Abstract
Objectives
Frequent attenders (FAs) create a substantial portion of primary care workload but little is known about FAs’ sickness absences. The aim of the study is to investigate how occasional and persistent frequent attendance is associated with sickness absences among the working population in occupational health (OH) primary care.
Setting and participants
This is a longitudinal study using medical record data (2014–2016) from an OH care provider in Finland. In total, 59 676 patients were included and categorised into occasional and persistent FAs or non-FAs. Sick-leave episodes and their lengths were collected along with associated diagnostic codes. Logistic regression was used to analyse associations between FA status and sick leaves of different lengths (1–3, 4–14 and ≥15 days).
Results
Both occasional and persistent FA had more and longer duration of sick leave than non-FA through the study years. Persistent FAs had consistently high absence rates. Occasional FAs had elevated absence rates even 2 years after their frequent attendance period. Persistent FAs (OR=11 95% CI 7.54 to 16.06 in 2016) and occasional FAs (OR=2.95 95% CI 2.50 to 3.49 in 2016) were associated with long (≥15 days) sickness absence when compared with non-FAs. Both groups of FAs had an increased risk of long-term sick leaves indicating a risk of disability pension.
Conclusion
Both occasional and persistent FAs should be identified in primary care units caring for working-age patients. As frequent attendance is associated with long sickness absences and possibly disability pensions, rehabilitation should be directed at this group to prevent work disability.
Keywords: sickness absence, occupational health, primary health care, longitudinal studies, public health, access to health care
Strengths and limitations of this study.
The study relies on large nationwide data including employees from rural and urban areas and public and private employers.
The longitudinal study design allows for examining sickness absences also after consultation rates reduce.
The use of medical records to define frequency of visits and sickness absences removes inaccuracy related to self-reporting.
The study lacks information on occupational status, education and use of other service providers as these are not available from occupational health medical records.
Loss to follow-up in occupational health services is larger than in the general practice setting since patients can be lost due to an employment relationship that ends.
Introduction
Frequent attendance is a costly and burdensome phenomenon for healthcare providers, society and patients. Patients, often referred to as frequent attenders (FAs), visit healthcare units repeatedly and constitute a substantial portion of both physician’s time and healthcare costs.1 2 On the other hand, FAs appear to be a vulnerable group of patients who suffer from multimorbidity, medically unexplained symptoms and low quality of life.3–5 For most patients, frequent attendance is transient while a group of persistent FAs (pFAs) continue recurrent visits for extended periods of time.2 6 Research indicates that pFAs often suffer from some combination of somatic, psychological and social problems and are prone to anxiety and worry more than transient FAs are.3 6 7
FAs in general practice (GP) are often unemployed or (disability)pensioners but to date, there is little known about the relationship between frequent attendance and sickness absences among the working population.8–11 The available research indicates that chronic disease and negative life events are predictive of long-term sickness absence among 1-year FAs (1yFAs).12 A Swedish study in GP setting showed that 19% of FAs versus 6% of non-FAs received a long-term sickness absence or disability pension over 5 years’ follow-up.12 Also, being on sick leave or on disability pension increased the mean number of visits in GP setting and was associated with being a FA.10 13 14 However, there are no data available on how occasional and persistent FAs differ in terms of sick leave and if frequent attendance is predictive of future sickness absences. Little is also known about the diagnostic groups associated with FAs’ sickness absences and whether these patterns are similar for occasional and persistent FAs. There is little research on working-age patients alone, and most research concerning working-age patients is conducted in GP setting. Occupational health (OH) primary care in Finland is an ideal place to study working-age patients solely as occupational health services (OHS) primary care is available to 90% of the working population and often used as the sole primary care provider.15 16
In Finland, the proportion of time spent on disability pension is increasingly due to mental disorders, in particular, depression.17 In turn, musculoskeletal and mental disorders are the most common causes for long-term sickness absences.18 19 Both diagnostic groups are also associated with frequent attendance in the Nordic countries in a GP setting and in OH primary care.20–22 Research shows that chronic illnesses that diminish work ability and symptoms related to work are associated with visiting OH primary care.23 In the same setting, in almost half of the visits caused by mental reasons and in one-third of visits due to musculoskeletal reasons, a sickness absence certificate was given.24 These associations suggest that FAs could be a potential risk group for sickness absences and work disability. To grasp the full picture of frequent attendance and the impact on society and individuals, we need to know if and how sickness absenteeism is associated with high use of services.
Understanding the association of frequent attendance with sickness absenteeism is vital to enable healthcare providers to use frequent attendance as an early marker for necessary rehabilitation. It has been shown that short-term sick leaves are associated with long sickness absences and long sick leaves in turn predict disability.25–27 If frequent attendance is predictive of future absences, this could be used to trigger early supportive measures possibly even before the next occurrence of sickness absence. We need to define whether both occasional and persistent FAs are at an equal risk of sickness absences to define appropriate groups for OH interventions where the aim is to prevent sickness absences and disability. Workplace interventions and OH intervention programmes on individuals at risk of sickness absences indicate both cost-effectiveness and reduction in sickness absence days.28–30 However, current interventions are often designed around sickness absences and do not take into account patterns of frequent use. Interventions should be aimed at the group of FAs who are also at risk of long-term sickness absences to ensure both resource management and disability prevention.
We aim to determine how sickness absences of different lengths are associated with occasional and persistent frequent attendance.
Material and methods
Study setting and design
In Finland, OH is an important primary care provider for the working population that functions in parallel with municipal and private primary care services. OHS are divided into obligatory preventive services and voluntary primary care services of which the latter is, however, well used and covers up to 90% of employees.16 OHS primary care is paid by the employers for the most part and is free of charge for the employees. In the Finnish OH primary care, in addition to work-related issues and issues related to work ability, acute and chronic illnesses and typical primary care issues are treated. In primary care issues, a patient can choose where to attend but three out four patients having visited OHS named their OHS unit as their main primary care provider.31 OHS primary care is often used as the sole primary care provider for the working population.15 The role of the OHS units in primary care has increased in the past years32 and primary care is used to support the preventive functions of the OHS by identifying individuals at risk of lowered work ability from the primary care appointments. Most professionals in OHS are specialised in OH. Physiotherapists and psychologists can be consulted after a referral from a nurse or a physician.
This study is conducted using data from Pihlajalinna Työterveys—a large nationwide private OHS provider. The clientele of Pihlajalinna includes employees from both municipal and private employers, with representation from different company sizes and industries. The study is a longitudinal register study using electronic medical record data of Pihlajalinna covering years 2014−2016.
Data collection
Data used for the study included all visits to healthcare professionals and diagnostic codes (International Classification of Diseases, 10th edition (ICD-10)) registered for the visit through the study years 2014–2016. The data also included sickness absences, employee sex and age and employers’ industry and size. Pihlajalinna collected the data and these were sent in pseudonymised format to the University of Tampere for analysis. There were no missing data.
The data initially comprised 78 507 patients. No sampling was done during data collection. The study population was limited to employees who had visited the OH unit during the study years and were aged 18–68 years. Only face-to-face contacts were included and occupational safety check-ups and other mandatory check-ups not initiated by the patient were excluded based on invoice codes. Patients who had no employer-provided primary care service plan were also excluded from the study. After these exclusions, the study population comprised 59 676 patients. Diagnostic codes, using ICD-10, are mandatory for visits to a physician. We used the first (ie, the main) ICD-10 diagnosis registered for each visit in this study. Most employers had all employees’ sickness absence certificates are entered into the medical records through a portal, even though they were certified outside the OHS.
Statistical analysis
We defined FA as the top decile of attenders.2 14 We used visits to physicians, nurses, physiotherapists and psychologists to define FAs and with our definition, FA visited OH units eight or more times yearly.22 The general characteristics of FAs in OHS are described previously, and we also made a secondary analysis of FAs using only visits to the physician, which did not alter the results.22 Patients being in the top decile in 2014 but not in any other study year were categorised as 1-year FAs (1yFAs) representing occasional FAs. Patients who were in the top decile during all three study years (2014–2016) were categorised as pFAs. Patients who were not in the top decile in any of the study years but who had at least once contact with the OHS during the study years were used as a reference group (non-FAs). To avoid confounding, patients who were FA in 2015 or 2016 but not during all three study years were excluded as they might have entered the practice during the study period, and without knowledge of their previous service use, they might have been wrongly categorised.
We divided the study population by sex and into four age categories (18–34, 35–44, 45–54, 55–68) for characterisation. Employer industries were categorised according to Statistics Finland/Statistical Classification of economic activities in the European Community (TOL2008/Nace Rev.2). We analysed sickness absences with different categorisations. First, we divided sickness absence episodes into groups according to the length: no absence, short (1–3 days), intermediate (4–14 days) and long (≥15 days) absence.33 In addition, we looked at the total number of sickness absence days per year with two different categorisations (0, 1–15 or >15 days per year and short (1–3 days) intermediate (4–14 days) and long (≥15 days)).34 Additional analyses using sickness absences as a continuous variable were conducted. When examining sickness absences yearly, we included self-certified and nurse-certified sick leaves. In the analysis of diagnostic codes associated with sickness absenteeism, only physician-certified sick leaves were used.
Chi-square and Kruskal-Wallis tests were used to test for significant differences between groups. Multinomial logistic regression was used to analyse associations of the dependent variable FA status (1yFA, pFA and non-FA) with the independent variables (occurrence of a sick-leave episode and number of sickness absence days yearly). The results were adjusted for sex, age, industry, number of ICD-10 diagnoses and the existence of cancer diagnosis (C00-C97). ORs with 95% CIs were determined. Statistical analyses were conducted in University of Tampere using IBM SPSS Statistics V.23. In all analyses, p values <0.05 were considered statistically significant.
Ethical considerations
According to Finnish legislation (Personal Data Act, Finland, 22.4.1999), individual consent was not needed as this is a large-scale register-based study where no single participant can be recognised.
Patient and public involvement
As it is a study of medical records, patients were not involved.
Results
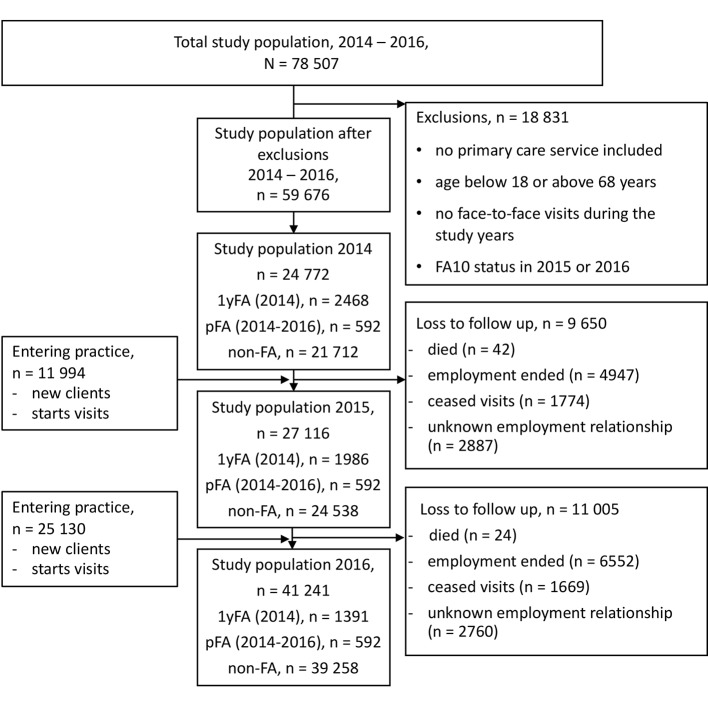
Our study population constituted 59 676 individuals during the study years (2014–2016). The population included 592 pFAs and 2468 1yFAs in 2014. The latter group diminished due to the loss for follow-up as time went on so that in 2015, there were 1986 individuals and in 2016, 1391 individuals in 1yFA group. Figure 1 shows the flow of the study population. Table 1 shows descriptive statistics of 1yFAs, pFAs and non-FAs during the study years. There were more women than men in both 1yFA and pFA groups throughout the study years. Over 90% of the pFA group received a sick-leave certificate from a physician every year and 90% of the 1yFA group received one in the first year. Thereafter of the 1yFA group, ≥70% received a sick-leave certificate from a physician during the study. In 2016, almost 70% of pFAs and 30% of 1yFAs had a sick leave longer than 15 days while only 9% of non-FAs had such a long absence.
Figure 1.
Flow of the study population. 1yFA, 1-year frequent attender; pFA, persistent frequent attender; non-FA, non-frequent attender.
Table 1.
Characteristics by status (1yFA, pFA and non-FA) yearly (2014–2016), n=59 676
| 2014, n=24 772 | 2015, n=27 116 | 2016, n=41 241 | |||||||
| 1yFA n=2468 |
pFA n=592 |
Non-FA n=21 712 |
1yFA n=1986 |
pFA n=592 |
Non-FA n=24 538 |
1yFA n=1391 |
pFA n=592 |
Non-FA n=39 258 |
|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Sex | |||||||||
| Male | 1 134 (46) | 262 (44) | 12 783 (59) | 924 (46) | 262 (44) | 14 628 (60) | 679 (49) | 262 (44) | 22 277 (57) |
| Female | 1 334 (54) | 330 (56) | 8 929 (41) | 1 062 (54) | 330 (56) | 9 910 (40) | 712 (51) | 330 (56) | 16 981 (43) |
| Age, years | |||||||||
| 18–34 | 704 (29) | 130 (22) | 6 751 (31) | 501 (25) | 121 (20) | 7 434 (30) | 264 (19) | 108 (18) | 12 106 (31) |
| 35–44 | 552 (22) | 145 (25) | 5 135 (24) | 465 (24) | 137 (23) | 5 841 (24) | 319 (23) | 132 (22) | 9 467 (24) |
| 45–54 | 638 (26) | 186 (31) | 5 673 (26) | 521 (26) | 190 (32) | 6 532 (27) | 413 (30) | 188 (32) | 10 139 (26) |
| 55–68 | 574 (23) | 131 (22) | 4 153 (19) | 499 (25) | 144 (25) | 4 731 (19) | 395 (28) | 164 (28) | 7 546 (19) |
| Absences | |||||||||
| Sickness absence certified by physician | 2 219 (90) | 551 (93) | 10 309 (47) | 1 511 (76) | 556 (94) | 11 642 (47) | 978 (70) | 547 (92) | 18 350 (47) |
| 0 days /year | 207 (8) | 33 (6) | 9 554 (44) | 377 (19) | 26 (4) | 10 374 (42) | 315 (23) | 34 (6) | 16 873 (43) |
| 1–15 days /year | 768 (31) | 147 (25) | 10 026 (46) | 873 (44) | 127 (22) | 11 722 (48) | 653 (47) | 150 (25) | 18 906 (48) |
| >15 days /year | 1493 (61) | 412 (69) | 2 132 (10) | 739 (37) | 439 (74) | 2 442 (10) | 423 (30) | 408 (69) | 3 479 (9) |
Statistically significant results with the Χ2tests, p<0.001.
FA status was defined as the top decile of attenders (FA 10%, FA10).
1yFA, patients who were in the top decile of attenders in 2014; non-FA, non-frequent attender patients who were never in the top decile were considered as a reference group; pFA, persistent frequent attender patients who were in the top decile in all three study years (2014, 2015 and 2016).
As a whole, the pFA group had a median of 16 absence episodes during the three study years, the 1yFA group had 7 episodes and the non-FA group had a median of 2 episodes, all certified by a physician (table 2). The pFA group had a constant median five to six sickness absence episodes yearly, whereas the 1yFA group had a median of four sickness absence episodes in 2014, after which the frequency of episodes diminished. However, the frequency of sickness episodes remained higher among the 1yFA group than in the non-FA group 2 years after the 1yFA group’s frequent attendance ended.
Table 2.
Median and average lengths of sickness absence episodes, median and average number of absence days yearly and median and average number of written sickness absence certificates yearly (2014–2016) by FA status, n=33 592 (patients with a sickness absence certified by a physician)
| Total length of sickness absences per year | Average length of a single sickness absence episode | Number of written sickness absence certificates | ||||
| av | md | av | md | av | md | |
| 2014 (n=23 232) | *** | *** | *** | |||
| 1yFA | 46.1 | 23 | 9.2 | 4 | 5.0 | 4 |
| pFA | 42.6 | 25 | 7.1 | 4 | 6.0 | 5 |
| Non-FA | 14.4 | 6 | 7.7 | 3 | 1.9 | 1 |
| 2015 (n=25 151) | *** | *** | *** | |||
| 1yFA | 41.2 | 14 | 11.7 | 4 | 3.5 | 3 |
| pFA | 51.4 | 29 | 8.0 | 4 | 6.4 | 6 |
| Non-FA | 14.0 | 5 | 7.5 | 3 | 1.9 | 1 |
| 2016 (n=38 054) | *** | *** | *** | |||
| 1yFA | 28.0 | 10 | 9.1 | 4 | 3.1 | 2 |
| pFA | 51.6 | 24 | 8.8 | 4 | 5.9 | 5 |
| Non-FA | 12.5 | 5 | 6.9 | 3 | 1.8 | 1 |
| 2014–2016 (n=56 042) | *** | *** | *** | |||
| 1yFA | 82.5 | 41 | 9.8 | 4 | 8.4 | 7 |
| pFA | 138.4 | 96 | 7.9 | 4 | 17.4 | 16 |
| Non-FA | 17.7 | 7 | 7.3 | 3 | 2.4 | 2 |
***P<0.001 (Kruskal-Wallis test).
FA status was defined as the top decile of attenders (FA 10%, FA10).
av, average; 1yFA, patients who were in the top decile of attenders in 2014; md, median; non-FA, non-frequent attender patients who were never in the top decile were considered as a reference group; pFA, persistent frequent attender patients who were in the top decile in all three study years (2014, 2015 and 2016).
The lengths of sickness absence episodes are shown in table 2. The average length of a sickness absence episode is consistently high for the pFA group. It is equally high for 1yFA in the first study year, their year of frequent attendance, but the mean and median length of sickness absence reduces slowly, while remaining higher through the study years compared with the non-FA group. The median lengths of single absence episodes are equal between the groups. The median length of single sickness absence episode due to mental and behavioural disorders (F00-F99) was 9, 7 and 7 days for 1yFAs, pFAs and non-FAs, respectively. The median lengths for musculoskeletal disorders (M00-M99) among 1yFAs, pFAs and non-FAs were 7, 5 and 5 days, respectively (data not shown).
Throughout the study years, long sickness absences (≥15 days yearly) were mostly due to musculoskeletal disorders (table 3). Injuries were the second largest diagnostic group for non-FA causing long absences, while for 1yFA and pFA, long absences were caused by mental and behavioural disorders. Musculoskeletal and mental disorders caused 64% of long sick-leave episodes for 1yFAs and 63% for pFAs, while for the non-FA group, the proportion was 46%.
Table 3.
Diagnostic codes associated with sickness absences of different lengths (for sickness absence certificates given by a physician), 2014–2016, n=number of sickness absence certificates
| ICD-10 | 1yFA, n=19 506 | pFA, n=10 117 | Non-FA, n=74 176 | ||||||
| 1–3 days, n=8597 |
4–14 days, n=8261 |
≥15 days, n=2648 |
1–3 days, n=4732 |
4–14 days, n=4357 |
≥15 days, n=1028 |
1–3 days, n=39 566 |
4–14 days, n=28 243 |
≥15 days, n=6367 |
|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| J00-J99 Diseases of the respiratory system | 4020 (47) | 1367 (17) | 48 (2) | 2150 (45) | 810 (17) | 19 (2) | 20 856 (53) | 6570 (23) | 118 (2) |
| M00-M99 Diseases of the musculoskeletal system and connective tissue | 1545 (18) | 3678 (45) | 1248 (47) | 1028 (22) | 2042 (47) | 483 (47) | 5585 (14) | 9820 (35) | 1982 (31) |
| S00-T98 Injury, poisoning and certain other consequences of external causes | 463 (5) | 1045 (13) | 366 (14) | 221 (5) | 461 (11) | 136 (13) | 2100 (5) | 4640 (16) | 1471 (23) |
| F00-F99 Mental and behavioural disorders | 281 (3) | 809 (10) | 439 (17) | 165 (4) | 353 (8) | 164 (16) | 829 (2) | 2171 (8) | 948 (15) |
| A00-B99 Certain infectious and parasitic diseases | 603 (7) | 145 (2) | 4 (0) | 255 (5) | 52 (1) | 4 (0) | 2749 (7) | 792 (3) | 35 (1) |
| Others | 1685 (20) | 1217 (15) | 543 (21) | 913 (19) | 639 (15) | 222 (22) | 7447 (19) | 42 500 (15) | 1813 (28) |
FA status was defined as the top decile of attenders (FA 10%, FA10).
1yFA, patients who were in the top decile of attenders in 2014; ICD-10, International Classification of Diseases, 10th edition; non-FA, patients who were never in the top decile were considered as a reference group, non-FAs; PFA, patients who were in the top decile in all three study years (2014, 2015 and 2016).
In the table are presented the five largest diagnostic groups that had the most sickness absence certificates written through the study years, arranged according to the number of certificates in each category.
In the fully adjusted multinomial logistic regression model, there was no significant difference between short absences between the groups (table 4). In the first year, pFAs and 1yFAs did not differ significantly in their risk of any length sickness absence. However, in the following years, pFAs had higher odds (OR 3.73, 95% CI 2.49 to 5.60 in 2016) of long sickness absence than 1yFA. These groups did not differ in their risk for intermediate length absences. Throughout the study years, both 1yFAs (OR 1.44, 95% CI 1.23 to 1.69 in 2016) and pFAs (OR 2.08, 95% CI 1.39 to 3.10 in 2016) had a higher risk for intermediate length absences than non-FA. This association was enhanced when studying long absences. In 2016, 1yFAs had higher odds (OR 2.95, 95% CI 2.50 to 3.49) for having ≥15 days’ absence than non-FAs, as did pFAs (OR 11.0, 95% CI 7.54 to 16.06).
Table 4.
Lengths of sickness absences associated with FA status in multinomial logistic regression (adjusted for sex, age, field of industry, cancer dg (C00-C97) and number of different ICD-10 diagnoses given by physicians), n=24 772–41 241
| 1yFA vs Non-FA | pFA vs Non-FA | pFA vs 1yFA | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sickness absences (2014) | ||||||
| No sickness absence (0 days) | 1.0 | 1.0 | 1.0 | |||
| Short (1–3 days) | 1.15 | 0.91 to 1.45 | 1.06 | 0.61 to 1.85 | 0.93 | 0.52 to 1.67 |
| Intermediate length (4–14 days) | 2.34 | 1.96 to 2.80 | 2.33 | 1.55 to 3.51 | 1.00 | 0.65 to 1.53 |
| Long (≥15 days) | 13.10 | 11.07 to 15.50 | 18.27 | 12.54 to 26.60 | 1.39 | 0.94 to 2.07 |
| Sickness absences (2015) | ||||||
| No sickness absence (0 days) | 1.0 | 1.0 | 1.0 | |||
| Short (1–3 days) | 1.20 | 1.01 to 1.42 | 1.32 | 0.72 to 2.40 | 1.09 | 0.59 to 2.04 |
| Intermediate length (4–14 days) | 1.89 | 1.64 to 2.17 | 2.92 | 1.87 to 4.57 | 1.55 | 0.97 to 2.46 |
| Long (≥15 days) | 4.48 | 3.88 to 5.16 | 17.96 | 11.83 to 27.25 | 4.01 | 2.60 to 6.18 |
| Sickness absences (2016) | ||||||
| No of sickness absence (0 days) | 1.0 | 1.0 | 1.0 | |||
| Short (1–3 days) | 1.08 | 0.89 to 1.29 | 0.93 | 0.54 to 1.59 | 0.86 | 0.49 to 1.52 |
| Intermediate length (4–14 days) | 1.44 | 1.23 to 1.69 | 2.08 | 1.39 to 3.10 | 1.44 | 0.94 to 2.20 |
| Long (≥15 days) | 2.95 | 2.50 to 3.49 | 11.00 | 7.54 to 16.06 | 3.73 | 2.49 to 5.60 |
FA status was defined as the top decile of attenders (FA 10%, FA10).
1yFA, patients who were in the top decile of attenders in 2014; 1.0, reference group; ICD-10, International Classification of Diseases, 10th edition; non-FA, non-frequent attender patients who were never in the top decile were considered as a reference group; pFA, persistent frequent attender patients who were in the top decile in all three study years (2014, 2015 and 2016).
One day of sickness absence in any of the study years increases the likelihood of being occasional or persistent FAs only slightly and the results are insignificant when comparing 1yFAs with pFAs (table 5). As the number of sickness absence days increases, the association with FA status grows stronger. Table 6 shows characteristics associated with FA status in sickness absences over 15 days. Female sex and morbidity (measured by the number of different diagnoses given by a physician) were associated with FA status in sickness absences over 15 days.
Table 5.
Sickness absence associated with FA status in multinomial logistic regression (adjusted for sex, age, field of industry, cancer dg (C00-C97) and number of different ICD-10 diagnoses given by physicians), n=24 772–41 241
| 1yFA vs Non-FA | pFA vs Non-FA | pFA vs 1yFA | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sickness absences (2014) | ||||||
| A single sickness absence day in 2014 | 1.02 | 1.02 to 1.02 | 1.02 | 1.02 to 1.02 | 1.00 | 0.99 to 1.00 |
| Sickness absences (2015) | ||||||
| A single sickness absence day in 2015 | 1.01 | 1.01 to 1.01 | 1.01 | 1.01 to 1.02 | 1.00 | 1.00 to 1.00 |
| Sickness absences (2016) | ||||||
| A single sickness absence day in 2016 | 1.01 | 1.01 to 1.01 | 1.02 | 1.02 to 1.02 | 1.01 | 1.01 to 1.01 |
FA status was defined as the top decile of attenders (FA 10%, FA10).
*1yFA, patients who were in the top decile of attenders in 2014; ICD-10, International Classification of Diseases, 10th edition; non-FA, non-frequent attender patients who were never in the top decile were considered as a reference group; pFA, persistent frequent attender patients who were in the top decile in all three study years (2014, 2015 and 2016).
Table 6.
Sickness absences >15 days associated with FA status in a multinomial logistic regression model (adjusted for age, field of industry and cancer dg (C00-C97) and number of different ICD-10 diagnoses given by physicians), n=24 772–41 241
| 1yFA vs non-FA | pFA vs non-FA | pFA vs 1yFA | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Sickness absences (2014) | ||||||
| Sex | ||||||
| Male | 1.0 | 1.0 | 1.0 | |||
| Female | 1.52 | 1.28 to 1.82 | 1.76 | 1.33 to 2.31 | 1.15 | 0.88 to 1.50 |
| Number of different ICD-10 diagnoses given by physicians | 2.22 | 2.08 to 2.36 | 2.84 | 2.60 to 3.10 | 1.28 | 1.19 to 1.38 |
| Sickness absences (2015) | ||||||
| Sex | ||||||
| Male | 1.0 | 1.0 | 1.0 | |||
| Female | 1.48 | 1.21 to 1.81 | 1.47 | 1.12 to 1.93 | 0.99 | 0.74 to 1.33 |
| Number of different ICD-10 diagnoses given by physicians | 1.71 | 1.58 to 1.84 | 2.93 | 2.67 to 3.22 | 1.71 | 1.57 to 1.88 |
| Sickness absences (2016) | ||||||
| Sex | ||||||
| Male | 1.0 | 1.0 | 1.0 | |||
| Female | 1.18 | 0.91 to 1.53 | 1.59 | 1.19 to 2.12 | 1.34 | 0.95 to 1.91 |
| Number of different ICD-10 diagnoses given by physicians | 1.76 | 1.63 to 1.91 | 2.82 | 2.58 to 3.09 | 1.60 | 1.45 to 1.77 |
FA status was defined as the top decile of attenders (FA 10%, FA10).
1yFA, patients who were in the top decile of attenders in 2014; 1.0, reference group; ICD-10, International Classification of Diseases, 10th edition; non-FA, non-frequent attender patients who were never in the top decile were considered as a reference group; pFA, persistent frequent attender patients who were in the top decile in all three study years (2014, 2015 and 2016).
Discussion
Our results indicate that pFAs have more and longer sickness absence episodes than other users of OH primary care. However, occasional FAs also have more and longer sickness absences than non-FAs, not only in their year of frequent attendance, but also in the following 2 years. Both FA groups are also associated with an increased risk of long sickness absences. These findings are novel and allow for better understanding of the risk for work disability associated with frequent attendance.
In a Finnish study on municipal employees’ sickness absence longer than 15 days was highly predictive of future disability pension, and a Danish study showed that the longer the absence the higher the risk for a disability pension for private sector employees.27 34 In our study, approximately 70% of pFAs had a sickness absence >15 days yearly, whereas for non-FAs, the proportion was a maximum of 10% through the study years. In 2014, almost two-thirds of occasional FAs had >15 days sickness absence and after 2 years follow-up, one-third of occasional FA had >15 days of absence. Our results indicate that both pFAs and occasional FAs have more and longer sickness absences than an average user and thus might be at an increased risk of retirement due to disability.
Most long sickness absences were caused by diseases of the musculoskeletal system in all groups, but the proportions were higher for occasional and persistent FAs than non-FAs. The second largest group causing long absences was mental disorders for both occasional and persistent FAs. Previous research indicates that musculoskeletal and mental disorders in particular cause recurrent sickness absences and that consultations for a specific illness tend to predict future consultations for the same illness group.35 36 Detection of these individuals for follow-up and necessary rehabilitative measures is important to maintain work ability. Additionally, in particular, sick leaves based on psychiatric and musculoskeletal reasons show increased risk in future for illness-based retirement.37 38 As our study shows that these diagnostic groups are associated with sickness absences of both occasional and persistent FAs, both groups should be of special interest in OHS and GP setting treating working-age patients.
Sickness absences predict future disability and retirement due to ill health and these individuals should be identified for rehabilitation. This study indicates that both pFAs and occasional FAs are at risk of long sickness absences that in turn are associated with risk of disability pension. Vast use of services could be used as an early indicator for interventions to protect work ability. Also, as frequent attendance is mostly a self-limiting condition, it has been argued whether occasional FAs should be a target group for interventions at all.39 However, our results indicate that occasional FAs’ sickness absences are higher than those of average users even after the consultation rates have reduced indicating that they are also in need of rehabilitative evaluation bearing in mind work ability. In addition to occasional FAs’ risk of future absences, pFAs also need attention. PFAs appear to be a group of patients whose needs have not been met. Both these patient groups should be identified and careful diagnostic evaluation should be conducted to enable meeting their needs and reducing absences.
So far, effective interventions on FAs have been those based on in-depth analysis of patient’s reasons for attendance and accordingly selected actions.40 The measured outcomes have been mostly consultation frequency or morbidity, but in the future, sickness absences and change in their frequency or length could be measured as well. Early detection of individuals at risk of work disability based on readily available markers is crucial for the implementation of timely interventions and rehabilitative measures to sustain patient’s work ability.38 Work ability/disability and work-relatedness could be also worth considering when discussing FAs. Determining how sickness absences are associated with frequent attendance is important due to the cost of absenteeism on employers and society, but also because of the effects on the individual, medically certified sickness absences are also associated with mortality.41 42
Strengths and limitations
The strengths of this study are the large study population from an OHS provider including a wide range of industries and company sizes from both rural and urban areas. The employees are representative of the working population in Finland including all ages, employment lengths and status, which allows generalisation outside this particular service provider. The results can be generalised to OHS sector in Finland where a variety of industries are present, and cautious interpretations can be made concerning the working population in general. As no sampling was done, there should not be selection bias in the FA groups. Also, the use of medical records to define the frequency of visits removes inaccuracy related to self-reported utilisation.43 The novel longitudinal study design employed in this study allows for examining sickness absences also after frequent attendance, which gives unique information on risks associated with frequent attendance. To support this aim, we chose to use FAs in 2014 only to represent occasional FA allowing to examine sickness absences after consultation rates have diminished and to allow equal follow-up time with the pFAs. Although there might be limitations to primary care services in OH, visits to nurses and physicians are not restricted. In Finland, the use of GPs in primary care by the working population appears to be scarce compared with use of OHS primary care.15 31 32 Thus, we assume that these results received from the OHS primary care in Finland can be to some extent generalised to the working population using GP services in other countries.
However, this study is limited by the lack of information on occupational status and education since they are not available from medical records. In addition, loss to follow-up in OHS may be larger than in the GP setting since patients can be lost due to an employment relationship that ends. We did not have access to medical record data of other service providers, thus, the sample might include individuals who use other service sectors widely and this could not be accounted for. However, there is evidence that when OH primary care is available, it is often used as the sole primary care provider.15 Also, we cannot track the service use of the patients lost for follow-up. This might add inaccuracy to the categorisation of different FA groups. However, we conducted confirmatory analyses on the subgroup of 1391 occasional FAs whose service use was known for the entire study time, and the results did not differ substantially. We have also conducted confirmatory analyses to ensure that we have sufficient data also on 1–3 days’ length sick leaves. All sick-leave certificates of one of the largest employers on the Pihlajalinna client lists are entered onto the Pihlajalinna sick-leave register. When comparing the proportions of different length absence episodes between this employer and all the data, the results did not differ to a great degree. We defined FAs according to attendance rates across the study population since we wanted to study the working population as a whole. Our study population includes only the working, which narrows the differences between different age groups. In our previous study,22 we analysed the risk of being FA in different age groups and we found no significant association of age with FA status in our study population when adjusted for confounding. We used visits to all healthcare professional in the OHS to categorise FAs. This should be taken into consideration when comparing internationally although we made secondary analysis including only physician visits and the results did not alter.
Conclusions
Both occasional and persistent FAs have higher odds for long and intermediate length absences, which suggests an elevated risk of future retirement due to disability. FAs should be identified in the working-age population and sickness absences should be taken into account when planning FA rehabilitation and interventions.
In future, a longer follow-up of sickness absences would be useful to see whether sickness absence rate eventually equalises with the non-FA group. More understanding is needed of how frequent attendance is associated with disability and retirement due to ill health.
Supplementary Material
Acknowledgments
The authors acknowledge the participation of the occupational health staff in the study and all the individual clients who are part of this study.
Footnotes
Contributors: JU: conceptualised study. NT: analysed the data. TR: wrote the first draft. All authors: planned study; planned datacollection and analysis; contributed to the final version by revising andcommenting on the draft; approved the final version.
Funding: This study is part of the ‘Effectiveness and Indicators of Occupational Health Services’ supported by the European Social Fund (reference number S20659).
Competing interests: None declared.
Ethics approval: The National Institute of Health and Welfare (THL/556/5.05.OO/2016) and the ethics committee of Pirkanmaa Hospital District (ETL R16041) approved the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data that support the findings of this study are available from Pihlajalinna Työterveys but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Pihlajalinna Työterveys.
References
- 1. Gill D, Dawes M, Sharpe M, et al. GP frequent consulters: their prevalence, natural history, and contribution to rising workload. Br J Gen Pract 1998;48:1856–7. [PMC free article] [PubMed] [Google Scholar]
- 2. Smits FT, Brouwer HJ, ter Riet G, et al. Epidemiology of frequent attenders: a 3-year historic cohort study comparing attendance, morbidity and prescriptions of one-year and persistent frequent attenders. BMC Public Health 2009;9:36 10.1186/1471-2458-9-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patel S, Kai J, Atha C, et al. Clinical characteristics of persistent frequent attenders in primary care: case-control study. Fam Pract 2015;32:cmv076–30. 10.1093/fampra/cmv076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Droomers M, Westert GP. Do lower socioeconomic groups use more health services, because they suffer from more illnesses? Eur J Public Health 2004;14:311–3. 10.1093/eurpub/14.3.311 [DOI] [PubMed] [Google Scholar]
- 5. Bergh H, Baigi A, Marklund B. Consultations for injuries by frequent attenders are found to be medically appropriate from general practitioners' perspective. Scand J Public Health 2005;33:228–32. 10.1080/14034940510005761 [DOI] [PubMed] [Google Scholar]
- 6. Pymont C, Butterworth P. Longitudinal cohort study describing persistent frequent attenders in Australian primary healthcare. BMJ Open 2015;5:e008975 10.1136/bmjopen-2015-008975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Smits FT, Brouwer HJ, Zwinderman AH, et al. Why do they keep coming back? Psychosocial etiology of persistence of frequent attendance in primary care: a prospective cohort study. J Psychosom Res 2014;77:492–503. 10.1016/j.jpsychores.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 8. Vedsted P, Christensen MB. Frequent attenders in general practice care: a literature review with special reference to methodological considerations. Public Health 2005;119:118–37. 10.1016/j.puhe.2004.03.007 [DOI] [PubMed] [Google Scholar]
- 9. Scaife B, Gill P, Heywood P, et al. Socio-economic characteristics of adult frequent attenders in general practice: secondary analysis of data. Fam Pract 2000;17:298–304. 10.1093/fampra/17.4.298 [DOI] [PubMed] [Google Scholar]
- 10. Ahmad AW, Dag E, Kurt S. The influence of sociodemographic characteristics on health care utilisation in a Swedish municipality. Ups J Med Sci 2004;109:33–42. 10.3109/2000-1967-108 [DOI] [PubMed] [Google Scholar]
- 11. Karlsson H, Lehtinen V, Joukamaa M. Frequent attenders of Finnish public primary health care: sociodemographic characteristics and physical morbidity. Fam Pract 1994;11:424–30. 10.1093/fampra/11.4.424 [DOI] [PubMed] [Google Scholar]
- 12. Bergh H, Baigi A, Månsson J, et al. Predictive factors for long-term sick leave and disability pension among frequent and normal attenders in primary health care over 5 years. Public Health 2007;121:25–33. 10.1016/j.puhe.2006.08.018 [DOI] [PubMed] [Google Scholar]
- 13. Jyväsjärvi S, Keinänen-Kiukaanniemi S, Väisänen E, et al. Frequent attenders in a Finnish health centre: morbidity and reasons for encounter. Scand J Prim Health Care 1998;16:141–8. [DOI] [PubMed] [Google Scholar]
- 14. Luciano JV, Fernández A, Pinto-Meza A, et al. Frequent attendance in primary care: comparison and implications of different definitions. Br J Gen Pract 2010;60:e49–55. 10.3399/bjgp10X483139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ikonen A, Räsänen K, Manninen P, et al. Use of health services by Finnish employees in regard to health-related factors: the population-based health 2000 study. Int Arch Occup Environ Health 2013;86:451–62. 10.1007/s00420-012-0778-0 [DOI] [PubMed] [Google Scholar]
- 16. Lappalainen K, Aminoff M, Hakulinen H, et al. Työterveyshuolto Suomessa vuonna 2015 [Occupational healthcare in Finland 2015 Report] (In Finnish with english summary). Työterveyslaitos 2016. [Google Scholar]
- 17. Laaksonen M, Rantala J, Järnefelt N, et al. Työkyvyttömyyden vuoksi menetetty työura. [Loss of working career due to illness based retirement] (In Finnish with english summary) . Finnish Centre for Pensions 2016. [Google Scholar]
- 18. Henderson M, Glozier N, Elliot KH. Editorials: Long term sickness absence. BMJ 2005;330:802–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pekkala J, Blomgren J, Pietiläinen O, et al. Occupational class differences in diagnostic-specific sickness absence: a register-based study in the Finnish population, 2005-2014. BMC Public Health 2017;17:670 10.1186/s12889-017-4674-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bergh H, Marklund B. Characteristics of frequent attenders in different age and sex groups in primary health care. Scand J Prim Health Care 2003;21:171–7. 10.1080/02813430310001149 [DOI] [PubMed] [Google Scholar]
- 21. Karlsson H, Lehtinen V, Joukamaa M. Psychiatric morbidity among frequent attender patients in primary care. Gen Hosp Psychiatry 1995;17:19–25. 10.1016/0163-8343(94)00059-M [DOI] [PubMed] [Google Scholar]
- 22. Reho TTM, Atkins SA, Talola N, et al. Frequent attenders in occupational health primary care: A cross-sectional study. Scand J Public Health 2018:140349481877743 10.1177/1403494818777436 [DOI] [PubMed] [Google Scholar]
- 23. Kimanen A, Rautio M, Manninen P, et al. Primary care visits to occupational health physicians and nurses in Finland. Scand J Public Health 2011;39:525–32. 10.1177/1403494811399651 [DOI] [PubMed] [Google Scholar]
- 24. Ikonen A, Räsänen K, Manninen P, et al. Work-related primary care in occupational health physician’s practice. J Occup Rehabil 2012;22:88–96. 10.1007/s10926-011-9325-1 [DOI] [PubMed] [Google Scholar]
- 25. Hultin H, Lindholm C, Möller J, et al. Is there an association between long-term sick leave and disability pension and unemployment beyond the effect of health status?--a cohort study. PLoS One 2012;7:e35614 10.1371/journal.pone.0035614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hultin H, Lindholm C, Malfert M, et al. Short-term sick leave and future risk of sickness absence and unemployment - the impact of health status. BMC Public Health 2012;12:861 10.1186/1471-2458-12-861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lund T, Kivimäki M, Labriola M, et al. Using administrative sickness absence data as a marker of future disability pension: the prospective DREAM study of Danish private sector employees. Occup Environ Med 2008;65:28–31. 10.1136/oem.2006.031393 [DOI] [PubMed] [Google Scholar]
- 28. Van Oostrom S, Driessen M, de Vet H, et al. Workplace interventions for preventing work disability (Review). Cochrane Database Syst Rev 2009:1–67. [DOI] [PubMed] [Google Scholar]
- 29. Taimela S, Justén S, Aronen P, et al. An occupational health intervention programme for workers at high risk for sickness absence. Cost effectiveness analysis based on a randomised controlled trial. Occup Environ Med 2008;65:242–8. 10.1136/oem.2007.033167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kant I, Jansen NW, van Amelsvoort LG, et al. Structured early consultation with the occupational physician reduces sickness absence among office workers at high risk for long-term sickness absence: a randomized controlled trial. J Occup Rehabil 2008;18:79–86. 10.1007/s10926-007-9114-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Virtanen P, Mattila K. Työterveyslääkärin potilas käy myös terveyskeskuksessa, tosin harvoin [Patients of occupational health physicians also visit health centre GPs, albeit seldom] (In Finnish with English summary). Suom Laakaril 2011;47:3583–6. [Google Scholar]
- 32. Vaarama M, Moisio P, Karvonen S. Finnish well-being 2010] (In Finnish) National Institute of Health and Welfare. Helsinki: Suomalaisten hyvinvointi 2010, 2010. [Google Scholar]
- 33. Laaksonen M, He L, Pitkäniemi J. The durations of past sickness absences predict future absence episodes. J Occup Environ Med 2013;55:87–92. 10.1097/JOM.0b013e318270d724 [DOI] [PubMed] [Google Scholar]
- 34. Kivimäki M, Forma P, Wikström J, et al. Sickness absence as a risk marker of future disability pension: the 10-town study. J Epidemiol Community Health 2004;58:710–1. 10.1136/jech.2003.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Roelen CA, Koopmans PC, Anema JR, et al. Recurrence of medically certified sickness absence according to diagnosis: a sickness absence register study. J Occup Rehabil 2010;20:113–21. 10.1007/s10926-009-9226-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jordan K, Ong BN, Croft P. Previous consultation and self reported health status as predictors of future demand for primary care. J Epidemiol Community Health 2003;57:109–13. 10.1136/jech.57.2.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kivimäki M, Ferrie JE, Hagberg J, et al. Diagnosis-specific sick leave as a risk marker for disability pension in a Swedish population. J Epidemiol Community Health 2007;61:915–20. 10.1136/jech.2006.055426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Alexanderson K, Kivimäki M, Ferrie JE, et al. Diagnosis-specific sick leave as a long-term predictor of disability pension: a 13-year follow-up of the GAZEL cohort study. J Epidemiol Community Health 2012;66:155–9. 10.1136/jech.2010.126789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Smits FT, Brouwer HJ, van Weert HC, et al. Predictability of persistent frequent attendance: a historic 3-year cohort study. Br J Gen Pract 2009;59:e44–50. 10.3399/bjgp09X395120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Haroun D, Smits F, van Etten-Jamaludin F, et al. The effects of interventions on quality of life, morbidity and consultation frequency in frequent attenders in primary care: A systematic review. Eur J Gen Pract 2016;22:71–82. 10.3109/13814788.2016.1161751 [DOI] [PubMed] [Google Scholar]
- 41. Kivimäki M, Head J, Ferrie JE, et al. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ 2003;327:364 10.1136/bmj.327.7411.364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Anema JR, van der Beek AJ. Medically certified sickness absence. BMJ 2008;337:a1174 10.1136/bmj.a1174 [DOI] [PubMed] [Google Scholar]
- 43. JÁ B, Lardelli P, De J, et al. Validity of self reported utilisation of primary health care services in an urban population in Spain. J Epidemiol Community Health 2000;54:544–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.