1. Introduction
The technique for pedicle screw instrumentation of the spine has gone through significant progress over the last two decades. The pedicle screws were initially used in the lumbar spine but as the surgeons have become more comfortable with the complex anatomy required for accurate screw placement, the technique for pedicle instrumentation has evolved to include their use in the thoraco-lumbar, thoracic and cervical levels.1
However, in the thoracic spine, the benefits of pedicle screws have been tempered by their potential risks and violation leading to spinal cord injury, pedicle fracture, nerve root compression, visceral injuries, vascular lesions and improper stabilization. Furthermore, the narrow and inconsistent shape of the thoracic pedicles, especially in spinal deformity, make pedicle screw placement technically challenging at this level.2
The “free-hand” technique for placement of pedicle instrumentation relies completely on the use of visible as well as palpable anatomic landmarks for accurate pedicle screw placement. Because of the variability in these individual parameters themselves, “free-hand” pedicle instrumentation in the upper and mid-thoracic spine based exclusively on anatomic landmarks may be imprecise and eventually lead to unacceptable rates of misplaced screws. In fact, both clinical and cadaveric studies have shown that about 15%–50% of thoracic screws placed using “freehand” technique may violate the pedicle cortex3,4,.5
It is still a matter of debate, but it seems that the addition of fluoroscopy modestly improves the accuracy of screw placement, especially in the upper and middle thoracic spine.6 However the impediment in use of fluoroscopy to obtain lateral views of the mid- and upper thoracic spine, the prolongation of operating time and the hazards of radiation exposure especially to the surgeon make “fluoroscopy assisted” technique of pedicle screw insertion less favourable.
The purpose of this post-operative CT scan based study is to determine the incidence of pedicle breach by screws applied by free hand as well as fluoroscopy guided techniques as well as the significance in difference in outcome of both the techniques with respect to safety, accuracy, time duration, radiation exposure and complications.
2. Materials and methods
A CT based prospective randomised comparative study was performed on adult patients who underwent posterior instrumentation by pedicle screw construct in the thoracic spine in a tertiary level centre for a period of 2 years. The study included 100 thoracic pedicle screws applied for indications including trauma, tumours and infections especially Tuberculosis. Those screws applied in conditions like pedicle fracture, deformed spine, myelomeningocoele and congenital abnormalities where the pedicle was deformed were excluded from the study.
The pedicle screws were applied by the two techniques on either side of the spine, the side with the specific technique decided based on Systematic Random Sampling. Irrespective of the side of application of the screws by a specific technique, the screws by free hand technique were applied first to eliminate the bias of prior orientation to the pedicle entry point and pedicle tract. Pedicle screws of the same size were applied on either side for each vertebral level.
2.1. Free-hand technique
2.1.1. Pedicle screw entry
Table 1: Entry point for pedicle screw based on the Intersection method.
Table 1.
Entry point for thoracic pedicle screw.
| Cephalad-Caudad Starting Points | Level | Medial –Lateral Starting Points |
|---|---|---|
| Middle of Transverse Process | T1-T4 | Lateral to mid-point of facet Joint |
| Upper end of Transverse Process | T5-T8 | Base and middle of facet joint |
| Middle of Transverse Process | T9-T12 | Slightly medial to lateral edge of the pars interarticularis |
The entry is created using an awl with stopper. The entry is then probed with a ball tip in the anterior, medial, lateral, superior and inferior directions making sure that cortical bone is felt in all directions.
Fig. 1A (Original Picture): Pedicle Screw entry point marked using the intersection method.
Fig. 1A.
Pedicle Screw entry point marked using the intersection method.
Fig. 1B (Original Picture): Entry created with starter. Pedicle screw tract (All the screws used were from standard manufacturers).
Fig. 1B.
Entry created with starter.
Once the entry has been created, the gear shift is used to create the tract for the pedicle screw. This thoracic gearshift is 2 mm blunt-tipped, slightly curved and makes a pathway with a total diameter of approximately 4 mm. The gearshift is initially pointed lateral as a safety measure to avoid medial wall perforation. After inserting the tip approximately 15–20 mm (the length of the pedicle), the gearshift is removed and the tip turned to face medial. Before advancing the pedicle finder, place the tip carefully to the base of the prior hole. This technique is extremely useful as vertebral rotation may be deceiving. The path down the pedicle is then continued medial into the body with an ultimate depth averaging 40–45 mm for the lower thoracic region, 35–40 mm in the mid thoracic region and 30–35 mm for the proximal thoracic region in adolescents and most adults. The tract is probed for every 5 mm progression of the gear shift. Progression with the thoracic gearshift should proceed in a smooth and consistent manner with a snug feel because of the small size of the thoracic pedicles. Any sudden advancement of the gearshift suggests penetration into soft tissue and thus a pedicle wall violation or vertebral body violation.
Fig. 2A (Original Picture): Pedicle screw tract created using gear shift.
Fig. 2A.
Pedicle screw tract created using gear shift.
Fig. 2B (Original Picture): Depth of the tract based on the markings on the gear shift.
Fig. 2B.
Depth of the tract based on the markings on the gear shift.
2.2. Fluoroscopy guided technique
This method begins with obtaining a true antero-posterior view of the vertebra. The superior endplate should appear as a sharply defined line and with the superior most portion of the pedicle just cephalic to the endplate. The pedicles should be symmetrical with one another.
The tip of the spinous process should be superimposed in the midline of the vertebra. The starter is positioned near the superior medial base of the transverse process superimposed at the 2-o'clock position for the right pedicle and the 10-o'clock position for the left pedicle and is used to penetrate the cortex and act as the starting point for a pedicle awl. The awl is advanced in small increments, monitoring the antero-posterior image. The awl should be directed medially so that it crosses from the lateral cortex to the medial cortex of the pedicle as it penetrates deeper.
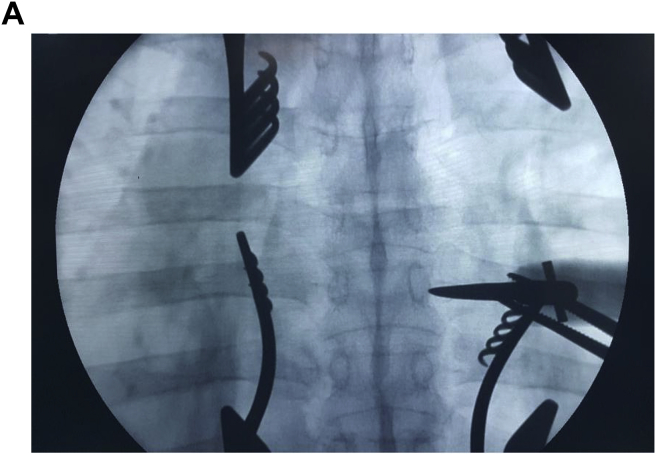
Fig. 3A (Original Picture): Pedicle entry created under fluoroscopy guidance – Antero-posterior view.
Fig. 3A.
Pedicle entry created under fluoroscopy guidance – Antero-posterior view.
Fig. 3B (Original Picture): Pedicle tract created under fluoroscopy guidance – Antero-posterior view.
Fig. 3B.
Pedicle tract created under fluoroscopy guidance – Antero-posterior view.
Trajectory of the awl should be such that the tip of awl rests at the medial cortex image after advancing to a depth of around 18 mm. This will allow the awl to traverse the length of the pedicle and enter the posterior vertebral body before becoming medial to the medial margin of the pedicle. This can be confirmed on lateral image intensifier views if the anatomy is atypical, however the lateral images are not always clearly distinctive especially with respect to the upper and middle thoracic spine.
Fig. 4 (Original Picture): Depth of tract under fluoroscopy guidance– Lateral view.
Fig. 4.
Depth of tract under fluoroscopy guidance– Lateral view.
As the awl is advanced, it should be directed slightly caudally. Once the awl is confirmed to have entered the vertebral body, it is advanced to the desired depth. It is not necessary to advance it into the anterior third of the body. Use a small ball-tipped probe to sound the pedicle for cortical breaches in all four quadrants and to confirm that the vertebral body was not penetrated anteriorly.
Post-operative CT assessment of the accuracy of the thoracic pedicle screws.
The position of each pedicle screw in relation to the corresponding pedicle is assessed by CT post-operatively.
The position is assessed for cortical breach in five directions i.e. anterior, medial, lateral, superior and inferior. The cortical breach if present is graded as per the Gertzbein and Robbins classification.
Fig. 5 (Original Picture): Post-operative CT assessment of screw position within the pedicle.
Fig. 5.
Post-operative CT assessment of screw position within the pedicle.
3. Results
44% of the thoracic pedicle screws were applied for tuberculosis spine, 50% for fracture and 6% for multiple myeloma.
44% of the screws were applied in the T5-T8 levels while 46% were in T9-T12 levels and 10% in T1-T4 levels.
A total of 349 C-Arm shots were taken for 50 screws inserted via the fluoroscopy guided technique. Hence an average of 7.0 C-Arm shots were taken per screw inserted.
By the free hand technique, 62% (31) of the screws took less than 2 min each for insertion while 34% (17) between 2 and 4 min and only 4% (2) took more than 4 min. No screws needed more than 6 min to insert by the free hand technique. Compared to this 48% (24) screws and 40% (20) screws applied by the fluoroscopy guided method took 4–6 min and 2–4 min respectively. Only 6% (3) screws needed less than 2 min to apply with the same number of screws taking more than 6 min. The results when evaluated by the Paired-t test shows a p value < 0.01.
The study revealed 78% of the screws were within the pedicle without violating the cortex in any direction. Among the screws that violated the cortex, 54.5% of the violation was caused by applying the screws by the free hand technique. Also noted was that the breach occurred equally in the medial and lateral directions. There were no breaches in the anterior, superior or inferior directions by either of the techniques.
Considering screws applied by free hand technique, there is only 1 breach which is violating the cortex by more than 4 mm and it is in the medial direction. There are 3 breaches (lateral) violating the cortex between 2 and 4 mm and there are 8 breaches with less than 2 mm violation (4 medial and 4 lateral). The fluoroscopy guided technique had only 3 violations in the 2–4 mm range (2 lateral and 1 medial) and 7 violations in the less than 2 mm group (5 medial and 2 lateral).
When these results were assessed by the McNemar Chi Square test Exact Significance of 0.481 was obtained.
64% (14) breaches occurred in the T5-T8 segments, 27% (6) breaches in the T1-T4 segments and 9% (2) in the T9-T12 segments.
4. Discussion
Our study shows the average time taken for a screw to be applied by free hand is almost 2 min less as compared to screws applied under fluoroscopy guidance which when evaluated by the Paired-t test establishes a statistically significant difference. The average number of C-Arm shots (7) per screw applied under fluoroscopy guidance lies between values recorded by Rampersaud et al.7 (8.5 shots per screw) and Archit Agarwal et al.8 (5 shots per screw). The radiation exposure though is well within the permissible limit, studies are yet to determine the long term accumulative effects.
The most significant part of the study was comparing the accuracy of pedicle screws applied by free hand and fluoroscopy guided methods. The results of the study when assessed by the McNemar Chi Square test Exact Significance of 0.481 was obtained which establishes no significant difference in the incidence in breach when the screws are applied by either technique. Also there were no complications recorded by screws inserted by either technique.
Our study shows that 10% of the screws applied by free hand had a medial breach. These values are comparable to or less than previously reported studies of 9.23% as reported by Archit Agarwal et al., 13.4% by Fisher et al.9 and 23.33% by Vaccaro et al.10 The occurrence of a lateral breach of 12% by free hand is less compared to reports of 17.71% and 17.9% by Vaccaro et al. and Fischer et al. respectively.
Considering the fluoroscopy guided technique, 12% of the screws applied by this method had a medial breach while only 8% had a lateral breach. Though the lateral breach is comparable with that reported by Archit Agarwal et al. the incidence of medial breach by this method in our study is higher compared to the 7% reported.
Belmont et al. reported a 6% anterior breach while our study did not have screws with cortical breach in the anterior direction.11
4.1. Demerits of the study
-
1.
Small number of screws
-
2.
Well experienced Spine surgeon
-
3.
Excellent C-Arm and Operation theatre setup.
5. Conclusion
Thoracic pedicle screw insertion is a challenging surgical technique one which requires meticulous preparation and execution. By this study we have been able to establish that the thoracic pedicle screw insertion by the free hand technique though has a steep learning curve and requires a precise knowledge of the thoracic pedicle anatomy; it is a safe, less time consuming and less harmful procedure with respect to radiation exposure and though the incidence is less, there is still cortical breach in spite of screw application under fluoroscopy guidance by the senior spine surgeon.
Contributor Information
Vinod V. Rajan, Email: vinodv07@gmail.com.
Chandhan Murugan, Email: m_chandhan@yahoo.com.
References
- 1.Mattei Tobias A, Meneses Murilo S, Milano Jeronimo B, Ramina Ricardo. Free-hand” technique for thoracolumbar pedicle screw instrumentation: critical appraisal of current “State-of-Art”. Neurol India. 2009;57:715–721. doi: 10.4103/0028-3886.59465. [DOI] [PubMed] [Google Scholar]
- 2.Zeiller S.C., Lee J., Lim M, Vaccaro A.R. Posterior thoracic segmental pedicle screw instrumentation: evolving methods of safe and effective placement. Neurol India. 2005;53:458–465. doi: 10.4103/0028-3886.22613. [DOI] [PubMed] [Google Scholar]
- 3.Liljenqvist U.R., Halm H.F., Link T.M. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 4.Cinotti G., Gumina S., Ripani M., Postacchini F. Pedicle instrumentation in the thoracic spine. A morphometric and cadaveric study for placement of screws. Spine. 1999;24:114–119. doi: 10.1097/00007632-199901150-00003. [DOI] [PubMed] [Google Scholar]
- 5.Weinstein J.N., Spratt K.F., Spengler D., Brick C., Reid S. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine. 1988;13:1012–1018. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Gertzbein S.D., Robbins S.E. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–15. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Rampersaud Y.R., Foley K.T., Shen A.C., Williams S., Solomito M. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine. 2000;25:2637–2645. doi: 10.1097/00007632-200010150-00016. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal Archit, Chauhan Vijendra, Singh Deepa, Shailendra Raghuvanshi, Maheshwari Rajesh, Juyal Anil. Pedicle screw fixation in dorsolumbar spine by freehand versus image assisted technique. Indian J Orthop. May 2016;50(3):243–249. doi: 10.4103/0019-5413.181779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher C.G., Sahajpal V., Keynan O. Accuracy and safety of pedicle screw fixation in thoracic spine trauma. J Neurosurg Spine. 2006 Dec;5(6):520–526. doi: 10.3171/spi.2006.5.6.520. [DOI] [PubMed] [Google Scholar]
- 10.Vaccaro A.R., Rizzolo S.J., Balderston R.A. Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Belmont P.J., Jr., Klemme W.R., Robinson M., Polly D.W., Jr. Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine. 2002;27:1558–1566. doi: 10.1097/00007632-200207150-00015. (Phila Pa 1976) [DOI] [PubMed] [Google Scholar]