Abstract
Context
Emergency action plans (EAPs) are policies that improve response times and ensure access to emergency equipment for the management of patients with acute injuries and medical conditions, yet the extent to which EAP standards are adopted and implemented is unknown.
Objective
To describe the extent of EAP adoption and implementation in secondary school (SS) athletics with athletic trainer (AT) services in the United States.
Design
Cross-sectional study.
Setting
Web-based questionnaire.
Patients or Other Participants
A national sample of ATs (n = 9642) was invited to participate in a Web-based questionnaire.
Main Outcome Measure(s)
Twelve components of EAP minimum best practices were derived from the “National Athletic Trainers' Association (NATA) Position Statement: Emergency Planning in Athletics.” Emergency action plan components were analyzed using descriptive statistics with 95% confidence intervals (CIs) around proportions. Contingency tables (2 × 2) were used to calculate odds ratios (with 95% CIs) to assess adoption of the components (dichotomized as yes or no), employment factors (eg, full time versus part time, employed by clinic/district), and access to emergency equipment.
Results
The response rate for the questionnaire was 13.2% (n = 1273). A majority of ATs (89.1%) reported having an EAP; however, only 9.9% described implementing all 12 components cited in the NATA position statement. Athletic trainers stated that they created the EAP in 62.8% (95% CI = 60.1%, 65.4%) of schools with an EAP. Athletic trainers employed full time were at greater odds of adopting 9 or more components of the EAP compared with ATs employed part time (odds ratio = 2.42 [95% CI = 1.66, 3.53]). A total of 85.7% of ATs noted access to an automated external defibrillator.
Conclusions
Although a majority of SSs had EAPs, the EAPs were often incomplete and lacked the necessary components for full compliance with the NATA position statement. These findings demonstrate the need for efforts to promote the adoption and implementation of comprehensive EAPs in SS athletics.
Keywords: policies, preparedness, catastrophic injury, death
Key Points
Although a majority of athletic trainers (ATs) acknowledged having an emergency action plan, interventions are necessary to increase compliance with all components outlined in the “National Athletic Trainers' Association Position Statement: Emergency Planning in Athletics.”
Athletic trainers employed full time described adopting a larger number of components, further documenting the need for full-time ATs in secondary schools.
A majority of ATs stated they had access to an automated external defibrillator, yet efforts to improve access to additional emergency equipment, such as rectal thermometers, are warranted.
An estimated 7.8 million athletes participated in secondary school (SS) sports in the United States in 2014–2015, a number that has nearly doubled in the past 40 years.1,2 Unfortunately, the number of injuries sustained in SS sports has increased with participation. Between 1982 and 2015, 752 fatalities were reported among SS athletes, and some of these deaths might have been prevented if emergency action plans (EAPs) had been in place.2,3 Similar to the procedures for fire drills performed during the school day, EAPs are specific written procedures that can reduce fatalities among SS athletes.
Emergency action plans outline the step-by-step procedures that should take place in the event of a serious injury or acute medical concern. Appropriate procedures for the response to such events during participation in SS athletics were outlined in the “National Athletic Trainers' Association (NATA) Position Statement: Emergency Planning in Athletics.”4 This document lists the personnel (eg, athletic trainers [ATs], athletic directors [ADs], coaches, other administrators) central to the creation, rehearsal, and adoption of an EAP. However, despite published best-practice recommendations, the extent of adoption of all recommended components of EAPs in SS sports has not been extensively investigated. Researchers have reported on EAP adoption by SSs,5–10 but only 3 groups5,8,11 assessed the individual recommendations set forth by the NATA position statement.4 Olympia et al11 observed that 70% of SSs self-reported having a written EAP, yet 36% did not practice or rehearse the EAP.11 Olympia et al11 provided valuable benchmark data for EAP adoption; however, limitations of this study included a failure to address all components in the NATA position statement, such as whether the EAP identified and was distributed to all relevant athletics stakeholders (eg, ATs, ADs, coaches) and who aided in the creation of the EAP. Between 13% and 38% of responding schools had venue-specific plans in place, yet evidence for adoption of the other recommendations outlined in the NATA position statement is lacking.5,8
One recommendation outlined in the NATA position statement was that EAPs should incorporate medical personnel, such as ATs and emergency medical services, to carry out the plan. Johnson et al5 found that having an AT at the SS was associated with having a venue-specific EAP,5 indicating that the AT may be the person responsible for creating and updating the plan. However, whether the AT was primarily responsible for developing the EAP or other personnel assumed this role was unknown. Although a majority of ATs at SSs reported adopting an EAP,6,8–11 additional research is needed to evaluate how comprehensive these plans are as described by ATs and if a national approach to improve EAP adoption is warranted.
To date, no published data are available on the extent of SS EAP adoption of all recommendations set forth in the NATA position statement, which highlighted the latest evidence for improving health and safety preparations in sport. The purpose of our investigation was to assess the current adoption and implementation rates of the recommended EAP components in the “NATA Position Statement: Emergency Planning in Athletics”4 as reported by ATs.
METHODS
Setting
We used a cross-sectional questionnaire designed to assess the current level of emergency preparedness from data collected electronically from a national sample of SSs in the United States. This study was classified as exempt by the University of Connecticut Institutional Review Board.
Participants
Athletic trainers employed in the SS setting across the nation were invited to participate in this study. Athletic trainers were sent invitations to participate if they were members of the NATA or involved in the “Athletic Training Locations and Services Project.” We contacted only those who permitted e-mail contact for research purposes.
In May 2017, e-mails were sent to 9642 SS ATs inviting them to complete a Web-based questionnaire (Qualtrics, LLC, Provo, UT) regarding their school's emergency planning for athletics. One follow-up invitation was sent a week after the initial e-mail.
A total of 1445 questionnaires were started in the Qualtrics system. Incomplete questionnaires (those with fewer than 20% of questions completed) were removed, and the completion rate for returned questionnaires was 88.14%. A total of 1273 ATs completed more than 20% of the questionnaire, resulting in a response rate of 13.2%. The question with the lowest response rate was “My school posts the EAP” (n = 1012, response rate = 9.5%). We made no assumptions regarding null responses to a question and report all percentages based on the total number of responses to each question. The NATA District 2 had the largest percentage of respondents, and District 10 had the smallest percentage. The geographic distribution of responses by NATA district is presented in Table 1.
Table 1.
Geographic Locations of Responding Athletic Trainers
| National Athletic Trainers' Association District |
No. (%) |
| 1 | 109 (8.5) |
| 2 | 217 (17.0) |
| 3 | 183 (14.5) |
| 4 | 215 (16.9) |
| 5 | 76 (5.9) |
| 6 | 121 (9.5) |
| 7 | 73 (5.7) |
| 8 | 93 (7.3) |
| 9 | 129 (10.1) |
| 10 | 57 (4.5) |
| Total | 1273 (100) |
Procedures
We created the Web-based questionnaire to assess overall EAP policy adoption and evaluate the integration of the EAP-recommended components outlined in the “NATA Position Statement: Emergency Planning in Athletics.”4 Additional questions regarding demographic information, access to emergency equipment, involvement in creation of the EAP, and level and mode of employment were also included. Operational definitions of these variables are given in Table 2. Participants were asked to identify if they had adopted the 12 components outlined in the NATA position statement. Answer options regarding the inclusion of individual EAP components were yes adoption and no adoption.
Table 2.
Operational Definitions of Variables
| Categories of EAP adoption | |
| Adoption | Any response delineating the school had an EAP in general |
| 9+ components | Sum of respondents' adoption of EAP components (maximum = 12) Dichotomized into 2 groups: ≥9 components and ≤8 components |
| Possible determinants of EAP adoption | |
| Emergency equipment | Respondents were asked to check all equipment accessible to them Dichotomized into yes and no based on whether respondents indicated they had access |
| Included automated external defibrillator, splint kit, rectal thermometer, cold-water immersion tub, stethoscope, blood pressure cuff, oxygen, first-aid supplies, cardiopulmonary resuscitation mask, equipment-removal tools, pulse oximeter | |
| Mode of employment | Employed by district, outreach (ie, clinic, hospital), per diem |
| Level of employment | Full time: eg, “Athletic trainer services provided to only 1 school, 5 d/wk, 30 h/wk and 10 mo/y” |
| Part time: eg, “Anything less than full time” | |
| Creation of the EAP | Respondents were asked to identify who created the EAP at their school Options: (1) Themselves (2) Another member of the staff (3) They were not sure who created it |
Abbreviation: EAP, emergency action plan.
Questionnaire Validation
Before being disseminated, the questionnaire underwent a rigorous validation process including internal (within the research institution), external (ATs at local SSs not involved with the research team), and expert (professionals knowledgeable about preventing sudden death in sport across the domain areas of cardiac arrest, exertional heat stroke, traumatic brain injury, and cervical spine injury) content validity. A pilot study with 30 ATs was also conducted and concluded with follow-up phone interviews for the main purpose of identifying gaps in the questionnaire content. Revisions to the questionnaire were based on the interview findings, resulting in the final 40-question instrument.
Data Analyses
We summarized the EAP policy-adoption responses by providing the frequencies and percentages, as well as the means and standard deviations (for continuous data) associated with the adoption of each policy. The 95% confidence intervals (CIs) for the proportions of adoption were calculated to estimate the probability that a component was adopted. Adoption was operationally defined as the participant reporting the presence of a written policy.
In addition to evaluating the individual components of the EAP separately, participants were also categorized into complete adoption if all 12 components were scored as adopted. Participants were classified as high adoption if they reported adoption of 9 to 12 components and low adoption if they reported adoption of fewer than 9 components. Due to the lack of an evidence-based cutpoint, the 9 out of 12 score was used because a natural cut in the data was observed in the percentage of participants adopting various numbers of components. Specifically, 54.4% of participants reported adopting 9 or more of the 12 components, and 45.6% adopted fewer than 9 components.
Chi-square tests of association with odds ratios and 95% CIs were conducted to examine whether certain AT characteristics (eg, access to emergency equipment, employment status) were associated with the participant being classified as majority or complete adoption. Analyses were performed using SPSS (version 24; IBM Corp, Armonk, NY) with a significance level of .05.
RESULTS
Emergency Action Plan and Components Adoption
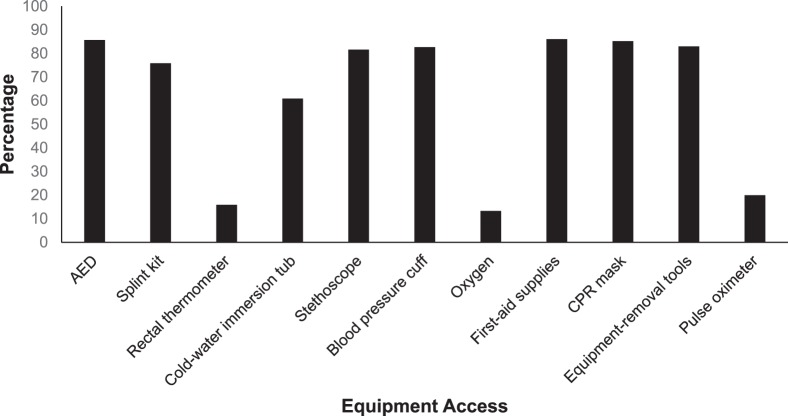
The data revealed that 89% of participants reported having an EAP present at their SS (Table 3). A total of 9.9% of ATs described the adoption of all 12 components and 54.4% indicated the adoption of 9 out of 12 components (Figure 1).
Table 3.
Emergency Action Plan (EAP) and Components Adoption
| Yes, My School _____ |
Athletic Trainers' Responses |
|
| % (n) |
95% Confidence Interval |
|
| Has a written EAP for managing serious and/or potentially life-threatening sport-related injuries. | 89.1 (1014/1138) | 87.3, 90.9 |
| Develops and coordinates the EAP with local emergency medical services, school public safety officials, onsite medical personnel or school medical staff, and school administrators. | 76.7 (790/1030) | 74.1, 79.3 |
| Distributes and reviews the EAP to all relevant athletics staff members annually. | 78.4 (808/1031) | 75.9, 80.9 |
| Rehearses the EAP annually with athletic trainers, athletic director, coaches, and other pertinent medical personnel. | 53.3 (549/1030) | 50.3, 56.3 |
| Updates the EAP annually by all relevant athletics staff members. | 78.3 (806/1029) | 75.8, 80.8 |
| Identifies the personnel and their responsibilities to carry out the plan of action with a designated chain of command. | 88.2 (909/1031) | 86.2, 90.1 |
| Identifies the location of on-site emergency equipment. | 90.2 (924/1024) | 88.4, 92.1 |
| Lists contact information for emergency medical services and other key personnel, as well as the facility address and location on the EAP. | 88.8 (909/1024) | 86.8, 90.7 |
| Provides recommendations for documentation that should be taken after a catastrophic injury. | 59.7 (610/1021) | 56.7, 62.8 |
| Includes information for health care professionals providing medical coverage included in the review and rehearsal of the plan. | 70.8 (726/1026) | 68.0, 73.5 |
| Has a venue-specific EAP. | 87.4 (890/1018) | 84.5, 89.4 |
| Posts the EAP at every venue. | 42.9 (434/1012) | 39.8, 45.9 |
Figure 1.
Percentage of respondents with number of components implemented in an emergency action plan.
Emergency Action Plan Creation
Of the ATs, 71% stated that they were involved in creation of the EAP (Table 4). Further, only 23.6% of ATs cited the principal or headmaster as being involved in creation of the EAP.
Table 4.
Roles Involved in the Creation and Updating of the Emergency Action Plan
| Role |
Percentage of Athletic Trainers Who Cited the Role as Being Involved in Emergency Action Plan Creation (95% Confidence Interval) |
| Principal or headmaster | 23.6 (21.2, 25.9) |
| Vice principal or assistant headmaster | 13.4 (11.6, 15.4) |
| Athletic director | 62.4 (59.7, 65.0) |
| Nurse | 20.8 (18.6, 23.0) |
| Athletic trainer | 71.7 (69.2, 74.2) |
| Strength and conditioning coach | 3.9 (2.9, 5.0) |
| Team physician | 25.1 (22.8, 27.5) |
Employment
Athletic trainers were employed full time (FT) by a school district (44.5%; 95% CI = 41.6%, 46.4%), FT by a clinic (33.9%; 95% CI = 31.2%, 36.6%, 7.4%), PT by a school district (5.4%; 95% CI = 4.1%, 6.7%), or per diem (0.5%; 95% CI = 0.1%, 0.9%). Those ATs at schools employing a FT AT were more likely to report adopting 9 or more EAP components than those at schools where ATs were employed PT (odds ratio [OR] = 2.42 [95% CI = 1.66, 3.53]). The ATs at schools contracting for an AT employed FT by a clinic were more likely to provide a list of contact information for emergency medical services and other personnel on their EAP (OR = 2.24 [95% CI = 1.33, 3.78]) and to include health care professionals responsible for medical care in the development and implementation of the EAP (OR = 1.64 [95% CI = 1.19, 2.27]) compared with ATs who had other types of employment. Athletic trainers employed FT by a school district implemented fewer than 9 components of an EAP (60.5%; 95% CI = 55.6, 65.4) compared with ATs employed by a clinic (39.5%; 95% CI = 34.6, 44.4, χ2 = 3.71, P = .05).
Access to Emergency Equipment
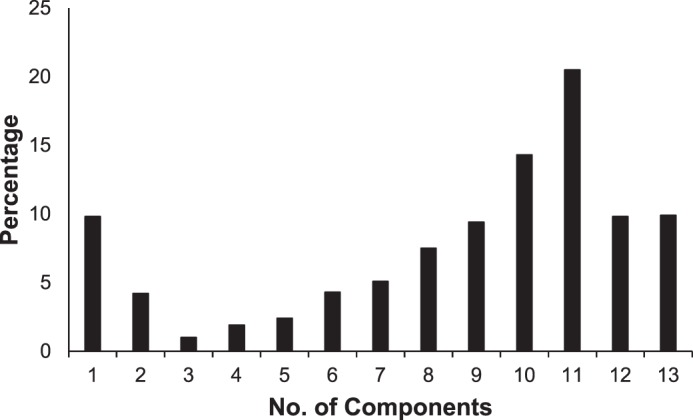
A majority of ATs described having access to vital emergency equipment such as an automated external defibrillator (AED; 85.7%), first-aid supplies (86.1%), and cardiopulmonary resuscitation mask (85.2%). The least available emergency equipment was a rectal thermometer (15.9%), oxygen (13.3%), and a pulse oximeter (20%; Figure 2). Athletic trainers who indicated implementing more than 9 components of EAPs were more likely to have access to a majority of the identified emergency equipment (Table 5). No other significant associations were observed (P values > .05).
Figure 2.
Athletic trainers' access to emergency equipment. Abbreviations: AED, automated external defibrillator; CPR, cardiopulmonary resuscitation.
Table 5.
Emergency Action Plan Component Adoption Associations With Emergency Equipmenta
| Schools With 9+ Components Were Associated With Having _____ |
χ2 Value |
P Value |
Odds Ratio (95% Confidence Interval) |
| Automated external defibrillator | 47.79 | <.001 | 9.13 (4.10, 20.35) |
| Splint kit | 38.57 | <.001 | 2.73 (1.97, 3.79) |
| Cold-water immersion tub | 61.90 | <.001 | 2.74 (2.19, 3.54) |
| Stethoscope | 56.64 | <.001 | 5.58 (3.41, 9.15) |
| Blood pressure cuff | 42.59 | <.001 | 4.67 (2.83, 7.70) |
| First-aid supplies | 46.76 | <.001 | 15.34 (5.40, 42.87) |
| Cardiopulmonary resuscitation mask | 45.61 | <.001 | 8.88 (4.19, 18.60) |
| Equipment-removal tools | 57.48 | <.001 | 6.92 (3.92, 12.20) |
No associations were observed between plan components and access to rectal thermometer, oxygen, and pulse oximeter.
DISCUSSION
The purpose of our investigation was to evaluate the current adoption of the recommendations outlined in the “NATA Position Statement: Emergency Planning in Athletics”4 in the SS setting. Among this sample, 9 out of 10 ATs reported having an EAP, a greater value than that described by Olympia et al.11 However, our data also offer evidence that only 1 out of 10 ATs in this sample were implementing all of the recommended components from the best-practices document, demonstrating a need to identify the reasons these recommendations were not adopted.
Emergency Action Plan Components Adoption
A majority of SS ATs reported adopting an EAP. Although this proportion was higher than previously described in the literature,5,6,8,9,12 it was closest to the proportion (75%) indicated by Harer and Yaeger.6 One explanation for the observed differences may be the variations in sample sizes and recruitment methods. For example, Olympia et al11 recruited via a paper questionnaire mailed through the US Postal Service to ATs, whereas our questionnaire was distributed electronically. Certain components were more frequently adopted than others. For example, most (87%) of the EAPs included venue-specific plans, but fewer than half of the ATs noted that the EAP was posted at each venue. Ensuring that the EAP is venue specific and posted for all stakeholders to reference in case of a catastrophic event allows for efficient and effective activation of the plan.3
Rehearsing the EAP familiarizes all potential responders with the plan and allows any deficiencies to be identified and addressed before a medical emergency occurs. However, fewer than half of the ATs surveyed reported rehearsing the EAP. A reason for not rehearsing the EAP may be a lack of understanding as to the importance of continued review. Reviewing and rehearsing the plan with all stakeholders in SS athletics is critical because the AT may not always be present at the time of a catastrophic injury. Recent data3 from fatal SS events suggested that appropriate medical services (eg, emergency medical services, ATs) were not present at 62% of the deaths. Therefore, ensuring enhanced memory recall through frequently practiced procedures for all stakeholders in an SS setting is crucial for efficient activation of the EAP, especially when medical services are not available.13,14 In brief, continued practice or rehearsal is needed, as knowledge quickly deteriorates if not used or updated regularly.15 This theory is supported by the literature on cardiopulmonary resuscitation retraining16–18 and hospital outcomes,19 which suggest a decay in knowledge and increased response time when action plans are not rehearsed. Similarly, fire drills are strategic plans developed to quickly evacuate a school or building in case of fire or emergency and are required of all faculty, staff, and students. Fire drills are often conducted every 1 to 3 months in SSs across the nation to ensure that all students and staff know their evacuation routes and assembly points. Investigators20 found that people in an organization gave different answers about their assembly points 3 months after a fire drill compared with the day after a drill. These school-based examples provide context for the continuing need to rehearse the EAP.
Our findings show that adoption of EAPs was almost 20% greater than noted by Olympia et al,11 who studied adoption of EAPs in a national sample of 521 ATs in 2005 and published their results in 2007. This improvement over time may be attributed to the change in athletic training accreditation standards and education competencies. The fourth edition of the Athletic Training Educational Competencies (released in 2005) stated that students should be able to “identify and describe basic component[s] of a comprehensive emergency plan,”21(p54) whereas the fifth edition of the standards (released in 2011) stated that students should be able to “develop comprehensive, venue-specific [EAPs] for the care of acutely injured or ill individuals.”22(p30) As such, the improvements in educational topics taught to students may have been effectively translated into this clinical finding. However, future researchers should investigate ATs' ages, years of experience, and educational levels as they relate to EAP adoption. Although a majority of our ATs described having an EAP for athletics, only 9.9% said the EAP contained all 12 of the recommended components. One reason for the disconnect between EAP adoption and a comprehensive EAP with all of the recommended components may be that ATs know they should have an EAP but lack awareness as to the specific components that should be included. Further changes to the educational curriculum and professional development opportunities should include the specific components and information on how to incorporate them into the AT's current EAP. Therefore, organizations such as the NATA, American College of Sports Medicine, National Federation of State High School Associations, and other groups that endorse best-practices documents should collectively develop strategies to promote the development of a comprehensive EAP at each SS. Educational efforts, including programs to help schools identify areas lacking in policy development and resources tailored to the current adoption and implementation of policies at the SS level, are warranted.
Emergency Action Plan Creation and Athletic Training Employment
Personnel described as being included or involved in creation of the EAP were ATs (72%), the AD (62%), and the team physician (25%). It is certainly important for the AD to be involved, but the team physicians' limited involvement is concerning. Given that recent researchers23 identified SS team physicians as helpful in improving strategies for preventing exertional heat illnesses, the lack of physician involvement in our study raises the question of the benefits a team physician would bring to EAP adoption. Increased presence and involvement of the team physician likely promotes planning and ensures that appropriate equipment is present in SSs.
Almost 80% of ATs in this sample stated they were employed FT. This finding is significantly more than the reported norm of 37%, but it may suggest that ATs employed FT were more likely to respond to the survey. Athletic trainers who were employed FT were more associated with adopting 9 or more components of EAPs than those who were PT. Those ATs employed full time have more hours at the school and thus likely have more time to dedicate to administrative duties such as EAP creation. However, ATs who are employed PT should be aware that their athletes do not have access to an AT on an FT basis; therefore, the potential for a catastrophic event to occur when the AT is not present is higher than when an AT is employed FT. As a result, ATs employed PT at SSs need to consider strategies to improve the EAP and confirm that a plan is in place for when the AT is not present.
Emergency Equipment
Our aim was not to evaluate treatment success in managing patients with catastrophic injuries, yet access to emergency equipment ensures that proper diagnosis is possible and appropriate treatment is available when needed. The majority of ATs stated they had an AED available for their SS athletics programs. This is promising given that, when AEDs are applied to patients within 1 to 3 minutes of collapse from cardiac arrest, survival rates are near 90%.24
In general, the availability of emergency equipment at the SSs for treating potential life-threatening emergencies requires improvement. When asked to “check all emergency equipment you have available to you,” only 86.1% of ATs indicated having access to first-aid supplies (described as gloves, gauze, etc). The least commonly available emergency equipment was rectal thermometers, oxygen, and pulse oximeters. Most notably, several documents25–29 have addressed the importance and validity of rectal temperature measurement compared with other devices when diagnosing athletes with possible exertional heat stroke. Only 15.9% of ATs reported access to a rectal thermometer, so we must be concerned about the ability to adequately assess SS patients with possible exertional heat stroke. Assessment of core body temperature along with vital signs such as heart rate, blood pressure, breathing rate, and blood oxygenation is imperative to determine the status of an athlete in distress; all such measurements are educational competencies for ATs.22 Obtaining vital signs using a pulse oximeter is an easy way to evaluate heart rate and blood oxygenation, both of which should be recorded when caring for an athlete experiencing an acute medical event. Along these lines, a small percentage of ATs cited access to supplemental oxygen. This finding, while not ideal, may indicate the lack of feasibility in providing ATs with access to supplemental oxygen. Despite the inclusion of the application of supplemental oxygen in the Education Competencies,22 the high cost, inconvenient storage, and lack of practicality for sideline use make access to oxygen a luxury only a few SSs can afford. For these reasons, the need for and feasibility of supplemental oxygen in SSs may warrant reevaluation as a recommendation.
Limitations and Future Research
As with most questionnaire research, we assumed participants were truthful in their responses. Additionally, an inherent response bias may have been present if those with EAPs were more likely to respond. Some respondents did not answer all questions; however, as more than 1000 ATs responded to each question, we are confident in our ability to draw conclusions. Still, we acknowledge that close to 80% of our respondents were FT ATs, which is significantly more than the 37% typically cited. Therefore, we caution against generalizing these data to the population of ATs, given differences in employment status. Our data were delimited by the decision to address the current level of emergency preparedness of SS athletics programs. Thus, our study addressed the current benchmark of EAP policy adoption in SS athletics, and our findings may not directly correlate with the preparedness of schools to adequately respond to a patient with a catastrophic injury. In other words, although the benchmark data provide insight into current EAP adoption as reported by ATs, we do not know if the implementation of all components from the best-practice statements relates to improved outcomes when responding to a patient with an emergent injury. Our aim was to evaluate the specific procedures outlined for athletics events, yet components of the EAP may be documented in a general school plan rather than an athletics-specific EAP. Therefore, components of overall school preparedness may or may not have been reflected in the current study responses, and future authors should investigate school community preparedness as it relates to athletics preparedness. We did not associate years of experience or educational level with EAP adoption; future researchers should consider whether these and other social determinants affect EAP adoption. Further, evaluation of ATs' knowledge of the Education Competencies22 as a potential factor influencing EAP adoption may be warranted. The possible creation of tailored strategies based on social determinants, facilitators, and barriers to EAP adoption in SSs should also be addressed.
CONCLUSIONS
Although a majority of ATs reported having an EAP at their schools, often the EAP was not comprehensive and lacked components such as rehearsal and public posting of the plan. Also, most ATs indicated they had access to most of the listed emergency equipment, but many cited limited access to rectal thermometers, supplemental oxygen, and pulse oximeters. Efforts to improve dissemination of the NATA position statement are needed to promote the development of comprehensive EAPs at all schools in order to minimize delays in the care of athletes requiring emergency treatment.
ACKNOWLEDGMENTS
This study was partially funded by the NATA Research & Education Foundation.
REFERENCES
- 1.Casa DJ, Almquist J, Anderson SA, et al. The inter-association task force for preventing sudden death in secondary school athletics programs: best-practices recommendations. J Athl Train. 2013;48(4):546–553. doi: 10.4085/1062-6050-48.4.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mueller FO, Kucera KL, Cox MS, Cantu RC. Catastrophic Sports Injury Research Thirty-First Annual Report: Fall 1982–Spring 2013 Vol 31. University of North Carolina at Chapel Hill: National Center for Catastrophic Sports Injury Research; 2015. p. 737. [Google Scholar]
- 3.Huggins RA, Olivadoti JM, Adams WM, et al. Presence of athletic trainers, emergency action plans, and emergency training at the time of sudden death in secondary school athletics. J Athl Train. 2017;52(suppl 6):S79. [Google Scholar]
- 4.Andersen J, Courson RW, Kleiner DM, McLoda TA. National Athletic Trainers' Association position statement: emergency planning in athletics. J Athl Train. 2002;37(1):99–104. [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson ST, Norcross MF, Bovbjerg VE, Hoffman MA, Chang E, Koester MC. Sports-related emergency preparedness in Oregon high schools. Sports Health. 2017;9(2):181–184. doi: 10.1177/1941738116686782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harer MW, Yaeger JP. A survey of certification for cardiopulmonary resuscitation in high school athletic coaches. WMJ. 2014;113(4):144–148. [PubMed] [Google Scholar]
- 7.Lear A, Hoang MH, Zyzanski SJ. Preventing sudden cardiac death: automated external defibrillators in Ohio high schools. J Athl Train. 2015;50(10):1054–1058. doi: 10.4085/1062-6050-50.8.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monroe A, Rosenbaum DA, Davis S. Emergency planning for sudden cardiac events in North Carolina high schools. N C Med J. 2009;70(3):198–204. [PubMed] [Google Scholar]
- 9.Toresdahl BG, Harmon KG, Drezner JA. High school automated external defibrillator programs as markers of emergency preparedness for sudden cardiac arrest. J Athl Train. 2013;48(2):242–247. doi: 10.4085/1062-6050-48.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wasilko SM, Lisle DK. Automated external defibrillators and emergency planning for sudden cardiac arrest in Vermont high schools: a rural state's perspective. Sports Health. 2013;5(6):548–552. doi: 10.1177/1941738113484250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olympia RP, Dixon T, Brady J, Avner JR. Emergency planning in school-based athletics. Pediatr Emerg Care. 2007;23(10):703–708. doi: 10.1097/PEC.0b013e318155adfc. [DOI] [PubMed] [Google Scholar]
- 12.Schneider DK, Grandhi RK, Bansal P, et al. Current state of concussion prevention strategies: a systematic review and meta-analysis of prospective, controlled studies. Br J Sports Med. 2017;51(20):1473–1482. doi: 10.1136/bjsports-2015-095645. [DOI] [PubMed] [Google Scholar]
- 13.Broomfield R. A quasi-experimental research to investigate the retention of basic cardiopulmonary resuscitation skills and knowledge by qualified nurses following a course in professional development. J Adv Nurs. 1996;23(5):1016–1023. doi: 10.1111/j.1365-2648.1996.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 14.Gross RD. Psychology:The Science of Mind and Behaviour 7th ed. Abingdon, UK: Bookpoint Ltd; 2015. [Google Scholar]
- 15.Kerr ZY, Dalton SL, Roos KG, Djoko A, Phelps J, Dompier TP. Comparison of Indiana high school football injury rates by inclusion of the USA Football “Heads Up Football” player safety coach. Orthop J Sports Med. 2016;4(5):2325967116648441. doi: 10.1177/2325967116648441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamilton R. Nurses' knowledge and skill retention following cardiopulmonary resuscitation training: a review of the literature. J Adv Nurs. 2005;51(3):288–297. doi: 10.1111/j.1365-2648.2005.03491.x. [DOI] [PubMed] [Google Scholar]
- 17.Sullivan N. An integrative review: instructional strategies to improve nurses' retention of cardiopulmonary resuscitation priorities. Int J Nurs Educ Scholar. 2015;12 doi: 10.1515/ijnes-2014-0012. [DOI] [PubMed] [Google Scholar]
- 18.Kaye W, Mancini ME. Retention of cardiopulmonary resuscitation skills by physicians, registered nurses, and the general public. Crit Care Med. 1986;14(7):620–622. doi: 10.1097/00003246-198607000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 20.Boyle T. Health and Safety: Risk Management Vol 21. Abingdon, UK: Routledge;; 2012. pp. 266–267. [Google Scholar]
- 21.Athletic Training Educational Competencies 4th ed. Dallas, TX: National Athletic Trainers' Association;; 2005. pp. 1–75. [Google Scholar]
- 22.Athletic Training Education Competencies 5th ed. Dallas, TX: National Athletic Trainers' Association;; 2011. pp. 1–34. [Google Scholar]
- 23.Pryor RR, Casa DJ, Yeargin SW, Kerr ZY. Sports medicine staff size influences exertional heat illness policies in high school football. Int J Athl Ther Train. 2018;23(4):172–177. [Google Scholar]
- 24.Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96(10):3308–3313. doi: 10.1161/01.cir.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 25.Huggins R, Glaviano N, Negishi N, Casa DJ, Hertel J. Comparison of rectal and aural core body temperature thermometry in hyperthermic, exercising individuals: a meta-analysis. J Athl Train. 2012;47(3):329–338. doi: 10.4085/1062-6050-47.3.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Casa DJ, Armstrong LE, Kenny GP, O'Connor FG, Huggins RA. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 2012;11(3):115–123. doi: 10.1249/JSR.0b013e31825615cc. [DOI] [PubMed] [Google Scholar]
- 27.Casa DJ, DeMartini JK, Bergeron MF, et al. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000. doi: 10.4085/1062-6050-50.9.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Casa DJ, Guskiewicz KM, Anderson SA, et al. National Athletic Trainers' Association position statement: preventing sudden death in sports. J Athl Train. 2012;47(1):96–118. doi: 10.4085/1062-6050-47.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Casa DJ, Stearns RL. Preventing Sudden Death in Sport & Physical Activity Vol 2. Burlington, MA: Jones & Bartlett Learning;; 2017. [Google Scholar]