Abstract
Background
Exercise is known to be an important component of treatment programs for individuals with neck pain. The study aimed to compare the effects of semispinalis cervicis (extensor) training, deep cervical flexor (flexor) training, and usual care (control) on functional disability, pain intensity, craniovertebral (CV) angle, and neck-muscle strength in chronic mechanical neck pain.
Methods
A total of 54 individuals with chronic mechanical neck pain were randomly allocated to three groups: extensor training, flexor training, or control. A Thai version of the Neck Disability Index, numeric pain scale (NPS), CV angle, and neck-muscle strength were measured at baseline, immediately after 6 weeks of training, and at 1- and 3 -month follow-up.
Results
Neck Disability Index scores improved significantly more in the exercise groups than in the control group after 6 weeks training and at 1- and 3-month follow-up in both the exten-sor (P=0.001) and flexor groups (P=0.003, P=0.001, P=0.004, respectively). NPS scores also improved significantly more in the exercise groups than in the control group after 6 weeks’ training in both the extensor (P<0.0001) and flexor groups (P=0.029. In both exercise groups, the CV angle improved significantly compared with the control group at 6 weeks and 3 months (extensor group, P=0.008 and P=0.01, respectively; flexor group, P=0.002 and 0.009, respectively). At 1 month, the CV angle had improved significantly in the flexor group (P=0.006). Muscle strength in both exercise groups had improved significantly more than in the control group at 6 weeks and 1- and 3-month follow-up (extensor group, P=0.04, P=0.02, P=0.002, respectively; flexor group, P=0.002, P=0.001, and 0.001, respectively). The semispinalis group gained extensor strength and the deep cervical flexor group gained flexor strength.
Conclusion
The results suggest that 6 weeks of training in both exercise groups can improve neck disability, pain intensity, CV angle, and neck-muscle strength in chronic mechanical neck pain.
Trial registration
Keywords: specific training, deep-neck muscles, chronic neck pain
Introduction
Neck pain is a common problem in the general population, with prevalence reported to be 43%–66.7%1 at some point in life. A study suggested that the incidence of neck pain was most commonly found in the working age-group 40–59 years old.2 The source of pain may arise from many structures of the cervical spine, and can develop into chronic pain.1 Neck problems can adversely affect physical, psychological, and social function. Neck pain also leads to high costs in national healthcare systems.3
Mechanical neck pain is the most common type found in neck-pain disorders.4 Studies have demonstrated altered behavior of the cervical muscles in mechanical neck-pain patients.5,6 Researchers have documented a reduction in the activity of the longus colli and longus capitis.6,7 Further, recent studies showed that women with chronic neck pain had lower neck-muscle strength during extension than a healthy female group,8 less activity was observed in the semispinalis cervicis and multifidus in patients with chronic neck pain when compared with a healthy population,9 and decreased semispinalis cervicis muscle activity was reported in neck-pain patients.10 Studies have shown the deep cervical extensor musculature to have altered cross-sectional area, particularly the semispinalis cervicis and cervical multifidus muscles in chronic neck-pain patients.11–13 Deficits in deep cervical muscle activity of the cervical spine may lead to poor control of joint movement, repeated microtrauma, and thus eventual pain.14
Exercise is known to be an important component of treatment programs for patients with neck pain.15,16 Recently, many studies have focused on specific training on deep cervical muscles. Craniocervical flexor-muscle training enhances ability and improves neuromuscular control of the deep cervical flexor muscles, including the longus colli and longus capitis.17,18 Numerous studies using craniocervical flexor exercise as a treatment have led to a reduction in pain and neck disability, and also enhanced activation of the deep and superficial cervical flexor muscles.19–24 Further, the cervical extensor muscles are believed to be equally important for the rehabilitation of patients with neck pain.25 The deep cervical extensors semispinalis and multifidus are the important cervical spine-stabilization muscles. Their impairment is observed in neck-pain patients,10,26 and activation of these deep muscles should be emphasized in the rehabilitation of people with neck pain.26 A study suggested that resisted isometric exercise at the level of the second cervical vertebra can achieve relative isolation of the semispinalis cervicis muscle.32 Therefore, isometric resisted exercise at the level of the second cervical vertebra may stimulate the semispinalis cervicis muscle. However, to date, specific exercise for the semispinalis cervicis muscle has not been investigated in patients with chronic mechanical neck pain. Further, the effectiveness of semispinalis cervicis exercise on functional disability, pain intensity, neck-muscle strength, and craniovertebral (CV) angle is unknown. Therefore, semispinalis cervicis exercise still requires evidence to support its use for clinical effects in chronic mechanical neck pain.
The aim of the current study was to compare the effects of semispinalis cervicis training, deep cervical flexor training, and usual care (control) on functional disability, pain intensity, CV angle, and neck-muscle strength on chronic mechanical neck pain. We hypothesized that semispinalis cervicis training would be superior or equal to deep cervical flexor training and would be superior to usual care (manual therapy, modality, and other exercises).
Methods
An assessor-blinded, randomized controlled trial was used to determine the effects of semispinalis cervicis training, deep cervical flexor training, and usual care on chronic mechanical neck pain. This trial was conducted in accordance with the Declaration of Helsinki. The research protocol was approved by the Research Ethics Committee for Human Research of Khon Kaen University (HE571381). All participants were asked to sign an informed-consent form before participating in the study. The participants in all figures in this paper signed an informed consent for their images to be published.
Participants
A total of 57 neck-pain patients were screened for eligibility in the current study. After assessment by the doctor and completion of the questionnaire, 54 eligible patients were enrolled. Exclusion criteria included positive neurological signs (n=2) and severe neck pain from spinal infection (n=1). A total of 54 participants with chronic mechanical neck pain took part in this study. Mechanical neck pain was defined as pain in the area of the neck and/or neck-shoulder with neck pain that could be provoked by mechanical characteristics, including sustained neck postures, cervical movement, or manual palpation of the cervical musculature.27,28 Specifically, the pain had to be localized to the dorsal part of the neck in an area limited by a horizontal line through the inferior portion of the occipital region and a horizontal line through the spinous process of the first thoracic vertebra.29 To be eligible for the study, participants had to meet three criteria: have neck-pain symptoms of at least 3 months’ duration, a score ≥10/100 on the Thai Version of the Neck Disability Index (NDI-TH) questionnaire,30 and be aged 18–60 years, to capture adults of working age.
Participants were excluded if they reported any of the following: 1) diagnosis of cervical radiculopathy or myelopathy (at least two of myotomal strength, sensation, or reflexes had to be diminished for nerve-root or spinal cord involvement to be considered); 2) history of cervical and thoracic spine fracture and/or dislocation; 3) history of surgery of the cervical and/or thoracic spine; 4) history of spinal osteoporosis, spinal infection, or fibromyalgia syndrome, and 5) history of whiplash injury and/or head/neck injuries.
Procedures
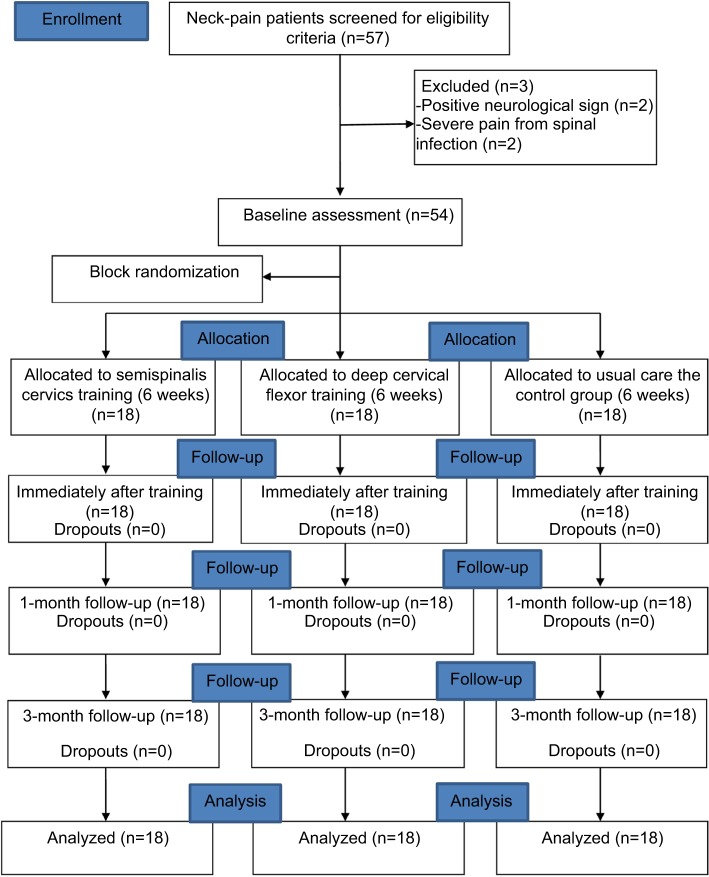
Participants were initially assessed by a doctor of rehabilitation medicine. All eligible participants were asked to complete the NDI-TH. A blinded assessor then measured pain intensity using a numeric pain scale (NPS), CV angle using a digital camera, and neck-flexor and extensor-muscle strength with a dynamometer. All 54 patients were randomly allocated to the control, semispinalis cervicis-training, or deep cervical flexor-training groups using a blocked randomization with a block size of three (Figure 1). Participants were asked to stop other treatments during participation in this study.
Figure 1.
Participant flow diagram and follow-up evaluation.
Interventions
Semispinalis cervicis-training group
Participants received semispinalis cervicis isometric exercise as described by Schomacher et al in their intramuscular electromyography (EMG) study.32 In that study, the semispinalis cervicis was selectively activated relative to the splenius capitis by applying manual static resistance to the vertebral arch of C2 and asking the upright-sitting patient to push backward.32 The aim of the exercise was to stimulate semispinalis cervicis activation selectively. In the current study, the exercise was performed by subjects while sitting on a stool without a backrest with hips and knees flexed 90° and feet placed on the floor. The researcher stood on the left of the subject, facing them. Next, the researcher placed the thumb and index finger of the right hand approximately on the posterior vertebral arches of the subject’s second cervical vertebra (C2) and pushed firmly/gently (slowly to increase resistance) into flexion (anteriorly), while the left hand stabilized the participant’s left shoulder to monitor the compensatory body movement. Subjects were asked to resist maximal voluntary contraction in the direction of extension without provocation of neck pain (Figure 2A). The exercise program was performed to hold resistance for 10 seconds, ten times per set, with three sets per day. A 30-second rest was allowed between sets. Each subject performed this exercise twice per week over a 6-week period with the physical therapist. The exercise was performed as tolerated without provocation of neck pain.
Figure 2.
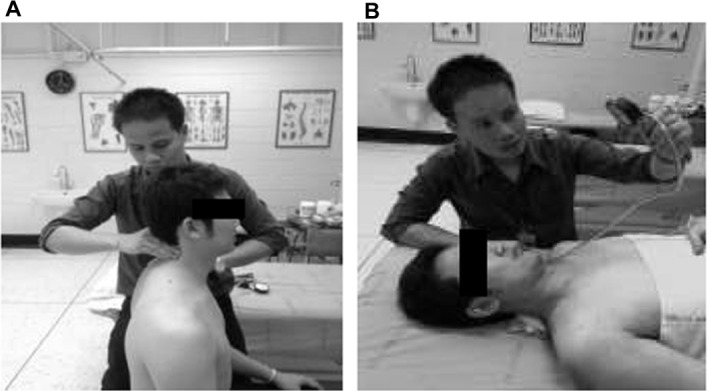
(A) Semispinalis cervicis training-exercise group: resisted contraction. (B) Deep cervical flexor training, using pressure biofeedback.
Deep cervical flexor-training group
Deep cervical flexor exercise is a low-load exercise focused on deep cervical flexor muscles, as described by Jull et al.19 This exercise targets the deep flexor muscles of the cervical region, rather than the superficial flexor muscles. In the current study, deep cervical flexor training was conducted in the supine position on the experimental table. Each participant was asked to move their head slowly to the inner range as if to say, “Yes”. To correct individual exercise technique, participants were guided in their movements by feedback from an air-filled pressure sensor, which was placed in the suboccipital region, ie, the posterior neck. The baseline of the pressure sensor was set to 20 mmHg inflation. Subjects were guided by the researcher to familiarize them with the deep cervical flexor exercise. The deep cervical flexor-exercise procedure was correct when performed without contraction of the superficial neck-flexor muscles. The action of superficial neck muscles was monitored by researcher palpation. Next, participants were assessed individually for their ability to perform the deep cervical flexor exercises correctly without provocation of neck pain. This assessment was performed at the highest incremental level of pressure appropriate for each individual (22, 24, 26, 28, or 30 mmHg; Figure 2B). The participants were instructed to perform the exercise ten times per set, with a short rest. A 30-second rest was allowed between sets. The exercise program was performed under supervision of the researcher twice per week. Participants were trained to perform deep cervical flexor exercises at the same range of motion as the exercise protocol without the air-filled pressure sensor, and each participant was instructed to train with this exercise twice per day at home.
Control group (usual care)
In this study, usual care was treatment deemed appropriate by the physical therapists using any general exercise, including stretching and upper-limb-strengthening exercises, modalities, manual therapy, or electrotherapy within the hospital.33 Participants randomized to usual care were not eligible to perform the exercises performed in the semispinalis cervicis-training and deep cervical flexor-training groups. Participants received usual care over 10–12 treatment appointments within 6 weeks. In the usual-care group, subjects received 20–30 minutes for each physiotherapy appointment.
Outcome measurements
Functional disability
As a primary outcome, the perceived level of disability due to subjects’ neck pain was assessed with the NDI-TH.30 This is a form of the NDI that has been translated into the Thai language and validated, and its internal consistency is high (intraclass correlation coefficient 0.85).30 It consists of ten sections: seven sections related to daily living activity, two sections related to pain, and one section related to concentration. Each item is scored from 0 to 5. A score of 0 represents the highest level of function, while a score of 5 represents the lowest level of function. Total scores are shown as a percentage of NDI-TH. A high score corresponds to a high degree of disability.
Neck-pain intensity
The level of pain intensity was measured using the NPS, an 11-point scale ranging from 0 to 10. The 0 represents no pain and 10 represents “the worst pain imaginable”. Subjects were asked to mark the number on the NPS corresponding to their neck-pain intensity level. The NPS has high validity to measure pain intensity.31
CV angle
CV angle was measured using a digital camera, with participants standing. The digital camera recorded the CV angle at a distance of 200 cm from the participant and was fixed on a 30 cm-wide tripod.34 The CV angle-measurement technique involved measuring from a line drawn between the tragus of the ear to the spinous process of the seventh vertebra (C7) and intersected an imaginary horizontal line that passed C7. This technique shows high reliability (intraclass correlation coefficient 0.94).35,36 Combinations of palpations were taken to place surface markers on the skin over the spinous process, including counting the cervical spinous process from the occiput to C7, and passive movements extending the cervical spine were used to find C7.36 For this protocol, tape was placed on the participants’ skin directly over the seventh cervical spinous process and tragus of the right ear.
Neck strength
Neck strength consisting of neck-flexor and extensor-muscle strength was measured using a dynamometer. Neck-extensor strength was measured in the prone position on the experimental table with the subject’s shoulder supported at the edge of the examination table and their head just over the edge of the examination table, causing their muscles to work against gravity. A Velcro strap was used to fix the upper thoracic spine. Participants were asked to hold their head in the neutral position. Then, the researcher placed the handheld dynamometer on the subjects’ vertebral arch of the second cervical vertebra (C2) and applied force in the cervical flexion direction. Participants were asked to match the resistance in the extension direction (Figure 3A). For this protocol, a handheld dynamometer was placed on C2 to stimulate activation of the semispinalis cervicis muscle. A previous study suggested that isometric resistance exercise at the level of the second cervical vertebra can achieve relative isolation of the semispinalis cervicis muscle.31
Figure 3.
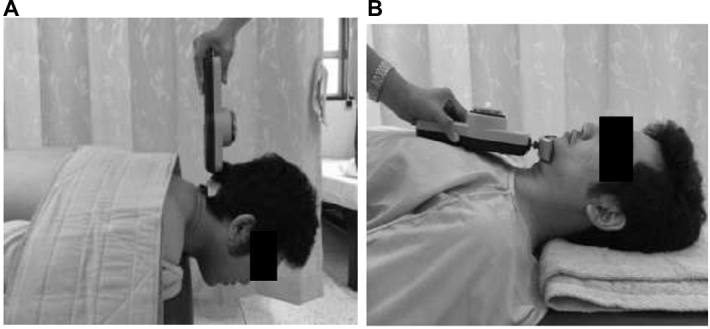
Neck strength.
Notes: (A) Measuring neck-extensor-muscle strength with dynamometer: Velcro strap across shoulders stabilizes upper body. (B) Measuring neck flexor-muscle strength with dynamometer.
Deep-neck-flexor strength was measured in a supine position on the experimental table. The researcher placed the handheld dynamometer on the mandible. Participants were instructed to nod their head such that their jaw pushed down onto the handheld dynamometer and to hold the resistance in the craniocervical flexion direction (nodding) against the handheld dynamometer (Figure 3B). At the same time, the researcher palpated the sternocleidomastoid muscle to monitor and provide feedback to prevent superficial flexor activation. For both measurements, only one maximum-strength test was performed to minimize the potential for reduced-force output with increased cervical pain due to repeated testing. Both measurements were performed without provocation of neck pain.
Sample size
Sample-size calculations were based on detecting a difference in the mean NDI of 4.2 points and a pooled variance estimation (σ2=33.2 between the semispinalis cervicis and the control group at 6 weeks immediately after the pilot study. The sample size was calculated statistically using the t-test formula, with test power 0.90 and α=0.05. Allowing for a dropout rate of 15%, we required at least 18 participants in this study.
Statistical analysis
Shapiro–Wilk tests were used to test the ANOVA assumption of normality for responses from the three cohorts of subjects. Univariate analysis of covariance (ANCOVA) (adjusted for baseline) was used to determine differences between groups for the NDI-TH, CV angle, and neck-muscle strength. When comparing estimated marginal means (adjusted for baseline), Bonferroni corrections were used. P<0.05 was considered statistically significant
Results
Demographic data of the participants are shown in Table 1. These data were similar in each group for age, height, weight, and pain duration.
Table 1.
Demographic and baseline data of participants
| Variables | SCT group | DCF group | Control group |
|---|---|---|---|
|
| |||
| Age (years) | 43.27±9.68 | 43.5±12 | 42.05±8.48 |
| Sex (male/female) | 1/17 | 2/16 | 3/15 |
| Weight (kg) | 61.16±14.77 | 59.38±11.13 | 59±7.34 |
| High (cm) | 159.5±4.59 | 158.72±5.78 | 159.5±7.44 |
| Duration of pain (months) | 11.61±7.47 | 10.55±6.31 | 16.44±37.7 |
| Side of pain (left/right) | 15/15 | 14/15 | 16/15 |
| NDI | 30±10.82 | 27.33±14.93 | 23.11±8.54 |
| NPS | 4.77±1.89 | 4.61±1.71 | 4.05±0.87 |
| Craniovertebral angle (°) | 47±4.34 | 48.22±4.65 | 47.55±4.03 |
| Neck-extensor strength (kg) | 4.50±0.81 | 4.50±0.40 | 4.64±0.41 |
| Neck-flexor strength (kg) | 1.66±0.19 | 1.82±0.19 | 1.85±0.24 |
Abbreviations: DCF, deep cervical flexors; NDI, Neck Disability Index; NPS, numeric pain scale; SCT, semispinalis cervicis training.
Functional ability in the semispinalis cervicis-training and the deep cervical flexor-training groups improved significantly more than in the control group on NDI-TH scores after 6 weeks of training and at 1- and 3-month follow-up (semispinalis cervicis-training group, P=0.001, P=0.001, and P=0.001, respectively; deep cervical flexor training group, P=0.003, P=0.001, and P=0.004, respectively; Table 2).
Table 2.
Results posttreatment: NDI and NPS scores and craniovertebral angle immediately after 6 weeks training and at 1- and 3-month follow-up
| Mean, adjusted
|
SCT vs DCF
|
SCT vs Con
|
DCF vs Con
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SCT | DCF | Con | Mean difference (95%CI) | P-value | Effect size | Mean difference (95% CI) | P-value | Effect size | Mean difference (95% CI) | P-value | Effect size | |
|
| ||||||||||||
| NDI (%) | ||||||||||||
| Immediate (week 6) | 13.29 | 14.99 | 20.24 | 1.73±1.76 (1.93–5.33) | 0.75 | 0.10 | 6.95±1.53 (3.15–10.76) | 0.001* | 0.25 | 5.25±1.50 (1.52–8.98) | 0.003* | 0.36 |
| 1-month follow-up (week 10) | 13.07 | 15.68 | 21.12 | 2.61±1.28 (−0.55 to 5.87) | 0.13 | 0.12 | 8.05±1.38 (4.81–11.30) | 0.001* | 0.49 | 5.44±1.28 (2.25–8.62) | 0.001* | 0.37 |
| 3-month follow-up (week 10) | 12.97 | 16.62 | 21.69 | 3.65±1.43 (0.09–7.20) | 0.05 | 0.20 | 8.72±1.50 (5.00–12.44) | 0.001* | 0.51 | 5.07±1.47 (1.42–8.72) | 0.004* | 0.33 |
| NPS | ||||||||||||
| Immediate (week 6) | 2.30 | 2.86 | 3.49 | 0.55±0.24 (0.02–1.13) | 0.07 | 0.32 | 1.18±0.23 (0.59–1.77) | <0.001* | 0.58 | 0.63±0.24 (0.05–1.22) | 0.029* | 0.26 |
| 1-month follow-up (week 10) | 2.53 | 2.93 | 3.06 | 0.39±0.22 (−0.16 to 0.95) | 0.25 | 0.32 | 0.53±0.24 (−0.05 to 1.12) | 0.09 | 0.20 | 0.13±0.24 (−0.45 to 0.72) | 1 | 0.20 |
| 3-month follow-up (week 10) | 2.79 | 3.27 | 3.37 | 0.47±0.27 (−0.19 to 1.14) | 0.24 | 0.42 | 0.57±0.28 (−0.13 to 1.28) | 0.14 | 0.22 | 0.10±0.28 (−0.60 to 0.80) | 1 | 0.21 |
| Craniovertebral angle | ||||||||||||
| Immediate (week 6) | 50.41 | 50.78 | 48.18 | 0.36±0.70 (−1.37 to 2.11) | 1 | 0.35 | 2.22±0.70 (0.49–3.96) | 0.008* | 0.50 | 2.59±0.70 (0.85–4.33) | 0.002* | 0.94 |
| 1-month follow-up (week 10) | 50.91 | 51.14 | 48.85 | 0.22±0.71 (−1.52 to 1.97) | 1 | 0.10 | 2.06±0.70 (0.32–3.82) | 0.01* | 0.86 | 2.28±0.70 (0.54–4.02) | 0.006* | 0.76 |
| 3-month follow-up (week 18) | 50.16 | 51.09 | 48.63 | 0.92±0.80 (−1.04 to 2.90) | 0.74 | 0.48 | 1.54±0.79 (–0.42 to 3.49) | 0.17 | 0.35 | 2.46±0.79 (0.5–4.42) | 0.009* | 0.97 |
Note:
P<0.05.
Abbreviations: Con, control; DCF, deep cervical flexor; NDI, Neck Disability Index. NPS, numeric pain scale; SCT, semispinalis cervicis training.
Neck-pain scores in the semispinalis cervicis-training group and the deep cervical flexor-training group improved significantly more than in the control group on the NPS after 6 weeks of training (P<0.001 and P=0.029, respectively), but not at 1- and 3-month follow-up (Table 2). For the CV angle, the semispinalis cervicis-training group improved significantly more than the control group only immediately after 6 weeks of training (P=0.008) and at 1-month (P=0.01) follow-up. The deep cervical flexor-training group improved significantly more than the control group in CV angle after 6 weeks of training (P=0.002), at 1-month follow-up (P=0.006), and at 3-month (P=0.009) follow-up (Table 2).
Neck-muscle strength in the semispinalis cervicis-training group improved significantly more than the control group in neck-extensor strength after 6 weeks of training (P=0.04), at 1-month follow-up (P=0.02), and at 3-month (P=0.002) follow-up. The semispinalis cervicis-training group improved significantly more than the deep cervical flexor group in neck-extensor strength after 6 weeks of training (P=0.02) and at 3-month (P=0.01) follow-up (Table 3). However, there was no significant difference in neck-extensor strength between the deep cervical flexor-training group and the control group (P>0.05). The deep cervical flexor-training group improved significantly more than the control group in deep-neck-flexor strength after 6 weeks of training (P=0.002) and at 1-month (P=0.001) and 3-month (P=0.001) follow-up. The deep cervical flexor-training group improved significantly more than the semispinalis cervicis-training group in deep-neck-flexor strength at 1-month (P=0.03) follow-up, but not at other time points (Table 3). However, there was no significant difference in neck-flexor strength between the semispinalis cervicis-training group and the control group (P>0.05).
Table 3.
Results immediately after 6 weeks training and at 1- and 3-month follow-up after neck-extensor and neck-flexor strength training
| Mean, adjusted
|
SCT vs DCF
|
SCT vs Con
|
DCF vs Con
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SCT | DCF | Con | Mean difference (95%CI) | P-value | Effect size | Mean difference (95% CI) | P-value | Effect size | Mean difference (95% CI) | P-value | Effect size | |
|
| ||||||||||||
| Neck-extensor strength (kg) | ||||||||||||
| Immediate (week 6) | 5.18 | 4.78 | 4.82 | 0.4±0.14 (0.04–0.76) | 0.02* | 0.73 | 0.36±0.15 (0–0.72) | 0.04* | 0.61 | 0.04±0.15 (−0.31 to 0.4) | 1 | 0.23 |
| 1-month follow-up (week 10) | 5.22 | 4.81 | 4.72 | 0.4±0.18 (−0.04 to 0.85) | 0.09 | 0.63 | 0.49±0.18 (0.04–0.95) | 0.02* | 0.82 | 0.09±0.18 (−0.36 to 0.55) | 1 | 0.15 |
| 3-month follow-up (week 18) | 5.25 | 4.81 | 4.70 | 0.44±0.15 (0.07–0.81) | 0.01* | 0.84 | 0.55±0.15 (0.17–0.93) | 0.002* | 0.83 | 0.11±0.15 (−0.26 to 0.50) | 1 | 0.20 |
|
| ||||||||||||
| Neck-flexor strength (kg) | ||||||||||||
| Immediate (week 6) | 1.89 | 2.07 | 1.77 | 0.18±0.09 (−0.03 to 0.4) | 0.12 | 0.77 | 0.12±0.09 (−0.09 to 0.34) | 0.47 | 0.40 | 0.31±0.08 (0.1–0.5) | 0.002* | 0.90 |
| 1-month follow-up (week 10) | 1.84 | 2.05 | 1.71 | 0.21±0.08 (0.02–0.39) | 0.03* | 0.85 | 0.13±0.08 (−0.06 to 0.32) | 0.28 | 0.42 | 0.34±0.07 (0.16–0.52) | 0.001* | 0.95 |
| 3-month follow-up (week 18) | 1.92 | 2.11 | 1.72 | 0.18±0.1 (−0.05 to 0.42) | 0.17 | 0.70 | 0.19±0.1 (0.04–0.43) | 0.15 | 0.48 | 0.38±0.09 (0.15–0.61) | 0.001* | 0.92 |
Note:
P<0.05.
Abbreviations: Con, control; DCF, deep cervical flexor; SCT, semispinalis cervicis training.
Discussion
The results supported our hypothesis that both semispinalis cervicis- and deep cervical flexor-training exercise resulted in reduced functional disability. The results of this study are consistent with previous studies on individuals with chronic neck pain.19–24,37,38 Researchers have investigated the effectiveness of craniocervical flexor training in chronic neck-pain patients, and found that functional disability was reduced after training.20,22–24,37,38 Our results indicate that specific exercise of the semispinalis cervicis muscles is supported for the treatment of chronic mechanical neck pain. The cervical extensor muscles are believed to be equally as important (as the flexor muscles) in the rehabilitation of individuals with chronic mechanical neck pain.25 Therefore, the activation of the deep cervical extensors should be emphasized in rehabilitation in chronic mechanical neck-pain patients. Research suggests that isometric resistance exercise at the cervical vertebra can improve activation of semispinalis cervicis muscles relative to splenius capitis.10 The results of the current study support the finding that semispinalis cervicis training with resistance applied at the second vertebral arch level can reduce functional disability and demonstrate a significant increase in neck-extensor-muscle strength when compared with the control group, which is important in the rehabilitation of individuals with chronic mechanical neck pain. However, although the difference in NDI-score change between the two groups was 6.95%, 8.05%, and 8.72% at 6 weeks, 1-month follow-up, and 3-month follow-up, respectively, this difference was lower than the minimal detectable change of the NDI – 10%.39 Therefore, although the difference in improvement between groups for the NDI was statistically significant, the gap could be of little importance clinically. Further qualitative study should be undertaken.
The current study showed that deep cervical flexor-muscle exercise significantly reduced pain intensity immediately at the conclusion of 6 weeks of training. Craniocervical flexor training enhanced the ability and improved neuromuscular control of deep cervical flexor muscles, including the longus colli and longus capitis, and reduced pain intensity in chronic neck-pain patients. This finding in the current study was in agreement with previous studies that have reported pain-intensity reduction after craniocervical flexor training in chronic neck-pain patients.20–24
The current study showed that the semispinalis cervicis (extensor)-exercise group experienced significantly reduced pain intensity immediately following 6 weeks of training. Specific exercises for the deep cervical extensors, especially the semispinalis cervicis muscle, have not been widely investigated. A recent study found that isometric head/neck extension performed in the head-neutral position activated both deep and superficial neck-extensor muscles, measured by muscle functional magnetic resonance imaging at the level of the second cervical vertebra.44 However, the results of the present study are not comparable with those findings, because pain intensity was not measured in the previous study.
Specific deep cervical muscle exercises may improve neuromuscular function and restore sensorimotor control of the cervical spine.14 One possible mechanism to describe the effect of exercise in reducing pain is that muscle contraction from the exercise training stimulated mechanoreceptors, including the muscle spindle, Golgi tendon organ, and pro-prioceptors of joints. Signals from the receptors cause the release of endogenous opioids and stimulate the release of endorphins from the pituitary gland.46,47
The findings of the current study revealed that the deep cervical flexor (longus colli and longus capitis muscles)-training group showed a significant improvement in CV angle compared with the control group at all follow-up periods. The results of the current study are consistent with previously reported studies about chronic neck-pain patients.40,41 To our knowledge, forward head posture (FHP) is the most common abnormality in neck-pain patients. FHP increases lordosis of the lower cervical spine, causing an increased extension of the middle cervical spine and flexion of the lower cervical spine, resulting in cervical muscle imbalance.42 In a previous EMG study, the concept of craniocervical flexor-exercise training was to focus more specifically on motor control and to train coordination between superficial and deep layers of cervical muscles.18–21 The focus on the longus colli and longus capitis muscles is to control head movement and stabilize the cervical spine. For these, craniocervical flexor-exercise training may eventually alter lordosis of the cervical spine, leading to improved FHP in individuals with neck pain. The results of the current study may confirm that craniocervical flexor training is essential for improvement of the CV angle in chronic mechanical neck pain patients.
The current study investigated the effect of muscle training, and showed that the deep cervical flexor-muscle exercise-training group demonstrated significant increases in neck-flexor-muscle strength when compared with the control group. This finding is consistent with the results of a previously reported study, where 6 weeks of craniocervical flexor training significantly improved isometric craniocervical flexor-muscle performance in chronic neck-pain patients.17 Patients with neck pain demonstrated a reduction in deep cervical flexor-muscle strength.43 The deep cervical muscles, including the longus colli and longus capitis, are important to stabilize the cervical spine. Therefore, specific exercise for deep cervical muscles should be emphasized.
In addition, the cervical extensor muscles are believed to be equally as important (as the flexor muscles) in the rehabilitation of patients with chronic mechanical neck pain.25 The current study demonstrated a significant increase in neck-extensor-muscle strength when compared with the control group. Previous study results have demonstrated that isometric exercises of the head/neck activate both deep and superficial extensor muscles.44 Specific exercises for the deep cervical extensors have not been extensively investigated. A recent muscle functional magnetic resonance-imaging study showed that an isometric head/neck extension performed at 20% of the maximum voluntary force activated both the deep and superficial extensors.44 One recent study reported that isometric resisted exercise at the second cervical vertebra can improve activation of semispinalis cervicis muscles relative to the splenius capitis muscle.45 The results of this study are consistent with previous studies. The current study supported semispinalis cervicis-exercise training with resistance applied at the second vertebral arch level to increase neck-extensor-muscle strength in chronic mechanical neck pain. Furthermore, the results from the current study confirmed that the neuromuscular control and morphological adaptations of deep cervical muscles did not automatically improve after pain or functional disability reduction in order to improve muscle strength. Therefore, exercise training should be focused to alter specific muscle impairment, especially deep cervical flexors and extensors muscles (based on assessment).
The NDI-TH in the current study showed a positive correlation with the NPS and CV angle (r=0.54, r=0.2, respectively) and showed a negative correlation with neck-extensor and -flexor strength (r=−0.22, r=−0.1, respectively) in semi-spinalis cervicis-exercise training. The NDI-TH showed a positive correlation with NPS and CV angle (r=0.38, r=0.26, respectively) and a negative correlation with neck-extensor and -flexor strength (r=−0.44, r=−0.1, respectively) in deep cervical flexor training.
Limitations
There are some limitations in the current study. First, we assessed only functional disability, CV angle, and neck strength. Future studies should measure other clinical outcomes to describe effects of this exercise on sensory and motor function in chronic neck pain, such as joint proprioception, balance, and muscle activity.16,17 Second, the current study measured only the global muscle strength of neck-extensor and -flexor muscles and not activation or changes in muscle properties of the deep cervical muscles. To extend the results of this study, further studies using EMG to measure activation of cervical muscles or ultrasound imaging to measure cervical muscle tightness and change in cross-sectional areas of the deep cervical muscles in chronic mechanical neck-pain patients would provide additional objective findings.
Conclusion
Semispinalis cervicis-training and deep cervical flexor-training outcomes showed benefits over usual-care outcomes. Specific exercise with a focus on deep cervical muscles may be an important intervention to treat patients with chronic mechanical neck pain. Exercise training should focus on specific impairments of cervical muscles, especially the deep cervical muscles.
Data sharing statement
The authors will allow sharing of participant data, such as functional disability and pain intensity. The data will be available for anyone who wishes to access them for any purpose. The data will be accessible from immediately following publication to 6 months after publication, and contact should be made via the principal investigator rungthiprt@gmail.com.
Acknowledgments
This study was supported by a grant from the Research Center in Back, Neck, Other Joint Pain, and Human Performance (BNOJPH), Khon Kaen University (Thavatchai/2560).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Côté P, Cassidy JD, Carroll L. The Saskatchewan health and back pain survey. the prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 1998;23(15):1689–1698. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Hogg-Johnson S, van der Velde G, Carroll LJ, et al. Bone and joint decade 2000–2010 Task Force on neck pain and its associated disorders. The burden and determinants of neck pain in general population: results of the bone and joint decade 2000–2010 Task Force on neck pain and it associated disorders. Spine (Phila Pa 1976) 2008;33(4 suppl):S 39–S51. doi: 10.1097/BRS.0b013e31816454c8. [DOI] [PubMed] [Google Scholar]
- 3.Korthals-de Bos IB, Hoving JL, van Tulder MW, et al. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial. BMJ. 2003;326(7395):911. doi: 10.1136/bmj.326.7395.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in general population: results of the bone and joint decade 2000–2010 Task Force on neck pain and it associated disorders. Spine (Phila Pa 1976) 2008;33(4 suppl):S39–S51. doi: 10.1097/BRS.0b013e31816454c8. [DOI] [PubMed] [Google Scholar]
- 5.Barton PM, Hayes KC. Neck flexor muscle strength, efficiency, and relaxation times in normal subjects and subjects with unilateral neck pain and headache. Arch Phys Med Rehabil. 1996;77(7):680–687. doi: 10.1016/s0003-9993(96)90008-8. [DOI] [PubMed] [Google Scholar]
- 6.Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther. 2004;9(2):89–94. doi: 10.1016/S1356-689X(03)00086-9. [DOI] [PubMed] [Google Scholar]
- 7.Falla D, Jull G, Hodges PW. Feedforward activity of the cervical flexor muscles during voluntary arm movements is delayed in chronic neck pain. Exp Brain Res. 2004;157(1):43–48. doi: 10.1007/s00221-003-1814-9. [DOI] [PubMed] [Google Scholar]
- 8.Cagnie B, Cools A, De Loose V, Cambier D, Danneels L. Differences in isometric neck muscle strength between healthy controls and women with chronic neck pain: the use of a reliable measurement. Arch Phys Med Rehabil. 2007;88(11):1441–1445. doi: 10.1016/j.apmr.2007.06.776. [DOI] [PubMed] [Google Scholar]
- 9.O’Leary S, Cagnie B, Reeve A, Jull G, Elliott JM. Is there altered activity of the extensor muscles in chronic mechanical neck pain? a functional magnetic resonance imaging study. Arch Phys Med Rehabil. 2011;92(6):929–934. doi: 10.1016/j.apmr.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 10.Schomacher J, Farina D, Lindstroem R, Falla D. Chronic trauma-induced neck pain impairs the neural control of the deep semispinailscervicis muscle. ClinNeurophysiol. 2012;123(123):1403–1408. doi: 10.1016/j.clinph.2011.11.033. [DOI] [PubMed] [Google Scholar]
- 11.Kristjansson E. Reliability of ultrasonography for the cervical multifidus muscle in asymptomatic and symptomatic subjects. Man Ther. 2004;9(2):83–88. doi: 10.1016/S1356-689X(03)00059-6. [DOI] [PubMed] [Google Scholar]
- 12.Elliott J, Jull G, Noteboom JT, Darnell R, Galloway G, Gibbon WW. Fatty infiltration in the cervical extensor muscles in persistent whiplash-associated disorders: a magnetic resonance imaging analysis. Spine (Phila Pa 1976) 2006;31(22):E847–E855. doi: 10.1097/01.brs.0000240841.07050.34. [DOI] [PubMed] [Google Scholar]
- 13.Elliott J, Jull G, Noteboom JT, Galloway G. MRI study of the cross-sectional area for the cervical extensor musculature in patients with persistent whiplash associated disorders (WAD) Man Ther. 2008;13(3):258–265. doi: 10.1016/j.math.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 14.Falla D, Farina D. Neural and muscular factors associated with motor impairment in neck pain. Curr Rheumatol Rep. 2007;9(6):497–502. doi: 10.1007/s11926-007-0080-4. [DOI] [PubMed] [Google Scholar]
- 15.Kay TM, Gross A, Goldsmith CH, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2012;8:CD004250. doi: 10.1002/14651858.CD004250.pub4. [DOI] [PubMed] [Google Scholar]
- 16.Leaver AM, Refshauge KM, Maher CG, McAuley JH. Conservative interventions provide short-term relief for non-specific neck pain: a systematic review. J Physiother. 2010;56(2):73–85. doi: 10.1016/s1836-9553(10)70037-0. [DOI] [PubMed] [Google Scholar]
- 17.O’Leary S, Jull G, Kim M, Vicenzino B. Specificity in retraining craniocervical flexor muscle performance. J Orthop Sports Phys Ther. 2007;37(1):3–9. doi: 10.2519/jospt.2007.2237. [DOI] [PubMed] [Google Scholar]
- 18.O’Leary S, Jull G, Kim M, Uthaikhup S, Vicenzino B. Training mode-dependent changes in motor performance in neck pain. Arch Phys Med Rehabil. 2012;93(7):1225–1233. doi: 10.1016/j.apmr.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 19.Jull G, Trott P, Potter H, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27(17):1835–1843. doi: 10.1097/00007632-200209010-00004. [DOI] [PubMed] [Google Scholar]
- 20.Jull GA, Falla D, Vicenzino B, Hodges PW. The effect of therapeutic exercise on activation of the deep cervical flexor muscles in people with chronic neck pain. Man Ther. 2009;14(6):696–701. doi: 10.1016/j.math.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Falla D, Jull G, Hodges P. Training the cervical muscles with prescribed motor tasks does not change muscle activation during a functional activity. Man Ther. 2008;13(6):507–512. doi: 10.1016/j.math.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Falla D, O’Leary S, Farina D, Jull G. The change in deep cervical flexor activity after training is associated with the degree of pain reduction in patients with chronic neck pain. Clin J Pain. 2012;28(7):628–634. doi: 10.1097/AJP.0b013e31823e9378. [DOI] [PubMed] [Google Scholar]
- 23.Borisut S, Vongsirinavarat M, Vachalathiti R, Sakulsriprasert P. Effects of strength and endurance training of superficial and deep neck muscles on muscle activities and pain levels of females with chronic neck pain. J Phys Ther Sci. 2013;25(9):1157–1162. doi: 10.1589/jpts.25.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lluch E, Schomacher J, Gizzi L, Petzke F, Seegar D, Falla D. Immediate effects of active cranio-cervical flexion exercise versus passive mobilisation of the upper cervical spine on pain and performance on the cranio-cervical flexion test. Manual Therapy. 2014;19(1):25–31. doi: 10.1016/j.math.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 25.O’Leary S, Falla D, Elliott JM, Jull G. Muscle dysfunction in cervical spine pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009;39(5):324–333. doi: 10.2519/jospt.2009.2872. [DOI] [PubMed] [Google Scholar]
- 26.O’Leary S, Cagnie B, Reeve A, Jull G, Elliott JM. Is there altered activity of the extensor muscles in chronic mechanical neck pain? A functional magnetic resonance imaging study. Arch Phys Med Rehabil. 2011;92(6):929–934. doi: 10.1016/j.apmr.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 27.Fernández-de-Las-Peñas C, Palomeque-del-Cerro L, Rodríguez-Blanco C, Gómez-Conesa A, Miangolarra-Page JC. Changes in neck pain and active range of motion after a single thoracic spine manipulation in subjects presenting with mechanical neck pain: a case series. J Manipulative Physiol Ther. 2007;30(4):312–320. doi: 10.1016/j.jmpt.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 28.Saavedra-Hernández M, Arroyo-Morales M, Cantarero-Villanueva I, et al. Short-term effects of spinal thrust joint manipulation in patients with chronic neck pain: a randomized clinical trial. Clin Rehabil. 2013;27(6):504–512. doi: 10.1177/0269215512464501. [DOI] [PubMed] [Google Scholar]
- 29.Evans R, Bronfort G, Nelson B, Goldsmith CH. Two-year follow-up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine (Phila Pa 1976) 2002;27(21):2383–2389. doi: 10.1097/00007632-200211010-00013. [DOI] [PubMed] [Google Scholar]
- 30.Uthaikhup S, Paungmali A, Pirunsan U. Validation of Thai versions of the Neck Disability Index and neck pain and disability scale in patients with neck pain. Spine (Phila Pa 1976) 2011;36(21):E1415–E1421. doi: 10.1097/BRS.0b013e31820e68ac. [DOI] [PubMed] [Google Scholar]
- 31.Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10(4):390–392. doi: 10.1111/j.1553-2712.2003.tb01355.x. [DOI] [PubMed] [Google Scholar]
- 32.Schomacher J, Petzke F, Falla D. Localised resistance selectively activates the semispinalis cervicis muscle in patients with neck pain. Man Ther. 2012;17(6):544–548. doi: 10.1016/j.math.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 33.McLean SM, Klaber Moffett JA, Sharp DM, Gardiner E. A randomised controlled trial comparing graded exercise treatment and usual physiotherapy for patients with non-specific neck pain (the GET UP neck pain trial) Man Ther. 2013;18(3):199–205. doi: 10.1016/j.math.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 34.Silva AG, Punt TD, Sharples P, Vilas-Boas JP, Johnson MI. Head posture and neck pain of chronic nontraumatic origin: a comparison between patients and pain-free persons. Arch Phys Med Rehabil. 2009;90(4):669–674. doi: 10.1016/j.apmr.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 35.Lee CH, Lee S, Shin G. Reliability of forward head posture evaluation while sitting, standing, walking and running. Hum Mov Sci. 2017;55(10):81–86. doi: 10.1016/j.humov.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 36.Robinson R, Robinson HS, Bjørke G, Kvale A. Reliability and validity of a palpation technique for identifying the spinous processes of C7 and L5. Man Ther. 2009;14(4):409–414. doi: 10.1016/j.math.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 37.Ris I, Søgaard K, Gram B, Agerbo K, Boyle E, Juul-Kristensen B. Does a combination of physical training, specific exercises and pain education improve health-related quality of life in patients with chronic neck pain? A randomised control trial with a 4-month follow up. Man Ther. 2016;26(12):132–140. doi: 10.1016/j.math.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 38.Ludvigsson ML, Peterson G, O’Leary S, Dedering Å, Peolsson A. The effect of neck-specific exercise with, or without a behavioral approach, on pain, disability, and self-efficacy in chronic whiplash-associated disorders: a randomized clinical trial. Clin J Pain. 2015;31(4):294–303. doi: 10.1097/AJP.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cleland JA, Glynn P, Whitman JM, Eberhart SL, MacDonald C, Childs JD. Short-term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: a randomized clinical trial. Phys Ther. 2007;87(4):431–440. doi: 10.2522/ptj.20060217. [DOI] [PubMed] [Google Scholar]
- 40.Gupta BD, Aggarwal S, Gupta B, Gupta M, Gupta N. Effect of deep cervical flexor training vs. Conventional isometric training on forward head posture, pain, Neck Disability Index in dentists suffering from chronic neck pain. J Clin Diagn Res. 2013;7(10):2261–2264. doi: 10.7860/JCDR/2013/6072.3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim BB, Lee JH, Jeong HJ, Cynn HS. Effects of suboccipital release with craniocervical flexion exercise on craniocervical alignment and extrinsic cervical muscle activity in subjects with forward head posture. J Electromyogr Kinesiol. 2016;30(10):31–37. doi: 10.1016/j.jelekin.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 42.Yoo WG, An DH, Dh A. The relationship between the active cervical range of motion and changes in head and neck posture after continuous VDT work. Ind Health. 2009;47(2):183–188. doi: 10.2486/indhealth.47.183. [DOI] [PubMed] [Google Scholar]
- 43.Falla DL, Jull GA, Hodges PW. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine (Phila Pa 1976) 2004;29(19):2108–2114. doi: 10.1097/01.brs.0000141170.89317.0e. [DOI] [PubMed] [Google Scholar]
- 44.Elliott JM, O’Leary SP, Cagnie B, Durbridge G, Danneels L, Jull G. Craniocervical orientation affects muscle activation when exercising the cervical extensors in healthy subjects. Arch Phys Med Rehabil. 2010;91(9):1418–1422. doi: 10.1016/j.apmr.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 45.Schomacher J, Erlenwein J, Dieterich A, Petzke F, Falla D. Can neck exercises enhance the activation of the semispinalis cervicis relative to the splenius capitis at specific spinal levels? Man Ther. 2015;20(5):694–702. doi: 10.1016/j.math.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 46.Koltyn KF, Brellenthin AG, Cook DB, Sehgal N, Hillard C. Mechanisms of exercise-induced hypoalgesia. J Pain. 2014;15(12):1294–1304. doi: 10.1016/j.jpain.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kami K, Tajima F, Senba E. Exercise-induced hypoalgesia: potential mechanisms in animal models of neuropathic pain. Anat Sci Int. 2017;92(1):79–90. doi: 10.1007/s12565-016-0360-z. [DOI] [PubMed] [Google Scholar]