Abstract
Objective:
This study aimed to identify factors associated with high obesity care self-competence among U.S. medical students.
Methods:
The authors performed a cross-sectional analysis of 2014 survey data on fourth year medical students collected online as part of the Medical Student Cognitive Habits and Growth Evaluation Study (CHANGES). Independent variables included quality and quantity of interaction with patients and peers with obesity; hours of communication and partnership skills training; negative remarks against patients with obesity by supervising physicians, and witnessed discrimination against patients with obesity. The dependent variable was self-competence in providing obesity care.
Results:
Of 5,823 students invited to participate, 3,689 (63%) responded and were included in our analyses. Most students were white (65%), half were women, and 42% had high self-competence in caring for patients with obesity. Factors associated with high self-competence included increased interaction with peers with obesity (39% versus 49%, p<0.001) and increased partnership skills training (32% versus 61%, p<0.001).
Conclusions:
Increased partnership skills training and quantity of interactions with peers with obesity were associated with high student self-competence in providing obesity-related care to patients.
Practice Implications:
Medical schools might consider increasing partnership skills training to improve students’ preparedness and skill in performing obesity-related care.
Keywords: Medical Education, Obesity, Self-Competence, Weight Management Services
1. Introduction
Obesity is highly prevalent in the United States, with recent data showing that more than 33% of adults1 and 17% of children2 are affected. Moreover, obesity is linked to comorbidities such as coronary artery disease, hypertension, and type 2 diabetes mellitus3. Care for patients with obesity often involves treating obesity itself rather than only treating the comorbid conditions; however, despite its prevalence, previous studies have demonstrated that physicians have low self-competence in caring for patients with obesity4,5. The term “self-competence” is defined as a self-perception of ability in an academic area6 or the overall sense of oneself as capable, and effective7, in this case in the realm of obesity care. Many physicians identify inadequate training in techniques to communicate about weight and help patients manage their weight in both medical school and residency as a barrier to providing obesity-related care4,5,8,9.
Several studies demonstrate that medical professionals are biased against patients with obesity10–14. Medical students and physicians frequently characterize patients with obesity as “lazy” and use them as targets for derogatory humor15,16. Even incoming first year medical students exhibit negative attitudes towards patients with obesity17. However, these biases are influenced for both better and worse throughout medical school, due to the formal medical curriculum that addresses obesity and communication skills and the informal learning that occurs through contact with patients with obesity and faculty role-modelling18. Thus, undergraduate medical education is an important time to introduce both formal and informal obesity-related training.
In response to the obesity epidemic and physician concerns regarding weight management training, many medical schools now include a formal obesity curriculum; however, this curriculum significantly varies between schools19. Evidence of the effectiveness of these different forms of training is lacking; a systematic review conducted in 2012 found only eleven studies pertinent to medical school obesity education, of which five included intervention and evaluation components, and only one study assessed self-confidence19. It is therefore unclear how both the formal and informal obesity curricula alter medical student self-competence in providing obesity care. The formal curricula can be made up of multiple components20, including lectures on causes and treatments of obesity, intentional exposure to patients with obesity, and structured interpersonal skills training (communication strategies, partnership building strategies). Similarly, the informal curriculum is multidimensional20,21 and includes elements such as the quality of interactions with patients with obesity, interactions with peers with obesity, and resident and attending role model attitudes towards patients with obesity.
Our objective was to identify components of the formal and informal medical school curriculum associated with greater self-competence in caring for patients with obesity among U.S. medical students. We hypothesized that the following factors would be associated with improved self-competence: (1) greater exposure to persons with obesity during medical school, and (2) more hours of interpersonal skills training, including communication and partnership skills. We also hypothesized that (3) more exposure to faculty and resident negative role modeling towards patients with obesity would be associated with impaired self-competence.
2. Methods
2.1. Survey Strategy
This study uses data collected as part of the Medical Student Cognitive Habits and Growth Evaluation Study (CHANGES), a longitudinal survey of medical students conducted upon induction into (2010) and expected graduation from (2014) medical school. The methods have been described in detail previously18,22. Briefly, in the fall of 2010, 49 medical schools were sampled from strata of public and private schools in six regions of the country using a stratified random sampling design.
First-year students were recruited using three strategies: (1) emailing students through a question in the Association of American Medical Colleges (AAMC) Matriculating Student Questionnaire; (2) purchasing an incomplete list of first year medical students from an American Medical Association (AMA) vendor; and (3) referral (i.e., “snowball”) sampling through previously recruited students. Students who consented then completed the online survey at baseline in 2010. In spring 2014, baseline responders completed follow-up measures. The University of Minnesota and Mayo Clinic Internal Review Board approved the study. All students who completed the surveys received a $50 incentive for participation at each time point.
2.2. Study Sample
The 5,823 invited students in 2010 represented 54% of all first-year students enrolled at the sampled schools. The demographic characteristics of the sample were similar to the demographics of all students enrolled in medical schools in 2010 as reported by the AAMC22. This sample of students was surveyed again in 2014, and 3,756 (65%) students responded. Our cross-sectional analysis focuses on variables collected in 2014. Students who had delayed graduation by two or more years or who were missing outcomes data were excluded, leaving 3,689 students eligible for analysis, 63% of students invited in 2010. This response rate was comparable to other published studies of medical students23. Our analytic sample had similar demographics to all students graduating medical school in 2014 as reported by the AAMC24,25.
2.3. Measures
Our dependent variable was “self-competence in caring for patients with obesity” as self-perceived by the students. Of note, there is no previous agreed upon definition of self-competency in regards to obesity care; therefore, we chose two dimensions critical to care for patients with obesity. We defined this variable by combining two questions: 1)”How prepared are you to handle an obese patient?” and 2) “How skilled are you in providing weight loss counseling to obese patients?”. Students responded to both questions using five-point Likert scales. We wanted to identify students who reported high self-competence in caring for patients with obesity and therefore dichotomized responses to these questions (e.g., “high” as very well prepared/well prepared compared to “low” as very unprepared/somewhat unprepared/somewhat prepared). We felt this dichotomy was ethically appropriate and just, as students should graduate medical school feeling more than “somewhat prepared” to handle a patient with obesity and more than “somewhat skilled” to provide weight loss counseling. Our self-competence variable was therefore “high” if both preparedness and skillfulness were high and “not high” if otherwise.
We examined three types of independent variables. First, we measured exposure to persons with obesity using six questions regarding quality and quantity of interactions with patients and peers with obesity. Peers included two separate measures of (1) physicians and (2) other medical students. Quality (e.g., “How favorable have your interactions been with obese patients?”) and quantity (e.g., “How much interaction have you had with obese patients?”) were measured on four-point Likert scales ranging from “very unfavorable” to “very favorable” and “none” to “substantial,” respectively. Quality variables were dichotomized to “favorable” (very favorable/favorable) interactions versus “unfavorable”, as positive and negative interactions may affect self-competence differentially26. Quantity variables were dichotomized to “adequate” (substantial/some interaction) versus “limited.” Second, we determined hours of skills training through two questions. One question assessed formal communication training (“How many hours of training have been devoted to communication skills?”) and the other partnership training (“How many hours of training have been devoted to partnership-building skills. Students could enter any number from 0 to 49 or 50+ (maximum value on scale) hours of formal training, using a sliding scale marked in ten-hour increments. Third, we assessed negative role modeling experiences through two questions. Students responded to the questions “While in medical school, how often have you heard/witnessed professors, instructors, attendings and/or residents make negative comments, disparaging remarks, or jokes about obese patients” and “While in medical school, how often have you heard/witnessed discriminatory treatment of obese patients”. These measures were assessed on five-point Likert scales ranging from “never” to “very often,” which were dichotomized to “infrequent” (never/rarely) versus “frequent,” as witnessing negative role modelling tends to decrease self-competence26. Of note, we did not asses the psychometric properties of the used scales.
Covariates included student demographics and attitudes. Demographics included age, sex, and race, body mass index (BMI), and intended specialty. Race was dichotomized as minority or white. Self-reported height and weight were used to calculate BMI. Students selected an intended specialty from a comprehensive list and were split into four general categories: primary care, surgical, non-primary care clinical specialty (e.g., allergy/immunology), and non-clinical specialty (e.g., nuclear medicine). We felt it was important to assess specialty as students going into different fields may have differential clinical clerkship experiences. We assessed social desirability using a modified version of the Social Desirability Scale27 to control for response bias, and assessed student attitudes towards patients with obesity using a 5-item modified version of the Attitudes Towards Obese Patients scale28.
2.4. Analysis
We performed descriptive analyses of all variables. We conducted bivariate analyses testing the association of the independent variables and covariates with the dependent variables. Given theoretical concern that many covariates may moderate the association between our exposures and “high self-competence” in caring for patients with obesity, we conducted analyses to assess for moderation; however, no covariates analyzed were moderators. In our final models, we adjusted for age, sex, race, BMI at year 4, intended specialty, attitudes towards patients with obesity, and social desirability.
We used logistic regression with list-wise deletion of missing cases29 to model relationships between independent and dependent variables. Given the complex, two-stage cluster sample design of the CHANGES survey, all models were assessed for collinearity and clustering using intraclass correlation. We performed multilevel multivariate logistic models examining the relationship between our dependent and independent variables and assessing for moderation. All final models were run using multilevel multivariate logistic regression, with clustering at the school level, adjusted for the covariates listed above. All results were converted to predicted probabilities for ease of interpretation. We performed all analyses using STATA (StataCorp LP, College Station, TX).
3. Results
Student characteristics are presented in Table 1. Half the students were women, and the majority was white. On average, students reported a healthy BMI, displayed a moderately negative attitude towards patients with obesity, and displayed an average social desirability bias. Just under one-half of students reported applying into primary care. Overall, 42% of students identified themselves as having high self-competence in caring for patients with obesity.
Table 1.
Characteristics of Students in Analytic Sample.
| N (%) unless specified | |
|---|---|
| Students, N | 3,689 |
| Mean age at matriculation | 24 years (SD 2.5) |
| Women | 1854 (50%) |
| Race | |
| White | 2,360 (65%) |
| Other | 1,250 (35%) |
| Mean BMI | 23.8 kg/m2 (SD 3.9) |
| Intended Specialty* | |
| Primary care | 1,794 (49%) |
| Surgical | 745 (20%) |
| Non-primary care clinical | 1,092 (30%) |
| Non-clinical | 44 (1%) |
| Mean Social Desirability Score** | 4.2 (SD 0.9) |
| Mean Attitudes Towards Obese Patients Score** | 3.3 (SD 1.2) |
”Primary care” includes family medicine, internal medicine, obstetrics & gynecology, pediatrics, physical medicine & rehabilitation, and preventive medicine. “Surgical” includes colon & rectal surgery, neurological surgery, ophthalmology, orthopedic surgery, otolaryngology, plastic surgery, surgery, thoracic surgery, and urology. “Non-primary care clinical” includes allergy & immunology, anesthesiology, dermatology, emergency medicine, neurology, radiology, and psychiatry. “Non-clinical” includes nuclear medicine, medical genetics, and pathology.
Scales range from 1–7, with 1 showing the least bias and 7 showing the greatest bias for attitudes towards patients with obesity and responding in a socially desirable manner. Abbreviations: BMI – Body Mass Index, SD – Standard Deviation.
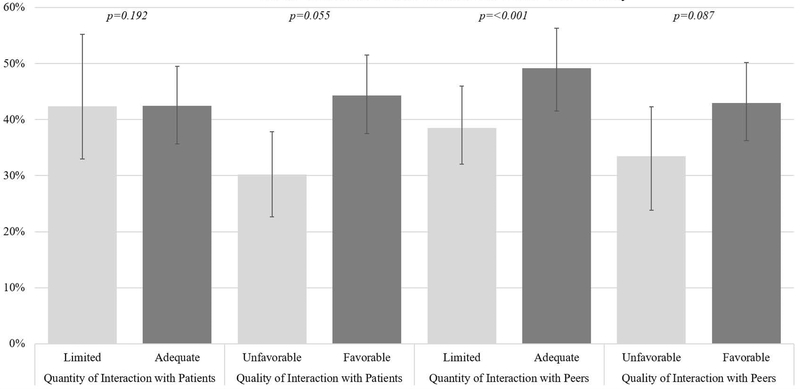
Student exposure to elements of the formal and informal curriculum is presented in Table 2. Most students reported adequate interaction with patients with obesity, and the majority of interactions were favorable. However, neither quantity of interaction with patients with obesity (42% vs 42%, p=0.192) nor quality of interaction with patients with obesity (30% vs 44%, p=0.055) significantly predicted medical students’ having high self-competence in caring for patients with obesity (Figure 1). Over one-third of students were exposed to peers with obesity, and most of these interactions were favorable. Adequate amounts of interactions with peers with obesity were significantly associated with high self-competence (39% vs 49%, p<0.001) (Figure 1), although quality of these interactions were not statistically significant (33% vs 43%, p=0.087).
Table 2.
Student Reported Exposure to Elements of the Formal and Informal Obesity Curriculum.
| H1. Exposure to Individuals with Obesity | |
| Quantity: Interaction with patients with obesity | |
| Limited | 144 (4%) |
| Adequate | 3,545 (96%) |
| Quality: Interaction with patients with obesity | |
| Unfavorable | 476 (13%) |
| Favorable | 3,213 (87%) |
| Quantity: Interaction with peers with obesity | |
| Limited | 2,336 (63%) |
| Adequate | 1,353 (37%) |
| Quality: Interaction with peers with obesity | |
| Unfavorable | 204 (6%) |
| Favorable | 3,485 (94%) |
| H2. Hours of Skills Training | |
| Hours of Communication Skills Training | |
| <10 hours | 401 (11%) |
| ≥ 10 to < 20 hours | 676 (18%) |
| ≥ 20 to < 30 hours | 718 (20%) |
| ≥ 30 to < 40 hours | 465 (13%) |
| ≥ 40 to < 50 hours | 345 (9%) |
| ≥50 hours | 1,084 (29%) |
| Hours of Partnership Skills Training | |
| <10 hours | 1,070 (29%) |
| ≥ 10 to < 20 hours | 902 (24%) |
| ≥ 20 to < 30 hours | 561 (15%) |
| ≥ 30 to < 40 hours | 322 (9%) |
| ≥ 40 to < 50 hours | 185 (5%) |
| ≥50 hours | 649 (18%) |
| H3. Negative Role Modeling | |
| Witnessed negative comments against patients with obesity | |
| Infrequent | 841 (23%) |
| Frequent | 2,848 (77%) |
| Witnessed discriminatory treatment against patients with obesity | |
| Infrequent | 2,736 (74%) |
| Frequent | 953 (26%) |
“Limited” is defined as students reporting none/little quantity of interaction, “adequate” defined as some/substantial quantity of interaction. “Unfavorable” defined as students reporting very unfavorable/unfavorable quality of interaction, “favorable” defined as favorable/very favorable quality of interaction. “Infrequent” defined as students reporting never/rarely observed event, “frequent” defined as sometimes/often/very often observed event. Witnessed negative comments are by residents and professors.
Figure 1.
Adjusted Predicted Probabilities of High Self-Competence Given Interaction with Patients and Peers with Obesity. Predicted probabilities adjusted for age, sex, race, BMI at year 4, intended specialty, attitudes towards patients with obesity, and social desirability. “Limited” is defined as students reporting none/little quantity of interaction, “adequate” defined as some/substantial quantity of interaction. “Unfavorable” defined as students reporting very unfavorable/unfavorable quality of interaction, “favorable” defined as favorable/very favorable quality of interaction.
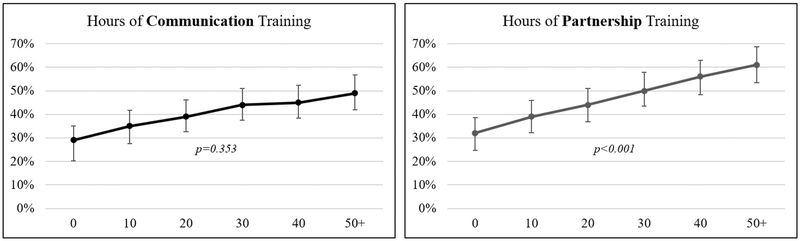
Exposure to skills training varied, with most students reporting at least 10 hours of communication skills and partnership skills training (Table 2). More hours of partnership skills training were associated with students having high self-competence in caring for patients with obesity (p<0.001) (Figure 2). More hours of communication skills training were not associated with students having high self-competence (p=0.353).
Figure 2.
Adjusted Predicted Probabilities of High Self-Competence Given Increasing Hours of Skills Training. Predicted probabilities adjusted for age, sex, race, BMI at year 4, intended specialty, attitudes towards patients with obesity, and social desirability.
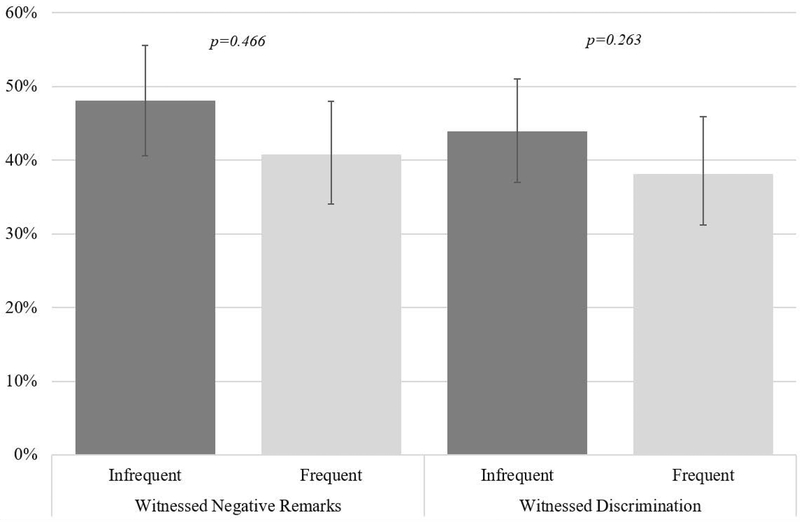
Three-quarters of students reported hearing negative comments from professors or residents regarding patients with obesity, and one-quarter witnessed overt discrimination against patients with obesity (Table 2). There was no statistically significant difference in perceived self-competence if students overheard negative remarks (48% vs 41%, p=0.466) or witnessed discrimination (44% vs 38%, p=0.263) against patients with obesity (Figure 3).
Figure 3.
Adjusted Predicted Probabilities of High Self-Competence Given Witnessed Negative Role Modelling Towards Patients with Obesity. Predicted probabilities adjusted for age, sex, race, BMI at year 4, intended specialty, attitudes towards patients with obesity, and social desirability. “Infrequent” defined as students reporting never/rarely witnessed negative remarks towards patients with obesity or discrimination towards patients with obesity, “frequent” defined as sometimes/often/very often witnessed negative remarks towards patients with obesity or discrimination towards patients with obesity event. Witnessed negative comments are by residents and professors.
4. Discussion and Conclusion
4.1. Discussion
This is the first study that we are aware of to examine the association between components of obesity-related formal and informal curricula and students’ self-competence in providing obesity care prior to residency. “Self-competence” is defined as a self-perception of ability in an academic area6 or a “sense of personal efficacy”7, in this case obesity care, which we believe should ideally be rated as high at the conclusion of medical school. Overall, we found that more contact with peers with obesity and more hours of partnership skills training was associated with students having high self-competence to care for patients with obesity. No other factors were significantly associated with increased self-competence.
In past studies, physicians report a lack of formal obesity management training4,5,8,9. However, our study demonstrates that current medical students are receiving some form of both a formal (interpersonal skills training, consisting of communication and partnership skills, and quantity of interaction with patients with obesity) and informal (quantity and quality of interactions with patients and peers with obesity, role modelling) obesity curriculum.
Prior studies have found that less than half of practicing physicians report high self-competence in treating patients with obesity30–32, although one recent study found that upwards of two-thirds of health care professions are comfortably discussing weight management with patients with obesity33. In comparison, our study found that 42% of medical students reported high self-competence. Whether this degree of self-competence is an improvement for students is unclear, as no prior studies have examined this self-competence among students. Additionally, comparing self-competence of students to practicing clinicians is problematic given differences in experience, training, and measures used to assess this construct. However, less than half of students have high self-competence at the end of their schooling, which raises concern that the current obesity curricula may not be improving future physicians’ skills in this area. Given that high perceived self-competence on a task has been linked to improved task performance34, it is critical to expand the effective parts of the obesity curricula and modify the ineffective parts.
We hypothesized that increased exposure to patients and peers with obesity would increase medical student self-competence in caring for patients with obesity. Peer interactions were defined as those with other medical students, as well as residents and professors. Past studies have found that increased medical student exposure to family members and patients who smoked was associated with increased counseling self-competence35, and that residents’ prior experience treating patients with disease diagnoses increased their self-competence in management of these conditions36. We found that medical students who had a high amount of interaction with peers with obesity were more likely to have high self-competence in providing obesity care. Unlike past studies of medical students and residents with smoking cessation or other counseling topics, we did not find a significant association with increased self-competence among students who had higher exposure to patients with obesity. Medical students likely have a different relationship with their peers than they do with their patients. While interactions with patients are frequently time-limited and place the student in an authority position, interactions with peers are long-term and the student is either an equal or subordinate. We theorize that these differences in the interactions may allow students to value their peers with obesity as people, rather than judging them due to their weight status. Altogether, these findings raise a controversial new discussion point – body-size diversity among medical students and physicians may potentially be beneficial. Past literature has focused on the importance of racial and gender diversity among peers and role-models for improving attitudes and enhancing the educational experience37–41, which may also be relevant to body-size. There is a paucity of research surrounding this topic, and future studies could consider examining the importance of body-size diversity in the medical profession on increasing self-competence in providing care for patients with obesity.
We also hypothesized that increased quality of interaction to patients and peers with obesity would be associated with increased medical student self-competence, given that favorable exposure to a concept tends to make individuals view the concept favorably42. For example, obstetric nursing staff perceived perinatal procedures more favorably if heavily exposed to them with positive results43, and psychiatrists showed high self-competence in providing antipsychotics with which they had high quality experiences44. Contrary to these prior studies, our findings showed no significant association between quality interactions with patient or peer with obesity and high weight management self-competence. Our data relied on students’ self-report of interaction quality, which may be subject to biases. Future studies should consider examining quality of students’ encounters with individuals with obesity objectively, such as through independent analysis of audiovisual recordings.
Previous studies have shown that interpersonal skills training, including partnership skills and communication skills, may increase physician self-competence in providing treatment in a variety of fields45,46. One study in obesity literature showed that when patients perceived their physicians were judging them for their weight, they were less likely to lose weight47, highlighting the value of general interpersonal skills. While we overall recognize the value of interpersonal skills, we had mixed results within our interpersonal skills categories, with more hours of partnership skills training significantly associated with higher self-competence in providing obesity care, while more hours of general communication skills training did not affect self-competence. We recognize that the questions regarding partnership and communication skills may not reflect students’ interactions with patients with obesity, but rather may include breaking bad news to a patient or other such stressful interactions. However, a recent study highlights that discomfort and embarrassment regarding weight management was one of the most common reasons for not bringing up treatment for obesity with patients33. Therefore, partnership is a key component of building rapport and creating a patient-centered experience48, which can improve patient satisfaction and adherence49. More than 70% of students stated that they received at least 20 hours of communication skills training, but only 46% of students received 20 hours of partnership training. Therefore, the additional hours of partnership training may confer a self-competence benefit. Future studies should confirm these findings using objective assessments of training hours and type with concrete definitions, as it is unclear if medical students perceived partnership training as additional formal educational exposure or as an alternative to communication skills training. It is important to determine which aspects of skills training are most effective in order to maximize student self-competence, as there is already limited time and space for large amounts content in undergraduate medical education.
Most students observed negative remarks by professors and residents towards patients with obesity, and over one-quarter observed discriminatory treatment against these patients. While witnessing discriminatory remarks or behavior against patients with obesity does not seem to be associated with self-competence in providing weight management services, the high proportion of students who have observed their patients’ weight discrimination is concerning. These remarks and behaviors have implications for patient care; patients who experience weight stigma may delay receiving preventive care services, potentially leading to worse outcomes14,50. A 2008 study showed that more overweight individuals have perceived weight discrimination over time – increasing from 7% to 12% in the U.S.51 The rates of perceived discrimination are significantly lower than the student-witnessed discriminatory treatment in our study. Students frequently witnessed negative remarks by professors or residents, which may suggest that these comments are occurring in spaces without patients (e.g., team rooms or lecture halls). Our results suggest that additional inquiry is needed to understand where and when these discriminatory remarks or behaviors occur to provide intervention targets for teaching institutions to improve role-modeling of empathic, patient-centered care.
4.2. Limitations
Our study has several limitations. As stated earlier, there is no previous agreed-upon definition of self-competency in obesity care; therefore, our definition is a precursor, and scales need to be developed and validated to further evaluate this domain. Indeed, many of the measures used in the survey were not previously validated, but created or shortened for the CHANGES study in order to reduce respondent burden while still gathering information about key experiences. Similarly, some measures such as consolidating five-point responses into binary responses could affect results depending on the point of division. Moreover, some measures, particularly the communication and partnership skills measures, and the terms “handle” and “weight loss counseling” may have been open to interpretation as no definition or clarification of terms was provided. Given the sampling approach, it is difficult to determine if the sample is representative of all medical students in the United States, although they appear demographically similar, and the representation of schools was geographically representative. We also could not include information from directly observed encounters or from the patient perspective to corroborate the students’ responses with real-life results. Finally, given this is a survey of past experiences conducted at a single time point, we can only definitively assess correlation, not causation, and the results may be affected by recall bias by design.
4.3. Conclusions
This is the first study to look at medical students’ self-competence in caring for patients with obesity given their experiences with the formal and informal curricula in medical schools across the country. Overall, we found that less than half of medical students have high weight management self-competence, and that increased exposure to peers with obesity and increased hours of partnership skills training is associated with improved self-competence.
4.4. Practice Implications
As increased interactions with peers with obesity is associated with higher self-competence, increasing body-size diversity may be valuable in undergraduate medical education. We praise schools for their work in communication training, and recommend that they consider providing more hours of partnership skills training, which has the potential to improve self-competence for future physicians providing weight management services.
Acknowledgements
RSD and SMP had access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
SMP and the CHANGES team participated in data collection. RSD and SMP conducted data analysis with input from KAG and the CHANGES team. RSD drafted the manuscript with assistance from KAG and SMP, and edits from LND, JFD, SB, ROW, SP, MY, and MVR.
RSD’s contribution was funded by the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research [grant number TL1 TR001078]. KAG was funded by grant K23HL116601. The CHANGE Study was funded by NHLBI under award R01HL085631. The contents of this manuscript are solely the responsibility of the authors and do not represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Footnotes
DISCLOSURES: No disclosures.
Contributor Information
Dr. Ruchi S Doshi, Duke University Hospital in Durham NC, USA..
Dr. Kimberly A Gudzune, Johns Hopkins University School of Medicine and the Welch Center for Prevention, Epidemiology, and Clinical Research, Johns Hopkins University in Baltimore MD, USA..
Dr. Liselotte N Dyrbye, Division of Primary Care Internal Medicine, Department of Medicine, Mayo Clinic, Rochester MN, USA..
Dr. John F Dovidio, Department of Psychology, at Yale University, New Haven CT, USA..
Dr. Sara E Burke, Syracuse University in the Department of Psychology, Syracuse NY, USA..
Dr. Richard O White, Division of Community Internal Medicine at Mayo Clinic, Jacksonville FL, USA..
Dr. Sylvia Perry, Department of Psychology at Northwestern University, Evanston IL, USA..
Dr. Mark Yeazel, Department of Family Medicine and Community Health at University of Minnesota, Twin Cities, Minneapolis MN, USA..
Dr. Michelle van Ryn, Division of Health Care Policy and Research, Department of Health Sciences Research at Mayo Clinic, Rochester MN, USA..
Dr. Sean M Phelan, Division of Health Care Policy and Research, Department of Health Sciences Research at Mayo Clinic, Rochester MN, USA..
References
- 1.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA 2016;315:2284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA 2016;315:2292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 2009;9:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jay M, Gillespie C, Ark T, et al. Do internists, pediatricians, and psychiatrists feel competent in obesity care?: using a needs assessment to drive curriculum design. J Gen Intern Med 2008;23:1066–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Block JP, DeSalvo KB, Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med 2003;36:669–75. [DOI] [PubMed] [Google Scholar]
- 6.Harter S The perceived competence scale for children. Child Development 1982;53:87–97. [PubMed] [Google Scholar]
- 7.Tafarodi RW, Swann WB Jr,. Self-liking and self-competence as dimensions of global self-esteem: initial validation of a measure. J Pers Assess 1995;65:322–42. [DOI] [PubMed] [Google Scholar]
- 8.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med 1995;24:546–52. [DOI] [PubMed] [Google Scholar]
- 9.Forman-Hoffman V, Little A, Wahls T. Barriers to obesity management: a pilot study of primary care clinicians. BMC Fam Pract 2006;7:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klein D, Najman J, Kohrman AF, Munro C. Patient characteristics that elicit negative responses from family physicians. J Fam Pract 1982;14:881–8. [PubMed] [Google Scholar]
- 11.Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res 2003;11:1033–9. [DOI] [PubMed] [Google Scholar]
- 12.Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord 2001;25:1246–52. [DOI] [PubMed] [Google Scholar]
- 13.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord 2001;25:1525–31. [DOI] [PubMed] [Google Scholar]
- 14.Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev 2015;16:319–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wear D, Aultman JM, Varley JD, Zarconi J. Making fun of patients: medical students’ perceptions and use of derogatory and cynical humor in clinical settings. Acad Med 2006;81:454–62. [DOI] [PubMed] [Google Scholar]
- 16.Price JH, Desmond SM, Krol RA, Snyder FF, O’Connell JK. Family practice physicians’ beliefs, attitudes, and practices regarding obesity. Am J Prev Med 1987;3:339–45. [PubMed] [Google Scholar]
- 17.Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring) 2014;22:1201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phelan SM, Puhl RM, Burke SE, et al. The mixed impact of medical school on medical students’ implicit and explicit weight bias. Med Educ 2015;49:983–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vitolins MZ, Crandall S, Miller D, Ip E, Marion G, Spangler JG. Obesity educational interventions in U.S. medical schools: a systematic review and identified gaps. Teach Learn Med 2012;24:267–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paul D, Ewen SC, Jones R. Cultural competence in medical education: aligning the formal, informal and hidden curricula. Adv Health Sci Educ Theory Pract 2014;19:751–8. [DOI] [PubMed] [Google Scholar]
- 21.Doja A, Bould MD, Clarkin C, Eady K, Sutherland S, Writer H. The hidden and informal curriculum across the continuum of training: A cross-sectional qualitative study. Med Teach 2016;38:410–8. [DOI] [PubMed] [Google Scholar]
- 22.Hardeman RR, Burgess D, Phelan S, Yeazel M, Nelson D, van Ryn M. Medical student socio-demographic characteristics and attitudes toward patient centered care: do race, socioeconomic status and gender matter? A report from the Medical Student CHANGES study. Patient Educ Couns 2015;98:350–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dyrbye LN, Thomas MR, Harper W, et al. The learning environment and medical student burnout: a multicentre study. Med Educ 2009;43:274–82. [DOI] [PubMed] [Google Scholar]
- 24.AAMC. Total Graduates by U.S. Medical School and Sex, 2011–2012 through 2015–2016. In: Table B-2.2: Total Graduates by U.S. Medical School and Sex -t-, ed.2016.
- 25.AAMC. Total Graduates by U.S. Medical School and Race/Ethnicity, 2015–2016. In: Table B-6: Total Graduates by U.S. Medical School and Race/Ethnicity -, ed.: AAMC; 2016. [Google Scholar]
- 26.Gist ME MT. Self-Efficacy: A Theoretical Analysis of its Determinants and Malleability. Academy of management review 1992;17:183–211. [Google Scholar]
- 27.Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol 1960;24:349–54. [DOI] [PubMed] [Google Scholar]
- 28.Puhl RM, Luedicke J, Grilo CM. Obesity bias in training: attitudes, beliefs, and observations among advanced trainees in professional health disciplines. Obesity (Silver Spring) 2014;22:1008–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Allison PD. Missing data techniques for structural equation modeling. J Abnorm Psychol 2003;112:545–57. [DOI] [PubMed] [Google Scholar]
- 30.Perrin EM, Flower KB, Garrett J, Ammerman AS. Preventing and treating obesity: pediatricians’ self-efficacy, barriers, resources, and advocacy. Ambul Pediatr 2005;5:150–6. [DOI] [PubMed] [Google Scholar]
- 31.Jay M, Kalet A, Ark T, et al. Physicians’ attitudes about obesity and their associations with competency and specialty: a cross-sectional study. BMC Health Serv Res 2009;9:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr 2008;27:287–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaplan LM, Golden A, Jinnett K, et al. Perceptions of Barriers to Effective Obesity Care: Results from the National ACTION Study. Obesity (Silver Spring) 2018;26:61–9. [DOI] [PubMed] [Google Scholar]
- 34.Bandura A Perceived Self-Efficacy in Cognitive Development and Functioning. Educational Psychologist 1993;28:117–48. [Google Scholar]
- 35.Xiao RS, Hayes RB, Waring ME, et al. Tobacco counseling experience prior to starting medical school, tobacco treatment self-efficacy and knowledge among first-year medical students in the United States. Prev Med 2015;73:119–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yudkowsky R, Downing SM, Ommert D. Prior experiences associated with residents’ scores on a communication and interpersonal skill OSCE. Patient Educ Couns 2006;62:368–73. [DOI] [PubMed] [Google Scholar]
- 37.Whitla DK, Orfield G, Silen W, Teperow C, Howard C, Reede J. Educational benefits of diversity in medical school: a survey of students. Acad Med 2003;78:460–6. [DOI] [PubMed] [Google Scholar]
- 38.Guiton G, Chang MJ, Wilkerson L. Student body diversity: relationship to medical students’ experiences and attitudes. Acad Med 2007;82:S85–8. [DOI] [PubMed] [Google Scholar]
- 39.Groman R, Ginsburg J, American College of P. Racial and ethnic disparities in health care: a position paper of the American College of Physicians. Ann Intern Med 2004;141:226–32. [DOI] [PubMed] [Google Scholar]
- 40.Bright CM, Duefield CA, Stone VE. Perceived barriers and biases in the medical education experience by gender and race. J Natl Med Assoc 1998;90:681–8. [PMC free article] [PubMed] [Google Scholar]
- 41.Mitchell DA, Lassiter SL. Addressing health care disparities and increasing workforce diversity: the next step for the dental, medical, and public health professions. Am J Public Health 2006;96:2093–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bornstein RF. Exposure and affect: Overview and meta-analysis of research, 1968–1987. Psychological Bulliten 1989;106:265–89. [Google Scholar]
- 43.Liva SJ, Hall WA, Klein MC, Wong ST. Factors associated with differences in Canadian perinatal nurses’ attitudes toward birth practices. J Obstet Gynecol Neonatal Nurs 2012;41:761–73. [DOI] [PubMed] [Google Scholar]
- 44.Makhinson M Biases in medication prescribing: the case of second-generation antipsychotics. J Psychiatr Pract 2010;16:15–21. [DOI] [PubMed] [Google Scholar]
- 45.McCallister JW, Gustin JL, Wells-Di Gregorio S, Way DP, Mastronarde JG. Communication skills training curriculum for pulmonary and critical care fellows. Ann Am Thorac Soc 2015;12:520–5. [DOI] [PubMed] [Google Scholar]
- 46.Norgaard B, Ammentorp J, Ohm Kyvik K, Kofoed PE. Communication skills training increases self-efficacy of health care professionals. J Contin Educ Health Prof 2012;32:90–7. [DOI] [PubMed] [Google Scholar]
- 47.Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Perceived judgment about weight can negatively influence weight loss: a cross-sectional study of overweight and obese patients. Prev Med 2014;62:103–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC)2001. [PubMed] [Google Scholar]
- 49.Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract 2002;15:25–38. [PubMed] [Google Scholar]
- 50.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health 2010;100:1019–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity (Silver Spring) 2008;16:1129–34. [DOI] [PubMed] [Google Scholar]