Abstract
Background
The assessment of acute heart failure (AHF) in patients with acute coronary syndrome (ACS) is challenging. This study tested whether measuring plasma adrenomedullin in patients admitted for ACS provides valuable information regarding the presence of AHF at admission or its occurrence during hospitalization.
Methods and results
The study population consisted of 927 prospectively enrolled patients with ACS. Blood samples for the measurement of plasma bio-adrenomedullin (bio-ADM) were collected at admission. Patients with alveolar pulmonary edema and interstitial pulmonary edema on chest radiography at admission had stepwise higher plasma concentrations of bio-ADM compared to patients with no or mild pulmonary congestion: 54.3 ± 10.6 vs. 27.6 ± 2.1 vs. 22.5 ± 0.7 ng/L, overall P < 0.001. Patients with ACS complicated by AHF during the index hospitalization displayed higher plasma bio-ADM concentrations at admission compared to patients without AHF (33.8 ± 2.7 vs. 21.8 ± 0.7, P < 0.001): the higher the severity of AHF, the higher plasma bio-ADM concentrations at admission. Patients with cardiogenic shock displayed the highest values. Accordingly, bio-ADM concentrations at admission were associated with a higher risk of occurrence of AHF during index hospitalization (odds ratio 1.018, 95% confidence interval 1.011–1.026, P < 0.001).
Conclusions
Plasma adrenomedullin is a marker associated with AHF severity in patients with ACS.
Keywords: Bio-adrenomedullin, Acute coronary syndrome, Acute heart failure, Pulmonary edema
1. Introduction
Acute coronary syndrome (ACS) and acute heart failure (AHF) often coexist and have reciprocal detrimental effects on prognosis [[1], [2], [3]]. The assessment of AHF in patients with ACS remains challenging because imaging techniques might be time-consuming and cause unacceptable delays in coronary revascularization, and the performance of natriuretic peptides in this context is modest [4]. Adrenomedullin is a vasoactive hormone reflecting excessive volume overload and plays an essential role in the development of acute circulatory failure. The aim of this study was to test whether the measurement of circulating adrenomedullin in patients admitted for ACS might provide valuable information regarding the presence of AHF at admission or its occurrence during hospitalization.
2. Materials and methods
Consecutive patients with acute coronary syndrome (ACS) admitted to University Hospital of Brno, (Czech Republic), from 2009 to 2012 were enrolled [5]. The diagnosis of ACS was based on the criteria of the European Society of Cardiology and the Third universal definition of myocardial infarction [6,7]. Exclusion criteria were age > 85 years, known malignancy or inflammatory disease, and absence of culprit lesion on coronary angiography. Venous EDTA-blood samples were immediately drawn upon admission, refrigerated, centrifuged within 10 min, and plasma was stored at −80 °C. Measurement of biologically active adrenomedullin (bio-ADM) in the plasma samples was performed, blinded to clinical data, by Sphingotec GmbH (Hennigsdorf, Germany) using a chemiluminescence immunoassay (sphingotest® bio-ADM®). As previously reported, the bio-ADM analytical assay sensitivity is 2 pg/mL, the median concentration in healthy adults equals 21 pg/mL [8]. Pulmonary congestion at admission was graded by certified radiologists blinded to laboratory values in 3 categories using conventional chest radiographs taken upon cardiac care unit admission: no or mild pulmonary congestion, interstitial pulmonary edema, alveolar pulmonary edema. The severity of acute heart failure (AHF) at admission and/or during the index hospitalization was graded according to the Killip classification [9]: cardiogenic shock (Killip IV), pulmonary edema (Killip III), mild heart failure (Killip II), no clinical signs of congestion (Killip I). The study was performed in accordance with the ethical standards of the Declaration of Helsinki and was approved by the local Ethics Committee. Written informed consent was obtained from all subjects before inclusion in the study. Values are expressed as mean (±standard error) or as number (percentage), as appropriate. Groups were compared with the Kruskal-Wallis H-test with pairwise comparisons and correction of the p-value for multiple comparisons. The association between biomarker concentration and outcome was assessed by logistic regression and is expressed as odds ratio with 95% confidence interval. The null hypothesis was rejected with an adjusted two-sided P < 0.05. All analyses were performed with the use of IBM SPSS Statistics, Version 25 (IBM Corp, Armonk NY, USA).
3. Results
From a total of 1021 prospectively enrolled ACS patients, 94 (9%) were excluded because of lack of chest radiography at admission. The study population (n = 927) consisted prevalently of middle-aged men (median age 61 years), with a high burden of cardiovascular risk factors. Two-thirds of patients presented with ST-elevation myocardial infarction. The baseline characteristics of the study population have been published previously [5].
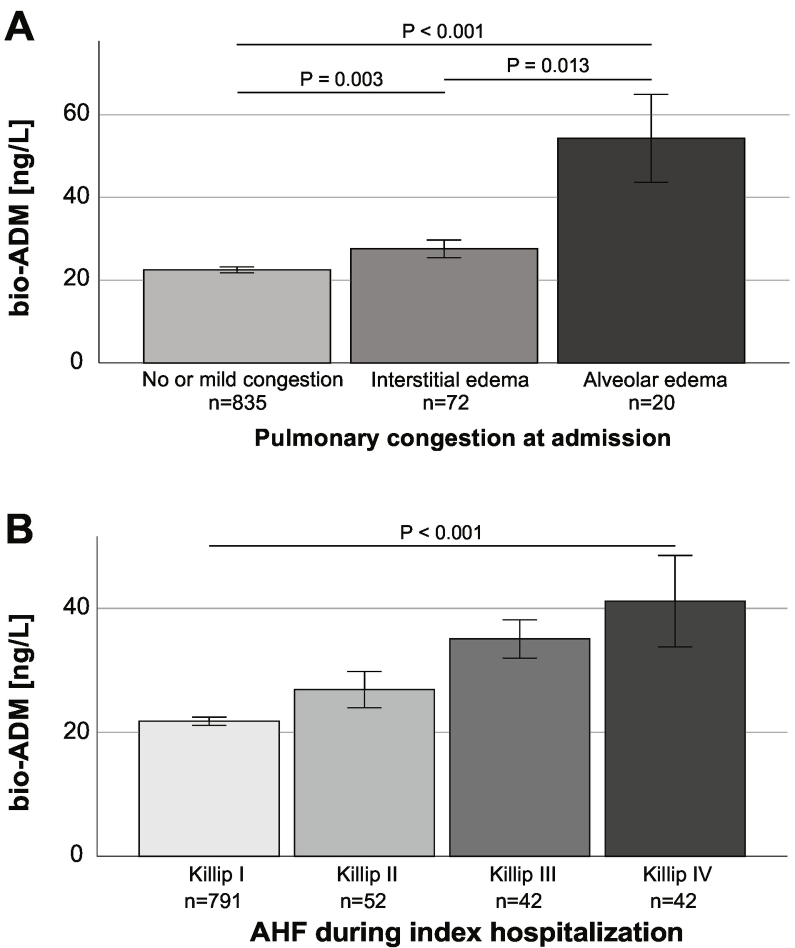
For the overall population, plasma concentration of bio-ADM was 23.5 ± 0.71 ng/L. Patients with alveolar pulmonary edema (n = 20) and interstitial pulmonary edema (n = 72) on chest radiography at admission had stepwise higher plasma concentrations of bio-ADM compared to patients with no or mild pulmonary congestion (n = 835): 54.3 ± 10.6 vs. 27.6 ± 2.1 vs. 22.5 ± 0.7 ng/L, overall P < 0.001 (Fig. 1A).
Fig. 1.
Circulating adrenomedullin (bio-ADM) baseline concentrations according to the presence of pulmonary congestion at admission (Panel A) and acute heart failure (AHF) during hospitalization (Panel B). Data are shown as mean ± SEM.
Patients with ACS complicated by AHF during the index hospitalization (n = 136, 17%) displayed higher plasma bio-ADM concentrations at admission compared to patients without AHF (21.8 ± 0.7 vs. 33.8 ± 2.7, P < 0.001).
As shown in Fig. 1B, the higher the severity of AHF during the index hospitalization, the higher plasma bio-ADM concentrations at admission (P < 0.001). The highest values were displayed by patients with cardiogenic shock (41.1 ± 7.4 ng/L), followed by patients with pulmonary edema (35.1 ± 3.1 ng/L), and those with mild congestion (26.9 ± 2.9 ng/L). Patients with no evidence of AHF displayed the lowest bio-ADM concentrations at admission (21.8 ± 0.7 ng/L). Consistent results were found after removal of patients with evidence of insufficient revascularization (post-procedural TIMI flow 0–1, n = 16). Accordingly, bio-ADM concentrations at admission were associated with a higher risk of occurrence of AHF during index hospitalization (odds ratio 1.018, 95% confidence interval 1.011–1.026, P < 0.001).
4. Discussion
This study firstly describes adrenomedullin, a vasoactive peptide hormone reflecting excessive volume overload, as a marker associated with pulmonary congestion and the risk of occurrence of AHF during hospitalization in patients admitted for ACS. Very recent data described bio-ADM as potential marker of AHF with greater discriminatory value for congestion compared to natriuretic peptides [10]. Bio-ADM showed consistently strong diagnostic properties for AHF both at admission and during hospitalization. Our analysis confirms the strength of bio-ADM for diagnosing pulmonary congestion at admission and AHF during the index hospitalization in patients admitted with ACS.
5. Limitations
Our study has some limitations. First, the results of this single-center prospective cohort study should be confirmed in multi-centric cohorts. Moreover, despite a considerable number of included patients, the proportion of patients with radiological evidence of pulmonary congestion was relatively small. Second, pulmonary congestion was assessed by conventional chest radiography at admission by one experienced, certified radiologist. Although this method reflects clinical practice, this might not always be reproducible. Third, the group of patients with alveolar edema displayed some relevant differences in baseline characteristics, which may have contributed to the observed differences in bio-ADM concentrations. Forth, no data about pre-existing chronic heart failure was recorded.
6. Conclusions
Plasma adrenomedullin is a marker associated with acute heart failure severity and congestion in patients with acute coronary syndrome.
Disclosures
No conflict of interest. This work was partly supported by the Ministry of Health of the Czech Republic – conceptual development of research organization (FNBr, 65269705; funding was given to University Hospital Brno) and project MUNI/A/1250/2017.
Contributor Information
Mattia Arrigo, Email: mattia.arrigo@usz.ch.
Alexandre Mebazaa, Email: alexandre.mebazaa@aphp.fr.
References
- 1.Arrigo M., Gayat E., Parenica J., Ishihara S., Zhang J., Choi D.-J., Park J.J., AlHabib K.F., Sato N., Miró Ò., Maggioni A.P., Zhang Y., Spinar J., Cohen-Solal A., Iwashyna T.J., Mebazaa A. Precipitating factors and 90-day outcome of acute heart failure: a report from the intercontinental GREAT registry. Eur. J. Heart Fail. 2017;19:201–208. doi: 10.1002/ejhf.682. [DOI] [PubMed] [Google Scholar]
- 2.Fonarow G.C., Abraham W.T., Albert N.M., Stough W.G., Gheorghiade M., Greenberg B.H., O'Connor C.M., Pieper K., Sun J.L., Yancy C.W., Young J.B., OPTIMIZE-HF Investigators and Hospitals Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: findings from OPTIMIZE-HF. Arch. Intern. Med. 2008;168:847–854. doi: 10.1001/archinte.168.8.847. [DOI] [PubMed] [Google Scholar]
- 3.Bahit M.C., Lopes R.D., Clare R.M., Newby L.K., Pieper K.S., Van de Werf F., Armstrong P.W., Mahaffey K.W., Harrington R.A., Diaz R., Ohman E.M., White H.D., James S., Granger C.B. Heart failure complicating non-ST-segment elevation acute coronary syndrome: timing, predictors, and clinical outcomes. JACC Heart Fail. 2013;1:223–229. doi: 10.1016/j.jchf.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Sabatine M.S., Morrow D.A., de Lemos J.A., Omland T., Desai M.Y., Tanasijevic M., Hall C., McCabe C.H., Braunwald E. Acute changes in circulating natriuretic peptide levels in relation to myocardial ischemia. J. Am. Coll. Cardiol. 2004;44:1988–1995. doi: 10.1016/j.jacc.2004.07.057. [DOI] [PubMed] [Google Scholar]
- 5.Kubena P., Arrigo M., Parenica J., Gayat E., Sadoune M., Ganovska E., Pavlusova M., Littnerova S., Spinar J., Mebazaa A., GREAT Network Plasma levels of soluble CD146 reflect the severity of pulmonary congestion better than brain natriuretic peptide in acute coronary syndrome. Ann. Lab. Med. 2016;36:300–305. doi: 10.3343/alm.2016.36.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Authors/Task Force Members, Steg PG, James SK, Atar D, Badano LP, Lundqvist CB, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van't Hof A, Widimsky P, Zahger D, ESC Committee for Practice Guidelines (CPG), Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J 2012;33:2569–2619. [DOI] [PubMed]
- 7.Hamm CW, Bassand J-P, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, Ohman M, Petrie MC, Sonntag F, Uva MS, Storey RF, Wijns W, Zahger D, ESC Committee for Practice Guidelines. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999–3054. [DOI] [PubMed]
- 8.Marino R, Struck J, Maisel AS, Magrini L, Bergmann A, Di Somma S. Plasma adrenomedullin is associated with short-term mortality and vasopressor requirement in patients admitted with sepsis. Crit. Care; 2014;18:R34. [DOI] [PMC free article] [PubMed]
- 9.Killip T., Kimball J.T. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am. J. Cardiol. 1967;20:457–464. doi: 10.1016/0002-9149(67)90023-9. [DOI] [PubMed] [Google Scholar]
- 10.Kremer D., ter JM Maaten, Voors A.A. Bio-adrenomedullin as a potential quick, reliable, and objective marker of congestion in heart failure. Eur. J. Heart Fail. 2018;20:1363–1365. doi: 10.1002/ejhf.1245. [DOI] [PubMed] [Google Scholar]