Abstract
Study Objectives:
Little information is available regarding the effect of sleep on the development of chronic kidney disease (CKD). This large-cohort study aimed to investigate the association between sleep and the incidence of CKD.
Methods:
We recruited 194,039 participants without CKD aged 20 years or older between 1996 and 2014. Incident CKD was defined as an estimated glomerular filtration rate of < 60 mL/min/1.73 m2. Information about sleep duration and quality was obtained from a questionnaire and used to generate a score reflecting the sleep profile. Cox proportional hazards regression models were used to calculate the hazard ratio (HR) and 95% confidence interval (CI) for CKD associations with sleep duration, quality, and score categories.
Results:
Regarding sleep duration, participants who slept for fewer than 4 hours (HR 1.45, 95% CI 1.22–1.71), 4 to 6 hours (1.07, 1.02–1.14), or more than 8 hours (1.12, 1.04–1.21) had an increased risk of incident CKD, compared to those who slept 6 to 8 hours. Regarding sleep quality, participants who fell asleep but awoke easily (1.13, 1.07–1.19), had difficulty falling asleep (1.14, 1.06–1.22), or used sleeping pills or sedatives (1.14, 1.20–1.66) had a higher risk of incident CKD, compared to those who slept well. Furthermore, participants with sleep scores of 4 to 6 (1.07, 1.02–1.13) and less than 4 (1.61, 1.37–1.89) had an increased risk of incident CKD, compared to those with a sleep score higher than 6.
Conclusions:
A poor sleep profile is associated with increased risk of CKD development. Therefore, sleep duration and quality should be considered when developing strategies to improve sleep and thus prevent CKD.
Commentary:
A commentary on this article appears in this issue on page 371.
Citation:
Bo Y, Yeoh EK, Guo C, Zhang Z, Tam T, Chan TC, Chang LY, Lao XQ. Sleep and the risk of chronic kidney disease: a cohort study. J Clin Sleep Med. 2019;15(3):393–400.
Keywords: chronic kidney disease, eGFR, estimated glomerular filtration rate, sleep
BRIEF SUMMARY
Current Knowledge/Study Rationale: Increasing evidence suggests that a short sleep duration and poor sleep quality are associated with an increased risk of chronic kidney disease. However, information about the joint effects of sleep quality and duration on chronic kidney disease is limited.
Study Impact: Our study found an association of poor sleep with an increased risk of chronic kidney disease development. This finding underscores the need to consider sleep duration and sleep quality when developing strategies to improve sleep and thus prevent chronic kidney disease.
INTRODUCTION
Chronic kidney disease (CKD), which is defined as the loss of kidney structure and function,1 is a global public health issue. The Global Disease Burden study of 2015 estimated that CKD-associated deaths increased by 31.7%, from 0.9 to 1.2 million, between 2005 and 2015. In that study, CKD was ranked as the 17th leading cause of death worldwide.2 The burden of CKD includes not only costly renal replacement therapy, but also a poor quality of life, cardiovascular events and mortality, and all-cause mortality, resulting in signifi-cant social and economic burdens.3–5
Sleep is a basic human physiologic process, and health requires a sufficient amount and quality of sleep. Sleep has been reported to be associated with cardiovascular risks, including obesity, hypertension, and diabetes, which are also known risk factors for CKD.6–9 However, the underlying mechanisms for the association between sleep and incident CKD remain unknown. Sleep disorders might contribute directly to CKD development through activation of the sympathetic nervous system10,11 and/or indirectly through increased inflammation, which can lead to glomerular endothelial injury.12
Previous cross-sectional studies have investigated the relationship between sleep and the prevalence of CKD.13–16 However, few large-cohort studies have investigated the effects of sleep on CKD development. Moreover, although both sleep duration and quality are important factors related to CKD, most previous studies have focused on only one aspect. We therefore conducted a longitudinal cohort study to investigate the association between the sleep profile (including duration and quality) and the development of CKD in a population of 194,039 adults in Taiwan.
METHODS
Study Population
The participants were selected from a large prospective Taiwanese cohort, as described in previous publications.7,17–19 Briefly, more than 500,000 Taiwanese residents participated in a standard medical examination program conducted by the MJ Health Management Institution (Taipei, Taiwan) from 1996 to 2014. During each visit, participants underwent a series of medical examinations, including a general physical examination, blood and urine analyses, and a standard self-administered questionnaire survey. For each participant, the estimated glomerular filtration rate (eGFR) was calculated using the equation reported by the Modification of Diet in Renal Disease (MDRD) Study.20
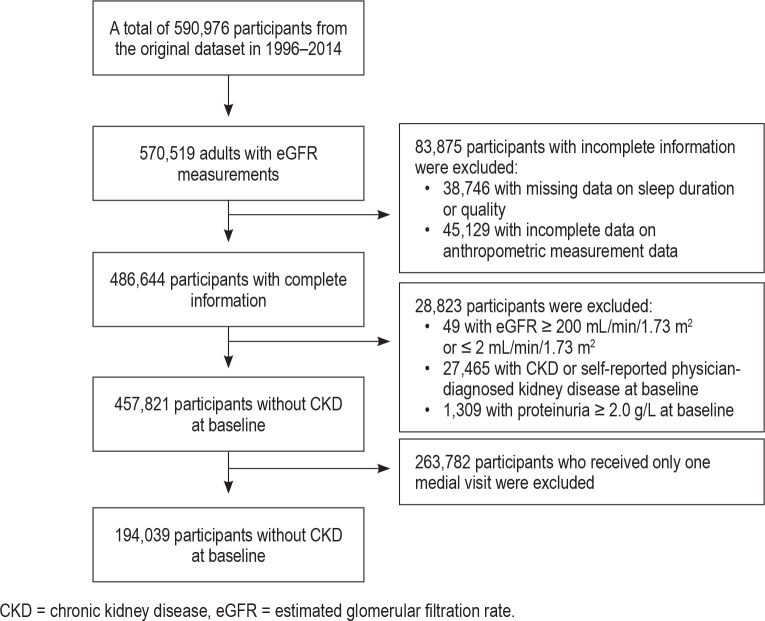
Figure 1 depicts the participant selection process. A total of 570,519 participants aged 20 years or older with available eGFR measurements were included between 1996 to 2014. Of these, 83,875 participants were excluded because of incomplete data (38,746 with missing data on sleep duration or quality and 45,129 with incomplete anthropometric measurement data). Of the remaining 486,644 participants, 28,823 were excluded for the following reasons: eGFR ≥ 200 mL/min/1.73 m2 or ≤ 2 mL/ min/1.73 m2, as these values suggest incorrect measurements due to technical error (n = 49); CKD (defined as an eGFR ≤ 60 mL/min/1.73 m2)21 or self-reported physician-diagnosed kidney disease at the initial visit (27,465); or proteinuria (urine protein ≥ 2.0 g/L), an important symptom of CKD, at their first visit (n = 1,309). Additionally, 263,782 participants were excluded because they participated in only one medical visit. Finally, 194,039 participants with 723,481 eGFR measurements were included in the analysis.
Figure 1. Flowchart of participant selection.
CKD = chronic kidney disease, eGFR = estimated glomerular filtration rate.
All participants provided written informed consent to authorize the use of data generated from the medical examination prior to joining the medical screening program. Personal identifying information was removed, and the data remained anonymous when released for research purposes. The Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee approved this study.
Sleep Profile Assessment
Slightly different questionnaires were used to collect information about sleep duration before 2009 and since 2009. Before 2009, the question “How many hours do you usually sleep each day?” was included. In 2009, this question was replaced with the question “How many hours do you usually sleep each night?” For both questions, the following four response options were provided: < 4, 4–6, 6–8, and > 8 hours. As a result, all participants were divided into four groups for analysis: < 4 hours, 4–6, 6–8, and > 8 h/d (Table S1 in the supplemental material).
Throughout the study period (1996–2014), information on sleep quality, including sleep latency, sleep disturbances, use of sleeping pills or sedative, and dreaming while sleeping was collected using the same question. Specifically, participants were asked “How did you evaluate your sleep situation last month?” and were asked to respond with one of the following five options: difficulty falling asleep, used sleeping pills or sedatives, excessive dreams while sleeping, could fall asleep but was easily awakened, and slept well (Table S1).
The sleep score, which comprised a combination of sleep quantity and quality, was used to reflect a participant's overall sleep profile. This score was calculated based on each sleep duration and quality category. For sleep quality, we assigned values of 5, 4, 3, 2, and 1 to the categories of slept well, fell asleep but was easily awakened, excessive dreams while sleeping, difficulty falling asleep, and used sleeping pills or sedatives, respectively. For sleep duration, we assigned values of 4, 3, 2, and 1 to the categories of 6–8, > 8, 4–6, and < 4 h/d, respectively. The sleep score was calculated using the following formula:
 |
The possible sleep scores ranged from 2 (worst) to 9 (best).
Outcome Ascertainment
A fasting blood sample was collected in the morning from each participant, and the serum creatinine level was measured using a Hitachi 7150 (Hitachi, Tokyo, Japan) before 2005 or Toshiba C8000 (Toshiba, Tokyo, Japan) device after 2005. The eGFR was calculated using the MDRD study equation as follows20:
 |
Serum creatinine values are reported in units of mg/dL.
The health outcome was incident CKD, which was defined as an eGFR < 60 mL/min/1.73 m2.21 As noted in the previous paragraph, participants with CKD (eGFR ≤ 60 mL/min/1.73 m2 or self-reported, physician-diagnosed kidney disease) at baseline were excluded. Incident CKD was thus identified via medical assessments in subsequent visits. The censoring point was either the first incidence of CKD or the final visit if CKD did not occur.
Covariates
Previous publications described the particulars of the medical examination program.7,17–19 Information about the participants' demographic characteristics, medical history, and lifestyle factors were collected using a standard self-administered questionnaire. Body mass index (BMI) was calculated as the weight (kg) divided by the square of the height (m2). The seated blood pressure was measured using a Citizen CH-5000 auto-sphygmomanometer (Citizen Systems Japan Co., Ltd., Tokyo, Japan). Total cholesterol and fasting glucose levels were analyzed using an automatic biochemical analyzer. Proteinuria was measured using a Roche Miditron/ROCHE Cobas U411 semiautomated computer-assisted urinalysis system (F. Hoff-mann-La Roche Ltd., Basel, Switzerland).
Statistical Analysis
Descriptive data are presented as mean (standard deviation) for continuous variables and number (percentage) for categorical variables. The person-years for each participant were calculated from the date of recruitment until the date of incident CKD or the final visit, if CKD did not occur.
The association between sleep and CKD development was assessed using the Cox proportional hazards regression method. Three models were developed. (1) A crude model with no adjustments. (2) Model 1 was adjusted for age (years), sex (male or female), smoking status (never, former, or current), alcohol consumption (seldom, < 1 time/wk; occasional, 1–3 times/ wk; or regular, > 3 times/wk), physical activity (seldom, < 1 h/wk; moderate, 1–2 h/wk; or frequent, > 2 h/wk), vegetable intake (seldom, < 1 serving/d; moderate, 1–2 servings/d; or frequent, > 2 servings/d), fruit intake (seldom, < 1 serving/d; moderate, 1–2 servings/d; or frequent, > 2 servings/d), BMI (kg/m2), fasting glucose (mg/dL), total cholesterol (mg/dL), systolic blood pressure (mmHg), diastolic blood pressure (mmHg), and baseline eGFR. (3) Model 2 was further adjusted for proteinuria (three levels, including negative, trace, and 1+ as individuals with a level of ≥ 2+ had been excluded). We used the results from Model 1 as our main model because protein-uria correlates with eGFR in patients with CKD.
We also conducted subgroup analyses and explored whether this association was modified by age (younger than 65 years or 65 years or older), sex (male or female), smoking status (never or ever), BMI (< 25 or ≥ 25 kg/m2), hypertension (systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, or self-reported, physician-diagnosed hypertension), diabetes (fasting blood glucose ≥ 126 mg/dL or self-reported, physician-diagnosed diabetes), and self-reported physician-diagnosed cardiovascular disease (yes or no). Each potential modifier was examined in a separate model by adding multiplicative interaction terms.
To test the stability of the associations, we conducted a series of sensitivity analyses. (1) We excluded participants followed up for less than 2 years because the effect of sleep on CKD is a chronic process. (2) We excluded individuals with hypertension, diabetes mellitus, or self-reported cardiovascular disease or cancer at baseline to eliminate the potential confounding effects of comorbidity. (3) We excluded participants enrolled since 2005 whose eGFR was measured using the Toshiba C8000 to avoid the potential measurement bias introduced by differences in analytical equipment. (4) To account for the introduction of a new question to collect sleep duration information in 2009, we excluded participants enrolled since 2009 to avoid the potential bias caused by the different questionnaires.
All statistical analysis was conducted in 2018 using SAS version 9.4 (SAS Institute Inc., Cary, North Carolina, United States). Two-sided values of P < .05 were considered statistically significant.
RESULTS
Participant Baseline Characteristics
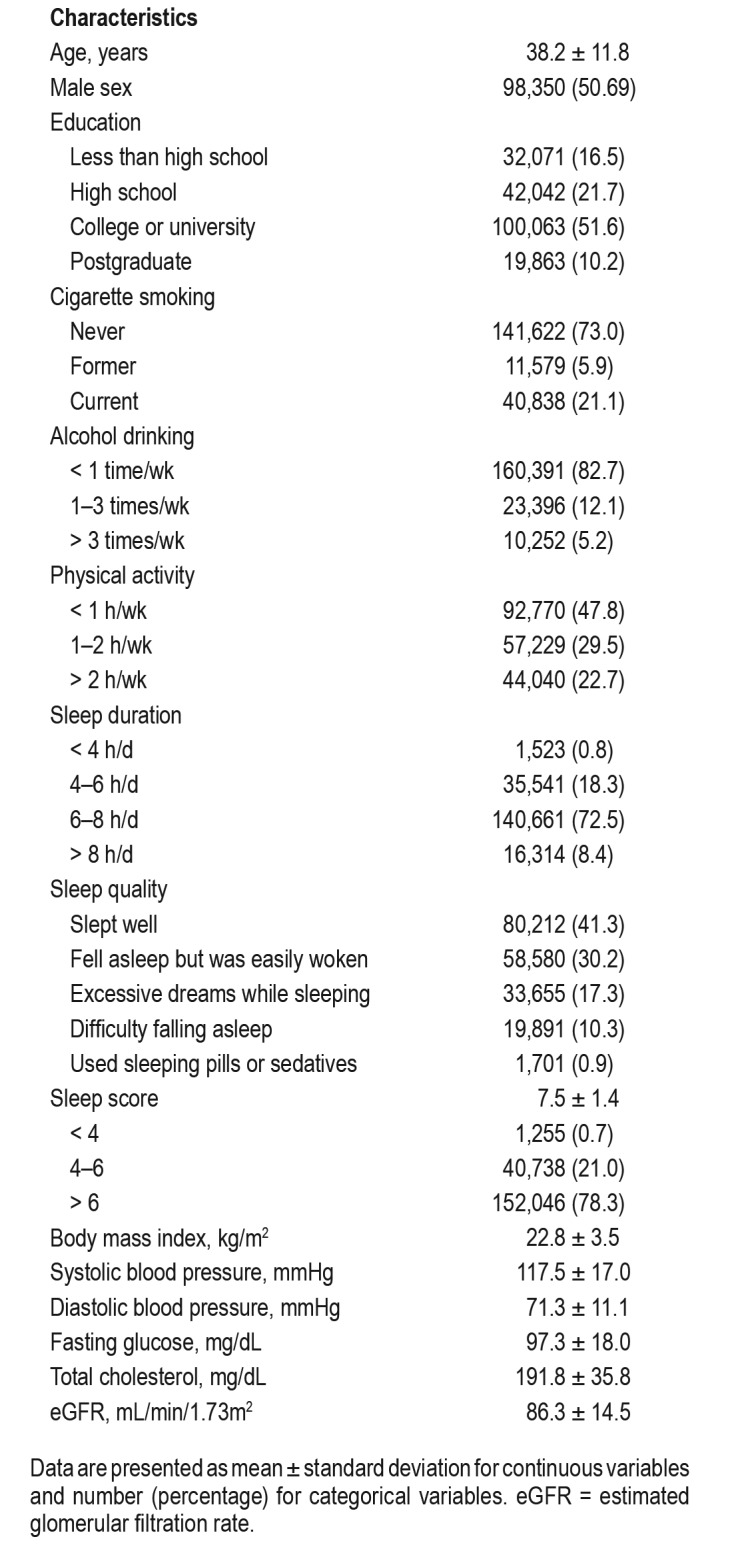
Table 1 presents the general characteristics of the participants. The study included 190,439 participants (50.69% men) with a mean age of 38.2 ± 11.8 years old at baseline. The mean follow-up duration was 5.56 ± 4.19 years, which yielded 1,058,685 person-years of follow-up. We identified 8,519 incident CKD cases during the follow-up period. The participants were generally well educated, and most were nonsmokers.
Table 1.
Baseline characteristics of the study participants (n = 194,039).
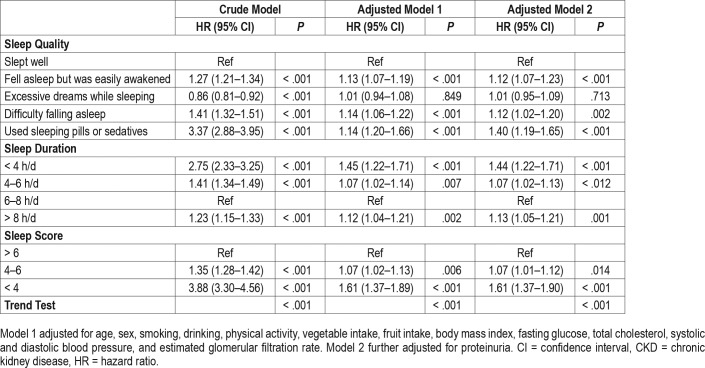
Association of Sleep and CKD Development
As shown in Table 2, we investigated the effects of the sleep quality, sleep duration, and sleep score on the risk of CKD development. Regarding sleep duration, participants who slept fewer than 4 hours (HR 1.45, 95% CI 1.22–1.71), 4 to 6 hours (1.07, 1.02–1.14), or more than 8 hours (1.12, 1.04–1.21) had an increased risk of incident CKD, compared to those who slept for 6 to 8 hours. For sleep quality, participants who fell asleep but were easily awakened (1.13, 1.07–1.19), had difficulty falling asleep (1.14, 1.06–1.22), and used sleeping pills or sedatives (1.14, 1.20–1.66) had a higher risk of CKD, compared to those who slept well. Regarding the sleep score, a combined indicator of sleep duration and quality, a lower value was significantly associated with a higher risk of incident CKD. Compared to participants with a sleep score higher than 6, those with sleep scores of 4 to 6 and less than 4 had an increased risk of CKD development.
Table 2.
Associations between sleep and incident CKD in Taiwanese adults.
Subgroup and Sensitivity Analyses
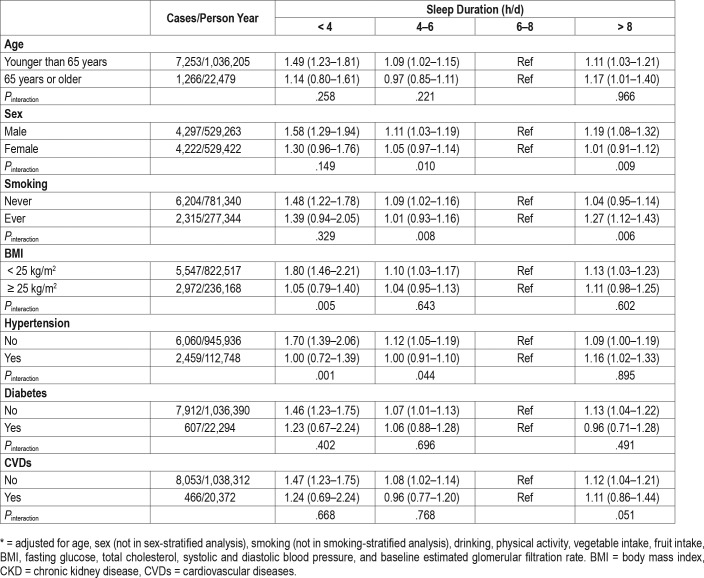
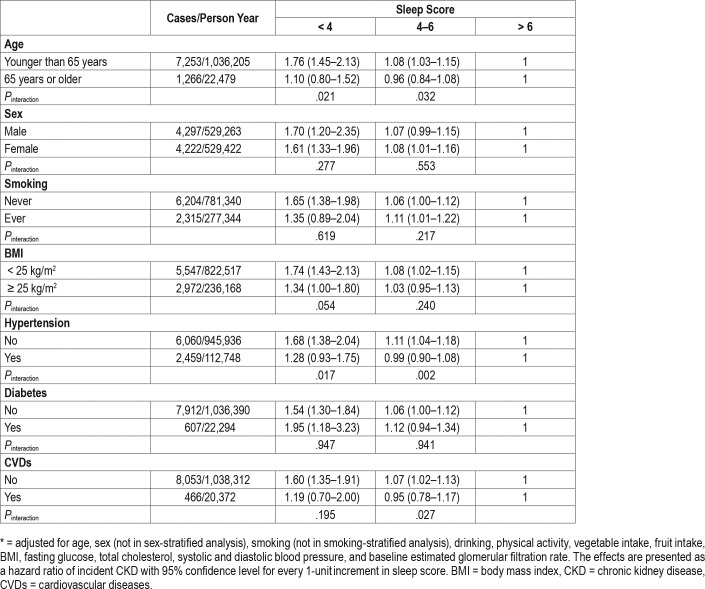
Subgroup analyses generally yielded similar results, although some differences did not reach statistical significance (Table 3, Table 4, and Table S2 in the supplemental material). Statistically significant interactions were observed for some factors, including BMI/hypertension and fewer than 4 hours of sleep, sex/smoking/hypertension and 4 to 6 hours of sleep, sex/smoking and more than 8 hours of sleep, age/hypertension/cardiovascular disease and the sleep score, sex and excessive dreams while sleeping, diabetes and difficulty falling asleep, age and the use of sleeping pills or sedatives. Table S3, Table S4, Table S5, and Table S6 in the supplemental material present the similar results of four sensitivity analyses.
Table 3.
Associations between sleep duration and incident CKD in Taiwanese adults in stratified analyses.*
Table 4.
Associations between sleep score and incident CKD in Taiwanese adults in stratified analyses.*
DISCUSSION
To the best of our knowledge, this is the first large-cohort study to investigate the effect of sleep on the risk of CKD development. We found a lower sleep score (ie, a poorer sleep profile, including the duration and quality of sleep) was associated with a higher risk of CKD development. Similarly, individuals who reported that they could fall asleep but were easily awakened, experienced difficulty falling asleep, reported the use of sleeping pills or sedatives, and/or had a short or prolonged sleep duration (6 or fewer hours; 8 or more hours) had a higher risk of CKD development.
The major strengths of this study are the cohort design and relatively long follow-up duration, which enabled us to investigate the effects of poor sleep on the development of CKD. Most previous studies used a cross-sectional design, and the authors could only demonstrate an association between sleep and the prevalence of CKD because this type of design could not exclude the potential of a reversed temporal association (ie, whether the poor sleep profile occurred before or merely accompanied CKD). Additionally, the large sample size allowed us to conduct subgroup analyses of participants stratified by BMI, hypertension, diabetes, and self-reported, physician-diagnosed cardiovascular diseases with the intent to eliminate the potential confounding/modifying effects of comorbidities. The large sample size also allowed us to conduct a series of sensitivity analyses. Both the subgroup and sensitivity analyses generally yielded similar results, indicating that the associations were robust. Moreover, we collected information about a wide range of potential confounders/modifiers and considered their potential effects. Finally, we considered the effects of both the duration and quality of sleep. In contrast to most previous studies, which focused on the effects of either sleep quality or sleep duration, we constructed a sleep score to reflect the joint effects of these factors.
Overall, data regarding the association between sleep and renal function/CKD were scarce and inconsistent. A previous cross-sectional study conducted in the United States reported that both short (6 hours or less) and long (8 hours or more) sleep duration were associated with a higher risk of prevalence of self-reported CKD, similar to our findings.16 In Korea, two cross-sectional studies reported that a very long (9 hours) sleep duration was associated with a higher risk of CKD.13,14 In contrast, a Japanese cohort study found no significant association of a long sleep duration (8 hours or more) with the risk of CKD, but did observe that a short sleep duration (5 hours) was associated with an increased risk of CKD among shift workers, but not all participants.22 Li et al. reported that a longer duration of attempted sleep (9 hours or more) was associated with an increased risk of rapid renal function decline,23 which further supported our findings.
Information on sleep quality and CKD is lacking. Bin demonstrated the importance of integrating sleep quality and duration in an examination of the independent and joint effects of these factors on health.24 A cross-sectional Chinese study demonstrated a significant association of poor sleep quality, but not sleep duration, with a high or very high risk of CKD.15
Our study design was similar to that of The Cancer Prevention Study II of the American Cancer Society,25 which also used a questionnaire to measure sleep duration. In that study, short or long sleep duration (fewer than 7 hours or more 7 hours) was associated with an increased risk of mortality. Several factors, such as population heterogeneity, different health outcomes, and different indicators of sleep quality, might make it difficult to compare our study directly with The Cancer Prevention Study II. Still, although the outcomes differed, both our study and The Cancer Prevention Study II reported the negative effects of a short or long sleep duration. Regarding sleep quality, Kripke et al. investigated the effects of insomnia and the use of sleeping pills but did not observe negative effects of insomnia.25
The underlying mechanisms linking sleep and CKD risk remain unknown. Disturbed sleep might lead to activation of the sympathetic nervous system,10 a well-known contributor to the development and progression of CKD.26 Another hypothesis suggests that sleep disorder-induced systemic inflammation may cause glomerular endothelial injury and proteinuria.12 Previous studies suggested that a short or prolonged sleep duration may promote systemic inflammation.27–29 Furthermore, higher levels of systemic inflammation might increase the risk of CKD development.30
This study had several limitations. First, a questionnaire was used to collect information about sleep, rather than objective measurements. However, the use of sleep monitoring devices to collect information would have been impractical in a large epidemiology study, given the high costs and logistical difficulties. Additionally, previous studies have reported a good correlation between self-reported and objective measurements.31,32 Second, we did not validate the questionnaire used in this study. Third, as noted previously, we changed the question used to obtain information about sleep duration in 2009 and therefore could not verify the total sleep duration per day for participants enrolled since 2009. We note that only a few adults may have taken afternoon naps; however, we could not determine the exact figure. A sensitivity analysis showed that this change to the questionnaire did not affect our conclusion. Fourth, objective information about obstructive sleep apnea, a cardiovascular risk factor, was not available and thus was not considered in this study. Fifth, our study population was generally well educated relative to the general Taiwanese population, indicating a better socioeconomic status. Therefore, the results should be generalized with caution. Finally, the construction of the sleep score was quite subjective. We assigned a value to each category of sleep duration and quality and although we were certain about the rank order of the categories, we did not know whether the differences between categories were proportionally equal.
In conclusion, we found that an abnormal sleep duration (6 hours or less; 8 hours or more), poor sleep quality, and lower sleep scores were associated with an increased risk of CKD development. This result indicates that the sleep duration and sleep quality should be considered when developing strategies to improve sleep and thus prevent CKD. Further studies of this issue that include objective measurements of sleep data and obstructive sleep apnea are warranted.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. This study was supported in part by the Environmental Health Research Fund of the Chinese University of Hong Kong (7104946). Yacong Bo and Cui Guo are supported by the PhD Studentship of the Chinese University of Hong Kong. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the MJ Health Research Foundation for authorizing our use of the MJ health data (Authorization code: MJHR2015002A). The interpretations or conclusions described in this paper do not represent the views of the MJ Health Research Foundation. This study was supported in part by the Environmental Health Research Fund of the Chinese University of Hong Kong (7104946). Yacong Bo and Cui Guo were supported by a PhD Studentship of the Chinese University of Hong Kong.
ABBREVIATIONS
- BMI
body mass index
- CI
confidence interval
- CKD
chronic kidney disease
- eGFR
estimated glomerular filtration rate
- HR
hazard ratio
- MDRD
Modification of Diet in Renal Disease
REFERENCES
- 1.Levey AS, Coresh J. Chronic kidney disease. Lancet. 2012;379(9811):165–180. doi: 10.1016/S0140-6736(11)60178-5. [DOI] [PubMed] [Google Scholar]
- 2.Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260–272. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 4.Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80(12):1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 5.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382(9889):339–352. doi: 10.1016/S0140-6736(13)60595-4. [DOI] [PubMed] [Google Scholar]
- 6.Wang F, Liu H, Wan Y, et al. Sleep duration and overweight/obesity in preschool-aged children: a prospective study of up to 48,922 children of the Jiaxing Birth Cohort. Sleep. 2016;39(11):2013–2019. doi: 10.5665/sleep.6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deng HB, Tam T, Zee BC, et al. Short sleep duration increases metabolic impact in healthy adults: a population-based cohort study. Sleep. 2017;40(10) doi: 10.1093/sleep/zsx130. [DOI] [PubMed] [Google Scholar]
- 8.Hermann D, Bassetti C. Role of sleep-disordered breathing and sleep-wake disturbances for stroke and stroke recovery. Neurology. 2016;87(13):1407–1416. doi: 10.1212/WNL.0000000000003037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dutil C, Chaput J. Inadequate sleep as a contributor to type 2 diabetes in children and adolescents. Nutr Diabetes. 2017;7(5):e266. doi: 10.1038/nutd.2017.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castro-Diehl C, Diez Roux AV, Redline S, et al. Sleep duration and quality in relation to autonomic nervous system measures: the multi-ethnic study of atherosclerosis (MESA) Sleep. 2016;39(11):1927–1940. doi: 10.5665/sleep.6218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petrov ME, Buman MP, Unruh ML, et al. Association of sleep duration with kidney function and albuminuria: NHANES 2009-2012. Sleep Health. 2016;2(1):75–81. doi: 10.1016/j.sleh.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamamoto R, Nagasawa Y, Iwatani H, et al. Self-reported sleep duration and prediction of proteinuria: a retrospective cohort study. Am J Kidney Dis. 2012;59(3):343–355. doi: 10.1053/j.ajkd.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 13.Kim C, Chang Y, Sung E, et al. Sleep duration and quality in relation to chronic kidney disease and glomerular hyperfiltration in healthy men and women. PLoS One. 2017;12(4):e0175298. doi: 10.1371/journal.pone.0175298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi H, Kim H, Lee J, Lee J, Choi D, Suh I. Sleep duration and chronic kidney disease: The Korean Genome and Epidemiology Study (KoGES)-Kangwha study. Korean J Intern Med. 2017;32(2):323–334. doi: 10.3904/kjim.2015.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li J, Huang Z, Hou J, et al. Sleep and CKD in Chinese adults: a cross-sectional study. Clin J Am Soc Nephrol. 2017;12(6):885–892. doi: 10.2215/CJN.09270816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salifu I, Tedla F, Pandey A, et al. Sleep duration and chronic kidney disease: analysis of the national health interview survey. Cardiorenal Med. 2014;4(3–4):210–216. doi: 10.1159/000368205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Z, Chang LY, Lau AKH, et al. Satellite-based estimates of long-term exposure to fine particulate matter are associated with C-reactive protein in 30 034 Taiwanese adults. Int J Epidemiol. 2017;46(4):1126–1136. doi: 10.1093/ije/dyx069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wen CP, Cheng TY, Tsai MK, et al. All-cause mortality attributable to chronic kidney disease: a prospective cohort study based on 462 293 adults in Taiwan. Lancet. 2008;371(9631):2173–82. doi: 10.1016/S0140-6736(08)60952-6. [DOI] [PubMed] [Google Scholar]
- 19.Guo C, Zhang Z, Lau AKH, et al. Effect of long-term exposure to fine particulate matter on lung function decline and risk of chronic obstructive pulmonary disease in Taiwan: a longitudinal, cohort study. Lancet Planet Health. 2018;2(3):e114–e125. doi: 10.1016/S2542-5196(18)30028-7. [DOI] [PubMed] [Google Scholar]
- 20.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–S266. [PubMed] [Google Scholar]
- 21.Levin A, Stevens PE, Bilous RW, et al. Kidney disease: improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150. [Google Scholar]
- 22.Sasaki S, Yoshioka E, Saijo Y, Kita T, Tamakoshi A, Kishi R. Short sleep duration increases the risk of chronic kidney disease in shift workers. J Occup Environ Med. 2014;56(12):1243–1248. doi: 10.1097/JOM.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 23.Li Y, Yang L, Wang H, et al. Longer time spent in bed attempting to sleep is associated with rapid renal function decline: the Dongfeng-Tongji cohort study. Ann Med. 2018;50(2):172–179. doi: 10.1080/07853890.2017.1421321. [DOI] [PubMed] [Google Scholar]
- 24.Bin YS. Is sleep quality more important than sleep duration for public health? Sleep. 2016;39(9):1629–1630. doi: 10.5665/sleep.6078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 26.Hering D, Esler MD, Schlaich MP. Chronic kidney disease: role of sympathetic nervous system activation and potential benefits of renal denervation. EuroIntervention. 2013;(9 Suppl R):R127–R135. doi: 10.4244/EIJV9SRA22. [DOI] [PubMed] [Google Scholar]
- 27.Prather AA, Vogelzangs N, Penninx BW. Sleep duration, insomnia, and markers of systemic inflammation: results from the Netherlands Study of Depression and Anxiety (NESDA) J Psychiatr Res. 2015;60:95–102. doi: 10.1016/j.jpsychires.2014.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80(1):40–52. doi: 10.1016/j.biopsych.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ferrie JE, Kivimaki M, Akbaraly TN, et al. Associations between change in sleep duration and inflammation: findings on C-reactive protein and interleukin 6 in the Whitehall II Study. Am J Epidemiol. 2013;178(6):956–961. doi: 10.1093/aje/kwt072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kochi M, Kohagura K, Shiohira Y, Iseki K, Ohya Y. Inflammation as a risk of developing chronic kidney disease in rheumatoid arthritis. PLoS One. 2016;11(8):e0160225. doi: 10.1371/journal.pone.0160225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838–845. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27(3):440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.