Abstract
Vitamin B12 deficiency has been associated with increased risk of adverse pregnancy outcomes. Few prospective studies have investigated the burden or determinants of vitamin B12 deficiency early in life, particularly among pregnant adolescents and their children. The objectives of this study were to determine the prevalence of vitamin B12 deficiency and to examine associations between maternal and neonatal vitamin B12 status in a cohort study of healthy pregnant adolescents. Serum vitamin B12 and folate concentrations were measured in adolescents at mid-gestation (n = 124; 26.4 ± 3.5 weeks) and delivery (n = 131; 40.0 ± 1.3 weeks), and in neonates at birth using cord blood. Linear regression was used to examine associations between maternal and neonatal vitamin B12 status. Although the prevalence of vitamin B12 deficiency (<148.0 pmol/L; 1.6%) in adolescents was low during pregnancy, 22.6% of adolescents were vitamin B12 insufficient (<221.0 pmol/L; 22.6%) at mid-gestation. Maternal vitamin B12 concentrations significantly decreased from mid-gestation to delivery (p < 0.0001), and 53.4% had insufficient vitamin B12 status at delivery. Maternal vitamin B12 concentrations (p < 0.001) and vitamin B12 deficiency (p = 0.002) at delivery were significantly associated with infant vitamin B12 concentrations in multivariate analyses, adjusting for gestational age, maternal age, parity, smoking status, relationship status, prenatal supplement use, pre-pregnancy body mass index, race, and intake of vitamin B12 and folate. Maternal vitamin B12 concentrations significantly decreased during pregnancy and predicted neonatal vitamin B12 status in a cohort of healthy pregnant adolescents.
Keywords: vitamin B12, micronutrients, pregnancy, adolescents, folate
1. Introduction
Vitamin B12 deficiency (serum vitamin B12 <148.0 pmol/L) is a major public health problem globally [1,2]. Although the overall prevalence of vitamin B12 deficiency in the United States is estimated to be relatively low (6%), the burden of vitamin B12 deficiency is higher in the elderly, pregnant women, and young children (6–25%) [3]. Pregnant adolescents are at increased risk for a variety of micronutrient deficiencies and pregnancy complications, though there is limited data from this high-risk obstetric population.
Vitamin B12 deficiency in pregnancy has been associated with increased risk of pregnancy outcomes, including spontaneous abortion, pregnancy loss, intrauterine growth restriction, low birthweight (<2500 g), and neural tube defects (NTDs) [4,5,6,7,8,9,10,11,12,13,14,15]. Inadequate supply of vitamin B12 in pregnancy and early childhood can lead to long-term deficits in growth development in children [16,17].
Maternal vitamin B12 concentrations during pregnancy are thought to predict fetal [18,19,20,21,22,23,24,25,26] and early infant [25,27,28,29] vitamin B12 status. Previous cross-sectional studies in Norway, Turkey, Germany, United Kingdom, Serbia, and Brazil have noted a significant correlation between maternal and infant vitamin B12 status at delivery [18,20,21,22,30,31,32,33]; however, in one study in Belgium, maternal and infant vitamin B12 concentrations were not significantly correlated [34]. In one study in Germany, maternal serum vitamin B12 and holotranscobalamin (holoTC) concentrations at delivery were significantly correlated with cord blood holoTC concentrations (p < 0.05) [18]. In contrast, findings from cross-sectional studies examining the associations between maternal and infant vitamin B12 concentrations later in the postpartum period have been heterogeneous [35,36,37,38,39,40]. Maternal vitamin B12 and holoTC concentrations were significantly correlated with infant vitamin B12 concentrations in the first month (i.e., 2–30 days) postpartum in a study in Turkey [38]. In analyses in mother–infant dyads in the first 6 months postpartum, maternal and infant vitamin B12 concentrations were significantly associated in Canada and Cambodia (i.e., 3–27 weeks) [37], but not in India (i.e., 1–6 months) [35].
Prospective studies to date in The Netherlands, Norway, Turkey, India, and Spain have reported significant associations [19,23,24,26,29] between maternal vitamin B12 status during pregnancy and infant vitamin B12 status in cord blood or serum. In a prospective study in India, maternal vitamin B12 status during pregnancy was associated with infant vitamin B12 concentrations at 6 weeks of age [28]. In contrast, a study in Norway was conducted to examine the associations between maternal vitamin B12 biomarkers during pregnancy and vitamin B12 status in infants at birth and 6 months of age; maternal vitamin B12 concentrations did not significantly predict cord blood or infant vitamin B12 status, although there were significant associations noted for other biomarkers (i.e., maternal holoTC, holohaptocorrin (holoHC), and methylmalonic acid (MMA)) [25]. Although some studies to date have been conducted to examine vitamin B12 status in pregnant adolescents [41,42,43], most studies investigating the associations between maternal and infant vitamin B12 status have been conducted among adult pregnant women (i.e., 18 to 40 years). Of these studies, three cross-sectional studies reported participants which included adolescents, with age ranges of 15 to 38 years [32], 16 to 40 years [38], and 17 to 43 years [27]. However, adolescents comprised a small proportion (<15%) of the sample, and data presented were not stratified by age group, which constrained analysis and interpretation of findings for adolescents. There are limited prospective studies on the associations between maternal and infant vitamin B12 status conducted in high-risk obstetric groups such as adolescents.
Pregnant adolescents are at increased risk for a variety of micronutrient deficiencies and pregnancy complications [41,44]. The inadequate dietary intake of key nutrients among adolescents in industrialized countries [45], coupled with increased nutritional requirements for growth and development, warrants concern for health outcomes among pregnant adolescents. However, few data exist on the extent of vitamin B12 deficiency or its implications for fetal and child health in this high-risk obstetric population, which comprises over 5% of the US population and 11% globally [46,47]. Well-designed prospective studies are needed to elucidate the burden of vitamin B12 insufficiency in this key high-risk population and its implications for maternal and child health.
We, therefore, conducted a prospective observational analysis to: (1) determine the prevalence of vitamin B12 deficiency and insufficiency in pregnant adolescents and their infants; and (2) examine the associations of maternal and neonatal vitamin B12 status in healthy pregnant adolescents.
2. Materials and Methods
2.1. Study Population
Participants included in this study were enrolled in one of two prospective cohort studies funded by the United States Department of Agriculture (USDA). One study examined maternal and fetal bone health among pregnant adolescents (“bone health study”) and collected maternal blood samples at mid-gestation and delivery, and cord blood samples at delivery. The other study evaluated iron status and anemia through gestation in pregnant adolescents aged 13 to 18 years and their infants (“anemia study”), and collected maternal and cord blood samples only at delivery. Both studies were observational cohort studies and not clinical trials (and, thus, do not need to be registered, as per protocol for clinical trials). Pregnant adolescents were recruited between 2006 and 2012, from the Rochester Adolescent Maternity Program (RAMP) in Rochester, New York.
Adolescents were eligible to participate if their pregnancies were 12 to 30 weeks in gestation at the time of the adolescents’ enrollment in prenatal care at RAMP, and if the adolescents were healthy and carrying a single fetus. Adolescents were excluded if they had any known medical complications, including diabetes, preeclampsia, gestational hypertension, eating disorders, gastrointestinal diseases, HIV infection, or any other diagnosed medical conditions. Data on maternal and neonatal iron status [48,49] and on vitamin B12 transporters in placental tissue from this population [50] have been previously reported.
2.2. Ethics
Written informed consent was obtained from all study participants. The research protocol and study procedures were approved by the Institutional Review Boards (IRB) at Cornell University and the University of Rochester. The IRB approval included laboratory analyses of micronutrients in maternal and infant cord blood samples, including vitamin B12 and folate concentrations.
2.3. Follow-Up Procedures
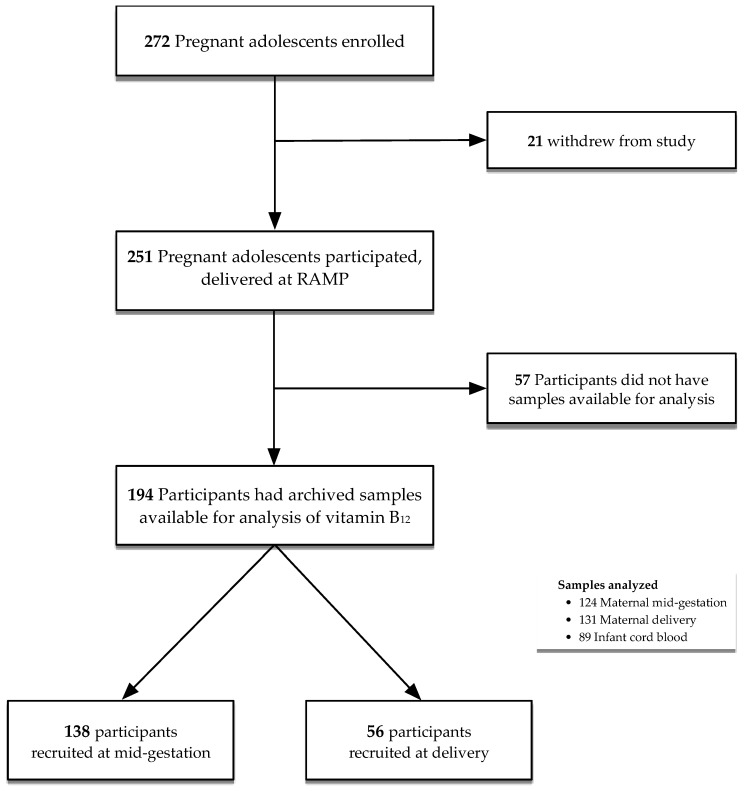
Structured interviews were conducted to collect demographic information, including maternal age, educational level, socioeconomic status, and obstetric history at the baseline clinic visit. Detailed clinical, dietary (i.e., 24-h dietary recall), anthropometric, and biochemical data were collected at each visit. The participant recruitment and flow chart are presented in Figure 1. Of 251 participants who delivered at RAMP, a total of 194 participants (n = 138 participants in the bone study, recruited at mid-gestation; n = 56 participants in the anemia study, recruited at delivery) had archived blood samples available for analysis (Figure 1). All adolescents attending the Rochester Adolescent Maternity Program were prescribed a prenatal supplement as standard of care, which contained 27 mg iron, 12 μg vitamin B12, 1000 μg folic acid, and other micronutrients (i.e., 1200 μg vitamin A, 120 mg vitamin C, 10 μg vitamin D3, 22 mg vitamin E, 1.84 mg thiamin, 3 mg riboflavin, 20 mg niacin, 10 mg vitamin B6, 200 mg calcium, 25 mg zinc, and 2000 μg copper).
Figure 1.
Participant flow diagram.
2.4. Laboratory Analyses
Non-fasting maternal venous blood samples (mid-gestation, delivery) and infant cord blood samples were allowed to clot at room temperature, separated by centrifugation, processed, and stored below −80 °C until analysis. A total of 124 maternal mid-gestation (26.4 ± 3.5 weeks), 131 maternal delivery (40.0 ± 1.3 weeks), and 89 infant cord blood samples were available for analysis.
Vitamin B12 concentrations were measured by electrochemiluminescence using the IMMULITE 2000 immunoassay system (Siemens Medical Solutions Diagnostics, Los Angeles, CA, USA). Three levels of controls (Bio-Rad) were used for serum vitamin B12, with inter-assay coefficients of variation (CV) of 4.2% for Level 1 and 4.8% for Level 3. Serum folate concentrations were measured using the IMMULITE 2000 immunoassay system. The Bio-Rad Liquichek Immunoassay Plus Control (High & Low) were used as controls, with intra-assay precision of 6.7% and inter-assay precision of 6.6%.
2.5. Definitions of Outcomes
Conventional cutoffs were used to categorize variables where available; otherwise, medians of variables were defined based on their distributions in the population. Vitamin B12 deficiency and insufficiency were defined, following standard Centers for Disease Control and Prevention (CDC) definitions, as less than 148 pmol/L and less than 221.0 pmol/L, respectively [51]. Anemia was defined as hemoglobin <11.0 g/dL during the first and third trimesters, <10.5 g/dL during the second trimester, and <11.0 g/dL at delivery; and anemia status was adjusted for race [52]. Folate deficiency was defined as <6.8 nmol/L [51]. Maternal BMI was defined as the ratio of weight in kg to height in m2 (kg/m2), and categorized as <18.5, 18.5 to <25.0, 25.0 to <30.0, and ≥30.0 kg/m2, in accordance with the CDC and World Health Organization (WHO) classifications [53]. Infant low birthweight was defined as <2500 g. Infant ponderal index was calculated as the ratio of weight in g to length in cm3 (g/cm3 × 100).
2.6. Statistical Analyses
Binomial and linear regression models were used to examine the associations of maternal vitamin B12 status at mid-gestation and delivery with infant vitamin B12 status at birth. Binomial regression models were used to obtain risk ratio (RR) estimates for dichotomous variables [54,55,56]. Non-normally distributed variables were natural logarithmically transformed to ensure normality before further analysis. We also examined the associations between maternal and infant folate status. The values in Table 1 are presented as non-transformed values for interpretation purposes.
Table 1.
Characteristics of the study population.
| Variables a | Original Cohort (n = 251) |
Current Study (n = 194) |
Recruited at Mid-Gestation (n = 138) |
Recruited at Delivery (n = 56) |
|---|---|---|---|---|
| Maternal | ||||
| Age at enrollment, years | 17.3 (16.5, 18.1) | 17.3 (16.5, 18.1) | 17.3 (16.4, 18.1) | 17.3 (16.6, 18.1) |
| Age at delivery, years | 17.5 (16.7, 18.3) | 17.6 (16.8, 18.4) | 17.6 (16.7, 18.4) | 17.4 (16.9, 18.2) |
| <16 years, % (n) | 12.0 (30) | 9.8 (19) | 9.4 (13) | 10.7 (6) |
| Gestational age at delivery, weeks | 39.9 (38.7, 40.7) | 40 (39.0, 40.9) | 40.0 (38.9, 40.9) | 40.0 (39.2, 41.0) |
| Pre-term (<37 weeks), % (n) | 8.0 (20) | 7.8 (15) | 8.8 (12) | 5.4 (3) |
| Parity ≥1, % (n) | 17.3 (43) | 15.1 (29) | 8.7 (12) | 30.9 (17) |
| Smoking at enrollment, % (n) | ||||
| Never a smoker | 77.8 (189) | 78.5 (150) | 77.5 (107) | 81.1 (43) |
| Past smoker | 15.2 (37) | 14.4 (27) | 12.3 (17) | 18.9 (10) |
| Current smoker | 7.0 (17) | 7.3 (14) | 10.1 (14) | 0.0 (0) |
| Relationship status b, % (n) | 13.5 (33) | 10.5 (20) | 1.5 (2) | 34.0 (18) |
| WIC c program participant | 60.9 (148) | 63.2 (120) | 80.0 (100) | 37.7 (20) |
| Self-reported prenatal supplement use, % (n) | ||||
| ≥2 pills per week | 54.1 (131) | 55.5 (106) | 56.6 (77) | 52.7 (29) |
| Dietary folate, µg/day | 617.2 (397.0, 948.9) | 617.2 (400.8, 950.45) | 692.7 (464.2, 1020.6) | 415.3 (283.9, 624.7) |
| Dietary vitamin B12, µg/day | 4.6 (2.7, 6.5) | 4.6 (2.7, 6.6) | 5.0 (3.7, 6.9) | 2.8 (1.4, 5.2) |
| Pre-pregnancy BMI, kg/m2 | 23.5 (20.8, 28.0) | 23.7 (20.8, 28.0) | 23.3 (20.8, 28.1) | 24.7 (20.8, 27.9) |
| <18.5 kg/m2, % (n) | 6.9 (17) | 7.3 (14) | 6.62 (9) | 9.1 (5) |
| ≥18.5 to <25 kg/m2, % (n) | 54.3 (133) | 52.4 (100) | 55.2 (75) | 45.5 (25) |
| ≥25.0 to <30 kg/m2, % (n) | 20.8 (51) | 21.5 (41) | 19.9 (27) | 25.5 (14) |
| ≥30 kg/m2, % (n) | 18.0 (44) | 18.9 (36) | 18.4 (25) | 20.0 (11) |
| Gestational weight gain (GWG), kg | 15.9 (11.8, 20.5) | 16.4 (11.8, 20.5) | 15.5 (11.8, 20.5) | 17.3 (12.3, 21.4) |
| Inadequate d GWG, % (n) | 15.0 (36) | 13.9 (26) | 14.3 (19) | 13.0 (7) |
| Within IOM range, % (n) | 22.9 (55) | 24.0 (45) | 26.3 (35) | 18.5 (10) |
| Excessive GWG, % (n) | 62.1 (149) | 62.0 (116) | 59.0 (79) | 68.5 (37) |
| Race, % (n) | ||||
| Caucasian | 27.9 (70) | 29.4 (57) | 33.3 (36) | 19.6 (11) |
| African American | 71.3 (179) | 69.6 (135) | 65.2 (90) | 80.4 (45) |
| Native American | 0.8 (2) | 1.0 (2) | 1.5 (2) | 0.0 (0) |
| Ethnicity, % (n) | ||||
| Hispanic | 24.3 (61) | 26.3 (51) | 24.6 (34) | 30.4 (17) |
| Infant | ||||
| Birthweight, g | 3206.0 (2904.0, 3550.0) | 3266.0 (2928.0, 3581.0) | 3258.0 (2892.0, 3581.0) | 3318.5 (3055.5, 3584.0) |
| Birth length, cm | 51.0 (49.0, 52.7) | 51.3 (49.5, 52.9) | 51.0 (49.5, 52.5) | 52.0 (50.0, 53.5) |
| Weight-for-length z-score < −2, % (n) | 27.0 (60) | 27.0 (47) | 27.3 (35) | 26.1 (12) |
| Ponderal index, g/cm3 × 100 | 2.4 (2.2, 2.7) | 2.4 (2.3, 2.7) | 2.4 (2.2, 2.7) | 2.4 (2.3, 2.6) |
| Male sex, % (n) | 52.8 (132) | 51.0 (99) | 50.7 (70) | 51.8 (29) |
a Values are median interquartile range (IQR) and % (n); b Data presented are adolescents that report being in a relationship during pregnancy vs. single; c The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); d Gestational Weight Gain: categorized as inadequate or excessive, using Institute of Medicine (IOM) recommendations that vary based on pre-partum body mass index (BMI).
We explored potential nonlinearity of the relationships between covariates and outcomes nonparametrically, using stepwise restricted cubic splines [57,58]. If nonlinear associations were not reported, they were not significant. The Rothman and Greenland approach was used to evaluate and adjust for confounding, in which all known or suspected risk factors for the outcome which lead to a >10% change-in-estimate were included in the models [59]. Observations with missing data for covariates were retained in analyses using the missing indicator method [60]. Statistical analyses were conducted using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC, USA).
3. Results
3.1. Baseline Characteristics
The characteristics of participants in this study are presented in Table 1. Participants and their infants enrolled in the overall cohort studies and in the current study (i.e., with available serum vitamin B12 data) were similar in terms of baseline characteristics, including maternal age, socioeconomic characteristics, and nutritional status. A total of 194 participants had archived samples available for analysis; 138 of these participants were recruited at mid-gestation (bone health study), and 56 participants were recruited at delivery (anemia study) (Figure 1). We also examined potential differences in demographic, socioeconomic, and nutritional factors between participants in the two cohort studies. These variables were identified a priori as potential confounders and were considered and adjusted for in all of the multivariate analyses. Vitamin B12 and folate concentrations were analyzed in maternal samples that were collected at mid-gestation (n = 124) and delivery (n = 131); and in infant cord blood samples (n = 89).
3.2. Maternal and Neonatal Vitamin B12 Status
Maternal and neonatal vitamin B12 status are presented in Table 2. At the mid-gestation visit (n = 124; 26.4 ± 3.5 weeks gestation), 1.6% of women were vitamin B12 deficient (n = 2/124; <148.0 pmol/L), and 22.6% were vitamin B12 insufficient (n = 28/124; <221.0 pmol/L). Maternal serum vitamin B12 concentrations significantly decreased from mid-gestation to delivery (n = 61; 39.9 ± 1.0 weeks; mid-gestation: median = 358.9, interquartile range (IQR) = 233.9, 400.7 vs. delivery: median = 226.2, IQR = 185.2, 311.8; p < 0.0001).
Table 2.
Maternal and infant vitamin B12 and folate status.
| Maternal | Infant | ||||||
|---|---|---|---|---|---|---|---|
| Mid-Gestation | Delivery | Cord Blood | |||||
| Variables a | Total | Total | Recruited at Mid-Gestation |
Recruited at Delivery | Total | Mothers Recruited at Mid-Gestation | Mothers Recruited at Delivery |
| n | 124 | 131 | 75 | 56 | 89 | 58 | 31 |
| Serum vitamin B12, pmol/L | 343.7 (237.8, 400.7) | 216.2 (161.6, 297.8) | 216.2 (173.4, 311.8) | 211.2 (158.7, 267.0) | 597.0 (471.6, 796.3) | 569.4 (478.6, 844.3) | 602.9 (406.6, 722.1) |
| <148.0 pmol/L | 1.6 (2) | 15.3 (20) | 14.7 (11) | 16.1 (9) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| ≥148 to <221.0 pmol/L | 21.0 (26) | 38.2 (50) | 37.3 (28) | 39.3 (22) | 2.3 (2) | 0.0 (0) | 6.5 (2) |
| ≥221 pmol/L | 77.4 (96) | 46.6 (61) | 48.0 (36) | 44.6 (25) | 99.8 (87) | 100.0 (58) | 93.5 (29) |
| n | 122 | 130 | 74 | 56 | 86 | 55 | 31 |
| Serum folate, nmol/L | 39.3 (31.7, 50.5) | 39.7 (31.8, 50.4) | 42.8 (32.2, 51.4) | 37.7 (28.8, 48.4) | 66.7 (53.1, 85.5) | 66.3 (52.1, 84.4) | 67.7 (55.5, 98.4) |
| ≤29.45b nmol/L | 19.7 (24) | 20.0 (26) | 13.5 (10) | 28.6 (16) | 2.3 (2) | 3.6 (2) | 0.0 (0) |
| >29.45, ≤35.79 nmol/L | 20.5 (25) | 16.9 (22) | 18.9 (14) | 14.3 (8) | 2.3 (2) | 3.6 (2) | 0.0 (0) |
| >35.79, ≤43.94 nmol/L | 19.7 (24) | 20.0 (26) | 17.6 (13) | 23.2 (13) | 4.7 (4) | 5.5 (3) | 3.2 (1) |
| >43.94, ≤52.66 nmol/L | 19.7 (24) | 22.3 (29) | 29.7 (22) | 12.5 (7) | 14.0 (12) | 12.7 (7) | 16.1 (5) |
| >52.66 nmol/L | 20.5 (25) | 20.8 (27) | 20.3 (15) | 21.4 (12) | 76.7 (66) | 74.6 (41) | 80.7 (25) |
a Values are median and interquartile range (IQR) and (%) n. b Note: No values of serum folate were <6.8 nmol/L; the cut-offs presented for serum folate are quintiles based on the distribution of serum folate concentrations at mid-gestation.
The prevalence of maternal vitamin B12 insufficiency at delivery (n = 70/131; 53.4%) was significantly higher than at mid-gestation (n = 28/124; 22.6%, p < 0.05). The prevalence of vitamin B12 insufficiency was low in infants at birth: 0.0% were vitamin B12 deficient (<148.0 pmol/L), and 2.3% were vitamin B12 insufficient (<221.0 pmol/L). No mothers or infants were folate deficient (<6.8 nmol/L) or insufficient (<10.0 nmol/L) during this study.
The associations between maternal and infant serum vitamin B12 concentrations are presented in Table 3. Maternal vitamin B12 status at mid-gestation was not significantly associated with infant serum vitamin B12 concentrations (p > 0.05).
Table 3.
Associations between maternal vitamin B12 and folate status with infant serum vitamin B12 concentrations.
| Univariate b | Multivariate c | Multivariate d | ||||||
|---|---|---|---|---|---|---|---|---|
| Maternal Variables | Time-Point | n | β (SE) | p-Value | β (SE) | p-Value | β (SE) | p-Value |
| Serum vitamin B12, a pmol/L | Mid-gestation | 54 | 0.29 (0.17) | 0.09 | 0.28 (0.16) | 0.08 | 0.31 (0.16) | 0.06 |
| Delivery (All) | 64 | 0.85 (0.12) | <0.0001 | 0.74 (0.12) | <0.0001 | 0.77 (0.12) | <0.001 | |
| Delivery (Recruited at mid-gestation) | 33 | 0.57 (0.20) | 0.004 | 0.53 (0.18) | 0.003 | 0.53 (0.16) | 0.001 | |
| Delivery (Recruited at delivery) | 31 | 1.09 (0.13) | <0.0001 | 0.97 (0.14) | <0.0001 | 1.02 (0.12) | <0.001 | |
| <148.0 pmol/L | Mid-gestation | 54 | n/a | n/a | n/a | n/a | n/a | n/a |
| Delivery (All) | 64 | −0.65 (0.16) | <0.0001 | −0.54 (0.14) | 0.0002 | −0.62 (0.15) | <0.0001 | |
| Delivery (Recruited at mid-gestation) | 33 | −0.63 (0.22) | 0.004 | −0.60 (0.19) | 0.002 | −0.56 (0.18) | 0.002 | |
| Delivery (Recruited at delivery) | 31 | −0.72 (0.22) | 0.001 | −0.59 (0.22) | 0.008 | −0.67 (0.21) | 0.002 | |
| <221.0 pmol/L | Mid-gestation | 54 | −0.16 (0.15) | 0.28 | −0.18 (0.14) | 0.20 | −0.18 (0.14) | 0.21 |
| Delivery (All) | 64 | −0.42 (0.12) | 0.0007 | −0.30 (0.12) | 0.01 | −0.33 (0.12) | 0.008 | |
| Delivery (Recruited at mid-gestation) | 33 | −0.23 (0.17) | 0.17 | −0.19 (0.16) | 0.22 | −0.26 (0.15) | 0.07 | |
| Delivery (Recruited at delivery) | 31 | −0.61 (0.17) | 0.0004 | −0.44 (0.17) | 0.01 | −0.41 (0.19) | 0.03 | |
| Serum folate a, nmol/L | Mid-gestation | 53 | −0.24 (0.14) | 0.09 | −0.24 (0.14) | 0.09 | −0.28 (0.15) | 0.06 |
| Delivery (All) | 64 | 0.12 (0.16) | 0.47 | 0.07 (0.16) | 0.68 | 0.09 (0.17) | 0.61 | |
| Delivery (Recruited at mid-gestation) | 33 | 0.09 (0.22) | 0.69 | 0.12 (0.23) | 0.60 | 0.16 (0.26) | 0.54 | |
| Delivery (Recruited at delivery) | 31 | 0.12 (0.25) | 0.63 | 0.06 (0.23) | 0.81 | 0.11 (0.22) | 0.62 | |
| <40.0 nmol/L | Mid-gestation | 53 | 0.10 (0.12) | 0.40 | 0.11 (0.12) | 0.37 | 0.14 (0.13) | 0.28 |
| Delivery (All) | 64 | −0.06 (0.13) | 0.65 | 0.02 (0.13) | 0.87 | 0.02 (0.13) | 0.88 | |
| Delivery (Recruited at mid-gestation) | 33 | −0.05 (0.17) | 0.76 | −0.08 (0.17) | 0.64 | 0.04 (0.20) | 0.86 | |
| Delivery (Recruited at delivery) | 31 | −0.08 (0.21) | 0.69 | 0.11 (0.18) | 0.56 | 0.15 (0.17) | 0.39 | |
a Statistical analyses: Linear regression models were used to examine associations between maternal vitamin B12 and folate status and infant serum vitamin B12 concentrations; vitamin B12 and folate concentrations were natural logarithmically transformed prior to analyses; b Adjusted for gestational age of sample collection; c Adjusted for gestational age of sample collection, maternal age at delivery, parity (≥1 vs. 0), ever smoked (yes vs. no), relationship status (single vs. married/in a relationship), self-reported prenatal supplement use (≥2 vs. <2 pills/week), pre-pregnancy BMI, and race (African American vs. other); d Adjusted for gestational age of sample collection, maternal age at delivery, parity (≥1 vs. 0), ever smoked (yes vs. no), relationship status (single vs. married/in a relationship), self-reported prenatal supplement use (≥2 vs. <2 pills/week), pre-pregnancy BMI, race (African American vs. other), intake of vitamin B12, and intake of folate.
At delivery, maternal serum vitamin B12 concentrations (p < 0.001) and vitamin B12 deficiency (p < 0.0001) were significantly associated with infant serum vitamin B12 concentrations in multivariate analyses, adjusting for gestational age at sample collection, maternal age, parity, smoking status, relationship status, reported prenatal supplement use, pre-pregnancy BMI, race, and intake of vitamin B12 and folate. Similarly, maternal vitamin B12 insufficiency at delivery was significantly associated with infant serum vitamin B12 concentrations (p < 0.01) in multivariate analyses, adjusting for gestational age at sample collection, maternal age, parity, smoking status, relationship status, reported prenatal supplement use, pre-pregnancy BMI, race, and intake of vitamin B12 and folate. Maternal serum folate concentrations were not significantly associated with infant serum vitamin B12 concentrations (p > 0.05).
The associations between maternal vitamin B12 and folate statuses and infant serum folate concentrations are presented in Table 4. Maternal serum folate concentrations at mid-gestation were not significantly associated with infant serum folate concentrations (p > 0.05).
Table 4.
Associations between maternal Vitamin B12 and folate status with infant serum folate concentrations.
| Univariate b | Multivariate c | Multivariate d | ||||||
|---|---|---|---|---|---|---|---|---|
| Maternal Variables | Time-Point | n | β (SE) | p-Value | β (SE) | p-Value | β (SE) | p-Value |
| Serum vitamin B12,a pmol/L | Mid-gestation | 51 | −0.04 (0.16) | 0.79 | −0.19 (0.14) | 0.17 | −0.16 (0.13) | 0.22 |
| Delivery (All) | 61 | −0.02 (0.11) | 0.88 | −0.08 (0.11) | 0.48 | −0.08 (0.11) | 0.45 | |
| Delivery (Recruited at mid-gestation) | 30 | −0.20 (0.15) | 0.18 | −0.20 (0.13) | 0.13 | −0.22 (0.12) | 0.07 | |
| Delivery (Recruited at delivery) | 31 | 0.14 (0.16) | 0.37 | 0.04 (0.15) | 0.78 | 0.06 (0.15) | 0.67 | |
| <148.0 pmol/L | Mid-gestation | 51 | n/a | n/a | n/a | n/a | n/a | n/a |
| Delivery (All) | 61 | 0.07 (0.13) | 0.60 | 0.16 (0.12) | 0.16 | 0.18 (0.12) | 0.14 | |
| Delivery (Recruited at mid-gestation) | 30 | 0.26 (0.17) | 0.13 | 0.26 (0.14) | 0.07 | 0.38 (0.13) | 0.005 | |
| Delivery (Recruited at delivery) | 31 | −0.10 (0.18) | 0.57 | 0.07 (0.17) | 0.65 | 0.03 (0.17) | 0.88 | |
| <221.0 pmol/L | Mid-gestation | 51 | −0.05 (0.14) | 0.71 | 0.01 (0.13) | 0.91 | 0.07 (0.12) | 0.54 |
| Delivery (All) | 61 | −0.01 (0.09) | 0.90 | 0.05 (0.09) | 0.58 | 0.07 (0.09) | 0.47 | |
| Delivery (Recruited at mid-gestation) | 30 | 0.18 (0.12) | 0.12 | 0.22 (0.11) | 0.04 | 0.27 (0.10) | 0.006 | |
| Delivery (Recruited at delivery) | 31 | −0.19 (0.13) | 0.15 | −0.09 (0.12) | 0.45 | −0.12 (0.13) | 0.37 | |
| Serum folate a, nmol/L | Mid-gestation | 50 | 0.27 (0.14) | 0.06 | 0.05 (0.13) | 0.69 | 0.003 (0.13) | 0.98 |
| Delivery (All) | 61 | 0.54 (0.09) | <0.0001 | 0.47 (0.10) | <0.0001 | 0.50 (0.10) | <0.0001 | |
| Delivery (Recruited at mid-gestation) | 30 | 0.54 (0.11) | <0.0001 | 0.55 (0.13) | <0.001 | 0.53 (0.15) | 0.0003 | |
| Delivery (Recruited at delivery) | 31 | 0.57 (0.13) | <0.0001 | 0.45 (0.13) | 0.0005 | 0.44 (0.12) | 0.0003 | |
| <40.0 nmol/L | Mid-gestation | 50 | −0.25 (0.12) | 0.03 | −0.13 (0.10) | 0.21 | −0.09 (0.10) | 0.39 |
| Delivery (All) | 61 | −0.42 (0.08) | <0.0001 | −0.40 (0.08) | <0.0001 | −0.42 (0.08) | <0.0001 | |
| Delivery (Recruited at mid-gestation) | 30 | −0.44 (0.09) | <0.0001 | −0.43 (0.10) | <0.0001 | −0.51 (0.12) | <0.0001 | |
| Delivery (Recruited at delivery) | 31 | −0.41 (0.12) | 0.0006 | −0.32 (0.12) | 0.01 | −0.33 (0.12) | 0.006 | |
a Statistical analyses: linear regression models were used to examine associations between maternal vitamin B12 and folate status and infant serum vitamin B12 concentrations; vitamin B12 and folate concentrations were natural logarithmically transformed prior to analyses; b Adjusted for gestational age of sample collection; c Adjusted for gestational age of sample collection, maternal age at delivery, parity (≥1 vs. 0), ever smoked (yes vs. no), relationship status (single vs. married/in a relationship), self-reported prenatal supplement use (≥2 vs. <2 pills/week), pre-pregnancy BMI, and race (African American vs. other); d Adjusted for gestational age of sample collection, maternal age at delivery, parity (≥1 vs. 0), ever smoked (yes vs. no), relationship status (single vs. married/in a relationship), self-reported prenatal supplement use (≥2 vs. <2 pills/week), pre-pregnancy BMI, race (African American vs. other), intake of vitamin B12, and intake of folate
Maternal serum folate concentrations at delivery were significantly associated with infant serum folate concentrations (p < 0.0001) in multivariate analyses, adjusting for gestational age at sample collection, maternal age, parity, smoking status, relationship status, prenatal supplement use, pre-pregnancy BMI, race, and intake of vitamin B12 and folate. Similarly, lower maternal serum folate concentrations (<40.0 nmol/L) at delivery were associated with lower infant serum folate concentrations (p < 0.0001) in multivariate analyses, adjusting for gestational age at sample collection, maternal age, parity, smoking status, relationship status, prenatal supplement use, pre-pregnancy BMI, race, and intake of vitamin B12 and folate.
4. Discussion
In this prospective analysis among pregnant adolescents, maternal vitamin B12 concentrations significantly decreased during pregnancy and predicted neonatal vitamin B12 status. Although the prevalence of vitamin B12 deficiency (<148.0 pmol/L; 1.6%) was low in adolescents during pregnancy, 22.6% of adolescents were vitamin B12 insufficient (<221.0 pmol/L; 22.6%) at mid-gestation. Maternal serum vitamin B12 concentrations decreased significantly during pregnancy, and at delivery, 15.3% of mothers were vitamin B12 deficient and 53.4% were vitamin B12 insufficient (Table 2).
This is among the first studies conducted to date to examine the burden of vitamin B12 deficiency in pregnant adolescents and its association with neonatal vitamin B12 status in this high-risk obstetric population. The prevalence of vitamin B12 deficiency in this study was low (1.6% mid-gestation, 15.3% delivery) and similar to a previous study conducted in Spain among pregnant adolescents (vitamin B12 deficiency, T1: 8.3%) [42]. However, the prevalence of vitamin B12 deficiency noted in this study was lower than previous studies conducted in pregnant adolescents in Canada (median, T3: 158 pmol/L, IQR: 114, 207 pmol/L; vitamin B12 <148.0 pmol/L: 43%) [43] and in Venezuela (vitamin B12 <200.0 pg/mL (<148.0 pmol/L), T1: 50.0%, T2: 58.8%, T3: 72.5%) [61]. Maternal vitamin B12 concentrations in our study were also higher than in a previous study in pregnant adolescents in the United Kingdom (geometric mean, Trimester 3 (T3): 177 pmol/L, 95% CI: 169, 185 pmol/L) [41].
The prevalence of vitamin B12 insufficiency (<221.0 pmol/L), however, was high in this study at both mid-gestation (22.6%) and delivery (53.4%). Although all participants were prescribed prenatal vitamins containing vitamin B12 and folic acid, self-reported adherence to prenatal supplements was low. Additionally, while most participants reported dietary intake of vitamin B12 at or above the RDA for this group (i.e., median (IQR): 4.5 (2.6, 6.6) µg/day vs. RDA: 2.6 µg/day), approximately 25% of participants reported dietary intake below the RDA. In addition to low dietary intake of vitamin B12, vitamin B12 absorption could also be impaired by inadequate bioavailability, losses from processing and cooking animal-source foods, high dose folic acid, metabolic changes during pregnancy (e.g., hemodilution, fetal transfer), gastrointestinal symptoms, infections, and medications [4,62]. For example, since vitamin B12 is bound to protein carriers in the food matrix, vitamin B12 bioavailability may vary by food source [62,63].
The decline in maternal vitamin B12 concentrations during gestation in this study is also consistent with previous studies in adult pregnant women in Canada [64], Spain [26], Norway [25,29], and India [28,65], and in 12 of 13 longitudinal studies included in a systematic review of vitamin B12 status and birthweight in adult pregnant women [66]. The observed decrease in vitamin B12 concentrations throughout pregnancy could be due to hemodilution, increased protein synthesis, increased requirements for methyl donors during gestation, or a low intake or adherence to prenatal supplements to meet increased requirements [67]. However, there are limited data from pregnant adolescents, who have higher nutritional requirements for their own growth.
The prevalence of vitamin B12 deficiency and insufficiency in infants was low in this study (0–3%). Infant vitamin B12 concentrations were 2.5-fold higher than maternal vitamin B12 concentrations at delivery. These findings are consistent with previous studies in adult pregnant women, which have reported neonatal vitamin B12 concentrations 27% to 100% higher than maternal concentrations at delivery [18,19,21,26,30,31,33] and mid-gestation [23], although this has not been reported in all studies [22,25,28,29]. Higher vitamin B12 concentrations in offspring indicate active transfer to the fetus, which may occur due to upregulation of placental B12 transporter proteins or other active transport mechanisms that have yet to be established.
In this study, maternal vitamin B12 status at delivery, but not at mid-gestation, was significantly associated with infant vitamin B12 status. Maternal vitamin B12 status at delivery has been associated with vitamin B12 status in offspring at birth in previous cross-sectional studies [18,20,21,22,30,31,32,33]. There are, however, limited prospective data on maternal vitamin B12 status during pregnancy and its association with infant vitamin B12 status—particularly among adolescents—to compare findings. Evidence from studies in adult pregnant women have reported significant correlations between maternal vitamin B12 status during pregnancy and their infants [19,23,24,26,29]. Few prospective analyses to date have considered potential confounders of these associations in multivariate analyses [25,28]. In a recent study in adult pregnant women (median age = 22, IQR = 20–24 years) in Southern India, maternal vitamin B12 status during each trimester was associated with infant vitamin B12 status at 6 weeks of age [28], even after adjusting for maternal vitamin B12 supplementation. Similarly, a study conducted among pregnant women (mean age = 29.9, SD = 4.4 years) in Norway found that maternal vitamin B12 levels did not significantly predict cord blood or infant vitamin B12 status, although other vitamin B12 biomarkers (i.e., maternal holoTC, holoHC, MMA) were associated [25].
This study has several limitations. Neonatal micronutrient status was assessed at a single time point from cord blood, precluding our ability to evaluate longer-term impacts on infant vitamin B12 status or functional outcomes. Longitudinal data on maternal vitamin B12 concentrations were available only from a subset of participants in the parent cohort studies, limiting our ability to examine changes in vitamin B12 concentrations during pregnancy. Although participants in both cohort studies had similar sociodemographic characteristics (e.g., maternal age, gestational age at initiation of prenatal care, adherence to prenatal vitamins, gestational age at delivery), participants enrolled at mid-gestation (bone study) were more likely to be participants in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) program, current smokers, Caucasian, primiparous, and had higher self-reported dietary intake of vitamin B12 and folate, compared to participants who were recruited at delivery (anemia). All of these variables were identified a priori as potential confounders and were considered and adjusted for in multivariate analyses; however, there may be residual confounding due to additional factors that were not evaluated or adjusted for in these studies. Vitamin B12 concentrations assessed at mid-gestation may not reflect vitamin B12 status during the relevant etiologic period periconceptionally or for maternal–fetal transfer of cobalamin and subsequent infant status and perinatal outcomes [68]. Additionally, serum folate is a biomarker of short-term dietary intake and does not reflect longer-term or usual intake. Vitamin B12 and folate assessments were also based on a single biomarker (i.e., total serum vitamin B12 and serum folate concentrations). Inclusion of additional circulating (i.e., holo-transcobalamin) and functional (i.e., methylmalonic acid) biomarkers of vitamin B12 metabolism and erythrocyte folate concentrations would improve assessment and interpretation of findings in mother–infant dyads [4]. Additionally, while the low prevalence of vitamin B12 deficiency in this study is similar to previous research in pregnant adolescents in Canada and the United Kingdom, a study population of generally adequate vitamin B12 status limits the generalizability of results to other populations that may be at greater risk for vitamin B12 deficiency, particularly in resource-limited settings [41,43]. Findings should also be interpreted in the context of a folate-replete population (i.e., among participants prescribed high-dose prenatal folic acid (1000 μg) and in a population exposed to folic acid fortification); this also limits the generalizability of findings to other settings. Finally, although findings from this study demonstrated an association of maternal and infant vitamin B12 status at delivery, the interpretation of these findings is not causal. Future prospective studies are needed to examine mechanisms of vitamin B12 transfer to the fetus and to determine the impact of vitamin B12 status on maternal and child health outcomes.
5. Conclusions
In summary, in this cohort of healthy pregnant adolescents, maternal vitamin B12 concentrations significantly decreased during pregnancy and predicted infant vitamin B12 status. This is one of the first prospective studies to date to evaluate the burden of vitamin B12 insufficiency in pregnant adolescents and their infants, a population that is at high risk for both micronutrient deficiencies and pregnancy complications. Findings suggest that vitamin B12 deficiency is an important public health problem in this high-risk obstetric population. Future research is needed to increase vitamin B12 status and improve the health of adolescent mothers and their children.
Acknowledgments
The authors are grateful to the mothers and children, and the midwives of the Strong Midwifery Group, who made this research possible.
Author Contributions
Conceptualization—parent cohort studies, K.O.O., R.G., and E.K.P.; conceptualization—vitamin B12 sub-study, J.L.F. and K.O.O.; analysis, J.L.F. and A.F.; writing—original draft manuscript, J.L.F.; writing—review and editing, J.L.F., K.O.O., H.M.G., and A.F.; supervision, R.G., E.K.P., and K.O.O.; project administration, E.K.P.; laboratory analyses, T.R.K.; funding acquisition, K.O.O. and J.L.F. All authors contributed to the development of this manuscript and read and approved the final version.
Funding
This research was funded by the United States Department of Agriculture (USDA) 2005-35200-15218, USDA 2010-34324-20769, and AFRI/USDA 2011-03424; and the Division of Nutritional Sciences, Cornell University.
Conflicts of Interest
The authors have no conflicts of interest to disclose. The funders had no role in the design of the study, in the collection, analyses, interpretation of data, or in the writing of the manuscript.
References
- 1.Allen L.H. How common is vitamin B-12 deficiency? Am. J. Clin. Nutr. 2009;89:693S–696S. doi: 10.3945/ajcn.2008.26947A. [DOI] [PubMed] [Google Scholar]
- 2.McLean E., de Benoist B., Allen L.H. Review of the magnitude of folate and vitamin B12 deficiencies worldwide. Food Nutr. Bull. 2008;29:S38–S51. doi: 10.1177/15648265080292S107. [DOI] [PubMed] [Google Scholar]
- 3.Allen L.H., Rosenberg I.H., Oakley G.P., Omenn G.S. Considering the case for vitamin B12 fortification of flour. Food Nutr. Bull. 2010;31:S36–S46. doi: 10.1177/15648265100311S104. [DOI] [PubMed] [Google Scholar]
- 4.Finkelstein J.L., Layden A.J., Stover P.J. Vitamin B-12 and Perinatal Health. Adv. Nutr. 2015;6:552–563. doi: 10.3945/an.115.008201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ratan S.K., Rattan K.N., Pandey R.M., Singhal S., Kharab S., Bala M., Singh V., Jhanwar A. Evaluation of the levels of folate, vitamin B12, homocysteine and fluoride in the parents and the affected neonates with neural tube defect and their matched controls. Pediatr. Surg. Int. 2008;24:803–808. doi: 10.1007/s00383-008-2167-z. [DOI] [PubMed] [Google Scholar]
- 6.Adams M.J., Jr., Khoury M.J., Scanlon K.S., Stevenson R.E., Knight G.J., Haddow J.E., Sylvester G.C., Cheek J.E., Henry J.P., Stabler S.P., et al. Elevated midtrimester serum methylmalonic acid levels as a risk factor for neural tube defects. Teratology. 1995;51:311–317. doi: 10.1002/tera.1420510507. [DOI] [PubMed] [Google Scholar]
- 7.Wilson A., Platt R., Wu Q., Leclerc D., Christensen B., Yang H., Gravel R.A., Rozen R. A common variant in methionine synthase reductase combined with low cobalamin (vitamin B12) increases risk for spina bifida. Mol. Genet. Metab. 1999;67:317–323. doi: 10.1006/mgme.1999.2879. [DOI] [PubMed] [Google Scholar]
- 8.Gu Q., Li Y., Cui Z.L., Luo X.P. Homocysteine, folate, vitamin B12 and B6 in mothers of children with neural tube defects in Xinjiang, China. Acta Paediatr. 2012;101:e486–e490. doi: 10.1111/j.1651-2227.2012.02795.x. [DOI] [PubMed] [Google Scholar]
- 9.Ray J.G., Wyatt P.R., Thompson M.D., Vermeulen M.J., Meier C., Wong P.Y., Farrell S.A., Cole D.E. Vitamin B12 and the risk of neural tube defects in a folic-acid-fortified population. Epidemiology. 2007;18:362–366. doi: 10.1097/01.ede.0000257063.77411.e9. [DOI] [PubMed] [Google Scholar]
- 10.Molloy A.M., Kirke P.N., Troendle J.F., Burke H., Sutton M., Brody L.C., Scott J.M., Mills J.L. Maternal vitamin B12 status and risk of neural tube defects in a population with high neural tube defect prevalence and no folic Acid fortification. Pediatrics. 2009;123:917–923. doi: 10.1542/peds.2008-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rowland A.S., Baird D.D., Shore D.L., Weinberg C.R., Savitz D.A., Wilcox A.J. Nitrous oxide and spontaneous abortion in female dental assistants. Am. J. Epidemiol. 1995;141:531–538. doi: 10.1093/oxfordjournals.aje.a117468. [DOI] [PubMed] [Google Scholar]
- 12.Hubner U., Alwan A., Jouma M., Tabbaa M., Schorr H., Herrmann W. Low serum vitamin B12 is associated with recurrent pregnancy loss in Syrian women. Clin. Chem. Lab. Med. 2008;46:1265–1269. doi: 10.1515/CCLM.2008.247. [DOI] [PubMed] [Google Scholar]
- 13.Reznikoff-Etievant M.F., Zittoun J., Vaylet C., Pernet P., Milliez J. Low Vitamin B(12) level as a risk factor for very early recurrent abortion. Eur. J. Obs. Gynecol. Reprod. Biol. 2002;104:156–159. doi: 10.1016/S0301-2115(02)00100-8. [DOI] [PubMed] [Google Scholar]
- 14.Hogeveen M., Blom H.J., den Heijer M. Maternal homocysteine and small-for-gestational-age offspring: Systematic review and meta-analysis. Am. J. Clin. Nutr. 2012;95:130–136. doi: 10.3945/ajcn.111.016212. [DOI] [PubMed] [Google Scholar]
- 15.Muthayya S., Kurpad A.V., Duggan C.P., Bosch R.J., Dwarkanath P., Mhaskar A., Mhaskar R., Thomas A., Vaz M., Bhat S., et al. Low maternal vitamin B12 status is associated with intrauterine growth retardation in urban South Indians. Eur. J. Clin. Nutr. 2006;60:791–801. doi: 10.1038/sj.ejcn.1602383. [DOI] [PubMed] [Google Scholar]
- 16.Black M.M. Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr. Bull. 2008;29:S126–S131. doi: 10.1177/15648265080292S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pepper M.R., Black M.M. B12 in fetal development. Semin. Cell Dev. Biol. 2011;22:619–623. doi: 10.1016/j.semcdb.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Obeid R., Morkbak A.L., Munz W., Nexo E., Herrmann W. The cobalamin-binding proteins transcobalamin and haptocorrin in maternal and cord blood sera at birth. Clin. Chem. 2006;52:263–269. doi: 10.1373/clinchem.2005.057810. [DOI] [PubMed] [Google Scholar]
- 19.Muthayya S., Dwarkanath P., Mhaskar M., Mhaskar R., Thomas A., Duggan C., Fawzi W.W., Bhat S., Vaz M., Kurpad A. The relationship of neonatal serum vitamin B12 status with birth weight. Asia Pac. J. Clin. Nutr. 2006;15:538–543. [PubMed] [Google Scholar]
- 20.Balci Y.I., Ergin A., Karabulut A., Polat A., Dogan M., Kucuktasci K. Serum vitamin B12 and folate concentrations and the effect of the Mediterranean diet on vulnerable populations. Pediatr. Hematol. Oncol. 2014;31:62–67. doi: 10.3109/08880018.2013.829894. [DOI] [PubMed] [Google Scholar]
- 21.Adaikalakoteswari A., Vatish M., Lawson A., Wood C., Sivakumar K., McTernan P.G., Webster C., Anderson N., Yajnik C.S., Tripathi G., et al. Low maternal vitamin B12 status is associated with lower cord blood HDL cholesterol in white Caucasians living in the UK. Nutrients. 2015;7:2401–2414. doi: 10.3390/nu7042401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radunovic N., Lockwood C.J., Stanojlovic O., Steric M., Kontic-Vucinic O., Sulovic N., Hrncic D., Ackerman Iv W.E. Fetal and maternal plasma homocysteine levels during the second half of uncomplicated pregnancy. J. Matern.-Fetal Neonatal Med. 2014 doi: 10.3109/14767058.2014.951626. [DOI] [PubMed] [Google Scholar]
- 23.Bergen N.E., Schalekamp-Timmermans S., Jaddoe V.W., Hofman A., Lindemans J., Russcher H., Tiemeier H., Steegers-Theunissen R.P., Steegers E.A. Maternal and neonatal markers of the homocysteine pathway and fetal growth: The Generation R Study. Paediatr. Perinat. Epidemiol. 2016;30:386–396. doi: 10.1111/ppe.12297. [DOI] [PubMed] [Google Scholar]
- 24.Kalay Z., Islek A., Parlak M., Kirecci A., Guney O., Koklu E., Kalay S. Reliable and powerful laboratory markers of cobalamin deficiency in the newborn: Plasma and urinary methylmalonic acid. J. Matern.-Fetal Neonatal Med. 2016;29:60–63. doi: 10.3109/14767058.2014.986649. [DOI] [PubMed] [Google Scholar]
- 25.Hay G., Clausen T., Whitelaw A., Trygg K., Johnston C., Henriksen T., Refsum H. Maternal folate and cobalamin status predicts vitamin status in newborns and 6-month-old infants. J. Nutr. 2010;140:557–564. doi: 10.3945/jn.109.117424. [DOI] [PubMed] [Google Scholar]
- 26.Murphy M.M., Molloy A.M., Ueland P.M., Fernandez-Ballart J.D., Schneede J., Arija V., Scott J.M. Longitudinal study of the effect of pregnancy on maternal and fetal cobalamin status in healthy women and their offspring. J. Nutr. 2007;137:1863–1867. doi: 10.1093/jn/137.8.1863. [DOI] [PubMed] [Google Scholar]
- 27.Deegan K.L., Jones K.M., Zuleta C., Ramirez-Zea M., Lildballe D.L., Nexo E., Allen L.H. Breast milk vitamin B-12 concentrations in Guatemalan women are correlated with maternal but not infant vitamin B-12 status at 12 months postpartum. J. Nutr. 2012;142:112–116. doi: 10.3945/jn.111.143917. [DOI] [PubMed] [Google Scholar]
- 28.Finkelstein J.L., Kurpad A.V., Thomas T., Srinivasan K., Duggan C. Vitamin B12 status in pregnant women and their infants in South India. Eur. J. Clin. Nutr. 2017;71:1046–1053. doi: 10.1038/ejcn.2017.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Varsi K., Ueland P.M., Torsvik I.K., Bjorke-Monsen A.L. Maternal serum cobalamin at 18 weeks of pregnancy predicts infant cobalamin status at 6 months—A prospective, observational study. J. Nutr. 2018;148:738–745. doi: 10.1093/jn/nxy028. [DOI] [PubMed] [Google Scholar]
- 30.Lindblad B., Zaman S., Malik A., Martin H., Ekstrom A., Amu S., Holmgren A., Norman M. Folate, vitamin B12, and homocysteine levels in South Asian women with growth-retarded fetuses. Acta Obstet. Gynecol. Scand. 2005;84:1055–1061. doi: 10.1111/j.0001-6349.2005.00876.x. [DOI] [PubMed] [Google Scholar]
- 31.Bjorke Monsen A.L., Ueland P.M., Vollset S.E., Guttormsen A.B., Markestad T., Solheim E., Refsum H. Determinants of cobalamin status in newborns. Pediatrics. 2001;108:624–630. doi: 10.1542/peds.108.3.624. [DOI] [PubMed] [Google Scholar]
- 32.Guerra-Shinohara E.M., Paiva A.A., Rondo P.H., Yamasaki K., Terzi C.A., D’Almeida V. Relationship between total homocysteine and folate levels in pregnant women and their newborn babies according to maternal serum levels of vitamin B12. BJOG. 2002;109:784–791. doi: 10.1111/j.1471-0528.2002.01307.x. [DOI] [PubMed] [Google Scholar]
- 33.Koc A., Kocyigit A., Soran M., Demir N., Sevinc E., Erel O., Mil Z. High frequency of maternal vitamin B12 deficiency as an important cause of infantile vitamin B12 deficiency in Sanliurfa province of Turkey. Eur. J. Nutr. 2006;45:291–297. doi: 10.1007/s00394-006-0598-7. [DOI] [PubMed] [Google Scholar]
- 34.Jacquemyn Y., Ajaji M., Karepouan N., Jacquemyn N., Van Sande H. Vitamin B12 and folic acid status of term pregnant women and newborns in the Antwerp region, Belgium. Clin. Exp. Obstet. Gynecol. 2014;41:141–143. [PubMed] [Google Scholar]
- 35.Mittal M., Bansal V., Jain R., Dabla P.K. Perturbing Status of Vitamin B12 in Indian Infants and Their Mothers. Food Nutr. Bull. 2017;38:209–215. doi: 10.1177/0379572117697535. [DOI] [PubMed] [Google Scholar]
- 36.Dilli D., Dogan N.N., Orun U.A., Koc M., Zenciroglu A., Karademir S., Akduman H. Maternal and neonatal micronutrient levels in newborns with CHD. Cardiol. Young. 2018;28:523–529. doi: 10.1017/S1047951117002372. [DOI] [PubMed] [Google Scholar]
- 37.Chebaya P., Karakochuk C.D., March K.M., Chen N.N., Stamm R.A., Kroeun H., Sophonneary P., Borath M., Shahab-Ferdows S., Hampel D., et al. Correlations between maternal, breast milk, and infant vitamin b12 concentrations among mother-infant dyads in Vancouver, Canada and Prey Veng, Cambodia: An exploratory analysis. Nutrients. 2017;9:270. doi: 10.3390/nu9030270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coban S., Yilmaz Keskin E., Igde M. Association between maternal and infantile markers of cobalamin status during the first month post-delivery. Indian J. Pediatr. 2018;85:517–522. doi: 10.1007/s12098-017-2598-4. [DOI] [PubMed] [Google Scholar]
- 39.Williams A.M., Stewart C.P., Shahab-Ferdows S., Hampel D., Kiprotich M., Achando B., Lin A., Null C.A., Allen L.H., Chantry C.J. Infant serum and maternal milk vitamin b-12 are positively correlated in Kenyan infant-mother dyads at 1–6 months postpartum, irrespective of infant feeding practice. J. Nutr. 2018;148:86–93. doi: 10.1093/jn/nxx009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bellows A.L., Smith E.R., Muhihi A., Briegleb C., Noor R.A., Mshamu S., Sudfeld C., Masanja H., Fawzi W.W. Micronutrient deficiencies among breastfeeding infants in Tanzania. Nutrients. 2017;9:1258. doi: 10.3390/nu9111258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baker P.N., Wheeler S.J., Sanders T.A., Thomas J.E., Hutchinson C.J., Clarke K., Berry J.L., Jones R.L., Seed P.T., Poston L. A prospective study of micronutrient status in adolescent pregnancy. Am. J. Clin. Nutr. 2009;89:1114–1124. doi: 10.3945/ajcn.2008.27097. [DOI] [PubMed] [Google Scholar]
- 42.Baron M.A., Solano L., Pena E., Moron A. (Nutritional status of folate, vitamin B12 and iron in pregnant adolescents) Arch. Latinoam. Nutr. 2003;53:150–156. [PubMed] [Google Scholar]
- 43.Gadowsky S., Gale K., Wolfe S.A., Jory J., Gibson R., O’Connor D. Biochemical folate, B12, and iron status of a group of pregnant adolescents accessed through the public health system in southern Ontario. J. Adolsc. Health. 1995;16:465–474. doi: 10.1016/1054-139X(94)00001-U. [DOI] [PubMed] [Google Scholar]
- 44.Davis L.M., Chang S.C., Mancini J., Nathanson M.S., Witter F.R., O’Brien K.O. Vitamin D insufficiency is prevalent among pregnant African American adolescents. J. Pediatr. Adolesc. Gynecol. 2010;23:45–52. doi: 10.1016/j.jpag.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 45.Moran V. A systematic review of dietary assessments of pregnant adolescents in industrialised countries. Br. J. Nutr. 2007;97:411–425. doi: 10.1017/S0007114507381373. [DOI] [PubMed] [Google Scholar]
- 46.Klein J.D. American Academy of Pediatrics Committee on, A. Adolescent pregnancy: Current trends and issues. Pediatrics. 2005;116:281–286. doi: 10.1542/peds.2005-0999. [DOI] [PubMed] [Google Scholar]
- 47.Sedgh G., Finer L.B., Bankole A., Eilers M.A., Singh S. Adolescent Pregnancy, Birth, and abortion rates across countries: Levels and recent trends. J. Adolesc. Health. 2015;56:223–230. doi: 10.1016/j.jadohealth.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee S., Guillet R., Cooper E.M., Westerman M., Orlando M., Kent T., Pressman E., O’Brien K.O. Prevalence of anemia and associations between neonatal iron status, hepcidin, and maternal iron status among neonates born to pregnant adolescents. Pediatr. Res. 2016;79:42–48. doi: 10.1038/pr.2015.183. [DOI] [PubMed] [Google Scholar]
- 49.Lee S., Guillet R., Cooper E.M., Westerman M., Orlando M., Pressman E., O’Brien K.O. Maternal inflammation at delivery affects assessment of maternal iron status. J. Nutr. 2014;144:1524–1532. doi: 10.3945/jn.114.191445. [DOI] [PubMed] [Google Scholar]
- 50.Layden A.J., O’Brien K.O., Pressman E.K., Cooper E.M., Kent T.R., Finkelstein J.L. Vitamin B12 and placental expression of transcobalamin in pregnant adolescents. Placenta. 2016;45:1–7. doi: 10.1016/j.placenta.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 51.Yetley E.A., Pfeiffer C.M., Phinney K.W., Bailey R.L., Blackmore S., Bock J.L., Brody L.C., Carmel R., Curtin L.R., Durazo-Arvizu R.A., et al. Biomarkers of vitamin B-12 status in NHANES: A roundtable summary. Am. J. Clin. Nutr. 2011;94:313S–321S. doi: 10.3945/ajcn.111.013243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sullivan K.M., Mei Z., Grummer-Strawn L., Parvanta I. Haemoglobin adjustments to define anaemia. Trop. Med. Int. Health. 2008;13:1267–1271. doi: 10.1111/j.1365-3156.2008.02143.x. [DOI] [PubMed] [Google Scholar]
- 53.WHO . Physical Status: The Use and Interpretation of Anthropometry. World Health Organization; Geneva, Switzerland: 1995. p. 329. Report of a WHO Expert Committee. [Google Scholar]
- 54.Spiegelman D., Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am. J. Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 55.Wacholder S. Binomial regression in GLIM: Estimating risk ratios and risk differences. Am. J. Epidemiol. 1986;123:174–184. doi: 10.1093/oxfordjournals.aje.a114212. [DOI] [PubMed] [Google Scholar]
- 56.Zou G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 57.Durrleman S., Simon R. Flexible regression models with cubic splines. Stat. Med. 1989;8:551–561. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 58.Govindarajulu U.S., Spiegelman D., Thurston S.W., Ganguli B., Eisen E.A. Comparing smoothing techniques in Cox models for exposure-response relationships. Stat. Med. 2007;26:3735–3752. doi: 10.1002/sim.2848. [DOI] [PubMed] [Google Scholar]
- 59.Greenland S. Modeling and variable selection in epidemiologic analysis. Am. J. Public Health. 1989;79:340–349. doi: 10.2105/AJPH.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miettinen O. Theoretical Epidemiology. Volume 107 John Wiley & Sons; New York, NY, USA: 1985. [Google Scholar]
- 61.Garcia-Casal M.N., Osorio C., Landaeta M., Leets I., Matus P., Fazzino F., Marcos E. High prevalence of folic acid and vitamin B12 deficiencies in infants, children, adolescents and pregnant women in Venezuela. Eur. J. Clin. Nutr. 2005;59:1064–1070. doi: 10.1038/sj.ejcn.1602212. [DOI] [PubMed] [Google Scholar]
- 62.Green R., Allen L.H., Bjorke-Monsen A.L., Brito A., Gueant J.L., Miller J.W., Molloy A.M., Nexo E., Stabler S., Toh B.H., et al. Vitamin B12 deficiency. Nat. Rev. Dis. Prim. 2017;3:17040. doi: 10.1038/nrdp.2017.40. [DOI] [PubMed] [Google Scholar]
- 63.Tucker K.L., Rich S., Rosenberg I., Jacques P., Dallal G., Wilson P.W., Selhub J. Plasma vitamin B-12 concentrations relate to intake source in the Framingham Offspring study. Am. J. Clin. Nutr. 2000;71:514–522. doi: 10.1093/ajcn/71.2.514. [DOI] [PubMed] [Google Scholar]
- 64.Visentin C.E., Masih S.P., Plumptre L., Schroder T.H., Sohn K.J., Ly A., Lausman A.Y., Berger H., Croxford R., Lamers Y., et al. Low serum vitamin b-12 concentrations are prevalent in a cohort of pregnant Canadian women. J. Nutr. 2016;146:1035–1042. doi: 10.3945/jn.115.226845. [DOI] [PubMed] [Google Scholar]
- 65.Wadhwani N.S., Pisal H.R., Mehendale S.S., Joshi S.R. A prospective study of maternal fatty acids, micronutrients and homocysteine and their association with birth outcome. Matern. Child Nutr. 2015;11:559–573. doi: 10.1111/mcn.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sukumar N., Rafnsson S.B., Kandala N.B., Bhopal R., Yajnik C.S., Saravanan P. Prevalence of vitamin B-12 insufficiency during pregnancy and its effect on offspring birth weight: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2016;103:1232–1251. doi: 10.3945/ajcn.115.123083. [DOI] [PubMed] [Google Scholar]
- 67.Rush E.C., Katre P., Yajnik C.S. Vitamin B12: One carbon metabolism, fetal growth and programming for chronic disease. Eur. J. Clin. Nutr. 2013;68:2–7. doi: 10.1038/ejcn.2013.232. [DOI] [PubMed] [Google Scholar]
- 68.De-Regil L.M., Harding K.B., Roche M.L. Preconceptional nutrition interventions for adolescent girls and adult women: Global guidelines and gaps in evidence and policy with emphasis on micronutrients. J. Nutr. 2016;146:1461S–1470S. doi: 10.3945/jn.115.223487. [DOI] [PubMed] [Google Scholar]