehydration, which is consistent with previous research19 in the same population. If EHI prevention and treatment resources are not already in place, health care providers for outdoor track and soccer should use our data to support the need for more resources. Of the sports with no EHIs, those played in indoor venues can be logically explained. However, surprising results occurred in men's tennis, outdoor track, and lacrosse. This could be explained by the season in which they are played. Lacrosse is a spring sport (February through May), and outdoor track and tennis spread across fall and spring with a winter break (September through May). Health care providers for all sports should have prevention strategies and education plans in place to minimize the most prevalent EHIs in their sport.
The majority of EHIs resulted in 1 to 6 days of participation restriction from sport activities, consistent with previous research1 examining EHIs in high school athletes. The majority of EHI patients (ie, those with heat cramps, dehydration, or heat syncope) return to play within this time frame.13 The percentage of patients requiring 7 to 21 days before returning to sport (ie, those with more severe injuries) was lower than in the previously mentioned high school study (3% versus 13%).1 Collegiate health care teams minimize the number of athletes requiring moderate and severe participation-restriction time from EHI, possibly due to treatment interventions and more liberal return-to-play protocols. Health care providers working with patients recovering from EHI should remember that due to the nature of some conditions, certain athletes may require extended return-to-play time frames.
Event Type, Time in Season, and Temperate Region
Most EHI events occurred during practices, but the competition rate was larger than the practice rate. This difference is likely due to the greater number of practices overall and the higher intensities attributed to competition. Athletic trainers should be prepared for all types of EHIs in both event settings given that each requires a different logistical preparation. For example, in the practice setting, a cold-water immersion tub may be better situated as a permanent fixture on the practice field versus a competition with sideline restrictions. In contrast, competition situations may allow for more personnel to be on-site to aid in intravenous fluid treatments as compared with daily practices.
The current results were consistent with prior epidemiologic research2,6,15 that established the highest EHI rates occurring in the preseason. Our findings highlight the large magnitude of EHI differences between football preseason practices and all other time periods. Football's practice EHI rate was 11 times larger than that of all other sports combined. These data highlight the need to ensure that current policies aiming to reduce the rate of EHIs during practices in football are implemented correctly. At the high school level, only a small percentage of football programs (2.9%) fully complied with recommended EHI-prevention policies.20 Moreover, because our findings also suggest a larger relative rate of EHI events during preseason practices compared with other times in the season in additional sports such as men's and women's soccer, sport-specific heat-safety policies for those activities are needed because none currently exist.21 Adapting EHI prevention guidelines from football to these sports will provide an important foundation for safe participation.
To further explore the rate of EHI events, we examined injury rate by state groupings on the basis of average temperatures during the study period. This not only aligns our results with recent research suggesting that average state temperatures are associated with the incidence of EHI events22 but also promotes greater clinical applicability so that ATs can find meteorologic data17 and create state-specific guidelines for their institutions. It is not surprising that the group whose states reported the highest average temperatures had higher EHI rates than the other 2 groups. This finding was maintained when data were stratified by sport and time in season. Our epidemiologic study provides strong support for several meteorologic studies6,22,23 that have indicated the need for environmental conditions specific to the state and institution to be evaluated and used as a primary prevention intervention instead of a secondary strategy. From an injury-surveillance standpoint, acquiring data on institution-specific environmental conditions for each exposure would help provide better insight into the environment's role in EHI rates; however, this may increase the workloads of those individuals who serve as data collectors. Continued discussion on how to collect such data while not overburdening data collectors is warranted.
Types of EHIs and Emergency Transportation
Similar to our results, earlier researchers3,6 noted that the majority of collegiate EHIs reported by ATs were heat cramps or heat exhaustion. Current etiologic theories of heat cramps are weakly supported, but they are the primary focus of clinicians in athletic settings.24 Evidence-supported causes must be identified so that we can develop effective prevention methods. Hydration and sodium levels are contributing factors to heat exhaustion13 and hyponatremia.11 Assessments of hydration knowledge among collegiate athletes have not shown promising results,25,26 and educational interventions in this population are scarce.27 To avoid both clinical concerns, hydration education for athletes and support staff should be developed by each institution's health care providers.14 We encourage ATs to use the updated National Athletic Trainers' Association (NATA) position statement on fluid replacement14 to determine contemporary strategies for addressing these EHIs at their institutions. One case of EHS and 3 cases of hyponatremia were reported in our data set, but the National Center for Catastrophic Sports Injury Research28 noted more than 15 instances of EHS from schools not within the sample and no hyponatremia cases during the same time period. Of note, 3 patients lost 7 to 21 days of time and 4 lost >21 days. However, none of these were the reported EHS or hyponatremia cases in our sample. This provides a learning opportunity for readers to make sure they understand the nuances of different EHIs to accurately diagnose conditions. Updated standard definitions of these conditions are provided in the NATA position statement,13 and ATs should make sure they are using the correct term for the presentation of the EHI.
The need for emergency transport in the current study was higher than demonstrated by previous EHI researchers.4,29 Even though only 1 case of EHS was reported, 19 patients with EHI required emergency transport. Health care professionals commonly struggle to give an exact heat-related diagnosis, as noted in 52% of emergency room cases.15 The NATA recommended that EHS be determined via rectal temperature greater than 104°F (40°C) and central nervous system dysfunction.13 Yet few ATs used rectal temperature to assess patients with possible EHS.20 This could explain the difference between reported EHS cases and emergency medical services transports. Furthermore, 3 individuals with potentially life-threatening conditions in this study were not transported; the reasons are unknown. Continued efforts to implement the use of algorithms13 with accurate assessment equipment and improve knowledge of how to diagnose life-threatening EHIs are needed.
Exertional heat stroke, hyponatremia, and heat exhaustion occurred more often during preseason football practices than during all other time periods in the sport. However, emergency transports were few. This could be interpreted as ATs who provided care for football players being more prepared and comfortable managing EHI than ATs working with other teams. The number of emergency transports increased for all sports during all other time periods. Despite the knowledge that EHI can occur in “normal” regular season environmental conditions,13 there may be a perception of decreased risk. Regardless of season, ATs for all sports need appropriate resources available for managing EHI. The reported patient with EHS surprisingly did not require emergency transport, which deviates from NATA guidelines.13 Specific reasons emergency transport is used or not used for patients with EHI should be further examined to reduce unnecessary or missed transportation scenarios.
Current and Future Development of EHI Prevention-Related Policies
Additional best practices12,13 could be adopted via national or institutional policies and with regard to participation-restriction time to minimize the incidence of EHI. Areas for improvement could include the length of practice and environmental conditions. The majority of EHIs occur after 2 hours,2 but the current policy allows for 3-hour practices. The common denominator between football and soccer is the environmental condition in August. Exertional heat illnesses occur as environmental conditions rise above 82°F (28°C).3,5,6 Regional variations are important to consider; however, the region's mean and extreme deviations from it are the primary factors in EHS.22 Future policy changes should require schools to use a practice-modification table based on environmental conditions that adjusts length and break intervals but allows the school to use a region-specific table.
The NCAA Sports Medicine Handbook21 provides additional EHI prevention recommendations, but these are not included in the NCAA bylaws.30 No significant changes were made to the preseason guidelines until the recent (2017) elimination of 2-a-day practices. This change may help to minimize players' exposure to heat, and it highlights the value of injury-surveillance data in forming safety policy. Future comparisons of these sports will indicate whether elimination of 2-a-day practices in football was effective in lowering the EHI incidence. Yet higher EHI rates during the preseason were consistent across sports, and the recent rule change affects only football. Sport-specific guidelines should be clearly stipulated in the bylaws.
Limitations
Exertional heat illness was infrequent, which limited our ability to further examine sport-specific differences. Although our findings were consistent with previous research,1,2,4,5 the results from our convenience sample may not be generalizable to the entire collegiate student-athlete population or to other levels of competition. This is particularly important to note because our convenience sample may have demonstrated a distribution of EHI diagnoses that may not be generalizable to the population. To maintain the anonymity of institutions, we could not provide the sample's geographic breakdown. Given this anonymity, we assumed that each institution adhered to the national guidelines, but we do not know if institution-specific guidelines were followed. In addition, a standard definition of each EHI diagnosis was not provided; however, we relied on the expertise of the ATs supplying the data. Finally, the EHI data did not include environmental conditions and, therefore, what influence these conditions had on EHI rates is unknown. Future researchers should consider improving upon these limitations.
CONCLUSIONS
Particularly during preseason practices, football players continued to experience the most EHI cases compared with athletes in all other sports. Therefore, enhancing preseason EHI-prevention policies for football is warranted. Exertional heat illness can occur in almost all NCAA sports; thus, sport-specific policies that address EHI should encompass all fall sports. The states with the hottest average temperatures had the highest EHI rates. The NCAA and its institutions should develop region-specific environmental practice-modification guidelines.
ACKNOWLEDGMENTS
We thank the many ATs who have volunteered their time and efforts to submit data to the NCAA-ISP. Their efforts are greatly appreciated and have had a tremendously positive effect on the safety of student-athletes. We also thank the NCAA Sport Science Institute, particularly John Parsons, PhD, ATC.
REFERENCES
- 1.Yard EE, Gilchrist J, Haileyesus T, et al. Heat illness among high school athletes—United States, 2005–2009. J Safety Res. 2010;41(6):471–474. doi: 10.1016/j.jsr.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Kerr ZY, Casa DJ, Marshall SW, Comstock RD. Epidemiology of exertional heat illness among US high school athletes. Am J Prev Med. 2013;44(1):8–14. doi: 10.1016/j.amepre.2012.09.058. [DOI] [PubMed] [Google Scholar]
- 3.Cooper ER, Ferrara MS, Broglio SP. Exertional heat illness and environmental conditions during a single football season in the southeast. J Athl Train. 2006;41(3):332–336. [PMC free article] [PubMed] [Google Scholar]
- 4.Yeargin SW, Kerr ZY, Casa DJ, et al. Epidemiology of exertional heat illnesses in youth, high school, and college football. Med Sci Sports Exerc. 2016;48(8):1523–1529. doi: 10.1249/MSS.0000000000000934. [DOI] [PubMed] [Google Scholar]
- 5.Tripp BL, Eberman LE, Smith MS. Exertional heat illnesses and environmental conditions during high school football practices. Am J Sports Med. 2015;43(10):2490–2495. doi: 10.1177/0363546515593947. [DOI] [PubMed] [Google Scholar]
- 6.Cooper ER, Ferrara MS, Casa DJ, et al. Exertional heat illness in American football players: when is the risk greatest? J Athl Train. 2016;51(8):593–600. doi: 10.4085/1062-6050-51.8.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119(8):1085–1092. doi: 10.1161/CIRCULATIONAHA.108.804617. [DOI] [PubMed] [Google Scholar]
- 8.Boden BP, Breit I, Beachler JA, Williams A, Mueller FO. Fatalities in high school and college football players. Am J Sports Med. 2013;41(5):1108–1116. doi: 10.1177/0363546513478572. [DOI] [PubMed] [Google Scholar]
- 9.Kucera K, Klossner D, Colgate B, Cantu R. Annual Survey of Football Injury Research 1931–2016. Chapel Hill, NC: National Center for Catastrophic Sports Injury Research;; 2017. [Google Scholar]
- 10.Yeargin SW, Casa DJ, Judelson DA, et al. Thermoregulatory responses and hydration practices in heat-acclimatized adolescents during preseason high school football. J Athl Train. 2010;45(2):136–146. doi: 10.4085/1062-6050-45.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hew-Butler T, Loi V, Pani A, Rosner MH. Exercise-associated hyponatremia: 2017 update. Front Med (Lausanne) 2017;4:21. doi: 10.3389/fmed.2017.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Sports Medicine. Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–572. doi: 10.1249/MSS.0b013e31802fa199. [DOI] [PubMed] [Google Scholar]
- 13.Casa DJ, DeMartini JK, Bergeron MF, et al. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000. doi: 10.4085/1062-6050-50.9.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDermott BP, Anderson SA, Armstrong LE, et al. National Athletic Trainers' Association position statement: fluid replacement for the physically active. J Athl Train. 2017;52(9):877–895. doi: 10.4085/1062-6050-52.9.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson NG, Collins CL, Comstock RD, McKenzie LB. Exertional heat-related injuries treated in emergency departments in the US, 1997–2006. Am J Prev Med. 2011;40(1):54–60. doi: 10.1016/j.amepre.2010.09.031. [DOI] [PubMed] [Google Scholar]
- 16.Kerr ZY, Dompier TP, Snook EM, et al. National Collegiate Athletic Association injury surveillance system: review of methods for 2004–2005 through 2013–2014 data collection. J Athl Train. 2014;49(4):552–560. doi: 10.4085/1062-6050-49.3.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Climate indices: monthly atmospheric and ocean time series. National Oceanic & Atmospheric Administration Web site. 2018 http://www.esrl.noaa.gov/psd/data/climateindices/list Accessed August 5.
- 18.Adams WM, Casa DJ, Drezner JA. Sport safety policy changes: saving lives and protecting athletes. J Athl Train. 2016;51(4):358–360. doi: 10.4085/1062-6050-51.4.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thigpen LK, Green JM, O'Neal EK. Hydration profile and sweat loss perception of male and female Division II basketball players during practice. J Strength Cond Res. 2014;28(12):3425–3431. doi: 10.1519/JSC.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 20.Kerr ZY, Marshall SW, Comstock RD, Casa DJ. Implementing exertional heat illness prevention strategies in US high school football. Med Sci Sports Exerc. 2014;46(1):124–130. doi: 10.1249/MSS.0b013e3182a11f45. [DOI] [PubMed] [Google Scholar]
- 21.National Collegiate Athletic Association (NCAA) NCAA Sports Medicine Handbook. Overland Park, KS: NCAA;; 2015. Committee on Competitive Safeguards and Medical Aspects of Sports. [Google Scholar]
- 22.Grundstein AJ, Hosokawa Y, Casa DJ. Fatal exertional heat stroke and American football players: the need for regional heat-safety guidelines. J Athl Train. 2018;53(1):43–50. doi: 10.4085/1062-6050-445-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grundstein AJ, Ramseyer C, Zhao F, et al. A retrospective analysis of American football hyperthermia deaths in the United States. Int J Biometeorol. 2012;56(1):11–20. doi: 10.1007/s00484-010-0391-4. [DOI] [PubMed] [Google Scholar]
- 24.Miller KC. Rethinking the cause of exercise-associated muscle cramping: moving beyond dehydration and electrolyte losses. Curr Sports Med Rep. 2015;14(5):353–354. doi: 10.1249/JSR.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 25.Judge LW, Kumley RF, Bellar DM, et al. Hydration and fluid replacement knowledge, attitudes, barriers, and behaviors of NCAA Division I American football players. J Strength Cond Res. 2016;30(11):2972–2978. doi: 10.1519/JSC.0000000000001397. [DOI] [PubMed] [Google Scholar]
- 26.Torres-McGehee TM, Pritchett KL, Zippel D, Minton DM, Cellamare A, Sibilia M. Sports nutrition knowledge among collegiate athletes, coaches, athletic trainers, and strength and conditioning specialists. J Athl Train. 2012;47(2):205–211. doi: 10.4085/1062-6050-47.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rossi FE, Landreth A, Beam S, Jones T, Norton L, Cholewa JM. The effects of a sports nutrition education intervention on nutritional status, sport nutrition knowledge, body composition, and performance during off season training in NCAA Division I baseball players. J Sports Sci Med. 2017;16(1):60–68. [PMC free article] [PubMed] [Google Scholar]
- 28.Mueller P, Costo R. NCCSIR Annual Report (National Center for Catastrophic Sports Injury Research) Chapel Hill, NC: National Center for Catastrophic Sports Injury Research;; 2015. [Google Scholar]
- 29.Hirschhorn RM, Kerr ZY, Wasserman EB, et al. Epidemiology of injuries requiring emergency transport among college and high school student-athletes. J Athl Train. 2018;53(9):906–914. doi: 10.4085/1062-6050-340-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Collegiate Athletic Association (NCAA) NCAA Division I Manual. Overland Park, KS: National Collegiate Athletic Association;; 1997. [Google Scholar]