Abstract
Background
American Indians and Alaska Natives (AI/ANs) may be uniquely vulnerable to coccidioidomycosis given the large population residing in the Southwestern United States. We describe coccidioidomycosis-associated hospitalizations and outpatient visits during 2001–2014 in the Indian Health Service (IHS) system and compare hospitalizations with data from the Agency for Healthcare Research and Quality’s National (Nationwide) Inpatient Sample (NIS).
Methods
We identified hospitalizations in the IHS and the NIS and outpatient visits in the IHS using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes 114.0–114.9. We calculated average annual hospitalization and outpatient visit rates per 1 000 000 population and used Poisson regression to calculate rate ratios (RRs) and 95% confidence intervals (CIs). We used multivariable logistic regression to assess factors associated with IHS hospitalization.
Results
AI/ANs had the highest average annual hospitalization rate (58.0; 95% CI, 49.5–66.6) of any racial/ethnic group in the NIS, compared with 13.4 (95% CI, 12.7–14.2) for non-Hispanic whites. IHS data showed a hospitalization rate of 37.0; the median length of stay (interquartile range) was 6 (3–10) days. The average annual outpatient visit rate in IHS was 764.2, and it increased from 529.9 in 2001 to 845.9 in 2014. Male sex, age ≥65 years, diabetes, and extrapulmonary or progressive coccidioidomycosis were independently associated with increased risk for hospitalization. Twenty-four percent of patients had ICD-9-CM codes for community-acquired pneumonia in the 3 months before coccidioidomycosis diagnosis.
Conclusions
AI/ANs experience high coccidioidomycosis-associated hospitalization rates, high morbidity, and possible missed opportunities for earlier diagnosis. Yearly trends in IHS data were similar to the general increase in hospitalizations and reported cases nationwide in the same period.
Keywords: Alaska Natives, coccidioidomycosis, hospitalization, Indians, North American, outpatients, United States
Coccidioidomycosis, also called “Valley fever,” is an infection caused by inhalation of the soil-dwelling fungi Coccidioides spp. Symptomatic infection occurs in approximately 40% of cases and usually presents as a self-limiting influenza-like illness or pneumonia, but a small proportion of patients develop life-threatening severe pulmonary or disseminated disease [1]. In the United States, coccidioidomycosis is known to be endemic in the Southwestern states, with hyperendemic foci in Arizona’s Sonoran Desert and California’s San Joaquin Valley [2]; however, recent evidence suggests that the true endemic areas are likely broader than previously recognized [3].
Several demographic groups are well known to be at higher risk for coccidioidomycosis and its complications: rates of reported infection are consistently highest among older adults [4], and higher rates of severe and disseminated disease have been described for blacks/African Americans and Filipinos [5–7]. Whether American Indians (AIs) are at increased risk for primary coccidioidomycosis, severe or disseminated disease, or death is less clear, and to our knowledge, no studies have comprehensively assessed coccidioidomycosis specifically among this population since the 1980s [8].
Given the well-described disparities in overall infectious disease–related hospitalizations and mortality affecting AIs and Alaska Natives (ANs) [9, 10] and the high concentration of AIs living in areas where coccidioidomycosis is endemic, a better understanding of the disease in this population is needed. To examine the epidemiology of coccidioidomycosis among AI/ANs, we describe coccidioidomycosis-associated inpatient visits using national-level hospitalization data compared with hospitalizations and outpatient visits among AI/ANs in the Indian Health Service (IHS), which provides more comprehensive data than the national data and allows for patient-level analyses.
METHODS
This study uses 2 data sources to estimate the number and rate of coccidioidomycosis inpatient and outpatient visits. Visits were selected for analysis when 1 of any 15 diagnoses listed on the record included the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes for 2 types of coccidioidomycosis: pulmonary and unspecified (114.0, 114.4, 114.5, 114.9) or extrapulmonary and progressive (114.1, 114.2, 114.3).
National (Nationwide) Inpatient Sample
The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project (HCUP), National (Nationwide) Inpatient Sample (NIS), a database derived from billing data from community hospitals from more than 97% of the US population, was used to describe coccidioidomycosis-associated hospitalizations among the general US population, including AI/ANs, during 2001–2014 [11]. The NIS does not include data from IHS-funded facilities and represents a sample of discharges from all participating hospitals. Before 2012, the NIS contained all discharges from a sample of hospitals. Estimates of the number of hospitalizations, with standard errors (SEs), were calculated using the HCUP weighting methodology for the NIS using SUDAAN software (RTI International, Raleigh, NC). We used National Center for Health Statistics annual bridged race population estimates to calculate annual and average annual hospitalization rates per 1 000 000 persons of the corresponding population [12]. The rates with 95% confidence intervals (CIs) were calculated as the weighted number of hospitalizations per 1 000 000 population for the corresponding groups. Estimates were suppressed as “not reliable” if the relative SE exceeded 0.30 or if the unweighted number of hospitalizations in the strata was <11.
Indian Health Service Data
The IHS National Patient Information Reporting System (NPIRS) data for 2001–2014 were examined to identify AI/ANs with coccidioidomycosis-associated inpatient and outpatient visits [13]. These data consist of hospital discharge and outpatient visit records from federal, tribally operated, and contracted health care facilities funded by IHS that provide service for eligible AI/ANs [14]. For the purposes of analyses, IHS-funded facilities were categorized into regions: Alaska, East, Northern Plains East, Northern Plains West, Southern Plains, Southwest, and West. The IHS West region, which includes California, Idaho, Oregon, and Washington, did not have any IHS- or tribally operated hospitals and was therefore excluded from the hospitalization analysis.
Hospitalization and outpatient visit rates were calculated as the number of visits per 1 000 000 user population. User population was defined by IHS as the unduplicated count of eligible AI/ANs by residence who had a direct or contract health care encounter (inpatient, outpatient, or dental) with the IHS-funded health system during the 3 preceding years. Age-adjusted rates were not presented if the count was <20. We examined demographic characteristics, seasonality, coccidioidomycosis type (pulmonary and unspecified vs extrapulmonary and progressive), medical conditions known to be associated with increased risk for severe or disseminated coccidioidomycosis [15], and diagnoses in the 3 months before patients were first assigned a coccidioidomycosis ICD-9-CM code (to examine potential missed or delayed coccidioidomycosis diagnosis). For inpatient records, the regional analysis was simplified to the Southwest compared with other regions combined because of small numbers of hospitalizations in most regions.
To identify possible risk factors for coccidioidomycosis-associated hospitalization among eligible AI/ANs within the IHS system, we divided IHS patients into those who had vs those who never had a coccidioidomycosis-associated hospitalization using a unique patient identifier available within the NPIRS. A univariate analysis using a chi-square test of association was performed on each factor and hospitalization outcome. Stepwise selection was applied to a logistic regression model with the inclusion criterion of P < .1 to determine independent factors for coccidioidomycosis-associated hospitalizations. Possible risk factors considered were sex, age group, coccidioidomycosis type, and presence or absence of previously diagnosed medical conditions known to be associated with increased risk for severe or disseminated coccidioidomycosis.
All age-adjusted rates used the direct method and the 2000 projected US population as the standard. Poisson regression was used to obtain rate ratios (RRs) and 95% confidence intervals (CIs) for comparison within groups and to test for trend over time. Hospitalization rates and 95% CIs were compared between the NIS and IHS data. Statistical tests were considered significant at P < .05. Data analysis was performed using SAS software, version 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
NIS
In the NIS, an estimated 80 563 (average annual rate, 18.4 per 1 000 000; 95% CI, 17.6–19.3) coccidioidomycosis-associated hospitalizations occurred nationwide among the US general population during 2001–2014 (Table 1). AI/ANs had the highest hospitalization rate of any racial/ethnic group (58.0; 95% CI, 49.5–66.6), higher than in non-Hispanic whites (13.4; 95% CI, 12.7–14.2). Among coccidioidomycosis-associated hospitalizations, 18 062 (22%; SE, 0.7) had an ICD-9-CM code for extrapulmonary or progressive coccidioidomycosis listed; 38% (n = 30 695; rate, 7.1; 95% CI, 6.7–7.4) had coccidioidomycosis listed as the primary diagnosis code. The median length of stay was 4.8 (SE, 0.3) days (interquartile range [IQR], 2.5; SE, 0.3; IQR, 9.2; SE, 0.4). The rate was highest among males and patients aged 65 years or older.
Table 1.
Any Listed Age-Adjusted Coccidioidomycosis Hospitalization Rates Among American Indian/Alaska Natives (Indian Health Service) and the General US Population (National [Nationwide] Inpatient Sample), 2001–2014a
| AI/AN | US | |||||
|---|---|---|---|---|---|---|
| Characteristic | No. (%) | Rate (95% CI) | RR (95% CI) | No. [SE], (%) [SE] | Rate (95% CI) | RR (95% CI) |
| Sex | ||||||
| Male | 315 (60.1) | 47.7 (42.2–53.2) | Ref | 49 452 [2367], (61.7) [0.6] | 23.9 (22.9–25.0) | Ref |
| Female | 209 (39.9) | 27.6 (23.8–31.5) | 0.6d | 30 741 [1806], (38.3) [0.6] | 13.5 (12.7–14.2) | 0.6 (0.5–0.7) |
| Age group, yc | ||||||
| <18 | 12 (2.3) | 1.9 | Ref | 2740 [421], (3.4) [0.5] | 2.7 (1.9–3.5) | Ref |
| 18–44 | 208 (39.7) | 28.6 | 14.7 (8.2–26.4) | 25 355 [1429], (31.5) [0.7] | 16.0 (14.3–17.8) | 6.0 (4.1–8.0) |
| 45–64 | 224 (42.7) | 69.1 | 35.6 (19.9–63.7) | 29 991 [1523], (37.3) [0.5] | 28.0 (25.3–30.8) | 10.5 (7.2–13.9) |
| 65+ | 80 (15.3) | 64.7 | 33.3 (18.2–61.1) | 22 332 [1416], (27.8) [0.9] | 40.7 (35.6–45.7) | 15.3 (10.3–20.3) |
| IHS region | ||||||
| Southwest | 500 (95.4) | 91.5 (83.3–99.8) | 0.03d | NA | NA | NA |
| Other | 24 (4.6) | 3.1 (1.9–4.6) | Ref | NA | NA | NA |
| US region | ||||||
| Northeast | NA | NA | NA | 1291 [107], (1.6) [0.2] | 1.5 (1.3–1.8) | Unreliable |
| Midwest | NA | NA | NA | 2882 [170], (3.6) [0.3] | 3.0 (2.7–3.3) | Unreliable |
| South | NA | NA | NA | 5429 [328], (6.7) [0.5] | 3.4 (3.1–3.6) | Ref |
| West | NA | NA | NA | 70 960 [4078], (88.1) [0.7] | 72.4 (68.8–76.0) | Unreliable |
| Race | ||||||
| White | NA | NA | NA | 42 567 [2679], (56.1) [1.2] | 13.4 (12.7–14.2) | Ref |
| Black | NA | NA | NA | 8388 [500], (11.1) [0.4] | 16.4 (15.2–17.7) | 1.2 (0.9–1.5) |
| Hispanic | NA | NA | NA | 18 767 [1126], (24.7) [1.0] | 36.3 (34.1–38.5) | 2.7 (2.1–3.3) |
| A/PI | NA | NA | NA | 3008 [209], (4.0) [0.2] | 15.6 (14.0–17.2) | Unreliable |
| AI/AN | NA | NA | NA | 1849 [252], (2.4) [0.3] | 58.0 (49.5–66.6) | Unreliable |
| ICD-9-CM codec | ||||||
| Primary coccidioidomycosis (114.0) | 186 (35.5) | 13.1 (11.2–15.1) | 37 379 [2410], (46.4) [1.0] | 8.5 (8.0–9.0) | ||
| Primary extrapulmonary coccidioidomycosis (114.1) | 8 (1.5) | b | 504 [52], (0.6) [0.1] | 0.1 (0.1–0.1) | ||
| Coccidioidal meningitis (114.2) | 73 (13.9) | 5.1 (4.0–6.4) | 6773 [414], (8.4) [0.4] | 1.6 (1.5–1.7) | ||
| Other forms of progressive coccidioidomycosis (114.3) | 77 (14.7) | 5.4 (4.2–6.8) | 11 480 [666], (14.3) [0.5] | 2.7 (2.5–2.9) | ||
| Chronic pulmonary coccidioidomycosis (114.4) | 40 (7.6) | 3.0 (2.1–4.0) | 5913 [371], [7.3) [0.3] | 1.3 (1.2–1.4) | ||
| Pulmonary coccidioidomycosis, unspecified (114.5) | 81 (15.5) | 5.9 (4.6–7.4) | 11 567 [609], (14.4) [0.4] | 2.6 (2.5–2.8) | ||
| Coccidioidomycosis, unspecified (114.9) | 77 (14.7) | 5.2 (4.1–6.6) | 9365 [443], (11.6) [0.4] | 2.1 (2.0–2.3) | ||
| Died in the hospital | ||||||
| Died | 10 (1.9) | 3184 [195], (4.0) [0.2] | ||||
| Discharged alive | 514 (98.1) | 36.2 (33.0–39.4) | 77 313 [3963], (96.0) [0.2] | 17.7 (16.9–18.5) | ||
| Total | 524 | 37.0 (33.7–40.2) | 80 563 (4097) | 18.4 (17.6–19.3) |
Gamma confidence intervals were used when normal confidence intervals were unreliable.
Abbreviations: AI/AN, American Indian/Alaska Native; A/PI, Asian/Pacific Islander; CI, confidence interval; RR, rate ratio; SE, standard error.
aFirst-listed coccidioidomycosis hospitalization rate is expressed as the number of hospitalizations with coccidioidomycosis (International Classification of Diseases, 9th Revision, Clinical Modification code 114) listed as the first diagnosis on the hospital record per 1 000 000 corresponding population.
bData not presented with ≤5 hospitalizations for AI/ANs using Indian Health Service data. Age-adjusted rates not calculated on ≤20 hospitalization/visits.
cThe rates for age group and ICD-9-CM codes are crude rates and are not age-adjusted.
dAssociated P value <.05.
IHS
Hospitalizations
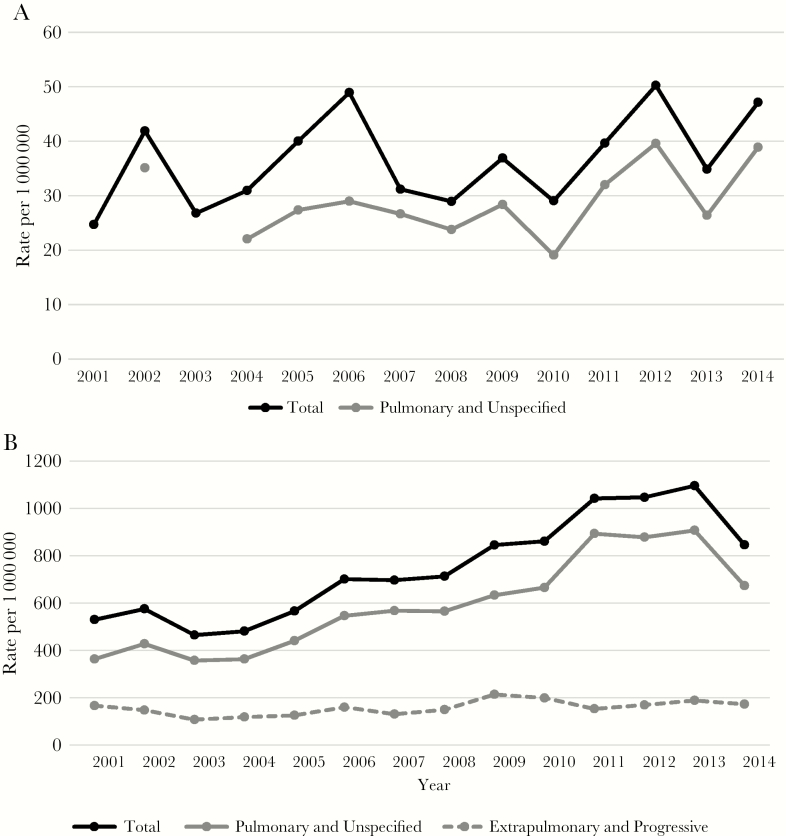
The IHS data contained 524 (average annual rate, 37.0 per 1 000 000; 95% CI, 33.7–40.2) coccidioidomycosis-associated hospitalizations among 328 unique patients (Table 1). Coccidioidomycosis was listed as the primary diagnosis on 38% (n = 197) of hospitalizations (rate, 13.5; 95% CI, 11.5–15.4), and 30% had an ICD-9 code for extrapulmonary or progressive coccidioidomycosis. The median length of stay was 6 days (range, 0–78; IQR, 3–10). Males and patients aged 45–64 years had the highest hospitalization rates. Most (92%) hospitalizations were in the Southwest. There was no significant trend in annual hospitalization rates (Figure 1A), and we did not observe substantial seasonal variation (data not shown).
Figure 1.
A, Trends in rates of coccidioidomycosis-associated inpatient visits among American Indian/Alaska Natives (Indian Health Service), 2001–2014. B, Trends in rates of coccidioidomycosis-associated outpatient visits among American Indian/Alaska Natives (Indian Health Service), 2001–2014. (Data are not shown for rates with <20 hospitalizations.)
Outpatient Data
There were 12 713 coccidioidomycosis-associated outpatient visits (average annual rate, 764.2 per 1 000 000; 95% CI, 750.5–777.8) among 1559 unique patients (rate, 91.5; 95% CI, 86.8–96.1). Patients had a mean of 8 visits and a median of 3 visits (range, 1–155; IQR, 1–8). Fifty-one percent of patients were male (rate, 98.9; 95% CI, 91.7–106.1). Twelve percent (n = 182) of patients had codes for extrapulmonary or progressive coccidioidomycosis, accounting for 2614 (21%) of the outpatient visits (Table 2).
Table 2.
Coccidioidomycosis-Associated Age-Adjusted and Age-Specific Outpatient Patient-Level and Visit-Level Rates Among American Indian/Alaska Natives (Indian Health Service), 2001–2014a
| Unique Patients | All Outpatient Visits | |||||
|---|---|---|---|---|---|---|
| Characteristic | No. (%) | Rate (95% CI) | RR (95% CI) | No. (%) | Rate (95% CI) | RR (95% CI) |
| Sex | ||||||
| Male | 787 (50.5) | 98.9 (91.7–106.1) | 1.2c | 7246 (57.0) | 929.8 (907.6–952.1) | 1.5+ |
| Female | 772 (49.5) | 84.8 (78.7–91.0) | Ref | 5467 (43.0) | 619.1 (602.3–635.8) | Ref |
| Age group, yc | ||||||
| <18 | 125 (8.0) | 17.9 | Ref | 644 (5.1) | 92.0 | Ref |
| 18–44 | 639 (41.0) | 77.2 | 4.3 (3.6–5.2) | 4720 (37.1) | 570.4 | 6.2 (5.7–6.7) |
| 45–64 | 593 (38.0) | 159.3 | 8.9 (7.4–10.8) | 5625 (44.2) | 1511.4 | 16.4 (15.1–17.8) |
| 65+ | 202 (13.0) | 142.7 | 8.0 (6.4–10.0) | 1724 (13.6) | 1218.3 | 13.2 (12.1–14.5) |
| Region | ||||||
| Alaska | 22 (1.4) | 15.3 (9.4–23.6) | 1.0 | 52 (0.4) | 35.7 (26.4–47.0) | 0.3c |
| East | 11 (0.7) | b | b | 23 (0.2) | 40.7 (25.4–61.8) | 0.4c |
| North Plains East | 20 (1.3) | 19.0 (11.3–29.8) | 1.2 | 71 (0.6) | 67.7 (52.5–86.0) | 0.6c |
| North Plains West | 30 (1.9) | 15.4 (9.9–22.7) | Ref | 211 (1.7) | 112.5 (96.7–128.4) | Ref |
| South Plains | 43 (2.8) | 11.0 (7.9–15.0) | 0.7 | 87 (0.7) | 25.2 (20.0–31.3) | 0.2c |
| Southwest | 1348 (86.5) | 234.7 (221.8–247.7) | 15.3c | 11 811 (92.9) | 2112.4 (2073.2–2151.6) | 18.8c |
| West | 85 (5.5) | 39.3 (31.1–49.0) | 2.6c | 458 (3.6) | 225.6 (204.2–247.0) | 2.0c |
| ICD-9-CM codec | ||||||
| Primary coccidioidomycosis (114.0) | 551 (35.3) | 32.3 (29.5–35.1) | 3192 (25.1) | 191.3 (184.5–198.1) | ||
| Primary extrapulmonary coccidioidomycosis (114.1) | 56 (3.6) | 3.1 (2.3–4.1) | 229 (1.8) | 13.3 (11.5–15.0) | ||
| Coccidioidal meningitis (114.2) | 48 (3.1) | 2.8 (2.1–3.8) | 1307 (10.3) | 77.5 (73.2–81.8) | ||
| Other forms of progressive coccidioidomycosis (114.3) | 79 (5.1) | 4.9 (3.8–6.1) | 1082 (8.5) | 68.3 (64.1–72.5) | ||
| Chronic pulmonary coccidioidomycosis (114.4) | 24 (1.5) | 1.5 (1.0–2.3) | 534 (4.2) | 33.7 (30.8–36.7) | ||
| Pulmonary coccidioidomycosis, unspecified (114.5) | 192 (12.3) | 11.4 (9.7–13.0) | 2271 (17.9) | 135.3 (129.6–141.1) | ||
| Coccidioidomycosis, unspecified (114.9) | 617 (39.6) | 36.0 (33.1–39.0) | 4150 (32.6) | 247.8 (240.0–255.5) | ||
| Total | 1559 | 91.5 (86.8–96.1) | 12 713 | 764.2 (750.5–777.8) |
Abbreviations: AI/AN, American Indian/Alaska Native; A/PI, Asian/Pacific Islander; CI, confidence interval; RR, rate ratio; SE, standard error.
aCoccidioidomycosis-associated outpatient visit rates are expressed as the number of hospitalizations/visits with coccidioidomycosis (International Classification of Diseases, 9th Revision, Clinical Modification code 114) listed anywhere on the visit record per 1 000 000 population.
bData not presented with ≤5 hospitalizations/visits. Age-adjusted rates not calculated on ≤20 hospitalization/visits.
cAssociated P value <.05. Significance of rate ratio calculated using z-test or Poisson regression.
The annual rate of outpatient visits increased from 529.9 in 2001 to 845.9 in 2014 (P < .001). The annual rate for unique outpatients also increased, from 143.6 in 2001 to 261.9 in 2013 (P ≤ .001), decreasing slightly to 239.7 in 2014 (Figure 1B). This increase was driven by pulmonary and unspecified coccidioidomycosis diagnoses; rates of outpatient visits for extrapulmonary or progressive coccidioidomycosis remained stable.
Previous Diagnoses
Among all 1624 unique IHS inpatients and outpatients (including 328 with a hospitalization and 1296 with an outpatient visit only), 92% had medical visits in the 3 months before their coccidioidomycosis-associated visit. The most common reasons for visits were diabetes (31% of patients) and hypertension (29%), followed by respiratory illnesses of unspecified cause: “Pneumonia, organism unspecified” (24%), “Other diseases of lung, not elsewhere classified” (13%), “Symptoms involving respiratory system and other chest symptoms; Cough” (12%), and “Special screening examination for bacterial and spirochetal diseases; Pulmonary tuberculosis” (12%) (Supplementary Table 1). The only 1 of these diagnoses in the top 10 most common diagnoses for all patients without coccidioidomycosis in the same period was “Symptoms involving respiratory system and other chest symptoms; Cough” (25%) (Supplementary Table 2).
Risk Factors for Hospitalization
Twenty percent of IHS patients with coccidioidomycosis (n = 328) had at least 1 coccidioidomycosis-associated hospitalization. In univariate analysis, male gender, HIV, diabetes, liver disease, and diagnosis with extrapulmonary or progressive forms of coccidioidomycosis put patients at increased odds of having coccidioidomycosis-associated hospitalization (Table 3).
Table 3.
Factors Associated With Hospitalization Among Indian Health Service Coccidioidomycosis Patients, 2001–2014a
| Condition | Total Unique Coccidioidomycosis Patients, No. (%) | Coccidioidomycosis Patients With Outpatient Visits Only, No. (%) | Coccidioidomycosis Patients Hospitalized, No. (%) | Unadjusted OR (95% CI) | P Value |
|---|---|---|---|---|---|
| Age category | |||||
| <18 y | 126 (8) | 117 (9) | 9 (3) | 0.31 (0.15–0.63) | .0012 |
| 18–44 y | 661 (41) | 530 (41) | 131 (40) | Ref | |
| 45–64 y | 617 (38) | 485 (37) | 132 (40) | 1.10 (0.84–1.44) | .4864 |
| 65+ y | 220 (14) | 164 (13) | 56 (17) | 1.38 (0.97–1.98) | .0773 |
| Sex | |||||
| Male | 820 (50) | 631 (49) | 189 (58) | 1.29 (1.01–1.65) | .0412 |
| Female | 804 (50) | 665 (51) | 139 (42) | Ref | |
| Type of coccidioidomycosis | |||||
| Pulmonary or unspecified | 1321 (20) | 1113 (86) | 208 (63) | Ref | |
| Extrapulmonary or progressive | 303 (19) | 183 (14) | 120 (37) | 3.51 (2.67–4.61) | <.0001 |
| Alcohol use disorders | 345 (21) | 267 (21) | 78 (24) | 1.20 (0.90–1.60) | .2091 |
| Hematologic malignancies | 31 (2) | 22 (2) | 9 (3) | 1.63 (0.75–3.58) | .2204 |
| Malignant neoplasm | 84 (5) | 64 (5) | 20 (6) | 1.25 (0.75–2.10) | .3979 |
| HIV | 86 (5) | 58 (4) | 28 (9) | 1.99 (1.25–3.18) | .0039 |
| Solid organ transplant | 36 (2) | 27 (2) | 9 (3) | 1.33 (0.62–2.85) | .4693 |
| Immune-mediated inflammatory diseaseb | 193 (12) | 169 (13) | 24 (7) | 0.53 (0.34–0.82) | .0048 |
| Chronic obstructive pulmonary disease | 636 (39) | 508 (39) | 128 (39) | 0.99 (0.77–1.27) | .9542 |
| Diabetes | 715 (44) | 540 (42) | 175 (53) | 1.60 (1.26–2.04) | .0002 |
| Asthma | 465 (29) | 386 (30) | 79 (24) | 0.75 (0.57–0.99) | .0419 |
| Liver disease | 212 (13) | 158 (12) | 54 (16) | 1.42 (1.01–1.99) | .0410 |
| Kidney disease | 225 (14) | 178 (14) | 47 (14) | 1.05 (0.74–1.49) | .7806 |
| Tuberculosis | 63 (4) | 45 (3) | 18 (5) | 1.61 (0.92–2.83) | .0941 |
| Pregnancyc | 22 (1) | ||||
| Any of the above conditions | 1286 (79) | 1005 (78) | 281 (86) | 1.73 (1.24–2.42) | .0013 |
| None of the above conditions | 338 (21) | 291 (22) | 47 (14) | Ref | |
| Total | 1624 | 1296 | 328 |
Abbreviations: CI, confidence interval; OR, odds ratio.
aColumn percentages shown.
bRheumatoid arthritis, inflammatory bowel disease, and psoriasis.
cPregnancy only counted if listed up to 1 year before first coccidioidomycosis visit. Due to small numbers, the counts for patients hospitalized and with outpatient-only visits for pregnancy diagnosis could not be displayed.
In multivariable analyses, independent risk factors for increased odds of coccidioidomycosis-associated hospitalization were male sex (odds ratio [OR], 1.33; 95% CI, 1.03–1.73), age ≥65 years or older (OR, 1.48; 95% CI, 1.01–2.16) compared with 18–44 years, extrapulmonary or progressive forms of coccidioidomycosis (OR, 3.60; 95% CI, 2.71–4.78) compared with pulmonary or unspecified coccidioidomycosis, and diabetes (OR, 1.59; 95% CI, 1.21–2.08), whereas patients <18 years old (OR, 0.36; 95% CI, 0.17–0.73) and patients with immune-mediated inflammatory conditions (eg, rheumatoid arthritis, psoriasis, and inflammatory bowel disease) had decreased odds of coccidioidomycosis-associated hospitalization (OR, 0.59; 95% CI, 0.37–0.94).
DISCUSSION
We provide an update on coccidioidomycosis hospitalizations and outpatient visits among AI/ANs. To our knowledge, this is the first comprehensive description of coccidioidomycosis among AI/ANs in several decades and is one of the first to examine the epidemiology of coccidioidomycosis in this population on a national level. We found disparities in coccidioidomycosis hospitalizations among AI/ANs compared with the general US population; high coccidioidomycosis-related morbidity, including potential missed opportunities for early diagnosis; and long-term trends similar to those seen nationwide.
Nationwide, AI/ANs had the highest coccidioidomycosis-associated hospitalization rate of any race/ethnicity, and the rate was more than 4 times higher than that among non-Hispanic whites, although the rate ratio was not reliable. These findings align with previous studies that suggest that this population might be at risk for severe coccidioidomycosis. A retrospective analysis of coccidioidomycosis among AIs in Arizona during 1959–1972 suggested that rates of disseminated disease and death were 3 and 5 times higher, respectively, than those among whites [16]. A subsequent study showed that the rates of disseminated disease and deaths due to coccidioidomycosis decreased during 1959–1980 but that primary infections as approximated by skin testing remained constant; these trends coincided with improvements in housing and working conditions (possibly resulting in reduced intensity of dust exposures), suggesting that environmental factors were larger determinants of coccidioidomycosis than genetic factors [8]. More recent state- and national-level analyses have found conflicting results about the relative frequency of coccidioidomycosis cases, hospitalizations, and deaths among AIs compared with other racial and ethnic groups; however, the comparatively small number of AIs in these analyses limits the ability to draw definitive conclusions [17–21].
AI/ANs might appear to be disproportionally affected by coccidioidomycosis simply because of the large population of AI/ANs who reside in coccidioidomycosis-endemic areas. In previous analyses of coccidioidomycosis-associated deaths, AI/ANs appeared to be at increased risk for death in a national-level data set [19]. A subsequent analysis limited to deaths that occurred in Arizona and California found that AI/ANs still had higher mortality rates than non-Hispanic whites, albeit to a lesser extent than in the national-level analysis, underscoring the importance of examining rates specifically among disease-endemic areas when the racial/ethnic composition of those areas differs from the country as a whole [22]. The fact that >90% of IHS visits with coccidioidomycosis ICD-9-CM codes occurred in the IHS Southwest region underscores the importance of taking geography into account. Unfortunately, the NIS data set does not allow for geographic analyses at a smaller scale than the regional level. The IHS Southwest region, which includes Nevada, Utah, New Mexico, Arizona, and parts of Texas, does not directly align with state boundaries, preventing analysis with state-specific hospitalization data and direct regional comparison with the NIS.
The high coccidioidomycosis hospitalization rates among AI/ANs in our analysis are similar to disparities found in studies of other diseases. For example, hospitalization rates for any infectious disease during 1998–2006 were higher in AI/AN than in the general population. Lower respiratory tract infections (LRTIs) were the most common manifestation, and LRTI rates were highest in the Southwest; ICD-9-CM code 486 (“Pneumonia, organism unspecified”) was the most common first-listed diagnosis, consistent with the clinical presentation and geographic distribution of coccidioidomycosis [10]. Similarly, AI/ANs have been found to have higher rates of death from infectious diseases than whites during 1999–2009, again with LRTI accounting for the highest proportion and the largest disparities in the Southwest [9]. The largest disparities were also observed among deaths due to tuberculosis and mycoses, although there were few deaths due to those causes [9]. In addition to such disparities in disease severity and mortality, public health surveillance data also suggest that AI/ANs experience higher rates of infectious diseases in general. One study described higher infectious disease incidence rates among AI/ANs than whites for more than half of the 26 notifiable diseases reported to the CDC during 2007–2011 [23]. Possible reasons for these disparities include reduced access to health care, particularly due to remoteness of homes, and lack of adequate sanitation [9, 10].
AI/ANs in our study had high morbidity due to coccidioidomycosis. Twenty percent of coccidioidomycosis patients had coccidioidomycosis-associated hospitalizations, likely an underestimate because the IHS West region does not include data on hospitalizations. Other studies have found that as many as 41% of patients in Arizona self-reported being hospitalized and that approximately 30% of patients detected by public health surveillance in California required hospitalization [21, 24]. The median duration of hospitalization in our analysis (6 days) was identical to that reported elsewhere [21, 24]. Notably, the IHS data showed higher rates of hospitalization with extrapulmonary and progressive forms of coccidioidomycosis than the NIS. Although this finding might reflect more severe disease in the IHS cohort, it might also be explained by more re-hospitalizations for severe disease in the IHS than the NIS, because patient-level analyses cannot be performed with the NIS. Differences in testing practices or coding might also explain this disparity. The average number of coccidioidomycosis-associated outpatient visits per person in the IHS data (mean, 8; median, 3) indicates that the disease can be slow to resolve and represents a substantial burden on health care systems. These findings are similar to a 1985 study that showed that college students with coccidioidomycosis visited campus health clinics an average of 6.6 times before the disease resolved [25]. Similarly, another study in Arizona found that patients >60 years of age had a median of 4 coccidioidomycosis-related visits [26].
Diabetes was the only comorbidity independently associated with increased risk for coccidioidomycosis-associated hospitalization in our multivariate analysis; the association between diabetes and severe coccidioidomycosis has been described in other populations [7, 21] and is not surprising given the disproportionately high prevalence of diabetes among AI/ANs compared with the overall US population [27]. A previous analysis of coccidioidomycosis-associated mortality in Arizona and California found a 6-fold higher age- and sex-adjusted mortality rate among AI/ANs with diabetes than among those without [22]. The reasons why immune-mediated inflammatory diseases appeared to be associated with a lower risk for hospitalization are unclear but could be due to misclassification of patients’ comorbidity status based on ICD-9-CM codes, an inherent limitation of our classification scheme. Another possibility is that patients with these diseases may receive more frequent and intensive medical care than those without. Such patients might therefore be more likely to be diagnosed with coccidioidomycosis when milder disease is present and managed in the outpatient setting without requiring hospitalization.
In our analysis, 24% of patients with health care visits in the 3 months before coccidioidomycosis diagnosis had “Pneumonia, organism unspecified” listed as a diagnosis. These visits might represent missed opportunities for earlier coccidioidomycosis diagnosis, as other studies in endemic areas have shown that coccidioidomycosis causes 15%–29% of community-acquired pneumonias (CAPs) but that only a small proportion (<15%) of CAP patients receive laboratory testing for coccidioidomycosis [28–31]. The IHS data do not contain laboratory test results, so we were unable to evaluate coccidioidomycosis testing practices, but our results suggest that coccidioidomycosis patients in the IHS might experience delays in being accurately diagnosed, as is common in the general population [24]. Twelve percent of IHS coccidioidomycosis patients had ICD-9-CM codes for pulmonary tuberculosis testing, further suggesting that patients might receive diagnostic testing for other respiratory illnesses before being diagnosed with coccidioidomycosis.
The overall increase in coccidioidomycosis in the IHS population during 2001–2014 was distinct but consistent with trends in cases detected by public health surveillance during the same period, which peaked in 2011 at 22 641 cases and decreased to 8232 cases in 2014 [32]. However, in this analysis, the peak occurred in 2012 among IHS hospitalized patients and in 2013 among IHS outpatients. The reasons for this difference are not clear but might be related to the smaller number of patients diagnosed in the IHS system. Although coccidioidomycosis is a nationally notifiable condition, federally funded facilities and tribal governments are not required to report cases to local health agencies. However, coccidioidomycosis serological testing is primarily performed in large commercial laboratories, most of which automatically report laboratory-positive cases to public health agencies, suggesting that differences in reporting are unlikely to explain differences in annual trends.
Some overarching limitations should be considered when interpreting our findings. This study is limited by its reliance on ICD codes, and the sensitivity and specificity of coccidioidomycosis ICD codes are unknown. Also, use of administrative data does not account for other underlying conditions in the population, but we attempted to assess this by looking at previous diagnosis codes as a proxy.
In conclusion, coccidioidomycosis-associated hospitalization rates are disproportionately high among AI/ANs compared with the overall US population, and AI/ANs appear to experience similar morbidity, probable underdiagnosis, and long-term trends as other patient groups. At least some of this racial disparity is likely explained by the disproportionately high number of AI/ANs who live in endemic areas. Coccidioidomycosis continues to be greatly under-recognized as a cause of respiratory illness. Strategies to reduce the public health burden of this disease include a focus on greater public and health care provider awareness and improved methods for earlier diagnosis.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
We thank the state data organizations that contribute data to the Healthcare Cost and Utilization Project (https://www.hcup-us.ahrq.gov/db/hcupdatapartners.jsp) and Marian McDonald, Rajal K. Mody, and Sara Seeman from the Centers for Disease Control and Prevention for early contributions to study design.
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Indian Health Service.
Prior presentation. Preliminary results were presented in part at the 60th Annual Coccidioidomycosis Study Group Meeting; 2016; Fresno, CA.
Conflicts of interest. None of the authors have any conflicts of interest to report. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Funding. None.
References
- 1. Smith CE, Beard RR. Varieties of coccidioidal infection in relation to the epidemiology and control of the diseases. Am J Public Health Nations Health 1946; 36:1394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Edwards PQ, Palmer CE. Prevalence of sensitivity to coccidioidin, with special reference to specific and nonspecific reactions to coccidioidin and to histoplasmin. Dis Chest 1957; 31:35–60. [DOI] [PubMed] [Google Scholar]
- 3. Marsden-Haug N, Hill H, Litvintseva AP, et al. ; Centers for Disease Control and Prevention (CDC) Coccidioides immitis identified in soil outside of its known range - Washington, 2013. MMWR Morb Mortal Wkly Rep 2014; 63:450. [PMC free article] [PubMed] [Google Scholar]
- 4. CDC. Increase in reported coccidioidomycosis — United States, 1998–2011. MMWR 2013; 62:217–21. [PMC free article] [PubMed] [Google Scholar]
- 5. Crum NF, Lederman ER, Stafford CM, et al. Coccidioidomycosis: a descriptive survey of a reemerging disease. Clinical characteristics and current controversies. Medicine (Baltimore) 2004; 83:149–75. [DOI] [PubMed] [Google Scholar]
- 6. Durry E, Pappagianis D, Werner SB, et al. Coccidioidomycosis in Tulare County, California, 1991: reemergence of an endemic disease. J Med Vet Mycol 1997; 35:321–6. [DOI] [PubMed] [Google Scholar]
- 7. Rosenstein NE, Emery KW, Werner SB, et al. Risk factors for severe pulmonary and disseminated coccidioidomycosis: Kern County, California, 1995-1996. Clin Infect Dis 2001; 32:708–15. [DOI] [PubMed] [Google Scholar]
- 8. Sievers ML, Fisher JR. Decreasing incidence of disseminated coccidioidomycosis among Piman and San Carlos Apache Indians. A probable environmental basis. Chest 1982; 82:455–60. [DOI] [PubMed] [Google Scholar]
- 9. Cheek JE, Holman RC, Redd JT, Haberling D, Hennessy TW. Infectious disease mortality among American Indians and Alaska Natives, 1999–2009. Am J Public Health 2014; 104(Suppl 3):S446–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Holman RC, Folkema AM, Singleton RJ, et al. Disparities in infectious disease hospitalizations for American Indian/Alaska Native people. Public Health Rep 2011; 126:508–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. HCUP National Inpatient Sample 2012–2014 and Nationwide Inpatient Sample 2001–2011. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research; and Quality; www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 29 May 2018. [Google Scholar]
- 12. National Center for Health Statistics. Intercensal estimates of the resident population of the United States for July 1, 2000 – July 1, 2014, by year, county, single-year of age, bridged race, Hispanic origin, and sex. Prepared under a collaborative arrangement with the U.S. Census Bureau.http://www.cdc.gov/nchs/nvss/bridged_race.htm. Accessed 29 May 2018.
- 13. Indian Health Service. Direct/Contract Health Service Inpatient and Outpatient Visit Data, Fiscal Years 2001–2014. Rockville, MD: Indian Health Service. 2016. [Google Scholar]
- 14. Indian Health Service. Trends in Indian Health: 2014 Edition. Rockville, MD: US Department of Health and Human Services. 2014. [Google Scholar]
- 15. Galgiani JN, Ampel NM, Blair JE, et al. Executive summary: 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis 2016; 63:717–22. [DOI] [PubMed] [Google Scholar]
- 16. Sievers ML. Disseminated coccidioidomycosis among Southwestern American Indians. Am Rev Respir Dis 1974; 109:602–12. [DOI] [PubMed] [Google Scholar]
- 17. Flaherman VJ, Hector R, Rutherford GW. Estimating severe coccidioidomycosis in California. Emerg Infect Dis 2007; 13:1087–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hector RF, Rutherford GW, Tsang CA, et al. The public health impact of coccidioidomycosis in Arizona and California. Int J Environ Res Public Health 2011; 8:1150–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huang JY, Bristow B, Shafir S, Sorvillo F. Coccidioidomycosis-associated deaths, United States, 1990-2008. Emerg Infect Dis 2012; 18:1723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Seitz AE, Prevots DR, Holland SM. Hospitalizations associated with disseminated coccidioidomycosis, Arizona and California, USA. Emerg Infect Dis 2012; 18:1476–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sondermeyer G, Lee L, Gilliss D, et al. Coccidioidomycosis-associated hospitalizations, California, USA, 2000-2011. Emerg Infect Dis 2013; 19:1590–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Noble JA, Nelson RG, Fufaa GD, et al. Effect of geography on the analysis of coccidioidomycosis-associated deaths, United States. Emerg Infect Dis 2016; 22:1821–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adekoya N, Truman B, Landen M; Centers for Disease Control and Prevention Incidence of notifiable diseases among American Indians/Alaska Natives - United States, 2007-2011. MMWR Morb Mortal Wkly Rep 2015; 64:16–9. [PMC free article] [PubMed] [Google Scholar]
- 24. Tsang CA, Anderson SM, Imholte SB, et al. Enhanced surveillance of coccidioidomycosis, Arizona, USA, 2007-2008. Emerg Infect Dis 2010; 16:1738–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kerrick SS, Lundergan LL, Galgiani JN. Coccidioidomycosis at a university health service. Am Rev Respir Dis 1985; 131:100–2. [DOI] [PubMed] [Google Scholar]
- 26. Leake JA, Mosley DG, England B, et al. Risk factors for acute symptomatic coccidioidomycosis among elderly persons in Arizona, 1996-1997. J Infect Dis 2000; 181:1435–40. [DOI] [PubMed] [Google Scholar]
- 27. CDC. Diabetes prevalence among American Indians and Alaska natives and the overall population—United States, 1994–2002. MMWR Morb Mortal Wkly Rep 2003; 52:702–4. [PubMed] [Google Scholar]
- 28. Kim MM, Blair JE, Carey EJ, et al. Coccidioidal pneumonia, Phoenix, Arizona, USA, 2000-2004. Emerg Infect Dis 2009; 15:397–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Valdivia L, Nix D, Wright M, et al. Coccidioidomycosis as a common cause of community-acquired pneumonia. Emerg Infect Dis 2006; 12:958–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chang DC, Anderson S, Wannemuehler K, et al. Testing for coccidioidomycosis among patients with community-acquired pneumonia. Emerg Infect Dis 2008; 14:1053–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tartof SY, Benedict K, Xie F, et al. Testing for coccidioidomycosis among community-acquired pneumonia patients, Southern California, USA. Emerg Infect Dis 2018; 24:779–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention. Valley fever (coccidioidomycosis) statistics 2018. https://www.cdc.gov/fungal/diseases/coccidioidomycosis/statistics.html. Accessed 19 March 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.