Abstract
Introduction
While the exact mechanism of primary adhesive capsulitis is unknown, we know that it has strong associations with diabetes mellitus (DM). Although self-limiting, a significant percentage of patients still have persistent pain and stiffness beyond 3 years. Arthroscopic capsular release (ACR) has been described as a successful intervention for recalcitrant adhesive capsulitis that provides early and long-term recovery. The aim of this study is to investigate the relationship between DM and ACR.
Methods
We reviewed prospectively collected data of 56 consecutive patients with idiopathic frozen shoulder who underwent ACR (360° arthroscopic capsulotomy) under a single surgeon. Range of motion, pain score and shoulder function (Constant Shoulder Score, Oxford Shoulder Score, University of California Los Angeles Shoulder Score) were documented preoperatively and one year postoperatively. Patients were dichotomized into diabetic (n = 32) and non-diabetic patients (n = 24) and compared using a mixed ANOVA design to investigate for differences in outcomes.
Results
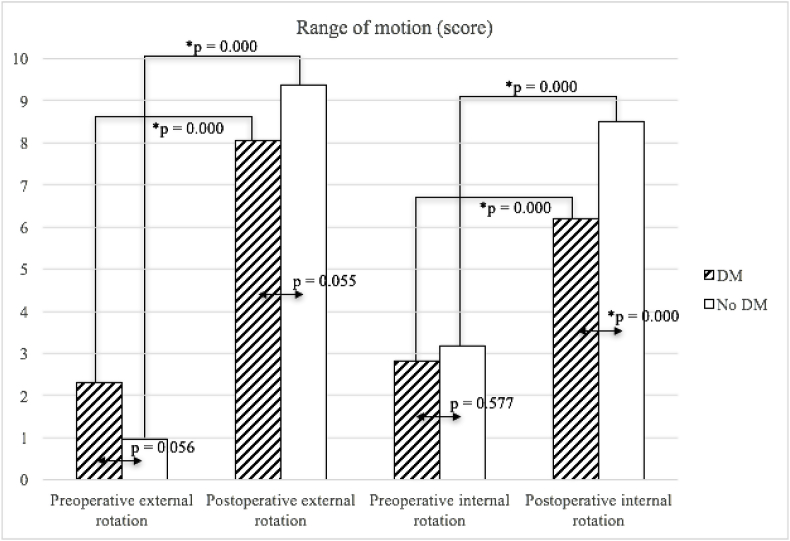
Both group of patients had significant improvement in range of motion, reduced pain scores and improved shoulder scores one year postoperatively (p = 0.000). Diabetic patients had poorer internal rotation (p = 0.000), forward flexion (p = 0.035) and poorer postoperative Constant Shoulder score (p < 0.05). Otherwise both groups improved equally in all other aspects.
Conclusion
ACR offered good outcomes in both diabetic and non-diabetic patients in terms of range of motion, pain relief and shoulder function. However diabetic patients had poorer improvement in internal rotation and forward flexion postoperatively. Preoperative counselling and postoperative rehabilitation can be better tailored to treat diabetic patients with idiopathic adhesive capsulitis.
Keywords: Frozen shoulder, Adhesive capsulitis, Diabetes mellitus, Arthroscopy, Arthroscopic capsular release
1. Introduction
Adhesive capsulitis of the shoulders is a common orthopaedic condition characterized by progressive pain and global restriction in movement at the glenohumeral joint as a result of synovial thickening of the capsule and global soft tissue contracture.1
Although adhesive capsulitis is generally self-limiting,2 studies have reported that up to 40% of patients experience persistent symptoms of pain and stiffness beyond 3 years and 7–15% have some degree of permanent functional loss.3,4 Arthroscopic capsular release (ACR), which involves the debridement of rotator interval between the supraspinatus and infraspinatus and the circumferential division of the shoulder capsule, is recognized as the definitive treatment for recalcitrant adhesive capsulitis and provides early and long-term recovery.5, 6, 7
While the exact mechanism is unknown in primary adhesive capsulitis,8 we know that risk factors include the female gender,9 diabetes mellitus (DM)10, 11, 12 and hyperthyroidism,13 among which DM demonstrated the strongest association with adhesive capsulitis, with an incidence of 28–40% in patients with adhesive capsulitis compared to 2–5% in the general population.14, 15, 16
The chronicity of DM and its complications make it a costly disease with large socioeconomic burden.17 The number of people affected by DM has increased from 108 million in 1980 to 422 million in 201418 and this rise is attributed to increasing trends of sedentary lifestyle, unhealthy diet and obesity.19 With rising incidence, we expect to see more patients with adhesive capsulitis having a background of DM.
Given the significant association between DM and adhesive capsulitis, we hypothesize that DM does affect outcomes of ACR for adhesive capsulitis.
2. Methods
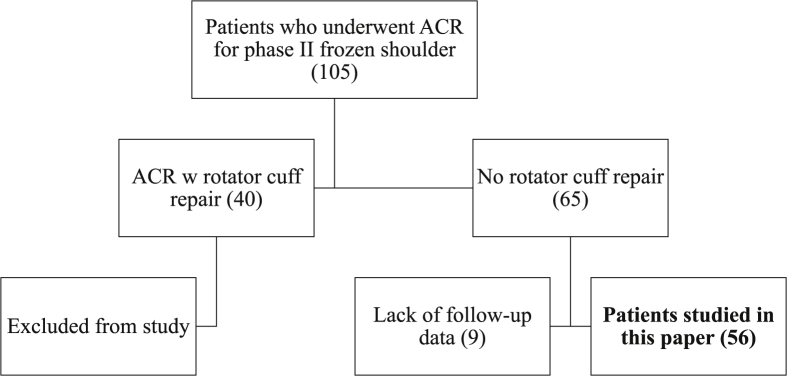
We retrospectively reviewed prospectively collected data of 105 consecutive patients with frozen shoulder who underwent ACR under a single fellowship trained shoulder surgeon (the senior author of this study) from 2010 to 2016. 40 patients had rotator cuff tears and were excluded from the study. 9 patients were subsequently excluded due to the lack of follow-up data. Fig. 1 illustrates the inclusion process of the studied subjects. The remaining 56 patients with the diagnosis of idiopathic frozen shoulder were dichotomized into diabetics and non-diabetics.
Fig. 1.
Subject selection.
Preoperatively, all patients had limitation in both active and passive ROM with no evidence of rotator cuff tear on imaging via ultrasound or magnetic resonance imaging. All subjects in this study were operated on in the frozen stage. They attempted physiotherapy for a minimum of 6 months with the use of oral anti-inflammatory and demonstrated poor clinical improvement with impairment of daily function.
ACR was performed under general anaesthesia in a beach chair position at 70° for all patients. This method is standardized and adopted for all patients undergoing arthroscopic capsular release in this institution and is a widely used approach.20,21 First, an inspection of the glenohumeral joint is done via the posterior viewing portal (Fig. 2A). The rotator interval is released using an electrocautery device (Fig. 2B) and the anterior capsule is divided down to the 6 o'clock position. The middle glenohumeral ligament (Fig. 2C) followed by the inferior capsule is then released (Fig. 2D). A gap is created between the anteroinferior capsule and head of the humerus to prevent recurrence (Fig. 2E). The articular surface of the subscapularis tendon is released but sparing the subscapularis muscle (Fig. 2F). Here, the integrity of the subscapularis and adequacy of release is tested by ranging and externally rotating the shoulder. Portals are then switched and posterior capsulotomy (Fig. 2G) and completion inferior capsulotomy (Fig. 2H) are performed via the anterior viewing portal, taking care not to damage the axillary nerve (Fig. 3). The joint is thoroughly irrigated before closure. All patients in this study had no rotator cuff pathology as confirmed both preoperatively with imaging and intraoperatively. None of the patients received intra-articular injections.
Fig. 2.
Technique of arthroscopic capsular release.
(A) Inspection. (B) Clearing the Rotator Interval. (C) Releasing the Anterior capsule. (D) Releasing the Middle glenohumeral ligament. (E) Releasing the Inferior capsule. (F) Creating a gap to prevent recurrence. (G) Releasing the Subscapularis. (H) Releasing the Posterior capsule. (I) Completing the release of the Inferior capsule.
Fig. 3.
Schematic representation of the right shoulder.
MGHL = Middle glenohumeral ligament.
Postoperatively, all patients were given appropriate analgesics and kept on arm sling up to one week for pain relief. All subjects were discharged on postoperative day one. Physiotherapy was initiated two weeks after surgery, starting with passive ROM exercises then progressing to active ROM exercises when pain was well controlled. The senior author of this study assessed the patients two weeks, one month, three months, six months and one year after surgery for clinical improvement and surgical complications.
Patient data was collected preoperatively, one month postoperatively, six months postoperatively and one year postoperatively by a group of experienced physiotherapists at a specialized data collection centre. ROM in forward flexion and abduction were measured using Dualer IQ Pro™ Digital Inclinometer and recorded in degrees. External rotation was recorded according to Active Function Composite External Rotation Constant score, where tasks involving shoulder and elbow movements are to be performed with the instruction of being ‘unassisted’ and ‘hands not touching the head’.22 Internal rotation was recorded according to the Active Functional Composite Internal Rotation Constant score, where tasks must be done ‘unassisted’, and the patient's thumb was used as a pointer for the ability of the hand to reach a certain level.22
Pain and functional status of the patients were evaluated using Visual analog scale (VAS), Constant-Murley Shoulder Score (CMSS),22 University of California at Los Angeles (UCLA) shoulder score23 and Oxford shoulder score (OSS),24 and data was collected using standardized survey forms. The VAS score measures solely patient reported pain. The CMSS evaluates the overall functionality of patients with shoulder disorders via the four parameters of pain, activities of daily living (ADLs), ROM (forward flexion, abduction, external and internal rotation) and strength. The UCLA Shoulder Score measures the level of disability using five parameters of pain, function, active forward elevation, strength of forward flexion and satisfaction, and the OSS measures the impact of shoulder conditions on patients' quality of life.
Patient demographics between the two groups were compared using Chi Square Test (categorical variables) and Student's T Test (continuous variables). Preoperative and one-year postoperative outcomes were compared between the two groups using a Mixed ANOVA design of repeated measures and Two-Way ANOVA. Repeated measures ANOVA testing for preoperative and postoperative difference. Two Way ANOVA was used to test for differences between diabetic and non-diabetic patients. Each paired variable was tested for separately. Post Hoc testing was carried out if main effects demonstrated significant interactions. All analyses were carried out using Statistical Package for the Social Sciences (SPSS) version 23.
3. Results
Table 1 demonstrates the baseline characteristics of both groups. There were no significant differences between diabetic and non-diabetic patients.
Table 1.
Patient demographics.
| Variables | Group distribution |
P | |
|---|---|---|---|
| Diabetic (32) | Non-Diabetic (24) | ||
| Gender (Female, percentage) | 44.4 | 41.4 | 1.00 |
| Gender (Male, percentage) | 55.6 | 58.6 | 1.00 |
| Age (years, range) | 56.9 | 53.6 | 0.14 |
| Mean duration of symptoms | 6 months–1 year | 6 months–1 year | 0.08 |
| Dominant shoulder affected | 17 | 15 | 0.546 |
All patients who underwent ACR demonstrated significant improvement (p < 0.05) in ROM, pain scores and shoulder scores. Diabetic patients had poorer improvement in internal rotation and forward flexion compared to non-diabetic patients. Diabetic patients also had poorer postoperative Constant Shoulder Scores. The findings are summarized in Fig. 4, Fig. 5 and Table 2.
Fig. 4.
Preoperative and postoperative forward flexion and abduction.
Fig. 5.
Preoperative and postoperative external and internal rotations.
Table 2.
Mixed ANOVA analysis.
| Preoperative |
Postoperative |
|||
|---|---|---|---|---|
| DM | No DM | DM | No DM | |
| Range of motion | ||||
| Forward Flexion (°) | 83.1 | 82.5 | 123.01 | 132.51 |
| Abduction (°) | 57.3 | 60.0 | 117.0 | 127.7 |
| External Rotation | 2.31 | 0.96 | 8.06 | 9.36 |
| Internal Rotation | 2.81 | 3.17 | 6.191 | 8.501 |
| Strength | ||||
| Isometric (lbs.) | 2.76 | 2.24 | 9.32 | 10.47 |
| Pain | ||||
| VAS | 6.47 | 6.96 | 2.09 | 1.20 |
| Constant Score (Pain) | 4.56 | 5.18 | 11.90 | 13.20 |
| Outcomes Scores | ||||
| Constant Shoulder Score | 29.2 | 24.4 | 64.31 | 74.21 |
| UCLA Score | 14.4 | 13.6 | 27.9 | 29.2 |
| Oxford Score | 35.3 | 38.5 | 14.4 | 17.7 |
1p-value (when comparing between DM and non-DM patients) is < 0.05.
4. Discussion
The relationship between musculoskeletal diseases, joint restriction and DM is well described.10,25 Of the multiple musculoskeletal diseases, frozen shoulder was the most common.10,26 Despite multiple reports of correlation between DM and reduced joint ROM, the pathophysiology remains unexplained,27 and there are very few studies describing the effects of DM on postoperative outcomes for adhesive capsulitis.
In our study with a sample size of 56 patients, all patients demonstrated significant improvement in ROM and outcome scores with decreased pain scores postoperatively. This is consistent with the established effectiveness of ACR.8,28,29 Various methods have been described for arthroscopic capsulotomy and some papers emphasize that anterior inferior capsulotomy alone was sufficient.10,30,31 In our study, 360° arthroscopic capsulotomy was performed for all patients.
Although there was improvement in all ROM, diabetic patients demonstrated poorer postoperative forward flexion and internal rotation. We believe that the thicker capsular contractures in diabetic patients, due to increased vascular endothelial growth factor expression, abnormal collagen cross-linking and fibrosis,32, 33, 34 had resulted in the inadequacy of the usual method of release. In particular, the use of a similar threshold of release for both diabetic and non-diabetic patients to avoid injury to the axillary nerve, which crosses the inferior border of the subscapularis just medial to the musculotendinous junction where it continues posteriorly along the inferior capsule (Fig. 3), possibly contributes to an insufficient extent of release of the inferior capsule for diabetic patients.35,36
All patients reported improvement in functional scores at one-year follow-up. Diabetic patients had less improvement of CMSS but no significant difference in OSS, UCLA shoulder score and VAS pain scores. This is likely due to the inclusion of ROM in all planes as part of the assessment in CMSS when compared to the other functional score. Although CMSS was reported to correlated with OSS,37 CMSS assesses ROM and strength on top of the subjective patient-reported measures (ADLs and pain)22 while OSS mainly reflects patient-reported outcomes.24 Similarly, when comparing CMSS to UCLA score, which integrates active ROM and strength of forward flexion with subjective patient-reported measures (pain, satisfaction and function),23 CMSS includes all four ROMs while UCLA score only reflects forward flexion in its objective measurement and does not reflect internal rotation. Patients in our study had significantly poorer internal rotation, which would have only been accounted for in CMSS. Overall, our results show that diabetic patients have similar improvement in function, pain and the other ROMs (abduction and external rotation) to non-diabetic patients. Our study points towards a poorer improvement in internal rotation as the main source of difference in CMSS between diabetic and non-diabetic patients.
The limitations of this study include the lack of data on diabetic control. Although previous study showed no definite association between glycosylated haemoglobin A1c and the severity of frozen shoulder,38 we believe that prolonged uncontrolled DM would inadvertently affect the degree of capsular fibrosis. This may be a worthwhile consideration for future studies. Other limitations include a small patient pool with the lack of blinding of assessors to the groups.
The strength of this paper includes the use of prospectively collected data by a dedicated data collection centre with standardized preoperative and postoperative management and rehabilitation. Recruiting patients under a single surgeon limits variability of the study, although we acknowledge that it brings about other biases.
5. Conclusion
We conclude that DM affects recovery in internal rotation and forward flexion post-ACR and that diabetic patients would benefit from better preoperative counselling and aggressive postoperative rehabilitation. ACR is still effective in improving ROM in the other planes, improving function and reducing pain despite the presence DM.
Contributor Information
Geraldine Lei Yanlei, Email: a0133295@u.nus.edu.
Mak Wai Keong, Email: waikeong.mak@mohh.com.sg.
Denny Lie Tijauw Tjoen, Email: denny.lie.t.t@singhealth.com.sg.
References
- 1.Zuckerman J.D., Rokito A. Frozen shoulder: a consensus definition. J Shoulder Elbow Surg. 2011;20:322–325. doi: 10.1016/j.jse.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Grey R.G. The natural history of "idiopathic" frozen shoulder. J Bone Joint Surg Am. 1978;60:564. [PubMed] [Google Scholar]
- 3.Robinson C.M., Seah K.T., Chee Y.H. Frozen shoulder. J Bone Joint Surg Br. 2012;94:1–9. doi: 10.1302/0301-620X.94B1.27093. [DOI] [PubMed] [Google Scholar]
- 4.Shaffer B., Tibone J.E., Kerlan R.K. Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am. 1992;74:738–746. [PubMed] [Google Scholar]
- 5.Segmuller H.E., Taylor D.E., Hogan C.S. Arthroscopic treatment of adhesive capsulitis. J Shoulder Elbow Surg. 1995;4:403–408. doi: 10.1016/s1058-2746(05)80030-8. [DOI] [PubMed] [Google Scholar]
- 6.Klinger H.M., Otte S., Baums M.H. Early arthroscopic release in refractory shoulder stiffness. Arch Orthop Trauma Surg. 2002;122:200–203. doi: 10.1007/s00402-001-0355-6. [DOI] [PubMed] [Google Scholar]
- 7.Smith C.D., Hamer P., Bunker T.D. Arthroscopic capsular release for idiopathic frozen shoulder with intra-articular injection and a controlled manipulation. Ann R Coll Surg Engl. 2014;96:55–60. doi: 10.1308/003588414X13824511650452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogilvie-Harris D.J., Myerthall S. The diabetic frozen shoulder: arthroscopic release. Arthroscopy. 1997;13:1–8. doi: 10.1016/s0749-8063(97)90203-6. [DOI] [PubMed] [Google Scholar]
- 9.Rizk T.E., Pinals R.S. Frozen shoulder. Semin Arthritis Rheum. 1982;11:440–452. doi: 10.1016/0049-0172(82)90030-0. [DOI] [PubMed] [Google Scholar]
- 10.Tighe C.B., Oakley W.S., Jr. The prevalence of a diabetic condition and adhesive capsulitis of the shoulder. South Med J. 2008;101:591–595. doi: 10.1097/SMJ.0b013e3181705d39. 2008/05/14. [DOI] [PubMed] [Google Scholar]
- 11.Thomas S.J., McDougall C., Brown I.D. Prevalence of symptoms and signs of shoulder problems in people with diabetes mellitus. J Shoulder Elbow Surg. 2007;16:748–751. doi: 10.1016/j.jse.2007.02.133. [DOI] [PubMed] [Google Scholar]
- 12.Moren-Hybbinette I., Moritz U., Schersten B. The clinical picture of the painful diabetic shoulder--natural history, social consequences and analysis of concomitant hand syndrome. Acta Med Scand. 1987;221:73–82. doi: 10.1111/j.0954-6820.1987.tb01247.x. [DOI] [PubMed] [Google Scholar]
- 13.Wohlgethan J.R. Frozen shoulder in hyperthyroidism. Arthritis Rheum. 1987;30:936–939. doi: 10.1002/art.1780300815. [DOI] [PubMed] [Google Scholar]
- 14.Hsu J.E., Anakwenze O.A., Warrender W.J. Current review of adhesive capsulitis. J Shoulder Elbow Surg. 2011;20:502–514. doi: 10.1016/j.jse.2010.08.023. [DOI] [PubMed] [Google Scholar]
- 15.Brue S., Valentin A., Forssblad M. Idiopathic adhesive capsulitis of the shoulder: a review. Knee Surg Sports Traumatol Arthrosc. 2007;15:1048–1054. doi: 10.1007/s00167-007-0291-2. [DOI] [PubMed] [Google Scholar]
- 16.Hannafin J.A., Chiaia T.A. Adhesive capsulitis. A treatment approach. Clin Orthop Relat Res. 2000:95–109. [PubMed] [Google Scholar]
- 17.Ettaro L., Songer T.J., Zhang P. Cost-of-illness studies in diabetes mellitus. Pharmacoeconomics. 2004;22:149–164. doi: 10.2165/00019053-200422030-00002. [DOI] [PubMed] [Google Scholar]
- 18.Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3 doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hu F.B. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34:1249–1257. doi: 10.2337/dc11-0442. 2011/05/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li X., Eichinger J.K., Hartshorn T. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery: advantages and complications. J Am Acad Orthop Surg. 2015;23:18–28. doi: 10.5435/JAAOS-23-01-18. 2014/12/30. [DOI] [PubMed] [Google Scholar]
- 21.Arce G. Arthroscopy Association of North America; 2016. Primary Frozen Shoulder Syndrome: Arthroscopic Capsular Release. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987:160–164. [PubMed] [Google Scholar]
- 23.Amstutz H.C., Sew Hoy A.L., Clarke I.C. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981:7–20. [PubMed] [Google Scholar]
- 24.Dawson J., Fitzpatrick R., Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 1996;78:593–600. [PubMed] [Google Scholar]
- 25.Lundberg B.J. The frozen shoulder. Clinical and radiographical observations. The effect of manipulation under general anesthesia. Structure and glycosaminoglycan content of the joint capsule. Local bone metabolism. Acta Orthop Scand Suppl. 1969;119:1–59. 1969/01/01. [PubMed] [Google Scholar]
- 26.Smith L.L., Burnet S.P., McNeil J.D. Musculoskeletal manifestations of diabetes mellitus. Br J Sports Med. 2003;37:30–35. doi: 10.1136/bjsm.37.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pal B., Anderson J., Dick W.C. Limitation of joint mobility and shoulder capsulitis in insulin- and non-insulin-dependent diabetes mellitus. Br J Rheumatol. 1986;25:147–151. doi: 10.1093/rheumatology/25.2.147. [DOI] [PubMed] [Google Scholar]
- 28.Nicholson G.P. Arthroscopic capsular release for stiff shoulders: effect of etiology on outcomes. Arthroscopy. 2003;19:40–49. doi: 10.1053/jars.2003.50010. [DOI] [PubMed] [Google Scholar]
- 29.Akpinar S., Ozalay M., Hersekli M.A. [Arthroscopic capsular release for frozen shoulder] Acta Orthop Traumatol Turcica. 2003;37:213–218. [PubMed] [Google Scholar]
- 30.Jerosch J. 360 degrees arthroscopic capsular release in patients with adhesive capsulitis of the glenohumeral joint--indication, surgical technique, results. Knee Surg Sports Traumatol Arthrosc. 2001;9:178–186. doi: 10.1007/s001670100194. [DOI] [PubMed] [Google Scholar]
- 31.Pollock R.G., Duralde X.A., Flatow E.L. The use of arthroscopy in the treatment of resistant frozen shoulder. Clin Orthop Relat Res. 1994:30–36. [PubMed] [Google Scholar]
- 32.Handa A., Gotoh M., Hamada K. Vascular endothelial growth factor 121 and 165 in the subacromial bursa are involved in shoulder joint contracture in type II diabetics with rotator cuff disease. J Orthop Res. 2003;21:1138–1144. doi: 10.1016/S0736-0266(03)00102-5. [DOI] [PubMed] [Google Scholar]
- 33.Rosenbloom A.L., Silverstein J.H. Connective tissue and joint disease in diabetes mellitus. Endocrinol Metab Clin N Am. 1996;25:473–483. doi: 10.1016/s0889-8529(05)70335-2. [DOI] [PubMed] [Google Scholar]
- 34.Monnier V.M., Glomb M., Elgawish A. The mechanism of collagen cross-linking in diabetes: a puzzle nearing resolution. Diabetes. 1996;45(Suppl 3):S67–S72. doi: 10.2337/diab.45.3.s67. [DOI] [PubMed] [Google Scholar]
- 35.Jerosch J., Filler T.J., Peuker E.T. Which joint position puts the axillary nerve at lowest risk when performing arthroscopic capsular release in patients with adhesive capsulitis of the shoulder? Knee Surg Sports Traumatol Arthrosc. 2002;10:126–129. doi: 10.1007/s00167-001-0270-y. [DOI] [PubMed] [Google Scholar]
- 36.Noud P.H., Esch J. Complications of arthroscopic shoulder surgery. Sports Med Arthrosc Rev. 2013;21:89–96. doi: 10.1097/JSA.0b013e31829006f0. [DOI] [PubMed] [Google Scholar]
- 37.Baker P., Nanda R., Goodchild L. A comparison of the Constant and Oxford shoulder scores in patients with conservatively treated proximal humeral fractures. J Shoulder Elbow Surg. 2008;17:37–41. doi: 10.1016/j.jse.2007.04.019. 2007/11/27. [DOI] [PubMed] [Google Scholar]
- 38.Yian E.H., Contreras R., Sodl J.F. Effects of glycemic control on prevalence of diabetic frozen shoulder. J Bone Joint Surg Am. 2012;94:919–923. doi: 10.2106/JBJS.J.01930. 2012/05/24. [DOI] [PubMed] [Google Scholar]