Abstract
Objectives:
To describe the architecture, design, and testing of an innovative mobile application (MEDIvate®) that facilities accurate sharing of medication lists with linked education.
Setting:
The deployment and testing of this app occurred in both the community and hospital settings in Pittsburgh, PA.
Practice innovation:
MEDIvate® is an iOS smartphone application and cloud architecture for patients and providers to keep medication and vaccine lists accurate by providing a method and tool to easily exchange these data. Medications are added directly to the app from the EHR or by the patient manually. Quick response (QR) code technology is used to trigger the secure transfer and sharing of medications on-demand using the HL-7 FHIR based data transfer. An iterative, user-centered design process involving patients and student pharmacists practicing in community settings was used to develop and refine functionality.
Practice description:
Adults with an iPhone were approached for participation in the design and evaluation of MEDIvate®. Its functionality and integration into clinical workflow at hospital discharge or vaccine administration in the community were determined.
Evaluation:
In the community setting, interviews of pharmacists were conducted. In the hospital, metrics of study participation and experience with app deployment were determined.
Results:
The app was deployed in the community for patients that received vaccinations. Interviews provided insight into barriers and logistics for successful engagement. The app was integrated into hospital workflow and demonstrated interoperability with the inpatient EHR. Thirteen patients were provided the app before discharge. Engagement with the app was evident through medication list shares, education access, and changes to medication lists. Patients noted strong agreement with use of the app to learn more about the purpose and side effects of medications prescribed.
Conclusion:
A mobile app to achieve medication and vaccine list portability was successfully designed and integrated into the inpatient and community settings.
Background
Approximately two million adverse drug events, 100,000 patient deaths, and $290 billion in healthcare expenditures are attributed to medication use problems annually.1 Adverse medication outcomes are driven by non-adherence and poor reconciliation during transitions of care which lead to medication errors.3,4 Approximately 30% to 50% of U.S. adults are non-adherent, resulting in 33%-69% of medication-related hospitalizations and 23% of all nursing home admissions.4,5 Inadequate medication reconciliation, particularly during the time of hospital discharge, results in half of all hospital-related medication errors.6 Medication errors can result from frequent medication or dosing changes and discordant medication lists as patients transition across settings and encounter different providers and pharmacies. For example, 90% of patients with heart failure (HF) take at least 4 medications and the average patient takes 11 different medications.7 Similarly, one-time medication administrations, such as vaccinations, are also poorly tracked as patients move between providers7,8
The uptake of health-focused personal technology is expanding rapidly, but few products target medication outcomes.9,10 Patients remain ultimately responsible for updating and maintaining accurate medication lists, and for adhering to complex medical regimens. However, medication list information has historically been compartmentalized within institutional or pharmacy-specific electronic health records (EHRs). To improve interoperability, the 21st Century Cures Act that was passed in 2016 included certification provisions that penalized EHR vendors who inhibit the exchange of electronic health information.11 Similarly, the Fast Healthcare Interoperability Resource (FHIR) specification provides a standard for the exchange of health information.12,13 The progressing implementation of these standards, and the platforms for development on them, represent new opportunities to connect users to health information, such as medication lists.12 Further, the entry of consumer-focused companies like Apple into the space show the increasing interest in healthcare technology by consumers.14
Beyond the current medication list itself, access to accurate and relevant drug information is also needed to avert medication problems. Personalized education, the use of feedback and reinforcement, and providing rewards may prove successful at improving medication outcomes when deployed through technology.15,16 Persuasive technologies can also be applied to achieve enhanced patient engagement and to transfer knowledge regarding the purpose and benefits of medications.7,17,18 The prevalence and application of these persuasive technologies make it an attractive method to engage patients.
The objective of this report is to describe the architecture, design, and early testing of an innovative mobile application (MEDIvate®) that facilities the accurate sharing of medication lists with linked, individualized education. Specifically, our aim was to use patient and community pharmacist input to inform iterative design and optimal integration workflows. We then assessed process metrics and data accuracy in community and hospital settings for transferring individual prescription-level (vaccine) data and entire discharge medication lists, to patients in employee vaccination clinics and patients discharged from a cardiology service, respectively.
Methods
Practice innovation
Technology overview and architecture
MEDIvate® is an iOS smartphone application and cloud architecture for patients and providers to keep medication lists accurate and up-to-date by providing a method and tool to easily exchange these data. Current medications can be added directly to the app from the EHR or by the patient manually. EHR medication data download is achieved through a process where the clinician triggers the initial data output to make it available to a patient (Figure 1). Through ubiquitous quick response (QR) code technology, patients can then trigger the secure transfer of their personal medication history using a scanner built into application. Furthermore, this same system enables downstream sharing with subsequent healthcare providers. The expectation is that digital transfer of data will improve medication list accuracy and will reduce the time typically spent on medication reconciliation tasks using inefficient paper processes to improve transitions of care. To increase patient engagement and provide additional resources, the application also automatically links internally created key drug facts from pharmacist experts within the app as medications are added. Vaccine information is also linked to the Centers for Disease Control and Prevention Vaccine Information Statements (VISs).
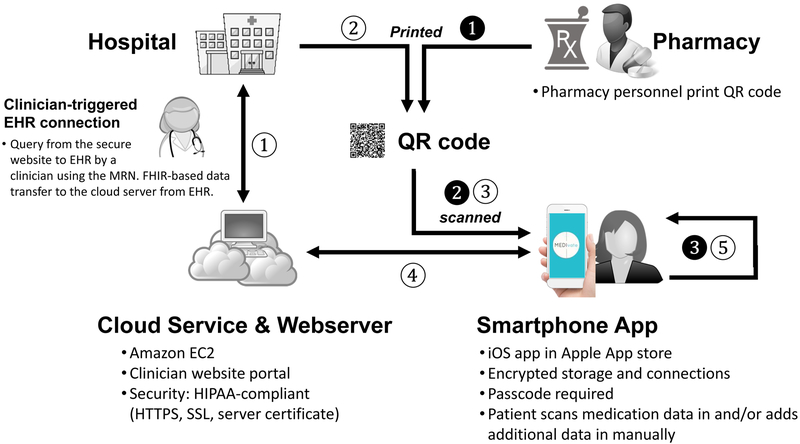
Figure 1: MEDIvate architecture and data flow.
MEDIvate consists of a cloud-based database, Webserver, and iOS smartphone app. Data flows for pharmacy (filled circles) and hospital (open circles) pilots are shown. Community pharmacy prescription data is ❶ printed in a QR code when a prescription (vaccine) is dispensed. ❷ The code is scanned by the patient using app in order to transfer the prescription data. In the hospital, a provider first ① queries the hospital EHR for patient discharge medication lists from the MEDIvate website and the medication list is transferred to the MEDIvate database in the cloud. ② A QR code is printed and ③ when scanned by the patient, ④ the medication list is securely transferred into the patient’s app. The patient may then add additional medications/vaccines manually (❸ and ⑤) and share the list with downstream providers.
In initial development, the cloud-based platform and Apple iOS smartphone application (Figure 1) was prototyped and refined in partnership with Infoshape Software (Pittsburgh, PA). The mobile application compatibility included functionality on iOS 9 or later and was published publicly in the Apple App Store and made available to users free of charge.
Iterative Design
To design the initial user interface, an iterative approach based on user and stakeholder feedback was completed by the staff and students of the Pharmacy Innovations Laboratory at the University of Pittsburgh School of Pharmacy. Using a standard user-centered, design-thinking method, this group identified core requirements and design of the application in order to identify and demonstrate clear value to user needs.19 This process was applied specifically to develop a functional user interface by this same group. Five patient volunteers participated in the initial structured user testing to refine the features and aesthetics of the app. Prioritized functionality was easy maintenance of an active medication list, display of relevant medication information and education, and the ability to share the medication list electronically. The user design was refined by the study team based on feature priority, feasibility, and relevance to end-user needs. The outcome from this process was a concept design for the application (Figure 2). Implementation planning utilized a focus group and app testing session with six student pharmacists with internships in targeted pharmacy settings. These student pharmacists were asked to complete specific tasks that reflected specific scenarios in use of the mobile application, such as adding and accessing new information regarding medication and vaccination history. The experience of completing these tasks were discussed as feedback from students about ease of task completion, barriers, and suggested improvements.
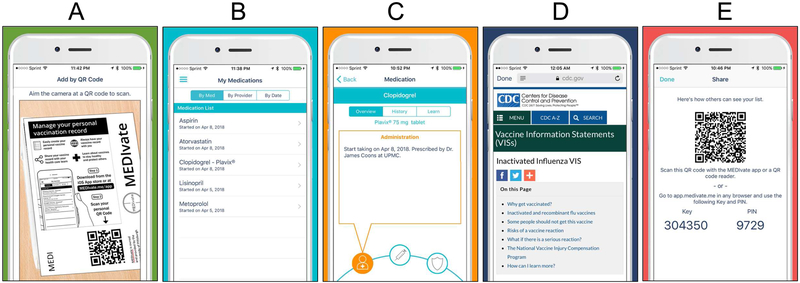
Figure 2: App design and user interfaces.
A. Entry into the app in facilitated by scanning a QR code for single prescription (shown) or an entire medication list; or can be entered manually in the app. B. Once entered, the main app screen is a simple list of routine medications (shown) and a separate listing of vaccinations. C. When a medication or vaccine is selected, users preferred sections for the medication/vaccine, history, and education. Within the medication section, a simple call out design split was used to show provider (shown), medication, and indication subsections. D. When “learn” is selected, users receive either in-app or linked reference education (e.g. vaccine information statement) (shown). E. For downstream sharing of the medication list, a share button creates a new QR code or a secure key/PIN to facilitate this on the MEDIvate website.
Practice description
The proof-of-concept design of the MEDIvate® mobile application, its initial functionality, and the clinical workflows to achieve its successful implementation were evaluated across multiple settings. Approval for each project was obtained from the University of Pittsburgh Institutional Review Board.
Community Phase
We first partnered with a regional grocery store chain pharmacy in western Pennsylvania to customize the app for receipt of prescription-level data (versus entire medication lists). This was prudent based on the practice model of community pharmacies in the U.S. where prescriptions are dispensed individually. A specific use case of vaccinations was selected by pharmacy leadership and the study team to focus the deployment and coincided with a larger project to increase adult vaccinations provided by community pharmacists. Patients who received an influenza vaccination within the pharmacy's employee vaccination clinics were targeted since these patients may seek additional documentation of the prescription/vaccine administration as well as specific vaccine information. This educational information is currently required to be dispensed in the form of a VIS. From a practical standpoint, the anticipated workflow also aligned with the requisite time needed to deploy the app in this setting. The first goal was informatics system integration, to encode key prescription level data in a QR code that could be provided along with the dispensed prescription. Users would first download the app and then scan the code to import these data into the MEDIvate® app and an electronic version of the VIS linked within the app. The second goal was to develop optimal clinical workflows to be both minimally disruptive and to engage patients.
MEDIvate® team members first met with informatics leadership of the pharmacy chain to come to consensus on what data fields needed to be transferred and to map these variables between the pharmacy dispensing system (PDX, Fort Worth, TX) and MEDIvate®. Once specified, these were formatted into a single data string, loaded into the software (printer driver) capable of printing the QR code. A patient directed flyer was designed to be both engaging to patients and to contain the prescription-specific QR code. The QR code size, quality, and data integrity was confirmed to be adequate to exchange the requisite data.
Next, prior to implementation, team members conducted semi-structured interviews with the pharmacy chain’s clinical pharmacists to assess workflow for integrating MEDIvate® into their employee vaccination clinics. It was decided that patients attending the vaccine clinics needed to be introduced to the app and directed how to download it from the Apple App Store. Specific QR codes for the influenza vaccines administered at the clinics could then be scanned by the patient at the time of vaccination. Overall workflow integration requirements included: printing out static QR codes in advance of the particular clinic tailored to the vaccines being administered that day, introduction to the MEDIvate® App (and procedure for downloading during the clinic workflow, and a reminder to scan the QR code following administration, The app was rolled out in employee vaccination clinics held over a one-month period. Semi-structured interviews of participating pharmacists were conducted over the telephone and audio-recorded. Interview questions were based on the Systems Engineering Initiative for Patient Safety (SEIPS) model of work system and patient safety.20 Question domains focused on the person, organization, technology, and tools. Interviews were transcribed verbatim and independently coded by three investigators using a common codebook. Discrepancies were reconciled through discussion. Nvivo 11 (QSR International, Victoria, Australia) was used to store and code each transcript. A qualitative deductive analysis guided by the SEIPS framework, was conducted.21 The research team identified themes and selected illustrative quotes for each theme. Process metrics such as number of users/app downloads and access of vaccine VIS information were also collected.
Hospital Phase
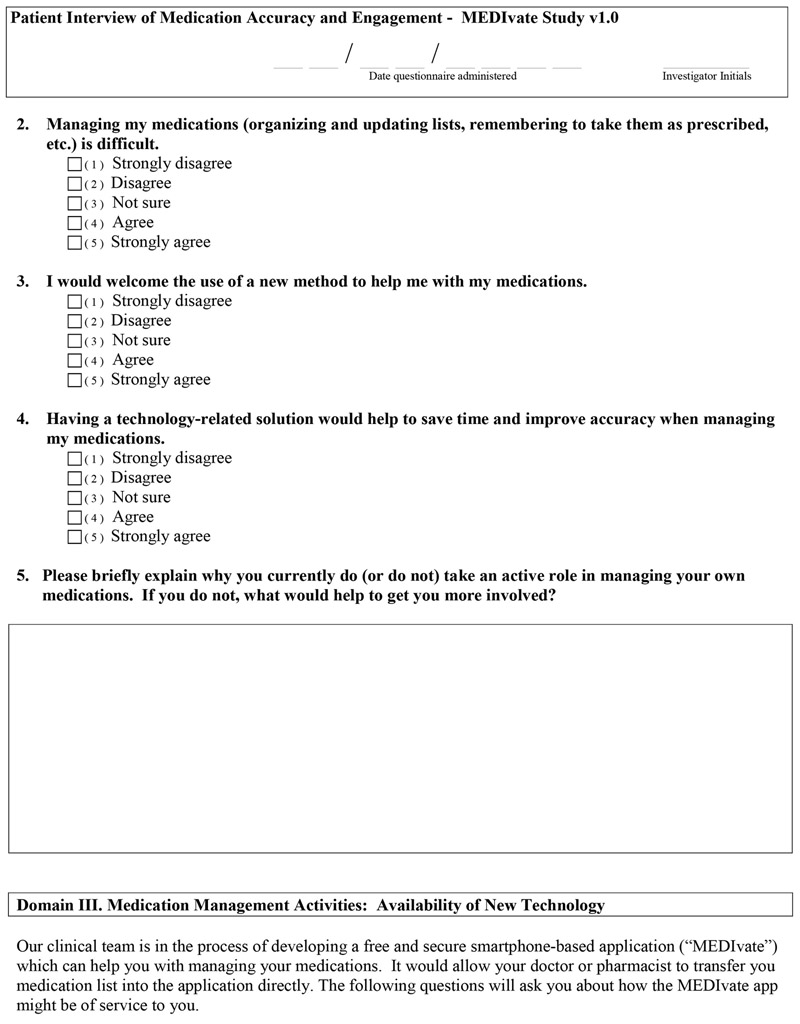
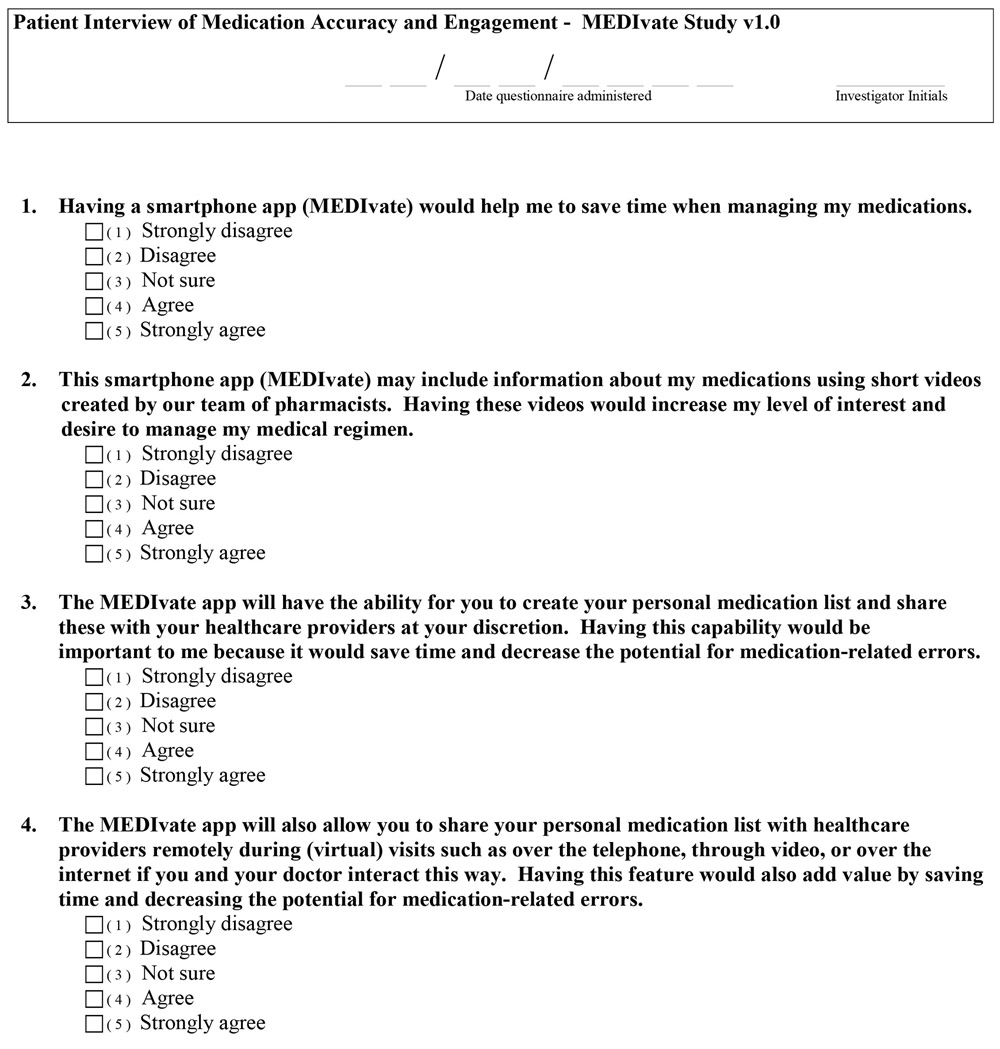
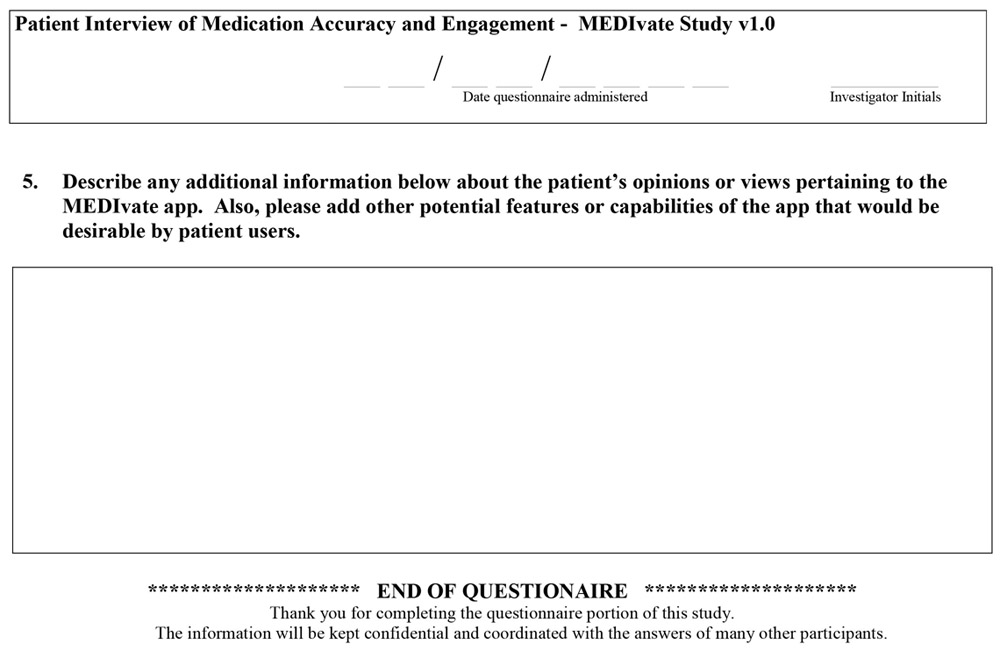
Research in the hospital setting was conducted in two phases. We conducted a survey of patient interests in phase one and a study of the feasibility of transferring entire medication lists into the MEDIvate® app at the time of inpatient hospital discharge in phase two.
In phase one, all adult outpatients seen in the University of Pittsburgh Medical Center (UPMC) Advanced Heart Failure (HF) Discharge Clinic at UPMC Presbyterian Hospital were eligible to participate in a survey of patient perceptions. Patients that are discharged from the inpatient service are eligible for follow-up in the HF Discharge Clinic. The goals of the clinic are to improve transitions of care, prevent medication-related problems, and lower the risk of readmission to the hospital.
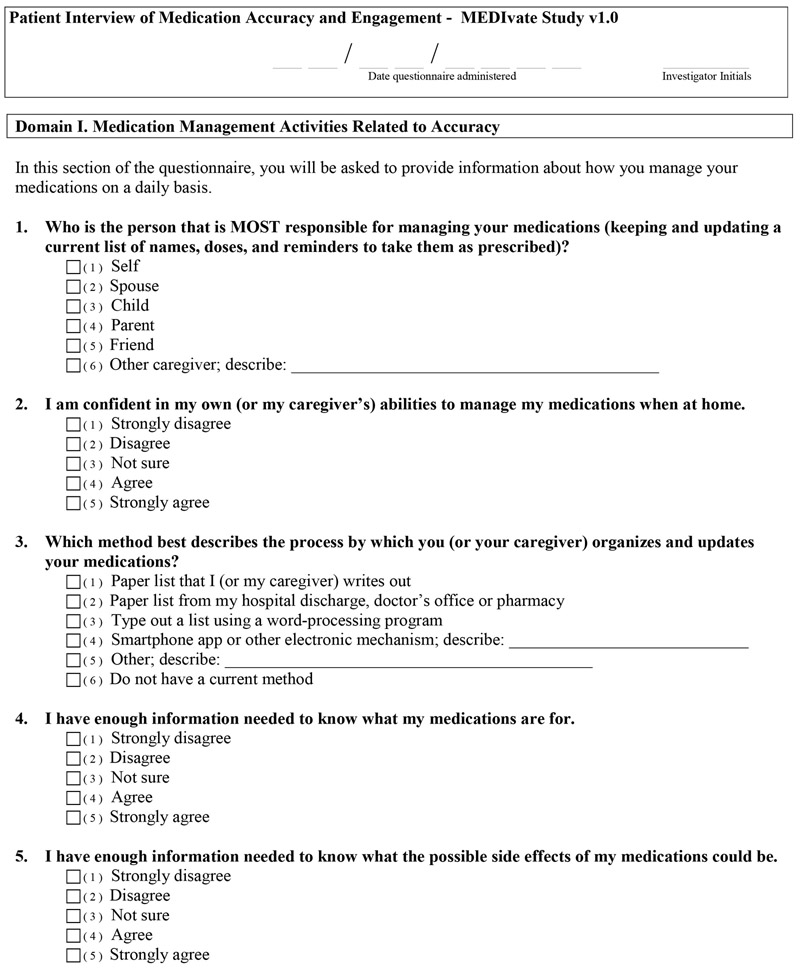
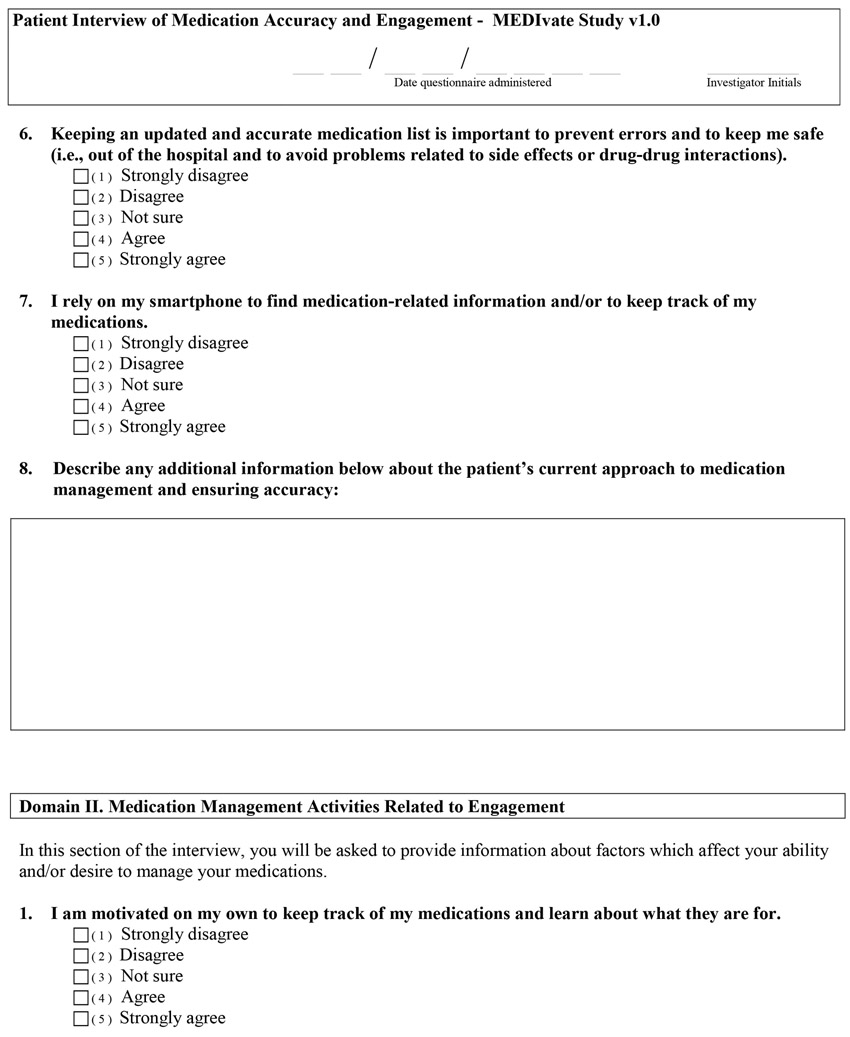
A clinical pharmacist introduced the study using a standardized script and informed consent was obtained by the principal investigator (PI). The goal of the survey was to identify the scope of medication-related problems (medication-taking behaviors, adherence, and education) and the potential utility for the MEDIvate® app as a solution. The survey (Appendix) evaluated the following domains: medication management related to accuracy, engagement, and perceptions about the utility of new technology to help with medication management activities. We were interested in learning more about what methods patients use to help ensure the accuracy of their medications and what factors are important to them for helping to remember to take their medications long-term. The survey information sought to validate the app concept, inform its design and iteration, and provide insight into eventual patient care integration. We targeted a convenience sample of 20 patients for participation.
Phase two of the study provided a mechanism by which the discharge medication list could be transferred on-demand from the inpatient EHR (Cerner, North Kansas City, MO) to the patient's mobile phone (e.g., iPhone®) using MEDIvate®. The initial goal was to evaluate the feasibility and accuracy of the medication list as compared to EHR data at the time of app deployment. This phase of the research occurred at or near the time of discharge medication reconciliation and targeted adult inpatients under the care of the advanced HF service as described above, as well as those patients with other cardiovascular conditions managed by other inpatient services. Patients scheduled for discharge from two of the inpatient cardiovascular wards at UPMC Presbyterian Hospital were first identified by a clinical pharmacist (PI) or a coinvestigator (co-I) through chart review and via daily meetings with care managers and advanced practice providers. These patients were then screened for possible participation during a brief encounter with the PI or co-I. Patients that had an iPhone® were eligible to participate. The PI then approached these patients for possible study participation and informed consent.
Data transfer between the MEDIvate® cloud-based HIPAA-compliant server and the EHR (Cerner Powerchart) (Figure 1) was achieved using the HL7 FHIR specification and was triggered by a secure query using the medical record number.13 The study participant’s discharge medication list was then transferred from the EHR to the MEDIvate® server using the FHIR-based query. The discharge medication list was then reviewed on a MEDIvate® website and adjudicated (if necessary) by the clinical pharmacist on the study team. Efficient creation of a patient account and data transfer to the patient’s iPhone via the MEDIvate® app (termed “onboarding”) was facilitated using the QR code that was printed locally on a patient-specific leaflet similar to the community deployment. Overall, hospital workflow integration requirements involved identification of patient to be discharged, whether they had an iOS device, and confirming the transferred list was accurate. Study participants received a follow-up telephone call at approximately 30 days after study enrollment at discharge for completion of a survey. The purpose of the survey was to conduct medication reconciliation (compare accuracy between self-report and medications stored on the app itself) and to collect feedback on the education experience with the app (improved understanding of purpose of new medications prescribed in the hospital and possible side effects).
Phase two outcomes presented herein focus on app deployment feasibility. Specifically, metrics of study participation (patient interest), experience with app deployment, and accuracy of the medication list transferred into the app at the time of study enrollment are reported.
Results
Community Phase
Five pharmacists participated in semi-structured interviews that focused on the workflow impact of the MEDIvate® app during employee influenza vaccination clinics. Analysis of data revealed four themes: (1) pharmacists believed the app is useful to help patients keep track of their vaccination history; (2) introducing the app and encouraging patients to download it at the beginning of the vaccine clinic workflow is ideal; (3) pharmacists believed patient-level barriers to technology exist that can limit widespread use by community-dwelling patients; and (4) that pharmacists believed that hands-on training of pharmacy staff with the app is the most effective way to facilitate its use. Supporting quotes are provided in Table 1. The initial deployment in pharmacy employer vaccination clinics produced 104 unique users downloading the app. Twenty-six (25%) of these patient users also showed an additional interest in electronic medication education by accessing the VIS through the MEDIvate® app.
Table 1.
Qualitative Feedback: MEDIvate® Integration into Employee Vaccination Clinic Workflow
| Themes | Supporting Quotes from Community Pharmacists |
|---|---|
| The app is useful to help patients keep track of their vaccination history |
|
| Introducing the app and encouraging patients to download it at the beginning of the vaccine clinic workflow is ideal |
|
| Patient-level barriers to technology exist that can limit widespread use by community-dwelling patients |
|
| Hands-on training of pharmacy staff with the app is the most effective way to facilitate its use. |
|
Hospital Phase
Twenty patients completed a survey of medication accuracy and engagement. Participants described their current practices for managing their medications, including updating and maintaining an accurate list. Table 2 summarizes the major themes from phase one of the hospital study. Approximately 79% of participants currently rely on a paper-based list or paper discharge summary to keep track of their medications. About 10% have no current method and another 10% use an electronic means of organizing and updating their medication list.
Table 2.
Survey of Patients with Heart Failure
| Strongly Agree |
Agree | Not Sure | Disagree | Strongly Disagree |
|
|---|---|---|---|---|---|
| Updated/accurate medication list is important to prevent errors and to keep patients safe | 74% | 26% | 0% | 0% | 0% |
| Self-motivated to keep track of medications and learn about them | 47% | 32 % | 5% | 5% | 11% |
| Would welcome the use of a new method to help with managing medications | 25% | 35% | 15% | 15% | 10% |
| MEDIvate® would save time and decrease potential for medication-related errors | 40% | 35% | 10% | 10% | 5% |
| MEDIvate® would add value to virtual visits with my healthcare provider | 50% | 30% | 5% | 10% | 5% |
Phase two of the study tested real-world data flows, onboarding, patient use, and patient/provider feedback. A total of 107 patients were screened for participation, of which 13 were consented and provided with the app prior to discharge. Reasons for study ineligibility included: no smartphone (26%), Android user (17%), iPhone but no app use (15%), not interested (17%), and caregiver use of iPhone to manage patient’s medications (12%). Patient ages ranged from 31 to 77 years and approximately70% were female.. Participants were under the care of a variety of cardiovascular services, which included the subspecialties of electrophysiology, interventional, and HF. The average number of medications prescribed at discharge was 11 (6 to 20 medications). Onboarding took approximately ten minutes per encounter.
EHR integration was 100% successful to the correct patient and accurate list of medications. In each case, the medication list was successfully pulled and accurate from Cerner® (North Kansas City, MO) to the MEDIvate® app via the FHIR look-up. However, some manual curation by the pharmacist investigator was required to delete medication duplications (current inpatient and discharge medication). There were also a few occasions when further clarification of the directions for use was needed. For example, converting inpatient dispensing formats to the outpatient prescription forms (e.g. take two 5 mg tablets to take one 10 mg tablet). None of these were discrepancies or errors, but were efforts undertaken to simplify the list for patients when feasible. Overall, these steps required approximately five to 10 minutes per patient enrollment. Onboarding required approximately five minutes per patient and included the following steps: text message, app download, account creation, and initial use.
Use of the app resulted in 40% of patients having made a change in their medication list between discharge and the follow-up survey at 30 days. Half of the patients added a new medication and 75% had an accurate medication list in the app as compared to what the patient reported they were taking. Engagement with the app was seen through 20 medication list shares, 104 instances of education being accessed, and 15 average launches by user. Patient feedback from the survey found strong agreement with use of the app to learn more about the purpose (100%) and possible side effects of medications prescribed (100%).
Discussion
We described the design, iteration, and clinical experience with a novel smartphone app used to facilitate the transfer of an accurate and portable medication and vaccine list. The patient's list was updated and shared using QR code technology or manually as needed. The architecture of the app itself represents a technologic advancement that facilitates simple interoperability between an EHR and a consumer targeted app. Interviews of pharmacists and surveys of patients show that medication and vaccine list management is important and that a solution is needed. The results of our pilot study demonstrated feasibility of successfully integrating the app into these complex clinical workflows.
Technological Challenges and Interoperability
The MEDIvate® app was designed to receive data from EHRs whether in the community or hospital settings. A strength of the architecture is that it achieves interoperability using leading technology standards (FHIR) while maintaining security and incorporating simple approaches to triggering the exchange of data (QR codes) that are familiar to users. Importantly, data transfer model using a patient app and cloud-based architecture further gives users the capability of updating and sharing their medication lists independent of original data owners.
Implications on Clinical Workflows and Medication-Related Endpoints
Our research in the community setting showed patients can download and use an app within a clinical environment, but identified important considerations for integration into these unique workflows. Pharmacists believed there is a need for such a solution and identified important practical considerations. Notably, that training and communication with the pharmacy staff was deemed critical to success.
The hospital setting of our study focused on transitions of care since this represents a particularly vulnerable time for medication errors. In fact, 60% of hospitalized patients have one or more discrepancies in their admission medication list.22,23 Nearly 40% of these discrepancies have the potential for patient harm.24 Further compounding the problem is that 20% of patients are estimated to experience an adverse effect.23,25 The importance of updating and maintaining an accurate medication list was apparent to patients in our study. Further, while most relied on a paper-based solution, the majority indicated that they would welcome a new technology-related solution to help manage their medications and that this method would be expected to save time and improve accuracy. Additionally, patients reported that having updated and portable medication information could help to prevent errors and to keep them safer by avoiding drug interactions and adverse effects. The patient experience with MEDIvate® demonstrated successful data integration, efficient onboarding, and active use of the app which resulted in medication changes and additions. Enthusiasm for the app was reflected by user engagement (medication list shares, education access, and user launches) as well as survey feedback.
Making an impact on medication-related errors through an improved reconciliation process during transitions of care is a significant challenge. The process of gathering, verifying, and updating medication information is a time and resource-intensive process for both patients and providers. The MEDIvate® app offers potential benefit to patients by facilitating an electronic exchange and by enhancing patient’s ability to self-manage their medications. Current EHRs, pharmacy systems, and insurance claims databases each store medication information, but generally in isolation. Interoperability progress continues to be made to exchange data between these disparate information sources, but is slow. A notable exception is the increased availability of pharmacy dispensing databases through Surescripts.26 However, these databases have their own limitations, can be costly, and do not include over-the-counter medicines or prescriptions products that are not processed through insurance. Therefore, a mobile medication app such as MEDIvate® could benefit patients by making the reconciliation process more patient-centered and clinically relevant.27 The mobile medication app concept also aligns with the recommendation to develop a personal health record that is integrated and easily transferable between sites of care.27 This could also offer advantages to healthcare professionals by streamlining the time and effort needed for the medication reconciliation process when patients are admitted to the hospital or are seen in different healthcare settings. The importance and complexity of medication reconciliation is further underscored by The Joint Commission designating it as a National Patient Safety Goal.28 Nonetheless, numerous stakeholders remain in the quest to solve medication reconciliation problems and improve patient safety. Interventions to resolve medication discrepancies have been shown to reduce hospital readmission rates by 30%.29
Landscape Analysis and Future Directions
There are a number of mobile-health apps currently available, however, those that provide medication management features largely focus on reminders to improve adherence. A recent report identified nearly 6,000 medication adherence apps from the Apple App Store and the Google Play Store.30 The MEDIvate® app was not designed specifically for adherence, but could improve this metric because it provides structured medication monographs which can improve patient education and communication about changes in treatment. It also links VIS for vaccines which could serve a similar purpose. We believe these patient education materials will increase engagement and perceived value of the app.
Despite the variety of medication apps which focus on adherence, investigators have reported a concerning lack of healthcare professional involvement in app development and a limited evidence base of effectiveness.30 Other medication-focused apps offer different functionality, such as prescription filling and cost comparisons.31 The design of a medication reconciliation application prototype to incorporate multiple data sources has also been described, but usability testing has not yet been evaluated.32 The design phase of the MEDIvate® app was conducted with a team that included the active involvement of pharmacists. We view involvement of domain experts as being essential to achieving objectives and successful integration into workflows. Workflow and feasibility testing was further driven by practicing pharmacists in both the community and hospital setting.
Study Limitations
We conducted a feasibility study of the MEDIvate® app, wherein we described the architecture, iterative design, and early clinical experience. Critically, we also successfully connected the app into our inpatient EHR to increase the efficiency of transferring entire medication lists from an EHR to MEDIvate®. However, we have not yet integrated into our outpatient EHR, nor have we demonstrated interoperability from MEDIvate® back into an EHR. These remain a goal of a future iteration of the app, so that we can assess the downstream impact on patients seen in our outpatient clinics. Nonetheless, the app functions effectively and independently from the EHRs, and can provide an unmet need for patients that seek an accurate and portable solution for medication management. Finally, our current version of the app is only iOS capable and our evaluations to-date only involved users of these devices. Future development will include an Android-capable platform and study of these users as well.
Conclusion
A mobile medication app (MEDIvate®) to achieve medication and vaccine list portability was successfully designed. The app was effectively integrated with an inpatient EHR and demonstrated feasibility through testing in both the inpatient and community settings. Ongoing clinical study will ascertain the full impact on medication accuracy, adverse outcomes, and user engagement.
Key Points.
Background
Medication use problems are especially prevalent during transitions of care.
Although many medication apps exist, few have reported successful integration into clinical workflow and demonstrated electronic health record interoperability.
Findings
A mobile app for medication management which uses QR code technology for data portability was successfully developed.
This is the first study, to our knowledge, of the feasibility of implementing a medication app for this purpose in both the inpatient and outpatient clinical setting.
Acknowledgments:
We acknowledge the following contributions: programming (InfoShape software) – Keith Overstreet; strategy – Max Dizard and Madeline Chavara, PharmD; application design (Pharmacy Innovations Lab): Eric LeCato, Marijanel Alilio, PharmD, Miranda Steinkopf; and concepts - Kyle McCormick, PharmD, Kelsey Moss, PharmD, and Christina Xia, PharmD; community semi-structured interviews – Joanna DeAngelis, PharmD Candidate, Emily Mattys, Brittany Steiner, PharmD Candidate
Funding: This work was supported by grants from the National Institutes of Health (UL1-TR000005), the National Association of Chain Drug Stores, Pittsburgh Innovations Challenge, and Pittsburgh Data Alliance Center for Commercial Applications.
Appendix
Footnotes
Conflicts of interest: None of the authors have any conflicts to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author roles: Coons (conceptualization, investigation, writing – original draft, writing – review & editing), Patel (software, investigation, project administration, writing – review & editing), Coley (data curation, investigation, methodology, project administration, writing – review & editing), Empey (conceptualization, data curation, investigation, methodology, project administration, software, supervision, writing – original draft, writing – review & editing)
Contributor Information
James C. Coons, Department of Pharmacy and Therapeutics, University of Pittsburgh School of Pharmacy and Clinical Pharmacist, Cardiology at UPMC Presbyterian Hospital, Pittsburgh, PA.
Ravi Patel, Department of Pharmacy and Therapeutics, University of Pittsburgh School of Pharmacy, Pittsburgh, PA..
Kim C. Coley, Department of Pharmacy and Therapeutics, University of Pittsburgh School of Pharmacy, Pittsburgh, PA.
Philip E. Empey, Department of Pharmacy and Therapeutics, Center for Clinical Pharmaceutics Sciences, University of Pittsburgh School of Pharmacy, Pittsburgh, PA.
References:
- 1.Kohn L To err is human: an interview with the Institute of Medicine's Linda Kohn. Jt Comm J Qual Improv 2000;4:227–34. [PubMed] [Google Scholar]
- 2.Benjamin RM. Medication adherence: helping patients take their medicines as directed. Public Health Rep 2012;127:2–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LaPointe NM, Jollis JG. Medication errors in hospitalized cardiovascular patients. Arch Intern Med 2003;12:1461–6. [DOI] [PubMed] [Google Scholar]
- 4.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;5:487–97. [DOI] [PubMed] [Google Scholar]
- 5.McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 2002;9:1331–6. [DOI] [PubMed] [Google Scholar]
- 6.Barnsteiner JH. Medication reconciliation: transfer of medication information across settings-keeping it free from error. J Infus Nurs 2005;2 Suppl:31–6. [DOI] [PubMed] [Google Scholar]
- 7.Lien CT, Gillespie ND, Struthers AD, McMurdo ME. Heart failure in frail elderly patients: diagnostic difficulties, co-morbidities, polypharmacy and treatment dilemmas. Eur J Heart Fail 2002;1:91–8. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 2016. IISAR data participation rates. https://www.cdc.gov/vaccines/programs/iis/annual-report-iisar/2016-data.html. Accessed June 15, 2018.
- 9.Workman B The explosion in health apps, and how they're disrupting the gigantic, lethargic health care industry. Business Insider, 2013. http://www.businessinsider.com/mobile-will-disrupt-health-care-2013-9. Accessed June 15, 2018. [Google Scholar]
- 10.Merrill M Report touts 'med-op' technology for older adults. Healtcare IT News, 2009. http://www.healthcareitnews.com/news/report-touts-med-op-technology-older-adults. Accessed June 15, 2018. [Google Scholar]
- 11.Davis J 21st century cures act brings provisions for EHRs, interoperability, precision medicine and more. Healtcare IT News, 2016. http://www.healthcareitnews.com/news/21st-century-cures-act-passes-provisions-ehrs-interoperability-precision-medicine-and-more. Accessed June 15, 2018. [Google Scholar]
- 12.Mandel JC, Kreda DA, Mandl KD, Kohane IS, Ramoni RB. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J Am Med Inform Assoc 2016;5:899–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.FHIR Overview. HL7.org. 2017. https://www.hl7.org/fhir/overview.html#2.11. Accessed June 15, 2018.
- 14.North F, Chaudhry R. Apple healthKit and health app: patient uptake and barriers in primary care. Telemed J E Health 2016;7:608–13. [DOI] [PubMed] [Google Scholar]
- 15.Marcum ZA, Sevick MA, Handler SM. Medication nonadherence: a diagnosable and treatable medical condition. JAMA 2013;20:2105–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med 2007;6:540–50. [DOI] [PubMed] [Google Scholar]
- 17.Bartlett YK, Webb TL, Hawley MS. Using persuasive technology to increase physical activity in people with chronic obstructive pulmonary disease by encouraging regular walking: a mixed-methods study exploring opinions and preferences. J Med Internet Res 2017;4:e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chatterjee S, Price A. Healthy living with persuasive technologies: framework, issues, and challenges. J Am Med Inform Assoc 2009;2:171–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eckman M, Gorski I, Mehta K. Leveraging design thinking to build sustainable mobile health systems. J Med Eng Technol. 2016;40:422–430. [DOI] [PubMed] [Google Scholar]
- 20.Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006;i50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. [DOI] [PubMed] [Google Scholar]
- 22.Lau HS, Florax C, Porsius AJ, De Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol 2000;6:597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beers MH, Munekata M, Storrie M. The accuracy of medication histories in the hospital medical records of elderly persons. J Am Geriatr Soc 1990;11:1183–7. [DOI] [PubMed] [Google Scholar]
- 24.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med 2005;4:424–9. [DOI] [PubMed] [Google Scholar]
- 25.Reeder TA, Mutnick A. Pharmacist- versus physician-obtained medication histories. Am J Health-Syst Pharm 2008;9:857–60. [DOI] [PubMed] [Google Scholar]
- 26.SureScripts.com. http://www.surescripts.com. Accessed June 15, 2018. [Google Scholar]
- 27.Greenwald JL, Halasyamani LK, Greene J, et al. Making inpatient medication reconciliation patient centered, clinically relevant, and implementable: a consensus statement on key principles and necessary first steps. Jt Comm J Qual Patient Saf 2010;11:504–13. [DOI] [PubMed] [Google Scholar]
- 28.American Pharmacists Association and American Society of Health-System Pharmacists. Improving care transitions: optimizing medication reconciliation. J Am Pharm Assoc 2012;4:e43–52. [DOI] [PubMed] [Google Scholar]
- 29.Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med 2011;14:1232–7. [DOI] [PubMed] [Google Scholar]
- 30.Ahmed I, Ahmad NS, Ali S, et al. Medication adherence apps: review and content analysis. JMIR Mhealth Uhealth 2018;3:e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silva BM, Rodrigues JJ, de la Torre Diez I, Lopez-Coronado M, Saleem K. Mobile-health: a review of current state in 2015. J Biomed Inform 2015;265–72. [DOI] [PubMed] [Google Scholar]
- 32.Cadwallader J, Spry K, Morea J, Russ AL, Duke J, Weiner M. Design of a medication reconciliation application: facilitating clinician-focused decision making with data from multiple sources. Appl Clin Inform 2013;1:110–25. [DOI] [PMC free article] [PubMed] [Google Scholar]