Abstract
Background: The teaching of endoscopic endonasal surgery has always been difficult because of the complex structure of the nasal cavity, and the unique endoscopic view angle and endoscopic surgical tools. In this study, we have designed a 3D printed multi-color model for training of endoscopic endonasal surgery, and obtained preliminary application results. Methods: The 3D printed model contained facial skin, bony skeleton, internal carotid artery, turbinate, optic chiasm, and a special sellar base with appropriate colors. After it was printed, six otolaryngologists and neurosurgeons assessed the model. Twenty graduate students and residents from otolaryngology or neurosurgery, without prior experience in endoscopic endonasal surgery were recruited and consented for the training. The training results were recorded. The subjective feeling of participants in terms of using 3D printed model in surgical training was investigated after training. Results: All experts strongly agreed or agreed that the 3D printed model has realistic anatomical structure of nasal passage and appropriate colors for different parts, and is a good teaching tool. As the trainees practiced more, the rate and quality of endoscopic operation increased gradually. Compared to the first practice, all recorded training parameters were improved significantly (all P < 0.05). All participants strongly agreed or agreed that they benefited from the training and the 3D printed model can inspire interest and enthusiasm of endoscopic endonasal surgical training. Conclusion: This 3D printed model has realistic anatomical structure of nasal passage and appropriate colors for different parts, and could be a good teaching tool of endoscopic endonasal surgery.
Keywords: 3D printed model, endoscopic endonasal surgery, surgical training, subjective feeling
Introduction
Since the development of endoscopic endonasal surgery, it has gradually expanded from a simple sinus surgery to treating various intracranial and sinus lesions [1-3]. It makes full use of the natural passage of the nasal cavity, provides good field of view, and achieves good results. Therefore, neurosurgeons pay more and more attention to it and try to perform endoscopic endonasal surgery. However, the nasal cavity has a complex structure, the unique endoscopic view angle, and surgical tools used are quite different from those of conventional surgery. For neurosurgeons who want to practice endoscopic endonasal surgery, necessary training is essential.
However, training with real surgery or cadaveric head is limited by short of resource and ethical issues [4]. If a good training model can be provided to young surgeons, it could be very helpful for learning and improving endoscopic endonasal surgical skills. In recent years, 3D printing technology has been widely used in medical education and surgical training because it can precisely replicate complex anatomical structures [5-7]. Different types of 3D training models for otolaryngology and neurosurgery have been invented to allow additional surgical training [8-11]. However, there have been only few simulators for endoscopic endonasal surgical training, with disadvantages. For example, some models lack the distinction of different anatomic structures with multiple colors; some research focused just on improving the techniques of drilling [12], and some lacked obvious validation of training effect and subjective feeling of participants [13,14]. In this study, we have designed a 3D printed multi-color model for training of endoscopic endonasal surgery, and obtained preliminary application results, hoping to inspire the design and application of more endoscopic endonasal surgery training models.
Materials and methods
Generation of the 3D printed model
The generation process can be subdivided to image acquisition, model design, and printing of the 3D model. Ethical approval was obtained from the Institutional Review Board of the School of Basic Medical Sciences, Fujian Medical University. All methods were performed in accordance with the approved guidelines. Informed consent form was obtained from the patients or their relatives.
Image acquisition
Magnetic resonance imaging (MRI) (Magnetom Verio Tim, Siemens, Erlangen, Germany) and computed tomography (CT) scan (Acquilion ONE, Toshiba Medical Systems, Nasu, Japan) data of three healthy volunteers were obtained and reviewed. MRI and CT scans were performed in the horizontal plane using a slice thickness of ≤ 1.0 mm. These data were examined by two experienced radiologists to confirm there was no brain disease. Slices that included all regions of the brain that are most appropriate for training purposes were selected. The coronal, sagittal, and axial views of selected data were exported to a digital imaging and communications in medicine (DICOM) file, respectively.
Modeling
The purpose of the 3D printed model developed in this study is to enable the trainees to familiarize themselves with the endonasal field of view and the use of endoscopic endonasal instruments with both hands, and be able to finish basic endoscopic endonasal operations such as drilling, curetting and biting, and aspiration.
Therefore, the 3D printed model was designed following the un-diseased human anatomy data. The process of segmenting the CT and MRI scan data into the regions to be 3D printed was performed using the PolyJet StudioTM software (Stratasys Shanghai Ltd., Shanghai, China) and the segmented image was saved as a **. STL file.
3D model printing
The STL files were imported into Stratasys J750 3D printer (Stratasys Shanghai Ltd., Shanghai, China) for model printing. Material selection is a critical part for making a realistic model. Different colors were used to distinguish anatomic structures with different physical properties. The 3D printed model contained facial skin, bony skeleton, internal carotid artery, turbinate, optic chiasm, and a special sellar base for holding an egg (for training purpose). It has a 1:1 ratio with human anatomy, and the nasal passage was similar to that of health human. The special sellar base is a ring, which can hold and secure one egg. Since the egg has shell, shell membrane, egg white, and yolk, it is a good tool for representing sellar base, dura mater, and lesions at the sellar base [9,10]. The trainees can practice drilling, curetting and biting, and aspiration skills with the egg. Furthermore, the egg can be replaced at anytime, so the same model can be used over and over again (Figure 1).
Figure 1.
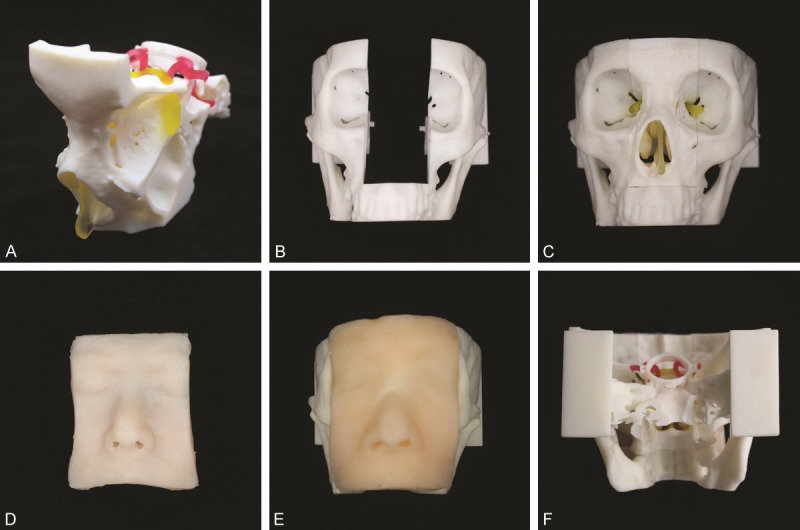
The 3D printed multi-color model for endoscopic endonasal surgical training. (A-D) Different parts of the printed model, including the replaceable nasal and sphenoidal structure (A), the special bony structure (B), and facial skin (D). The replaceable nasal and sphenoidal structure was snap fitted into the center of the bony structure, the septal, inferior turbinate, middle turbinate and optic nerve can be seen (C); The frontal view of the whole model, endoscope can be placed through the nasal passage (E); The posterior view of the whole model, the inferior carotid artery and the special sellar base can be seen (F).
Assessment by experts
After printing of the 3D model, six otolaryngologists and neurosurgeons who had experience as endoscopic attending surgeon were recruited to assess the model, which was to practice endoscopic endonasal operation on the egg secured on the holder of the 3D printed model. After the practice operation, all experts completed a 4-question feedback questionnaire: 1. Replication: the 3D printed model had realistic anatomical condition, and the operational endonasal space of the model was similar to that of the actual operation; 2. Color: the different parts of 3D printed model were colored appropriately; 3. Practicability: It is possible to perform basic endoscopic endonasal operations including drilling, curetting and biting, and aspiration with this model; 4. Quality: The model had high quality, and was satisfactory. All questions were answered on a 5-point scale (1 = strongly disagree; 2 = disagree; 3 = neutral; 4 = agree; and 5 = strongly agree).
Participants
20 graduate students or residents from the departments of otolarynogology or neurosurergy of the Affiliated Xiehe Hospital or The First Affiliated Hospital of Fujian Medical School, without prior endoscopic endonasal experience, participated in the training with 3D model. All trainees finished theoretical study, had observed endoscopic endonasal surgeries, and knew how to operate surgical tools such as the high speed drill, micro dissector, mucosa cutting forceps, and aspirator.
Endoscopic endonasal surgical training
Instruments and equipment
STORZ endoscopic system was used with HOPKINS II in-viewing endoscope and neurosurgical power tool. Endoscopic endonasal operation tools included: high speed drill, scissors, nerve dissector, scalpel, mucosa cutting forceps, rongeur, grasping forceps, curette, and aspirator.
Training procedure and requirements
For training, an egg was secured at the special sellar base of the model. The endonasal endoscope and surgical tools were placed through the two nostrils, respectively (Figure 2A). Drilling, curetting and biting, and aspiration were performed in sequence with endoscopic surgical instruments (Figure 2B-D): (1) Drilling: The abrasive drill was used to mill off the shell for an area measured to be at least 1.5 cm × 1.5 cm. The milling should be as fast as possible but without breaking the shell membrane. (2) Curetting and biting: Micro dissector and grasping forceps were used to remove free and small pieces of broken shells to enlarge shell opening within the reach of the tools. This operation was timed to be finished within 3 minutes, without breaking the shell membrane; (3) Aspiration: Mucosa cutting forceps or scalpel were used to open the shell membrane, and the aspirator was used to aspirate off egg white while leaving the yolk intact without breaking the vitelline membrane. The egg was replaced after all of the steps were finished and every trainee practiced the procedure for five times. Cutting and bipolar coagulation were not performed as they could damage the 3D printed model.
Figure 2.
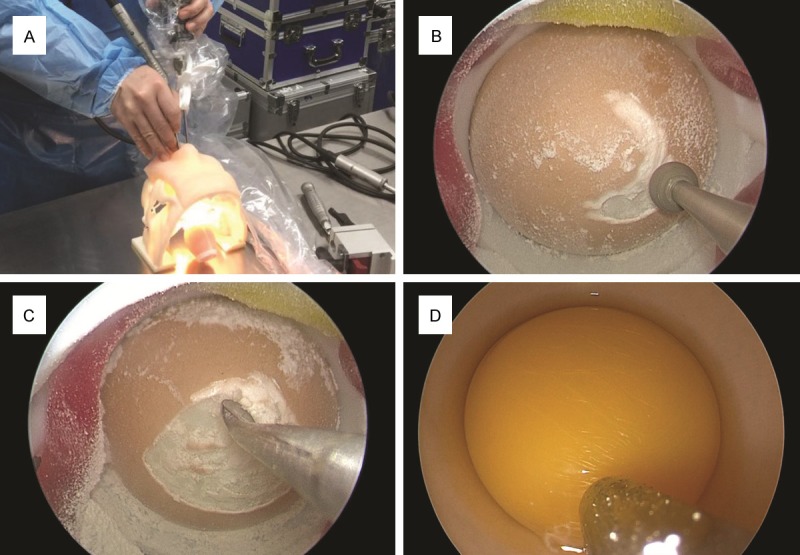
Endoscopic endonasal surgical training with 3D printed model. (A) An egg was secured at the special sellar base. The endoscope and endoscopic tools were passed through the nostrils, respectively. (B-D) The tools were used to finish drilling of the shell (B), curetting and biting of the shell to further enlarge area of shell removal (C), and aspirating off egg white (D).
Validation of the training model
Training results of participants
The following parameters were recorded: (1) Time needed to mill out the shell (started when the endoscope was placed into the nostril); (2) If the shell membrane broke during milling; (3) If the shell membrane broke when removing free and small pieces of shell; (4) If the vitelline broke during aspiration of egg white. The total score was calculated by addition scores of individual steps. For the milling step, removing time > 4 minutes was scored 1, between 3 and 4 minutes was scored 2, and < 3 minutes was scored 3; For steps (2)-(4), if the membrane (shell/vitelline) was intact, it was scored 1, otherwise 0. The range of the final score was between 1 and 6.
Post-training subjective feeling
After the last practice, all participants were asked to complete a feedback questionnaire included five questions to assess their subjective feeling of using the 3D printed model in training. The first four questions were answered based on a 5-point scale (1 = strongly disagree; 2 = disagree; 3 = neutral; 4 = agree; and 5 = strongly agree): 1. do you agree that you can be benefitted from the training; 2. do you agree that the 3D printed model can inspire interest and enthusiasm of endoscopic endonasal surgical training; 3. do you agree that this training enables you to practice basic endoscopic skills; 4. do you agree that with this training, you can practice endoscopic endonasal surgery. And the last question was “In your mind, the limitation(s) of the 3D printed model is/are that____.” (Table 1). For the first four questions, the responses of “agree” and “strongly agree” were designated as positive answers.
Table 1.
The feedback questionnaire used to assess participants’ subjective feeling of using the 3D printed model in training
| No. | Question | Response* | |
|---|---|---|---|
| Subjective feeling | 1 | Do you agree you can be benefitted from the training? | |
| 2 | Do you agree that the 3D printed model can inspire interest and enthusiasm of endoscopic endonasal surgical training? | ||
| 3 | Do you agree that this training enables you to practice basic endoscopic skills? | ||
| 4 | Do you agree that with this training, you can practice endoscopic endonasal surgery? | ||
| Suggestions | 5 | In your mind, the limitation(s) of the 3D printed model is/are that ____. |
Questions 1-4 were replied on a scale of 1 to 5: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree.
Statistical analysis
Continuous data were shown as mean ± standard deviation (SD) or median (interquartile range, [IQR]) and categorical variables as number (%). Training results were analyzed using one-way analysis of variance (ANOVA) after testing for homogeneity. Tukey’s test was performed for pairwise comparison if ANOVA indicated a significant difference. For categorical data, potential differences were evaluated using Kruskal-Wallis H test followed by Mann-Whitney U test for multiple post-hoc comparisons or chi-square tests. Statistical analysis was performed using an IBM SPSS statistical package (version 19.0, IBM Corp, Armonk, NY). A P-value of < 0.05 was considered statistically significant.
Results
Experts’ evaluation of the 3D printed model
The models used in endoscopic endonasal surgical training were successfully 3D printed (Figure 1). All experts strongly agreed or agreed that the 3D printed model has realistic anatomical structure of nasal passage and appropriate colors for different parts and it enabled practice of basic endoscopic endonasal skills, including drilling, curetting and biting, and aspiration (Figure 3).
Figure 3.
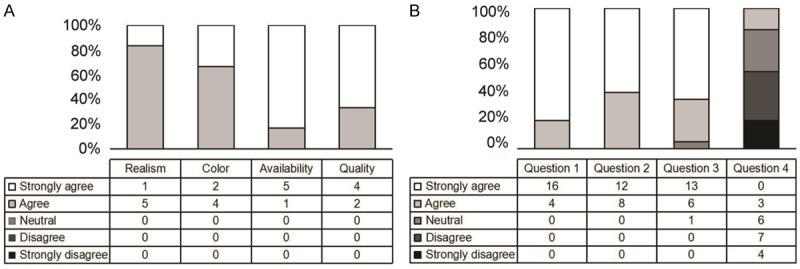
Results of the subjective assessment by experts and participants. A. Detailed breakdown of the experts’ responses; B: Detailed breakdown of the trainees’ answers to the questionnaire.
Participant demographics
The 20 trainees included 13 graduate students (65%, 13/20) and 7 residents (35%, 7/20), with 20% (4/20) of them being female.
Training results and post-training subjective feeling of participants
Training results
In the five practices, from the first time to the last time, the average time for the trainees to complete the task of milling out the eggshell was 4.10±0.80 min, 3.98±0.56 min, 3.57±0.42 min, 3.20±0.39 min, and 3.00±0.46 min, respectively; the probability of breaking the shell membrane when drilling and milling the shell was 95.0% (19/20), 70.0% (14/20), 55.0% (11/20), 55.0% (10/20) and 30.0% (6/20), respectively; the probability of breaking the membrane when curetting and biting was 100.0% (20/20), 80% (16/20), 65% (13/20), 40% (8/20) and 45.0% (9/20), respectively; the probability of breaking the vitelline membrane when aspirating off the egg white was 60% (12/20), 55% (11/20), 35% (7/20), 20% (4/20) and 15% (3/20), respectively; the total score was 2.00±0.73, 2.55±1.00, 3.35±0.93, 4.05±0.89 and 4.65±0.88. It can be seen that as the practice time increased, the speed and quality of operation under the endoscope improved gradually (Figure 4).
Figure 4.
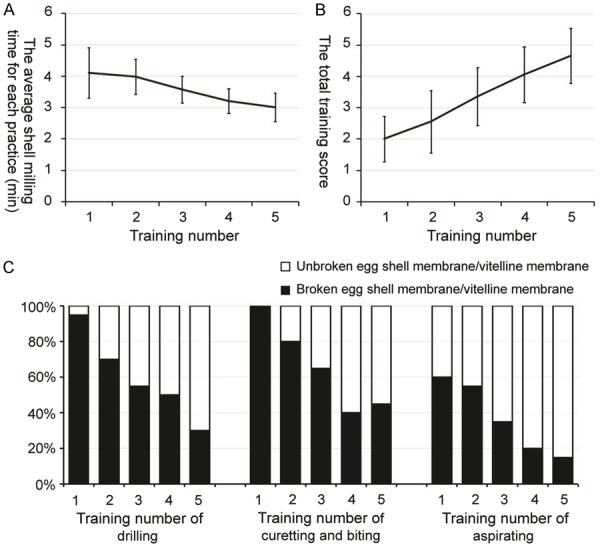
The training results of participants. A. The average shell milling time for each practice; B. The total training score; C. Percent of trainee who broke the membrane/vitelline membrane during drilling, curetting and biting, or aspiration.
Comparison of the results between the first and the last practices
Compared to the first practice, all training parameters improved significantly at the last practice (Table 2).
Table 2.
Comparisons of the results between the first and the last practices
| The first training (n = 20) | The last training (n = 20) | t/χ2 | P value | |
|---|---|---|---|---|
| Time for shell milling (min) | 4.10±0.80 | 3.00±0.46 | -10.426 | < 0.001 |
| Times shell membrane broke when milling the shell | 19 (95%) | 6 (30%) | 18.027 | < 0.001 |
| Times membrane broke when removing shell pieces | 20 (100%) | 9 (45%) | 15.172 | < 0.001 |
| Times vitelline membrane broke when removing egg white | 12 (60%) | 3 (15%) | 8.640 | 0.003 |
| Total score | 2.00±0.73 | 4.65±0.88 | 5.329 | < 0.001 |
*Compared with Fisher’s exact test.
Comparison of the training results between the graduate students and the young residents
At the first practice, the time for young resident to mill out the egg shell was significantly less than that of graduate students (3.55±0.41 min vs. 4.39±0.82 min, t = 2.551, P = 0.020), and the total score was obviously higher than that of graduate students (2.57±0.79 vs. 1.69±0.48, t = -3.125, P = 0.006). However, by the last practice, every training parameter, when compared between the young residents and graduate students, were not statistically different.
Post-training subjective feeling
All participants completed the feedback questionnaire (Table 1). Positive responses (“agree” or “strongly agree” based on a 5-point scale) were found ≥ 95% answers for the first three questions, and were found in only 15% answers for the fourth question (Figure 3). For the fifth question, the most common limitations were: 1. The model cannot reflect complex abnormal or diseased anatomic structure (55%, 9/20); 2. Bipolar coagulation and resection cannot be practiced with this model.
Discussion
With the development of endonasal endoscopic techniques, endoscopic endonasal surgery has gradually being used in otolaryngology and neurosurgery with high safety and efficiency [15-18]. More and more neurosurgeons are becoming aware and trying to perform endoscopic endonasal surgery. Training under endoscope is an essential step for a surgeon to become ready for endoscopic endonasal surgery. However, practice with actual surgery or cadaveric head was faced with difficulties such as limited source and ethics issues [4]. The cadaveric structure is the best source but not suitable for trainees without basic training in endoscopic endonasal operation. On one hand, the availability of cadaveric head is very limited, and not all trainees can be trained; on the other hand, trainees without basic training would focus more on how to use endoscopic surgical tools and neglect the anatomic features of the specimen. When they became familiar with the tools, the anatomic features are often damaged and cannot be recognized, which is a waste of the cadaveric specimen. Therefore, in this study, we have designed and developed a 3D printed multi-color model and evaluated its efficiency in the training of endoscopic endonasal skills. In recent years, because it can precisely replicate complex anatomical structures, 3D printing technology has been widely used in medical education and surgical training [5-7]. 3D printed model can be used throughout the whole clinical process, from patient education [19-21] to quantitative and qualitative assessments of disease [22], preoperative planning [23], and intraoperative guidance [24], leading to individualized, precise, minimal invasive, and highly effective treatments. A lot of research has shown that 3D printed model can be an excellent substitute of cadaver in surgical training [8-11]. The teaching of endoscopic endonasal surgery has always been difficult in otolaryngology and neurosurgery because of the complex structure of the nasal cavity, the unique view angle, and the differences in operation instruments compared to conventional surgery [25]. 3D printing could make 1:1 surgical training model, which is helpful for teaching. 3D printed model can solve the problems of limited source and ethics issues of training with cadaveric head or during surgery, and provides unlimited chances for trainees to practice basic endoscopic endonasal skills, which lays a solid foundation for dissection and actual surgical operation.
The 3D printed model contained facial skin, skeleton, internal carotid artery, turbinate, optic chiasm, and a special sellar base for holding an egg (for training purpose). The facial skin, turbinate, internal carotid artery and optic chiasm were made with soft material, the bony skeleton was made with hard material, and different structures were distinguished with different colors. The nasal passage of the model was the same as that of normal human. Six otolaryngologists and neurosurgeons who had experience as an endoscopic attending surgeon carefully assessed the model, and all strongly agreed or agreed that the 3D printed model is practical, has realistic anatomical condition of nasal passage and appropriate colors for different parts.
The operational nasal space of this model is the same as what is found during actual surgery. A special sellar base was designed so the trainees can practice endonasal endoscopic skills with different surgical tools. The special sellar base is a ring, which can hold and secure one egg. Since the egg has shell, shell membrane, egg white, and yolk, it is appropriate to use it to represent sellar base, dura mater and lesions at the sellar base, so the trainees can practice drilling, curetting, biting and aspiration [9,10]. The model can be reused by simply replace the used egg. Since the nasal and sphenoidal parts are replaceable, even the special sellar base, turbinate or septal was accidentally broke, only the corresponding part needs to be changed, further reduces cost.
In this study, 3D printed model was designed and used for endoscopic endonasal surgical training. 20 graduate students and young residents without prior endoscopic endonasal experience were enrolled in this training and practiced with the model for 5 times. Results showed that the speed and quality of endoscopic endonasal operation of the trainees improved gradually. Compared to the first practice, by the last practice, the shell mill out time, probabilities of breaking shell membrane when milling or removing the shell, the probability of breaking the vitelline when aspirating off the egg white, as well as the total score of the practice all improved significantly. Practice with 3D printed model can significantly improve the endoscopic endonasal surgical skills such as milling, curetting and biting, and aspiration for trainees without any endoscopic endonasal surgical experience.
The findings of participants’ post-training subjective feeling showed that all participants strongly agreed or agreed that they can be benefitted from the endoscopic endonasal training and the 3D printed model can inspire interest and enthusiasm of endoscopic endonasal surgical training. 95% of participants strongly agreed or agreed that with this training, they became familiar with the basic endoscopic endonasal skills. However, most trainees also mentioned that surgical training with 3D printed model cannot completely replace training with cadaveric head or assisting in the actual endoscopic endonasal surgery, only 15% of participants agreed (no one strongly agreed) that training with 3D printed model can ensure participants to master endoscopic endonasal surgery. The most common limitations, as mentioned by the trainees, were 1. The model cannot reflect complex abnormal or diseased anatomic structure (55%, 9/20); 2. Bipolar coagulation and resection cannot be practiced with this model.
Combining the training results and the participants’ subjective feeling, 3D printed model is a good tool for endoscopic endonasal training, especially for young surgeons without prior experience. This 3D printed model can help trainees to familiarize themselves with the field of view of the endoscope, operation with both hands, as well as basic endoscopic practices. However, it should be clearly stated that surgical training with just 3D printed model is not enough for participants to master endoscopic endonasal surgery. This 3D printed model is designed to represent healthy condition for the purpose of practicality and repeatability. However, it still lacks the capability to represent the real surgical condition, as it is not able to reflect complex anatomic abnormalities and lesions. Therefore, the major advantage of surgical training with the 3D printed model is to enable trainees without any experience in endoscopic endonasal surgery to learn some surgical skills, before they are ready for cadaveric head dissection or assisting an endoscopic endonasal surgery.
With this training, the participants can focus on the anatomic structure when dissecting the cadaveric head, and on learning surgical techniques when assisting a surgery, which shortens the learning curve and improves learning efficiency of endoscopic endonasal surgery.
Conclusion
This 3D printed model has realistic anatomical condition of nasal passage and appropriate colors for different parts, and is a good tool for learning endoscopic endonasal surgery. Endoscopic endonasal surgical training using this 3D printed model can effectively improve surgical skills of trainees without prior endoscopic endonasal surgical experience. We believed that training using this 3D printed model can help the participants to focus on the anatomic structure when dissecting the cadaveric head, and on learning surgery techniques when assisting an endoscopic endonasal surgery, which shortens the learning curve and improves learning efficiency of endoscopic endonasal surgery.
Disclosure of conflict of interest
None.
References
- 1.Barkhoudarian G, Zada G, Laws ER. Endoscopic endonasal surgery for nonadenomatous sellar/parasellar lesions. World Neurosurg. 2014;82:S138–146. doi: 10.1016/j.wneu.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 2.Hoshide R, Teo C. Neuroendoscopy to achieve superior glioma resection outcomes. Neurosurgery. 2017;64:139–143. doi: 10.1093/neuros/nyx274. [DOI] [PubMed] [Google Scholar]
- 3.Tayebi Meybodi A, Benet A, Vigo V, Rodriguez Rubio R, Yousef S, Mokhtari P, Dones F, Kakaizada S, Lawton MT. Assessment of the endoscopic endonasal approach to the basilar apex region for aneurysm clipping. J Neurosurg. 2018:1–12. doi: 10.3171/2018.1.JNS172813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasan T. Is dissection humane? J Med Ethics Hist Med. 2011;4:4. [PMC free article] [PubMed] [Google Scholar]
- 5.Thawani JP, Singh N, Pisapia JM, Abdullah KG, Parker D, Pukenas BA, Zager EL, Verma R, Brem S. Three-dimensional printed modeling of diffuse low-grade gliomas and associated white matter tract anatomy. Neurosurgery. 2017;80:635–645. doi: 10.1093/neuros/nyx009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen S, Pan Z, Wu Y, Gu Z, Li M, Liang Z, Zhu H, Yao Y, Shui W, Shen Z, Zhao J, Pan H. The role of three-dimensional printed models of skull in anatomy education: a randomized controlled trail. Sci Rep. 2017;7:575. doi: 10.1038/s41598-017-00647-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu F, Qin Z, Xu C, Chen XY, Li RX, Wang LN, Peng DW, Sun HT, Tu Y, Chen C, Zhang S, Zhao ML, Li XH. Magnetic resonance imaging-three-dimensional printing technology fabricates customized scaffolds for brain tissue engineering. Neural Regen Res. 2017;12:614–622. doi: 10.4103/1673-5374.205101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AlReefi MA, Nguyen LH, Mongeau LG, Haq BU, Boyanapalli S, Hafeez N, Cegarra-Escolano F, Tewfik MA. Development and validation of a septoplasty training model using 3-dimensional printing technology. Int Forum Allergy Rhinol. 2017;7:399–404. doi: 10.1002/alr.21887. [DOI] [PubMed] [Google Scholar]
- 9.Weinstock P, Rehder R, Prabhu SP, Forbes PW, Roussin CJ, Cohen AR. Creation of a novel simulator for minimally invasive neurosurgery: fusion of 3D printing and special effects. J Neurosurg Pediatr. 2017;20:1–9. doi: 10.3171/2017.1.PEDS16568. [DOI] [PubMed] [Google Scholar]
- 10.Alrasheed AS, Nguyen LHP, Mongeau L, Funnell WRJ, Tewfik MA. Development and validation of a 3D-printed model of the ostiomeatal complex and frontal sinus for endoscopic sinus surgery training. Int Forum Allergy Rhinol. 2017;7:837–841. doi: 10.1002/alr.21960. [DOI] [PubMed] [Google Scholar]
- 11.Dong M, Chen G, Qin K, Ding X, Zhou D, Peng C, Zeng S, Deng X. Development of three-dimensional brain arteriovenous malformation model for patient communication and young neurosurgeon education. Br J Neurosurg. 2018:1–4. doi: 10.1080/02688697.2018.1424320. [DOI] [PubMed] [Google Scholar]
- 12.Tai BL, Wang AC, Joseph JR, Wang PI, Sullivan SE, McKean EL, Shih AJ, Rooney DM. A physical simulator for endoscopic endonasal drilling techniques: technical note. J Neurosurg. 2016;124:811–816. doi: 10.3171/2015.3.JNS1552. [DOI] [PubMed] [Google Scholar]
- 13.Wen G, Cong Z, Liu K, Tang C, Zhong C, Li L, Dai X, Ma C. A practical 3D printed simulator for endoscopic endonasal transsphenoidal surgery to improve basic operational skills. Childs Nerv Syst. 2016;32:1109–1116. doi: 10.1007/s00381-016-3051-0. [DOI] [PubMed] [Google Scholar]
- 14.Okuda T, Kataoka K, Kato A. Training in endoscopic endonasal transsphenoidal surgery using a skull model and eggs. Acta Neurochir (Wien) 2010;152:1801–1804. doi: 10.1007/s00701-010-0728-0. [DOI] [PubMed] [Google Scholar]
- 15.Christian E, Harris B, Wrobel B, Zada G. Endoscopic endonasal transsphenoidal surgery: implementation of an operative and perioperative checklist. Neurosurg Focus. 2014;37:E1. doi: 10.3171/2014.7.FOCUS14360. [DOI] [PubMed] [Google Scholar]
- 16.Koutourousiou M, Fernandez-Miranda JC, Stefko ST, Wang EW, Snyderman CH, Gardner PA. Endoscopic endonasal surgery for suprasellar meningiomas: experience with 75 patients. J Neurosurg. 2014;120:1326–1339. doi: 10.3171/2014.2.JNS13767. [DOI] [PubMed] [Google Scholar]
- 17.Cailleaux C, Papon JF, Nevoux J. Endoscopic endonasal surgery to correct congenital obstruction of the lacrimal pathway. Clin Otolaryngol. 2018 doi: 10.1111/coa.13180. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Willson TJ, Rowan NR, Wang EW. Middle turbinate manipulation and postoperative sinus obstruction after endoscopic endonasal skull-base surgery. Int Forum Allergy Rhinol. 2018;8:1132–1135. doi: 10.1002/alr.22151. [DOI] [PubMed] [Google Scholar]
- 19.Guo HC, Wang Y, Dai J, Ren CW, Li JH, Lai YQ. Application of 3D printing in the surgical planning of hypertrophic obstructive cardiomyopathy and physician-patient communication: a preliminary study. J Thorac Dis. 2018;10:867–873. doi: 10.21037/jtd.2018.01.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van de Belt TH, Nijmeijer H, Grim D, Engelen L, Vreeken R, van Gelder M, Ter Laan M. Patient-specific actual-size three-dimensional printed models for patient education in glioma treatment: first experiences. World Neurosurg. 2018;117:e99–e105. doi: 10.1016/j.wneu.2018.05.190. [DOI] [PubMed] [Google Scholar]
- 21.Bernhard JC, Isotani S, Matsugasumi T, Duddalwar V, Hung AJ, Suer E, Baco E, Satkunasivam R, Djaladat H, Metcalfe C, Hu B, Wong K, Park D, Nguyen M, Hwang D, Bazargani ST, de Castro Abreu AL, Aron M, Ukimura O, Gill IS. Personalized 3D printed model of kidney and tumor anatomy: a useful tool for patient education. World J Urol. 2016;34:337–345. doi: 10.1007/s00345-015-1632-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lau IWW, Liu D, Xu L, Fan Z, Sun Z. Clinical value of patient-specific three-dimensional printing of congenital heart disease: quantitative and qualitative assessments. PLoS One. 2018;13:e0194333. doi: 10.1371/journal.pone.0194333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tran NH, Tantidhnazet S, Raocharernporn S, Kiattavornchareon S, Pairuchvej V, Wongsirichat N. Accuracy of three-dimensional planning in surgery-first orthognathic surgery: planning versus outcome. J Clin Med Res. 2018;10:429–436. doi: 10.14740/jocmr3372w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Itagaki MW. Using 3D printed models for planning and guidance during endovascular intervention: a technical advance. Diagn Interv Radiol. 2015;21:338–341. doi: 10.5152/dir.2015.14469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chi F, Wang Y, Lin Y, Ge J, Qiu Y, Guo L. A learning curve of endoscopic transsphenoidal surgery for pituitary adenoma. J Craniofac Surg. 2013;24:2064–2067. doi: 10.1097/SCS.0b013e3182a24328. [DOI] [PubMed] [Google Scholar]


