Abstract
Purpose of review
Inadequate knowledge of the benefits, risks and opportunities for living donation is an important, potentially modifiable barrier to living donor transplantation. We assessed the current state of the evidence regarding strategies to increase knowledge, communication and access to living donor transplantation, as reported in peer-reviewed medical literature.
Recent Findings
Nineteen studies were reviewed, categorized as programs evaluated in randomized controlled trials (8 studies) and programs supported by observational (non-randomized) studies (11 studies). Content extraction demonstrated that comprehensive education about living donation and living donor transplantation involves multiple learners – the transplant candidate, potential living donors, and social support networks – and requires communicating complex information about the risks and benefits of donation, transplantation and alternative therapies to these different audiences. Transplant centers can help transplant patients learn about living donor transplantation through a variety of formats and modalities, including center-based, home-based and remote technology-based education, outreach to dialysis centers, and social media. Evaluation of these strategies and program themes informed a new Organ Procurement and Transplantation Network (OPTN)/United Network for Organ Sharing (UNOS) public education brochure.
Summary
Increasing transplant candidate knowledge and comfort in talking about living donation and transplantation can reduce educational barriers to pursuit of living donor transplants. Ongoing efforts are needed to develop, refine and disseminate educational programs to help improve transplant access for more patients in need of organ donors.
Keywords: Decision making, health education, living organ donation, living donor transplantation, patient education
INTRODUCTION
Living donor transplantation can provide excellent patient outcomes. The growing organ shortage translates to high morbidity and mortality rates on the deceased donor transplant waiting lists. Living donor kidney transplantation (LDKT) offers patients with end-stage renal disease (ESRD) the best chance for long-term dialysis-free survival.1 The benefits include faster access to transplant, with less time on dialysis and its associated risks, and superior long-term patient survival compared to both dialysis and deceased donor kidney transplantation (DDKT), at lower cost to the healthcare system. Despite these benefits and a rise in the kidney transplant waiting list to 100,000 persons,2 LDKT is the least common treatment option, currently performed in 5,800 cases in the United States per year compared to more than 14,000 DDKT in 2017. Living donor liver transplantation (LDLT) can also provide excellent recipient outcomes and reduce morbidity and mortality for patients with liver failure. Potential benefits of LDLT over deceased donor liver transplantation include the ability to control the timing of the transplant before the patient becomes too ill for transplant. The liver transplant waiting list currently comprises 14,000 persons.2 LDLT is performed for approximately 350 U.S. patients each year, compared to 7,700 deceased donor liver transplants in 2017.
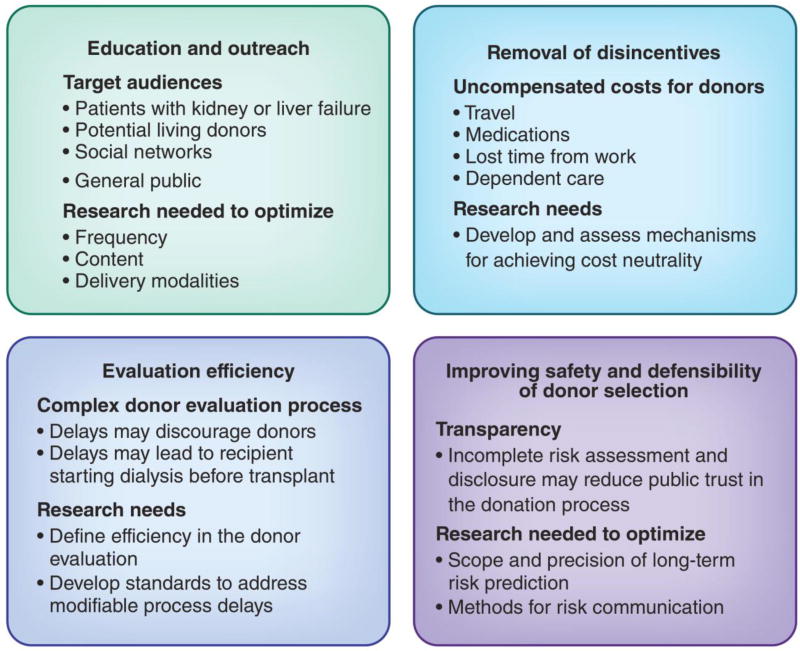
Based on data and surveys supporting positive public perceptions of living donation,3 a number of initiatives are underway to increase awareness of living donor transplantation. One example is an American Society of Transplantation Consensus Statement promoting LDKT as the “best treatment option” for eligible patients with kidney failure.4 The 2017 Kidney Disease: Improving Global Outcomes (KDIGO) “Clinical Practice Guideline on the Evaluation and Care of Living Kidney Donors” recognizes that public awareness of opportunities for living donation should be improved through education.5 While the need and benefits are clearly established, multiple barriers to living donor transplantation exist. Barriers include inadequate education and outreach, the complexity and potential inefficiencies in the living donor evaluation process, disincentives such as uncompensated costs for the donor, and ongoing needs to support and advance donor safety and risk assessment to sustain public trust in the donation process. Each barrier is a potential target for focused interventions (Figure 1).6
Figure 1.
Used with permission from the Clinical Journal of American Society of Nephrology.
Educational barriers to the pursuit of potential living donors by transplant candidates, or more specifically, inadequate knowledge of the benefits, risks and opportunities for the procedure, are important and modifiable. Comprehensive education about living donation and living donor transplantation involves multiple learners – the transplant candidate, potential living donors, and social support networks – and requires communicating complex information about the risks and benefits of living donation, transplantation and alternative therapies to these different audiences.7 Transplant programs can help transplant candidates learn about living donor transplantation through a variety of formats and modalities, including center-based, home-based and remote technology-based education, outreach to dialysis centers, and social media. Understanding the impact of such interventions is necessary to inform center choice and investment in programs suitable for their resources, processes, and patient populations, and to encourage patients to seek and participate in available programs at their centers.
To reduce educational barriers to living donor transplantation, a work group of the Organ Procurement and Transplantation Network (OPTN)/United Network for Organ Sharing (UNOS) Living Donor Committee formulated a project to create a new educational brochure for transplant candidates. As a foundational step in the brochure development, the work group reviewed the state of current evidence on strategies to increase knowledge, communication and access to living donor transplantation, as reported in peer-reviewed medical literature, as well as some emerging programs that have not yet been formally evaluated. This article describes the processes and findings of our evidence review.
Figure 1. Focal points for research to define effective strategies for increasing access to living donor transplantation. [Adapted with permission from Lentine KL and Mandelbrodt D, Clin J Am Soc Nephrol 2017.6]
EVIDENCE REVIEW METHODOLOGY
Process of Educational Program Identification
The work group identified and reviewed studies of living organ donor educational programs reported in the medical literature. We queried the MEDLINE electronic database for reports published through February 28, 2017 using the Medical Subject Headings (MeSH) terms “living donor* or living organ donor*”, “live donor* or live organ donor,” “live donor kidney transplantation”, “live donor liver transplantation”, “living donation”, “tissue donor*”, “kidney transplant*”, “liver transplant*”, “education”, “patient education,” “health education,” “education program,” “education session,” “teaching or teaching session,” “counseling,” “decision aid,” “pamphlet,” “handout or patient education handout,” “audiovisual aid” “teaching materials,” “consumer health information,” “health knowledge, attitudes, practice,” and “healthcare disparities”. Searches were limited to articles published in English. Manual review of the reference lists of identified articles was also performed. Each study was reviewed to extract a brief program description (Tables 1 and 2), a description of supporting evidence, and information about study limitations or other considerations. One work group member performed the primary extraction for each identified article, and a second work group member confirmed the extraction.
Table 1.
Description of programs evaluated in clinical trials
| Program | Additional Program Description |
|---|---|
| “House Calls” or Home-Based Education Program, (Rodrigue et al, 2007 & 2014) 10,39 |
|
| “Kidney Team at Home” (Ismail et al, 2014; Massey et al, 2016)11,12 |
|
| “Talking About Live Kidney Donation” (TALK) and “TALK-Social Worker” Intervention Programs (Boulware et al, 2013; DePasquale et al, 2012)13,14 |
|
| “Living ACTS” (About Choices in Transplantation and Sharing) (Arriola et al, 2014)15 |
|
| “Infórmate” Culturally Targeted Website (Gordon et al, 2015 & 2016) 16,17 |
|
| “Written Educational Materials followed by Structured Educational Session” (Barnieh et al, 2011) 18 |
|
ESRD, end-stage renal disease; HB, home-based; LDKT, living donor kidney transplantation
Table 2.
Description of programs supported by observational (non-randomized) studies
| Program | Additional Program Description |
|---|---|
| “Patient Navigators in Community-Based Nephrology Practices” (Marlow et al, 2016)19 |
|
| “Living Donor Family Education” (Schweitzer et al, 1997 & 2000; Foster et al, 2002)20–22 |
|
| “Seminars on Saturdays” (Brown et al, 2011)23 |
|
| “Live Donor Champion” (LDC) (Garonzik-Wang et al, 2012)24 |
|
| “Hispanic Transplant Education” (Gordon et al, 2014)25 |
|
| “Educational Intervention Based in Peer Experiences” (Delair et al, 2010)26 |
|
| “Pre-Dialysis Education” (PDEP) (Cankaya et al, 2013)27 |
|
| “Living Donation Education” (LED) (Cervera et al, 2015)28 |
|
| Social Media/ Facebook Apps (Kumar et al, 2016)29 |
|
| “My Transplant Coach” Decision Aid (Axelrod et al, 2017)30 |
|
LDC, live donor champion; LDKT, living donor kidney transplantation
The project was not designed as a systematic review in which only a narrow range of studies are assessed. Rather, the work group sought to identify the full range of living donor transplant and donation educational programs that have been developed and evaluated. Studies were categorized by methodologic rigor based on study design, ranging from randomized controlled trials, to observational or non-randomized studies. Emerging programs that have not yet been formally evaluated or that do not yet have published data were described but were not included in the data extraction.
Based on the available evidence, the work group identified key elements of effective educational strategies. The evidence is predominantly related to LDKT. While educational programs focused on LDLT are also critically important, there is currently a paucity of evidence for the effectiveness of educational programs related to this transplant option.
EDUCATIONAL PROGRAM SUMMARIES AND EVIDENCE
We identified 19 studies meeting selection criteria. The identified educational programs are described below, categorized as programs evaluated in randomized controlled trials (8 studies) and programs supported by observational (non-randomized) studies (11 studies).
Each educational program description includes a brief summary of: 1) the program’s overall approach (further programmatic information is presented in Tables 1 and 2); 2) the evidence supporting the program’s efficacy; and 3) other commentary. Following the program summaries and evidence, we briefly describe several emerging programs that have not yet been formally evaluated. Finally, we summarize some of the educational programs’ commonalities with respect to design, content and delivery teams and suggest next steps to advance patient education.
Programs Evaluated in Randomized Controlled Trials (Table 1)
While randomized controlled trials offer the highest standard of evidence, only a limited number of trials have been performed to evaluate educational interventions related to living donor transplantation. Most included knowledge and attitudes as endpoints, while only a subset reported living donor evaluations or access to living donor transplantation.
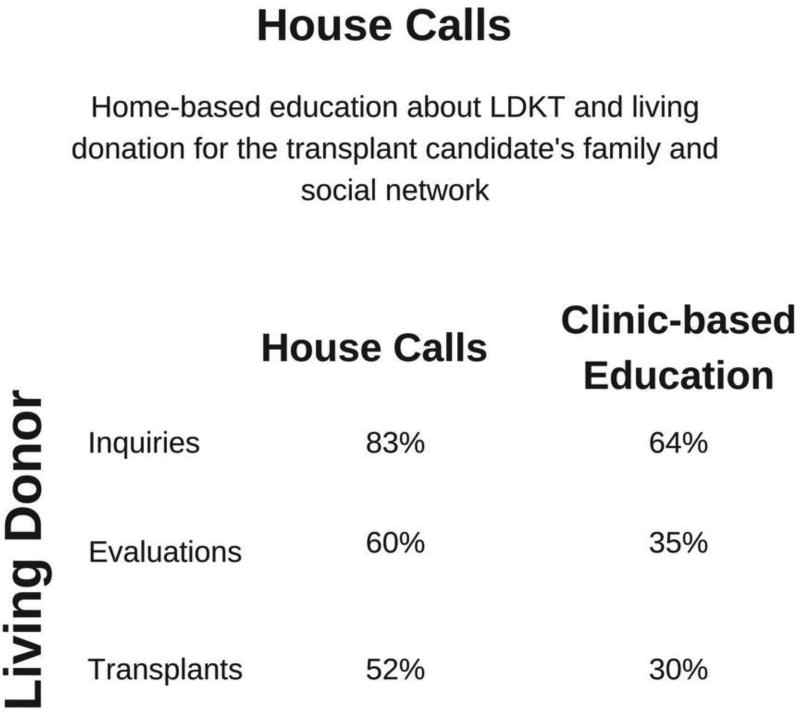
“House Calls” or Home-Based Education Program
Program
“House Calls” is a home-based (HB) intervention in which trained transplant health educators perform a 60 to 90-minute LDKT education session involving family and members of the candidate’s social network. [Figure 2]
Figure 2.
“House Calls” or Home-Based Education Program
Evidence
In one single-center trial, 152 kidney transplant candidates were randomized to clinic-based (CB) education or CB+HB. Compared to CB alone, significantly more patients who received CB+HB had living donor inquiries (83% vs 64%), donor evaluations (60% vs 35%) and LDKT (52% vs 30%) one-year following the intervention.8 Both groups demonstrated increased LDKT knowledge after CB education, but HB education led to the largest increase in LDKT knowledge, and also to greater willingness to discuss LDKT with others and a decrease in LDKT concerns.
A secondary analysis provided details on culturally sensitive aspects of the intervention:9 This analysis found that increases in both donor evaluations and LDKT at 1 year with CB+HB compared to CB were larger for black (versus white) candidates. Notably, the LDKT rate for black patients who received HB education mirrored the LDKT rate of white patients before the intervention; i.e., the intervention appeared to eliminate the initial racial disparity in LDKT at that center.
In a second single-center trial, 152 black kidney transplant candidates were randomized to the HB intervention, CB education in a group session with other patients and their guests at the transplant center, or CB individual patient counseling.10 Although rates of LDKT did not differ significantly between the three groups at the 2-year endpoint, patients receiving HB education were more likely than patients in the other two groups to have at least one donor inquiry (82% vs. 61% vs. 47%) and evaluation (65% vs. 39% vs. 27%). Patients in the HB group also had higher LDKT knowledge, fewer LDKT concerns, and higher willingness to talk to others about donation 6 weeks after intervention.
Commentary. Results of these two trials may be limited by possible self-selection bias among those who gave consent and completed the study (i.e., such patients already may have been thinking about LDKT). In the first trial, there was a higher dropout rate among patients randomized to receive HB education, suggesting further self-selection, and the drop-out rate was higher among black (versus white) patients. The degree to which trial results generalize to other groups of patients and to other regions of the United States is unknown. Training and supporting staff to perform the HB intervention may be too costly or logistically prohibitive for some centers.
“Kidney Team at Home” Home-Based Family Intervention
Program
This program is a Dutch adaptation of the “House Calls” intervention.
Evidence
In a single-center trial, 163 patients referred for transplant evaluation or on the DDKT waiting list were randomized to usual education or usual care plus + HB education.11 All participants had been unable to find a potential living donor prior to enrollment. Patients in the CB+HB group showed significantly more improvements in LDKT knowledge and communication compared to the control group. Participating members of the patient’s social network also showed significant increases in knowledge and positive attitudes related to discussing kidney replacement therapies and willingness to donate a kidney, and a decrease in risk perception. Excluding patients who died or who received a DDKT, those who received CB+HB education (versus CB education alone) had significantly more living donor inquiries (32% vs. 74%), evaluations (17% vs. 64%) and actual LDKTs (10% vs. 44%) at 6 months following the intervention. In a second trial involving patients who had not yet initiated renal replacement therapy, patients who received CB+HB education (versus CB education alone) were substantially more likely to receive a preemptive LDKT (65% vs 39% of those who received LDKT within 2 years of intervention).12
Commentary. The follow-up period for LDKT in the first trial was relatively brief and the trial results may be limited by possible self-selection bias among those who gave consent and completed the study. Of note, the LDKT rate at the study center already was very high (~70%), so patients enrolled in the trial may have faced more substantial barriers to LDKT than other patients at the center, given the baseline success at this center. Drop-out was associated with limited social networks, suggesting that the intervention may be less effective in patients with fewer family members and friends. The second trial well-received by those who used it, but had a high non-participation rate among the target population of 60%, with many declining for the very barriers that such educational programs aim to overcome (concern for burdening others; concern for insufficient social network). Also, although aimed at encouraging pre-emptive LDKT, a large proportion of participants did not progress to needing renal replacement during the 2-year study period, demonstrating the challenge of appropriately timing transplant education for pre-dialysis patients.
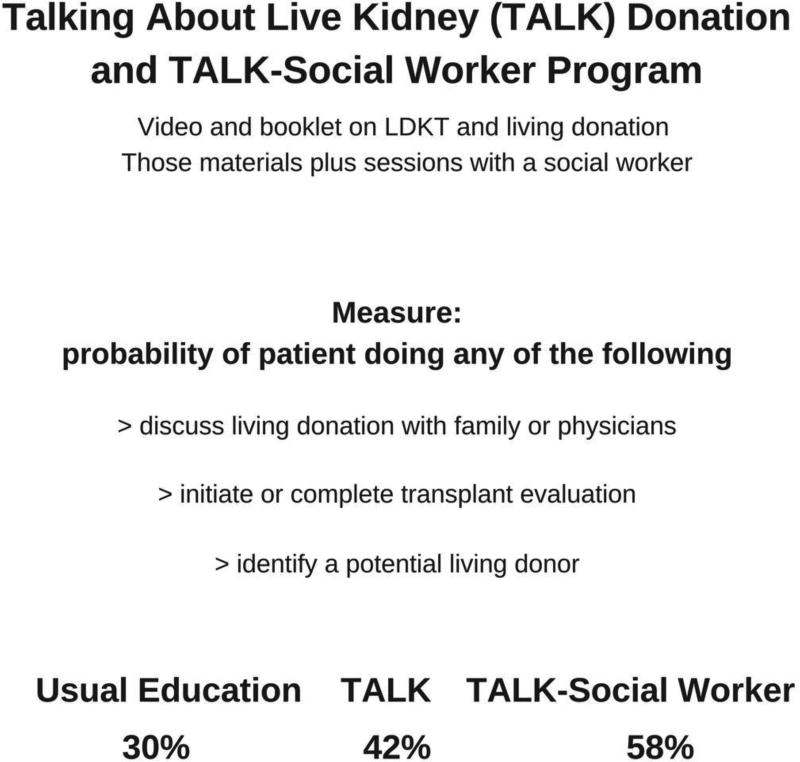
“Talking About Live Kidney Donation” (TALK) and “TALK-Social Worker” Intervention programs
Program
The TALK education intervention consists of a video and booklet on LDKT.13 The “TALK-Social Worker” intervention combines the video/booklet with two hour-long sessions delivered by a social worker either in the patient’s home or in the transplant center.14 In the first session, the social worker distributes the video and booklet and helps the patient identify barriers to considering or pursuing LDKT. The patient is asked to invite family/friends to a second session. At the second session, the social worker helps social network members identify barriers to discussing LDKT and living donation. Problem-solving and motivational interviewing techniques are employed at both sessions. [Figure 3]
Figure 3.
Talking About Live Kidney (TALK) Donation and TALK-Social Worker Program
Evidence
In this trial, 130 patients were randomized by site (nephrology practice) into three study arms (usual care with nephrologists, and one of the two TALK conditions). Eligible patients were drawn from academically affiliated or community nephrology practices, and were not yet on dialysis (although they may have had a transplant evaluation). The primary outcome was whether patients engaged in any one of five behaviors reflecting discussion and/or pursuit of living donor transplantation (discussions with family, discussions with physicians, initiating transplant evaluation, completing transplant evaluation, identifying a potential living donor). Engagement in at least one behavior over 6 months was 30% with usual care, 42% with TALK-education, and 58% with the “TALK-Social Worker” intervention. Results were not significantly different between the two TALK arms. The most common behaviors were talking to family and physicians. No differences were observed between groups in interest or concerns about LDKT.
Commentary. The follow-up period was relatively brief, and the study did not consider actual receipt of LDKT. The educational materials did not provide extensive information on risks and benefits of LDKT, and financial barriers were not considered in the TALK interventions. Only 67% of patients in the “TALK-Social Worker” intervention attended both sessions, and 19% of patients attending the second session did not bring family/friends. More complete uptake of the interventions may have been limited by the high percentage of pre-dialysis patients who may not have been “primed” or ready for focused discussion of LDKT and living donation.
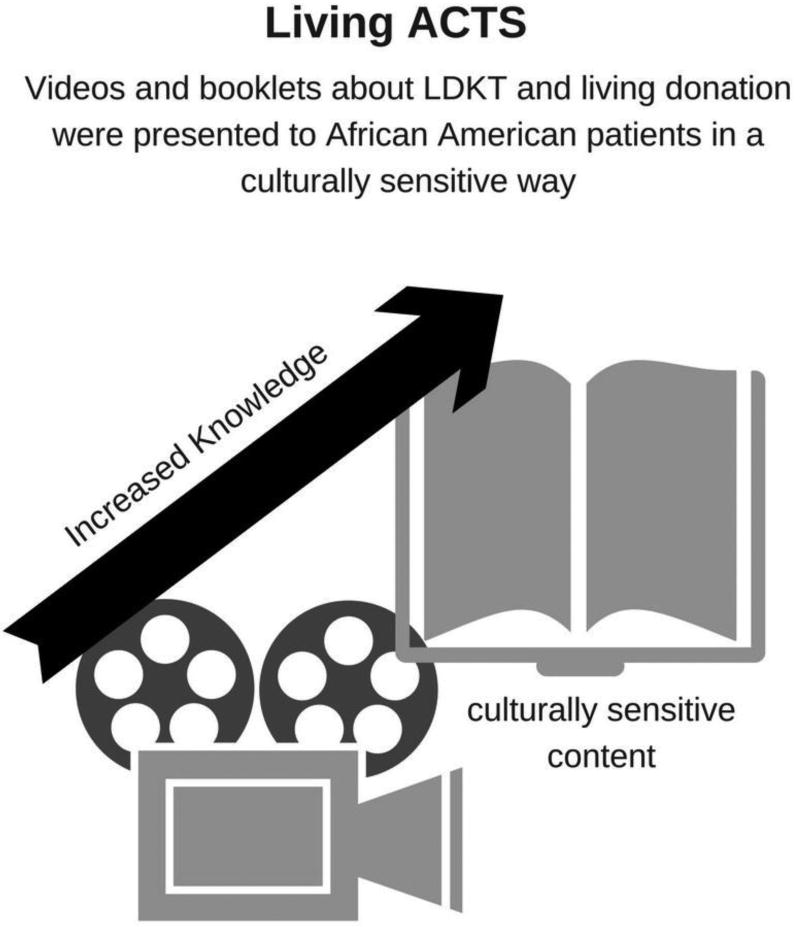
“Living ACTS” (About Choices in Transplantation and Sharing) [Figure 4]
Figure 4.
Living ACTS
Program
“Living ACTS” (About Choices in Transplant and Sharing) was designed as a culturally sensitive intervention targeted to African-American patients.15 The intervention consists of a video and booklet.
Evidence
In a single-center trial, 296 black adults who presented for transplant evaluation were randomized to receive standard education plus the “Living ACTS” intervention, or standard transplant education plus an attention-control video about exercise.15 Standard education comprised a web-based course (transplant-specific education) completed before the evaluation. Knowledge about LDKT and willingness to talk with family about living donation were assessed before randomization, immediately after education, and 6 months later. Subjects in the “Living ACTS” group showed a significantly greater increase in knowledge about living donor transplantation immediately after the intervention than did controls; this was maintained through the 6-month follow-up period. Although the intervention group showed significantly higher willingness to talk with family about living donation, this difference was evident at baseline and did not change over time. Intervention participants endorsed greater perceived benefits of living donor transplantation than did controls immediately after the intervention, but this effect did not persist at the 6-month follow-up.
Commentary. Although 96% of patients approached agreed to enroll, the sample was one of convenience and generalizability is not known. In addition, the analyses did not follow an intent-to-treat approach and included only those with complete follow-up data. Because no information was collected from patients on educational activities or interactions with family regarding living donation after they returned home, it is difficult to speculate on why the intervention affected only patients’ knowledge.
“Infórmate” Culturally Targeted Website for Hispanic Transplant Candidates
Program
The authors developed a bilingual, culturally targeted website, “Infórmate”, for Hispanic transplant candidates and members of their social network. The website was designed to overcome many of the known sociocultural barriers to LDKT among Hispanics, including misconceptions about living donation, language barriers, immigrant status issues, financial concerns, and distrust of the healthcare system. 16
Evidence
In a two-center trial, 282 new kidney transplant candidates were randomized to receive access to the website or to usual care.17 Usual care comprised attending a transplant education class on the day of their initial evaluation. Patients and their family members in both groups received this standard care; however, one group was also given access to “Infórmate” before attending the class. Patients and family members in both groups had significant improvements in LDKT knowledge from pre-intervention to the 3-week follow-up; however, knowledge gains were larger for patients assigned to website group. [Figure 5]
Figure 5.
Culturally Targeted Website for Hispanic Transplant Candidates
Commentary. The majority of study participants were family members of the transplant candidate. Knowledge gains were not presented by participant type, thus it is unknown whether knowledge gains occurred equally for patients and family members. There is also a possibility of intervention contamination, as the website intervention occurred before a group education session including all study participants. Patients and family members who had access to the website may have shared its content and information with participants in the usual care group, thus potentially suppressing the effects of the website intervention. Finally, the study evaluated changes in knowledge only, so it is not known whether the website impacts rates of living kidney donation or LDKT.
Written Educational Materials followed by Structured Educational Session
Program
In this intervention, patients newly referred for transplant evaluation are mailed written materials about living kidney donation and the benefits of LDKT.18 Approximately two weeks later, patients and their invited guests attend a 2-hour educational session at the transplant center.
Evidence
In a single-center trial, 100 patients who presented for their initial transplant evaluation were randomized to receive either usual care or usual care plus the enhanced LDKT educational program.18 Usual care comprised informal discussions with providers about all aspects of kidney transplantation as patients progressed through the evaluation process. The primary outcome was potential living donor contacts with the transplant centers within 3 months after the intervention. Also, patients completed questionnaires about LDKT knowledge and ESRD treatment preferences before and 2 weeks after the intervention. The two groups did not differ significantly in the number of potential living donors who contacted the center. Extending the follow-up period to 6 months also did not yield significant between-groups differences. Patients in the intervention group who had not identified LDKT as their treatment preference initially were more likely to state that this was now their treatment preference 2 weeks after the intervention.
Commentary. The trial only enrolled 50% of the intended sample size, and the authors acknowledge that the study was under-powered. Although LDKT knowledge was assessed, these results are not reported. Details are lacking regarding the content of usual care, making it difficult to determine the nature and dose of any LDKT information the control group may have received. Finally, the drop-out rate for the intervention was very high (30% did not attend the education session), suggesting further self-selection.
Programs Supported by Observational (Non-Randomized) Studies (Table 2)
A variety of additional programs have been developed that may be offered at transplant centers or elsewhere but that have not yet been tested in randomized controlled trials. Thus, efficacy in improving knowledge or identification of potential living donors has not been fully established. These programs relied on quasi-experimental designs (e.g., use of historical controls or comparison groups), or single group pre-post observational designs, often in small pilot samples. Despite the early nature of the evidence, the programs below are noteworthy for their creativity in developing strategies using peer-mentors, social media tools, and mobile decision aids.
“Patient Navigators” in Community-Based Nephrology Practices
Program
Social workers, or “Patient Navigators”, are placed in community-based nephrology practices after receiving training in transplantation, living donation, and cultural sensitivity from transplant physicians, nurse coordinators, and social workers. 19 The social workers meet with patients before or after their appointment with the nephrologist and, upon request, schedule additional individual appointments with patients.
Evidence
In a non-randomized observational study conducted over 58-months, patients referred to the transplant center from two nephrology offices with a social worker-navigator were compared to patients referred from 90 nephrology offices without patient navigation.19 The investigators retrieved outcomes data on 2,722 transplant candidates and 424 transplant recipients at their center. Social worker-navigators had a mean of 6 contacts per patient (range: 1 to 32). Patients from nephrology practices with a social worker-navigator were more likely to have potential living donor inquiries (38% versus 34%) and initial screening (30% versus 26%) compared to patients from nephrology practices without navigators. However, the two groups did not differ significantly in rates of complete living donor evaluations or LDKT (4% in both groups).
Commentary. The “dose” of the intervention was not standardized, which may be relevant to efficacy of the program. Patients who had more contacts with social worker-navigators may have progressed more rapidly through the transplant evaluation process and had more interest in LDKT. Social workers were hired as full-time employees, which may make the intervention cost-prohibitive for many transplant programs to adopt. Finally, there was no defined, consistent time period from navigation to the observed outcomes (living donor inquiries and evaluations, LDKTs) across the sample.
“Living Donor Family Education” Program
Program
Designed and then refined across a series of publications, this program is offered at the transplant center during the evaluation process to “recipient families,” which includes relatives as well as friends of candidates for kidney or simultaneous kidney-pancreas transplant.20–22 The intervention comprises a didactic presentation and discussion led by nurse coordinators familiar with living donation, LDKT, and related literature. The intervention also includes an educational video.
Evidence
In an initial publication, after the program had been offered for over one year, the percentage of patients who had potential living donors submit blood samples to screen for candidacy in the group receiving the new program were compared to the percentage of patients screened before the program existed. 20 Among 1,363 patients registered on the transplant waiting list during the 54-month study period, a significantly higher percentage of patients had at least one potential living donor tissue typed after versus before the program was implemented (39% vs. 33%). The program was particularly effective for blacks and older patients, who had higher rates of living donor screening after versus before program implementation (36% vs. 28% for blacks; 31% vs. 19% for older patients). In additional analyses, the authors observed that the rate of kidney transplant was significantly higher after the program’s initiation than before, but post-transplant survival rates were not affected. In subsequent analyses over a 4-year period after program inception, the authors continued to find increased rates of potential living donors submitting blood tests after versus before program inception, but findings were inconsistent in terms of subgroup effects.
Commentary. The results are primarily limited by reliance on a historical comparison group; rates of potential living donors submitting blood tests may have increased naturally over time even without the intervention. In addition, although the authors conclude that it is important to have ethnically appropriate teaching materials, they did not directly evaluate whether that specific component contributed to any effects. The study included only a single center and generalizability is not known.
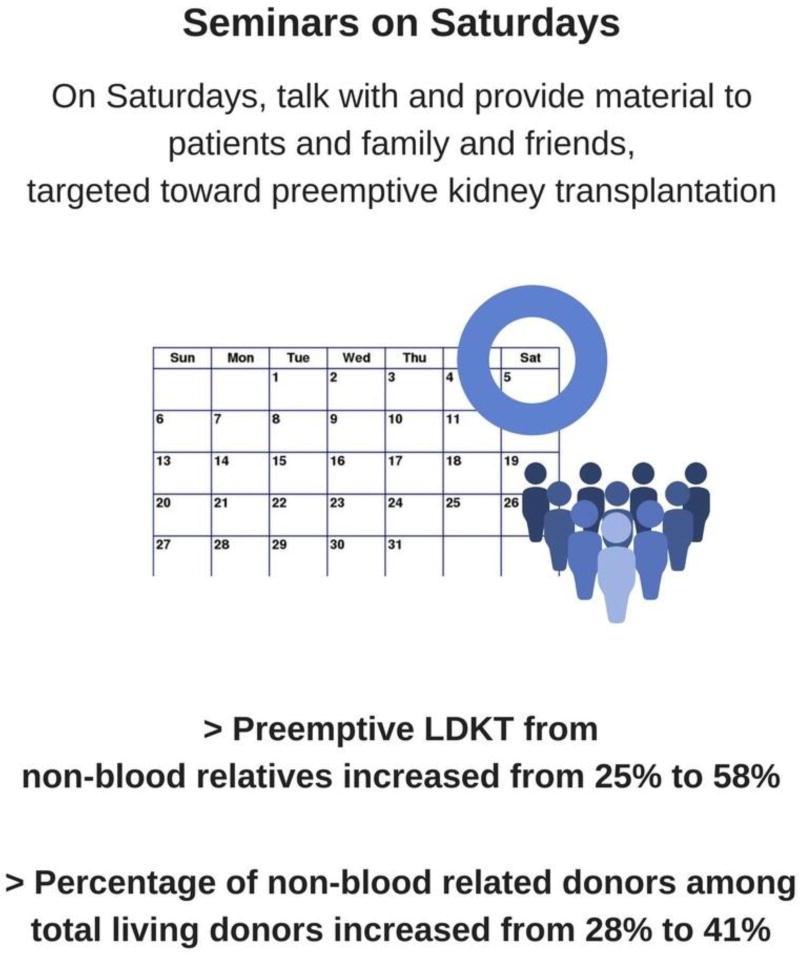
“Seminars on Saturdays” Program
Program
The intervention is targeted toward (but not exclusive to) preemptive kidney transplantation, and consists of formal talks, facilitated discussion during break-out sessions, audiovisual aides, and an information packet, along with follow-up contact by a transplant coordinator to determine if more information is needed.23 The program is offered by a multi-disciplinary team every 2 months (6 times per year) on a Saturday to pre-dialysis patients and their family/friends, as well as to all patients on the kidney waitlist, and to all dialysis patients not yet waitlisted but deemed suitable for transplant. [Figure 6]
Figure 6.
Seminars on Saturdays
Evidence
Analyses are based on comparisons of outcomes collected annually during a period spanning 3 years before and 3 years after the program began to be offered at a single center.23 The investigators report a growth in program attendance and a significant increase in the percentage of LDKTs that were preemptive at their center (from 28% to 44%). The percentage of non-blood-related donors among total living donors increased from 28% to 41% (statistical significance not reported). Preemptive LDKT that were from non-blood-related donors significantly increased (from 25% to 58%). The authors also found that the percentages of minority donors increased from 39% in earlier years to 52% in later years (statistical significance not reported).
Commentary. The results focus on comparisons of annual data and do not directly compare outcomes in individuals who attended an intervention session versus those who did not attend. The changes over time cannot be specifically attributed to launching the intervention. The analyses do not appear to specifically analyze trends over time but instead compare rates across 6 nominal groups (defined by year). In other words, the authors report a difference across the 6 groups defined by year but do not test directly that the percentages monotonically increase by year. Some effects are not subjected to any statistical test.
“Live Donor Champion” Program
Program
The “Live Donor Champion” (LDC) program was designed on the premise that training a “champion” or advocate to share about the transplant candidate’s disease and need for an organ donor would help identify more living donors. 24 In the LDC program, each transplant candidate identifies one person to be their “Live Donor Champion”, who is then trained to talk about kidney disease, organ donation and transplant, and skills for initiating conversations. Anti-coercion training is an important part of the curriculum. Champions are provided with educational materials, “business cards” with contact information, and other resources from the transplant center.
Evidence
Pilot data come from a single-center prospective cohort study of 15 adult kidney transplant candidates who had been on the DDKT waitlist for at least 3 months and had no potential living donors at the time of enrollment.24 Each candidate identified someone from their social network to serve as their LDC. LDC comfort in initiating conversations about transplantation increased over time. Twenty-five potential donors contacted the center on behalf of LDC participants; four participants achieved LDKT and three additional participants had donors in evaluation, compared to none of the 15 matched controls. [Figure 7]
Figure 7.
Live Donor Champion
Commentary. This was a non-randomized, small pilot study subject to selection bias because those patients who nominated “LDCs” may have been more motivated and willing to pursue LDKT. While nearly half of the “LDC” were black, it is unknown whether the intervention yielded the same benefit regardless of race. The lengthy duration of the intervention (6 months) is a practical limitation, especially for those patients seeking preemptive LDKT. Finally, patients with smaller social networks may benefit less from the intervention, particularly if they are unable to identify a champion.
“Hispanic Transplant Education” Program
Program
This intervention is designed to be a linguistically and culturally competent educational program for Hispanic transplant candidates, using an established framework for standardizing the measurement and reporting of high quality, culturally competent care.25 The intervention consists of two educational sessions offered at the time of patients’ evaluation for transplant at the center.
Evidence
The study used a pre-post design in which 43 patients and 70 family members completed pre-intervention measures, received the intervention, and then immediately completed post-intervention measures.25 Family members’ and friends’ attitudes about being a living kidney donor were also assessed. Knowledge level significantly increased among both patients and family/friends. Knowledge was higher at post-test among patients than in family/friends, and among younger and more educated individuals. Pre-to-post attitude change was noted in some areas: patients became more motivated to pursue LDKT and felt more favorable about it. Family/friends increased in willingness to become living donors and became more motivated to begin the living donor evaluation. High levels of satisfaction with the intervention were noted.
Commentary. The resources needed to mount this type of intervention may not be available to all transplant programs. The study did not include a comparison group and the analyses focused on patients who completed the intervention. Thus, the robustness and generalizability of the findings are unknown. There was no follow-up period to determine if knowledge and attitudes were maintained over time. It is unclear whether improved attitudes regarding living donation and motivation to pursue living donation translated into an increase in the number of living donor inquiries among those family/friends.
Educational Intervention Based in Peer Experiences
Program
This intervention was developed to expose liver transplant candidates (and potential living liver donors in their social network) to the experiences of former living liver donors.26 The intervention includes a booklet and video (available in 6 languages), and a website that includes the same written and video materials.
Evidence
Across 5 transplant centers, the investigators compared 338 liver transplant candidates who received the intervention to 437 patients who received “usual education” at those same centers before the intervention was offered.26 Primary outcomes were patients’ living donation/transplantation knowledge and feelings of self-efficacy to discuss living donation with others. Patients in the intervention group reported significantly more knowledge and higher levels of self-efficacy than those in the comparison group. Patients in the intervention group were significantly more likely to have talked about living donation with others than those in the comparison group. The total number of family/friends who presented for donor evaluation and the number of actual living donors both increased from before to after intervention over a 3-year period. Among those in the intervention group who were known to either have viewed the intervention materials (27% of the group) or not viewed them (58% of the group), those who viewed them showed significantly higher self-efficacy for discussing living donation with others.
Commentary. The results are primarily limited by reliance on a historical comparison group; other elements may have led to the differences observed in knowledge and self-efficacy, and the numbers of donor candidate evaluations and ultimate donations may also have changed over time due to other factors. Only a minority of patients in the intervention group reported viewing the intervention materials, and so the actual exposure to the intervention was limited.
“Pre-Dialysis Education” Program
Program
A “Pre-Dialysis Education” program (PDEP) was developed as a training kit using visual and written information cards and comprising 6 modules targeted towards the degree of kidney disease experienced by patients with chronic kidney failure.27
Evidence
The intervention was evaluated in a single university hospital in Turkey in a non-randomized retrospective design.27 Among 88 LDKT recipients over an 8-year period, 61 patients who received PDEP were compared to 27 patients who received transplants before PDEP was available. Significantly more PDEP patients had preemptive LDKT than those who did not receive PDEP (43% vs. 19%). PDEP participants were more likely to receive preemptive transplants from spouses, siblings and non-parent relatives, and less likely to receive preemptive transplants from parents, than patients not exposed to PDEP.
Commentary. Very limited detail is available regarding the conceptualization, development or specific content of the PDEP modules, challenging both the ability to replicate the intervention in other settings, and the evaluation of strengths and limitations of the intervention.
“Living Donation Education” Program, center-based LDKT education for black and Hispanic patients
Program
The “Living Donation Education” (LDE) program was developed to address common barriers to LDKT and living kidney donation among black and Hispanic patients.28 The intervention is delivered in two phases at the transplant center. In Phase I, patients and family members attend a formal education session with healthcare providers. In Phase II, patients and family members are invited to meet with a living donor and recipient pair. The study originally was designed to also examine HB education developed by others;8 however, this group was dropped after only one patient chose to participate in a HB education session.
Evidence
In a single-center study, 294 patients on the kidney transplant waiting list were informed about LDE by telephone and encouraged to attend the program. 28 Of these, 75 patients attended the Phase I educational session and 7 patients returned for the Phase II session. The authors tracked the number of patients who attended the LDE and examined whether they had a higher likelihood of living donor inquiries, evaluations, and transplants compared to patients who did not attend an LDE session but who attended the transplant program’s regular patient support group. There were no statistically significant differences between the two groups on any of these outcomes. Also, the two groups did not differ in changes in LDKT knowledge, willingness, concerns, or readiness.
Commentary. The study is limited by low statistical power, non-randomized design, selection bias, and cross-contamination. Few patients attended the sessions, particularly the second session. It is possible that interest in LDE was limited because the transplant program in which the study occurred was not able to perform LDKT for a year due to program issues that occurred shortly after study initiation. While the program was permitted to evaluate potential living donors, the restriction on performing LDKT could have adversely impacted study participation rates and outcomes. Also, half of the patients receiving the LDE intervention also participated in the control condition by attending one or more support group sessions. The initial study design included a HB education arm which could not be assessed due to lack of participation.
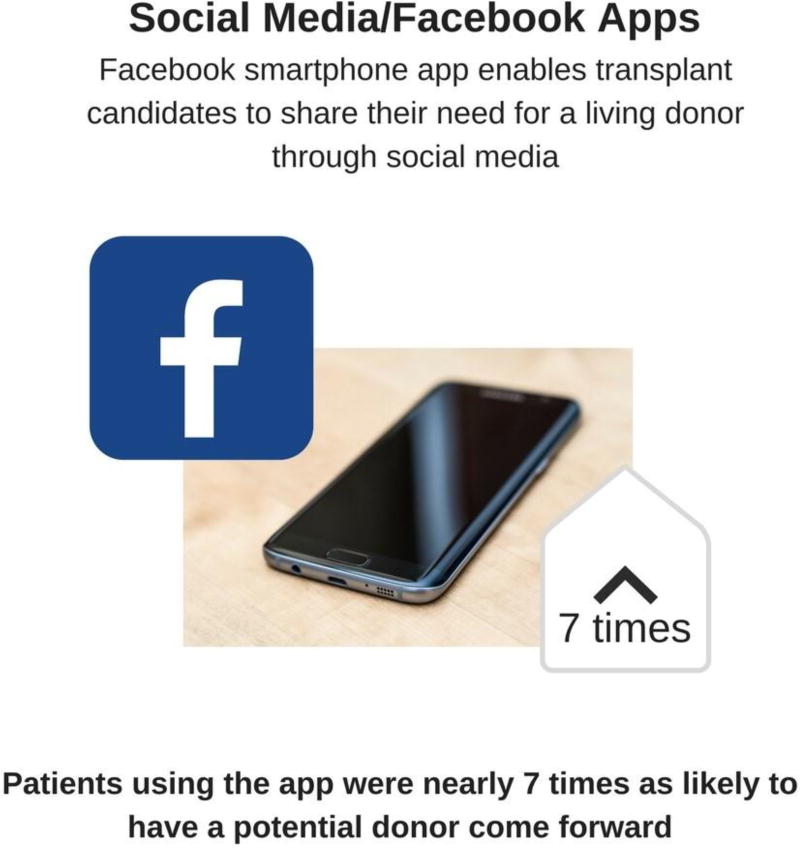
Social Media/Facebook Apps
Program
A Facebook smartphone app was developed that enables transplant candidates to share their need for a living donor through social media, providing an indirect means for communication with a broad social network.29
Evidence
In a pilot study among 54 adult transplant candidates without potential living donors at the time of enrollment, the majority of candidates using the smartphone app reported it to be “good” to “excellent” with respect to the installation process, readability, simplicity, clarity and content.29 Compared to matched controls, patients using the app were nearly 7-times as likely to have a potential donor come forward on their behalf within 10-months after enrollment. [Figure 8]
Figure 8.
Social Media/Facebook Apps
Commentary. Limitations of this initial study include the small sample size, non-randomized design, and potential selection bias from enrollment of more motivated or technologically sophisticated candidates. Future studies should assess the impact of the Facebook smartphone app on conversion of donor referrals to LDKT, cost-effectiveness (including consideration of staff time for referral intake and screening), and the quality of patient shared-decision making about transplant options and donation.
“My Transplant Coach” Decision Aid
Program
A mobile iOS (iPad) app was created utilizing animated patient education and individualized, risk-adjusted outcomes following kidney transplantation to improve overall transplant knowledge in kidney transplant candidates. The patient-centered information allows candidates to consider the relative benefits of LDKT and various types of DDKT (e.g., low-moderate kidney donor profile index (KDPI), high KDPI, or an Increased Infection Risk donor). 30
Evidence
In a pilot study of 81 patients at two large US transplant programs, the participants were guided through the app by a research assistant prior to receiving any standard educational sessions at their transplant program. Participants completed pre- and post-surveys of the app to assess comfort with technology, knowledge of transplant options and acceptability and cultural competency of the app. Overall, the app resulted in significant increases in patient knowledge of transplantation, acceptance of LDKT and DDKT options and comfort in discussing transplantation with others.
Commentary. A strength of the app is the presentation of patient-centric education based on the individual candidate’s demographic and clinical information and relevant data for their anticipated Donation Service Area. Though the app scored well for overall impression and appropriateness for participant’s race/ethnicity, the study participants were of modestly higher education than the average ESRD population and already possessed moderate health literacy. The app improved transplant knowledge and understanding of outcome differences between LDKT and DDKT options; however, differences were observed based upon pre-existing access to and comfort with technology. The app is also only available in English, and so may not fully address the educational needs of candidates with limited English skills; however, a Spanish translation is expected in the next version of the app. The study did not assess the impact of the app on the participants’ actual pursuit and acceptance of organs.
Emerging Programs
Other educational programs focused on LDKT and living donation are emerging, including in planned trials, but have not yet been formally evaluated. Examples of such emerging programs include:
“Explore Transplant at Home.”31 This program will offer video and print educational resources about DDKT and LDKT developed as part of the “Explore Transplant” program to socioeconomically disadvantaged dialysis patients in their homes, with or without supplementary telephone interactions with a health educator. Thus, the study is focused on the impact of home-based delivery of previously developed educational resources.
“ELITE” Program.32 This program will use and adapt the “Explore Transplant” materials as part of the education of potential adult kidney transplant candidates attending their initial transplant evaluation at one transplant center, in addition to usual educational materials. The program will focus on knowledge of living donation and living donor transplantation, and include a video and meeting with a transplant educator.
“Your Path to Transplant.”33 This study will evaluate materials from the “Explore Transplant” program in a computer-tailored format. The novel aspect of this program is examination of a validated transplant decision-making measure that can be delivered either in person, via the telephone, or electronically via a computer.
“iChoose Kidney.”34 “iChoose Kidney” was developed by a multi-disciplinary team as a shared decision aid for clinicians to present individualized risk predictions of short-term patient survival with kidney transplantation versus dialysis to patients. It is available through the Internet (http://ichoosekidney.emory.edu/) or a mobile (iOS) app. “iChoose Kidney” presents the patient survival or mortality risk in a patient-friendly manner using both graphical and numeric representations. A randomized trial to assess knowledge, treatment preferences and access to transplant including LDKT is underway.34
Educational Program Commonalities: Design, Content and Delivery Teams
While education programs differ in detail, published studies suggest some commonalities among effective programs, including provision of information early in the organ disease process, an opportunity to include family and friends, ideally in a comfortable setting, and opportunities to talk with living donors and living donor transplant recipients (Table 3). Many of the published interventions seek to help transplant candidates identify individuals from their social network to participate with the candidate in educational sessions. A common design theme focuses on supporting productive communication between transplant candidates and members of his or her social network on organ donation and transplantation, often in the presence of a transplant medical expert to answer questions and concerns for both parties, or after training the patient or an advocate to communicate with the social network. Some of these programs provide educational materials (e.g., brochures, videos, decision aids) prepared for both the transplant candidates and potential donors. Social media tools for sharing a patient’s need for an organ donor safely and effectively with their social network are also emerging.
Table 3.
Common Design Elements of Effective Living Donor Transplant Education Programs
|
Regarding content, effective educational programs generally include core subject matter related to the need, risks, benefits and outcomes of living donation and living donor transplantation, compared to other treatment options (Table 4).
Table 4.
Core Content of Living Donor Transplant Education Programs
|
|
To deliver education, effective living donor transplant educational programs include a cross-section of transplant professionals and volunteers (Table 5). Educational programs need not rely disproportionately on any one category of transplant professional. Multi-disciplinary transplant teams, often supported by peers including living donors and transplant recipients, help provide and support effective education.
Table 5.
Common Delivery Teams for Living Donor Transplant Education Programs
|
Transplant center education programs can also positively influence patients’ use of the internet in connection with organ transplantation.35 First, transplant programs can help vet the factual basis of online information when patients begin to consider their options. This is particularly important given the amount of information – and misinformation – about living donation accessible on the internet. Second, educating patients and their friends and family about living donation can increase their appropriate and constructive communication about living organ donation and transplantation on social media, as described above. Importantly, literacy-related disparities in technology access and use are widespread, such that patients with lower levels of literacy are less likely to own smartphones or to access and use the internet, particularly for health reasons.36 Thus, future interventions should consider these disparities and ensure that health promotion activities do not further exacerbate disparities.
Conclusions and Next Steps
Living donor transplantation is an important treatment option for end-stage organ disease that can be performed safely to benefit many patients and society.4, 5 However, living donor transplantation has not increased in response to the growing organ shortage. Increasing transplant candidate knowledge and comfort in talking about living donation and transplantation can reduce educational barriers to pursuit of living donor transplants. The likelihood that transplant candidates will identify someone willing to consider living donation can be increased by the provision of clearly stated educational information, involving the patient’s social network, and repeated over phases of care. Electronic-health technology is emerging as an efficient modality for education delivery, but more comparative work is needed to determine whether electronic-learning, telehealth, or telephone-based education programs are as effective as programs that deliver education with an in-person educator. New technology-based tools, such as social media, also show promise as strategies to help patients expand their social network, but require careful development with attention to online privacy and safety, and efforts to avoid disadvantaging those with low access to technology. A new patient-focused educational brochure, “How to Find a Living Donor: Make Your Transplant Happen”, describes some evidence-based education strategies and is available as a print-on-demand resource from the OPTN website (https://optn.transplant.hrsa.gov/media/2267/find_a_living_donor.pdf).
Unanswered questions related to living donor transplant educational interventions include how much educational content (i.e., “dose”) should be provided and at what time points in the transplant evaluation pathway.7 It is also unclear whether the dose should vary based on patient characteristics (e.g., disease state, race/ethnicity, size of social network, etc.) and to what extent interventions should be tailored to these patient characteristics. There are known disparities in access to living donor transplant based on race/ethnicity, literacy and health literacy, and other factors,37, 38 and efforts to improve equity for non-white patients and those with lower levels of socioeconomic status and health literacy are important priorities. Empirical studies of approaches to support and increase living donor transplantation including formal evaluations of education, incorporating assessment of transplant rates as hard outcomes and associated costs, are feasible and necessary to advance evidence-based, effective practices.6 Robust efforts to develop and evaluate strategies for increasing knowledge, communication and access to living donor transplantation must to continue to support opportunities for more healthy, willing persons to give the gift of life to patients in need.
Acknowledgments
The authors thank OPTN/UNOS Communications and OPTN/UNOS Committees for review of project materials, including Patient Affairs, Minority Affairs, Pediatrics, Transplant Administrators, Transplant Coordinators, and Organ Procurement Organizations Committees. The authors also thank subject matter experts for feedback, including Elisa Gordon, PhD; Rachel Patzer, PhD; Dorry Segev, MD, PhD; Amy Waterman, PhD; and the team at Health Literacy Media (St. Louis, MO).
Preparation of this manuscript was supported by Awards from the National Institute of Diabetes and Digestive and Kidney Diseases No. R01DK098727 to James R. Rodrigue, No. R01DK101715 to Mary Amanda Dew, and No. K01DK114388 to Macey Henderson. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
ABBREVIATIONS and ACRONYMS
- ACTS
“About Choices in Transplant and Sharing”
- CB
Clinic-based
- DDKT
Deceased donor kidney transplantation
- DSA
Donation Service Area
- ESRD
End-stage renal disease
- HB
Home-based
- KDIGO
Kidney Disease: Improving Global Outcomes
- KDPI
Kidney Donor Profile Index
- LDC
“Live Donor Champion”
- LDE
Living donation education
- LDKT
Live donor kidney transplantation
- LDLT
Living donor liver transplantation
- MeSH
Medical Subject Headings
- OPTN
Organ Procurement and Transplant Network
- PDEP
“Pre-Dialysis Education” program
- TALK
“Talk About Live Kidney Donation”
- UNOS
United Network for Organ Sharing
APPENDIX. Resources for more information
| Program | Investigators | Contact |
|---|---|---|
|
| ||
| “House Calls” | James Rodrigue, PhD | jrrodrig@bidmc.harvard.edu |
| Beth Israel Deaconess Medical Center | ||
| Boston, MA, USA | ||
|
| ||
| “Kidney Team at Home” | Emma Massey, PhD | e.massey@erasmusmc.nl |
| Erasmus Medical Center | ||
| Rotterdam, The Netherlands | ||
|
| ||
| “TALK” | L. Ebony Boulware, MD | ebony.boulware@duke.edu; http://ckddecisions.org/ |
| Duke University School of Medicine, | ||
| Durham, NC, USA | ||
|
| ||
| “ACTS” | Kimberly Jacob Arriola, PhD | kjacoba@sph.emory.edu |
| Emory University School of Medicine | ||
| Atlanta, GA, USA | ||
|
| ||
| “Infórmate” | Elisa Gordon, PhD | e-gordon@northwestern.edu |
| Northwestern University School of Medicine Chicago, IL, USA | www.informate.org | |
|
| ||
| “Structured Education” | Brenda R. Hemmelgarn, MD, PhD | brenda.hemmelgarn@albertahealthservices.ca |
| Foothills Medical Centre | ||
| Calgary, Alberta, Canada | ||
|
| ||
| “Patient Navigators” | Prabhakar Baliga, MD | baligap@musc.edu |
| Medical University of South Carolina Charleston, SC, USA | ||
|
| ||
| “Living Donor Family Education” | Clarence Foster, MD | foster@uci.edu |
| University of California Irvine, Orange, CA, USA | ||
|
| ||
| “Seminars on Saturdays” | Wendy Brown, MD | wendy.brown@imperial.nhs.uk |
| Hammersmith Hospital, London, UK | ||
|
| ||
| “Live Donor Champion” | Dorry Segev, MD | dorry@jhmi.edu |
| Johns Hopkins University School of Medicine Baltimore, MD, USA | ||
|
| ||
| Hispanic Transplant Education | Elisa Gordon, PhD | e-gordon@northwestern.edu |
| Northwestern University School of Medicine Chicago, IL, USA | ||
|
| ||
| Peer-based education | Samantha DeLair, MSE | sdelair@nyclt.org; http:/www.nyclt.org/living_donor/ |
| New York Center for Liver Transplantation | ||
| East Greenbush, NY, USA | ||
|
| ||
| “Pre-Dialysis Education” | Erdem Cankaya, MD & Mustafa Keles, MD | dr25erdem@gmail.com; keles.m@gmail.com |
| Ataturk University Medical School | ||
| Erzurum, Turkey | ||
|
| ||
| “Living Donation Education” | Liise Kayler, MD | lkayler@ecmc.edu |
| Erie County Medical Center, Buffalo, NY, USA | ||
|
| ||
| Social Media / Facebook Apps | Andrew Cameron, MD | acamero5@jhmi.edu |
| Johns Hopkins University School of Medicine Baltimore, MD, USA | ||
|
| ||
| “My Transplant Coach” | Explore Transplant | awaterman@mednet.ucla.edu; david.a.axelrod@lahey.org |
| Health Literacy Media | ||
| St. Louis, MO, USA | ||
Footnotes
Compliance with Ethical Guidelines
Conflict of Interest
Macey Henderson is a member of the board of directors for OPTN/UNOS (unpaid, no conflict).
Krista Lentine, James Rodrigue, Mary Amanda Dew, Randolph Schaffer, Patrick Kacani, Pono Shim, Lee Bolton, and William Sanchez declare no conflicts of interest.
Randee Bloom and Mary Amanda Dew report funds paid by OPTN/UNOS for committee meeting attendance (unpaid, no conflict). Heather Hunt is President of LIVE ON Organ Donation, Inc., a non-profit organization that raises money to support living organ donors’ non-medical expenses (unpaid, no conflict).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
••Of major importance
- 1.U. S. Renal Data System. USRDS 2015 Annual Data Report: End-stage Renal Disease (ESRD) in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; [Accessed: July 2, 2017]. 2016. Ch 7: Transplantation. Available at: https://www.usrds.org/2016/view/v2_07.aspx. [Google Scholar]
- 2.OPTN (Organ Procurement and Transplantation Network)/UNOS (United Network for Organ Sharing) National Data Reports, Transplants by Donor Type, Latest Data. https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/ (Access date: Sept 21, 2017)
- 3.National Kidney Foundation. [Accessed: July 8, 2016];Cross-Sectional Survey. Public Says "Yes" to Strangers. https://www.kidney.org/news/newsroom/newsreleases/0083. Published June 22, 2000.
- 4.LaPointe Rudow D, Hays R, Baliga P, Cohen DJ, Cooper M, Danovitch GM, Dew MA, Gordon EJ, Mandelbrot DA, McGuire S, Milton J, Moore DR, Morgievich M, Schold JD, Segev DL, Serur D, Steiner RW, Tan JC, Waterman AD, Zavala EY, Rodrigue JR. Consensus conference on best practices in live kidney donation: recommendations to optimize education, access, and care. American Journal of Transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2015;15:914–22. doi: 10.1111/ajt.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5**.Lentine KL, Kasiske BL, Levey AS, Adams PL, Alberu J, Bakr MA, Gallon L, Garvey CA, Guleria S, Li PK, Segev DL, Taler SJ, Tanabe K, Wright L, Zeier MG, Cheung M, Garg AX. KDIGO Clinical Practice Guideline on the Evaluation and Care of Living Kidney Donors. Transplantation. 2017;101:S1–S109. doi: 10.1097/TP.0000000000001769. New international guideline on living kidney donation that explicitly recognizes the need to increase public awareness of opportunities for living donation through education. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lentine KL, Mandelbrot D. Moving from Intuition to Data: Building the Evidence to Support and Increase Living Donor Kidney Transplantation. Clin J Am Soc Nephrol. 2017;12:1383–1385. doi: 10.2215/CJN.07150717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waterman AD, Robbins ML, Peipert JD. Educating Prospective Kidney Transplant Recipients and Living Donors about Living Donation: Practical and Theoretical Recommendations for Increasing Living Donation Rates. Current transplantation reports. 2016;3:1–9. doi: 10.1007/s40472-016-0090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodrigue JR, Cornell DL, Lin JK, Kaplan B, Howard RJ. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. American Journal of Transplantation. 2007;7:394–401. doi: 10.1111/j.1600-6143.2006.01623.x. [DOI] [PubMed] [Google Scholar]
- 9.Rodrigue JR, Cornell DL, Kaplan B, Howard RJ. A randomized trial of a home-based educational approach to increase live donor kidney transplantation: effects in blacks and whites. Am J Kidney Dis. 2008;51:663–70. doi: 10.1053/j.ajkd.2007.11.027. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigue JR, Paek MJ, Egbuna O, Waterman AD, Schold JD, Pavlakis M, Mandelbrot DA. Making House Calls Increases Living Donor Inquiries and Evaluations for Blacks on the Kidney Transplant Waiting List. Transplantation. 2014;98:979–86. doi: 10.1097/TP.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ismail SY, Luchtenburg AE, Timman R, Zuidema WC, Boonstra C, Weimar W, Busschbach JJ, Massey EK. Home-based family intervention increases knowledge, communication and living donation rates: a randomized controlled trial. American Journal of Transplantation. 2014;14:1862–9. doi: 10.1111/ajt.12751. [DOI] [PubMed] [Google Scholar]
- 12.Massey EK, Gregoor PJ, Nette RW, van den Dorpel MA, van Kooij A, Zietse R, Zuidema WC, Timman R, Busschbach JJ, Weimar W. Early home-based group education to support informed decision-making among patients with end-stage renal disease: a multi-centre randomized controlled trial. Nephrol Dial Transplant. 2016;31:823–30. doi: 10.1093/ndt/gfv322. [DOI] [PubMed] [Google Scholar]
- 13.Boulware LE, Hill-Briggs F, Kraus ES, Melancon JK, Falcone B, Ephraim PL, Jaar BG, Gimenez L, Choi M, Senga M, Kolotos M, Lewis-Boyer L, Cook C, Light L, DePasquale N, Noletto T, Powe NR. Effectiveness of educational and social worker interventions to activate patients' discussion and pursuit of preemptive living donor kidney transplantation: a randomized controlled trial. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2013;61:476–86. doi: 10.1053/j.ajkd.2012.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DePasquale N, Hill-Briggs F, Darrell L, Boyer LL, Ephraim P, Boulware LE. Feasibility and acceptability of the TALK social worker intervention to improve live kidney transplantation. Health & social work. 2012;37:234–49. doi: 10.1093/hsw/hls034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arriola KR, Powell CL, Thompson NJ, Perryman JP, Basu M. Living donor transplant education for African American patients with end-stage renal disease. Prog Transplant. 2014;24:362–70. doi: 10.7182/pit2014830. [DOI] [PubMed] [Google Scholar]
- 16.Gordon EJ, Feinglass J, Carney P, Ramirez D, Olivero M, O'Connor K, MacLean J, Brucker J, Caicedo JC. An interactive, bilingual, culturally targeted website about living kidney donation and transplantation for Hispanics: development and formative evaluation. JMIR Res Protoc. 2015:e42. doi: 10.2196/resprot.3838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gordon EJ, Feinglass J, Carney P, Vera K, Olivero M, Black A, O'Connor K, MacLean J, Nichols S, Sageshima J, Preczewski L, Caicedo JC. A culturally targeted website for hispanics/latinos about living kidney donation and transplantation: a randomized controlled trial of increased knowledge. Transplantation. 2016;100:1149–60. doi: 10.1097/TP.0000000000000932. [DOI] [PubMed] [Google Scholar]
- 18.Barnieh L, McLaughlin K, Manns BJ, Klarenbach S, Yilmaz S, Taub K, Hemmelgarn BR. Evaluation of an education intervention to increase the pursuit of living kidney donation: a randomized controlled trial. Prog Transplant. 2011;21:36–42. doi: 10.1177/152692481102100105. [DOI] [PubMed] [Google Scholar]
- 19.Marlow NM, Kazley AS, Chavin KD, Simpson KN, Balliet W, Baliga PK. A patient navigator and education program for increasing potential living donors: a comparative observational study. Clin Transplant. 2016;30:619–27. doi: 10.1111/ctr.12728. [DOI] [PubMed] [Google Scholar]
- 20.Schweitzer EJ, Yoon S, Hart J, Anderson L, Barnes R, Evans D, Hartman K, Jaekels J, Johnson LB, Kuo PC, Hoehn-Saric E, Klassen DK, Weir MR, Bartlett ST. Increased living donor volunteer rates with a formal recipient family education program. Am J Kidney Dis. 1997;29:739–45. doi: 10.1016/s0272-6386(97)90128-1. [DOI] [PubMed] [Google Scholar]
- 21.Schweitzer EJ, Wilson J, Jacobs S, Machan CH, Philosophe B, Farney A, Colonna J, Jarrell BE, Bartlett ST. Increased rates of donation with laparoscopic donor nephrectomy. Annals of surgery. 2000;232:392–400. doi: 10.1097/00000658-200009000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foster CE, 3rd, Philosophe B, Schweitzer EJ, Colonna JO, Farney AC, Jarrell B, Anderson L, Bartlett ST. A decade of experience with renal transplantation in African-Americans. Annals of surgery. 2002;236:794–804. doi: 10.1097/00000658-200212000-00012. discussion-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown W, McDermott J, Figueiredo AE, Loucaidou M, Galliford J, Papalois V. Invited manuscript poster on renal-related education American Society of Nephrology. Nov. 16–21, 2010. Improving access to kidney transplant information has increased preemptive living kidney donation. Renal failure. 2011;33:658–62. doi: 10.3109/0886022X.2011.589948. [DOI] [PubMed] [Google Scholar]
- 24**.Garonzik-Wang JM, Berger JC, Ros RL, Kucirka LM, Deshpande NA, Boyarsky BJ, Montgomery RA, Hall EC, James NT, Segev DL. Live donor champion: finding live kidney donors by separating the advocate from the patient. Transplantation. 2012;93:1147–50. doi: 10.1097/TP.0b013e31824e75a5. Pilot report of an innovative educational program designed to overcome the reluctance of patients to ask others to consider living donation by training an advocate to share about the transplant candidate’s disease and need for an organ donor with their social network. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gordon EJ, Reddy E, Gil S, Feinglass J, Rodde J, Abecassis MM, Caicedo JC. Culturally competent transplant program improves Hispanics' knowledge and attitudes about live kidney donation and transplant. Prog Transplant. 2014;24:56–68. doi: 10.7182/pit2014378. [DOI] [PubMed] [Google Scholar]
- 26*.Delair S, Feeley TH, Kim H, Del Rio Martin J, Kim-Schluger L, Lapointe Rudow D, Orloff M, Sheiner PA, Teperman L. A peer-based intervention to educate liver transplant candidates about living donor liver transplantation. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2010;16:42–8. doi: 10.1002/lt.21937. Educational interventions related to living donor liver transplantation are under-studied. The study developed educational materials for liver transplant candidates including the experiences of former living liver donors, such as views about the surgery, recovery, costs, employment, and life after donation. [DOI] [PubMed] [Google Scholar]
- 27.Cankaya E, Cetinkaya R, Keles M, Gulcan E, Uyanik A, Kisaoglu A, Ozogul B, Ozturk G, Aydinli B. Does a predialysis education program increase the number of pre-emptive renal transplantations? Transplantation proceedings. 2013;45:887–9. doi: 10.1016/j.transproceed.2013.02.075. [DOI] [PubMed] [Google Scholar]
- 28.Cervera I, Gomez DeVargas M, Cortes CM, Ahsanuddin S, DeFeao M, McDonough P, Velez C, Kim J, Marcus P, Kayler LK. A hospital-based educational approach to increase live donor kidney transplantation among blacks and Hispanics. Medical Science Technology. 2015;56:43–52. [Google Scholar]
- 29.Kumar K, King EA, Muzaale AD, Konel JM, Bramstedt KA, Massie AB, Segev DL, Cameron AM. A Smartphone App for Increasing Live Organ Donation. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16:3548–53. doi: 10.1111/ajt.13961. [DOI] [PubMed] [Google Scholar]
- 30.Axelrod DA, Kynard-Amerson CS, Wojciechowski D, Jacobs M, Lentine KL, Schnitzler M, Peipert JD, Waterman AD. Cultural competency of a mobile, customized patient education tool for improving potential kidney transplant recipients' knowledge and decision-making. Clin Transplant. 2017;31 doi: 10.1111/ctr.12944. [DOI] [PubMed] [Google Scholar]
- 31.Waterman AD, McSorley AM, Peipert JD, Goalby CJ, Peace LJ, Lutz PA, Thein JL. Explore Transplant at Home: a randomized control trial of an educational intervention to increase transplant knowledge for Black and White socioeconomically disadvantaged dialysis patients. BMC nephrology. 2015;16:150. doi: 10.1186/s12882-015-0143-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weng FL, Brown DR, Peipert JD, Holland B, Waterman AD. Protocol of a cluster randomized trial of an educational intervention to increase knowledge of living donor kidney transplant among potential transplant candidates. BMC nephrology. 2013;14:256. doi: 10.1186/1471-2369-14-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Waterman AD, Robbins ML, Paiva AL, Peipert JD, Kynard-Amerson CS, Goalby CJ, Davis LA, Thein JL, Schenk EA, Baldwin KA, Skelton SL, Amoyal NR, Brick LA. Your Path to Transplant: a randomized controlled trial of a tailored computer education intervention to increase living donor kidney transplant. BMC nephrology. 2014;15:166. doi: 10.1186/1471-2369-15-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patzer RE, Basu M, Mohan S, Smith KD, Wolf M, Ladner D, Friedewald JJ, Chiles M, Russell A, McPherson L, Gander J, Pastan S. A Randomized Controlled Trial of a Mobile Clinical Decision Aid to Improve Access to Kidney Transplantation: iChoose Kidney. Kidney Int Rep. 2016;1:34–42. doi: 10.1016/j.ekir.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Henderson ML, Clayville KA, Fisher JS, Kuntz KK, Mysel H, Purnell TS, Schaffer RL, Sherman LA, Willock EP, Gordon EJ. Social media and organ donation: Ethically navigating the next frontier. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2017;17:2803–09. doi: 10.1111/ajt.14444. [DOI] [PubMed] [Google Scholar]
- 36.Bailey SC, O'Conor R, Bojarski EA, Mullen R, Patzer RE, Vicencio D, Jacobson KL, Parker RM, Wolf MS. Literacy disparities in patient access and health-related use of internet and mobile technologies. Health Expect. 2015;18:3079–87. doi: 10.1111/hex.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Axelrod DA, Dzebisashvili N, Schnitzler MA, Salvalaggio PR, Segev DL, Gentry SE, Tuttle-Newhall J, Lentine KL. The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol. 2010;5:2276–88. doi: 10.2215/CJN.04940610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hall EC, James NT, Garonzik Wang JM, Berger JC, Montgomery RA, Dagher NN, Desai NM, Segev DL. Center-level factors and racial disparities in living donor kidney transplantation. Am J Kidney Dis. 2012;59:849–57. doi: 10.1053/j.ajkd.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 39**.Rodrigue JR, Cornell DL, Lin JK, Kaplan B, Howard RJ. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. American Journal of Transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2007;7:394–401. doi: 10.1111/j.1600-6143.2006.01623.x. Extension of a seminal trial demonstrating that home-based education of kidney transplant candidates and members of their social network significantly increases living donor evaluations and donations/transplantations. This trial was directed at African-American patients to help resolve racial disparities in access to living donor transplantation. [DOI] [PubMed] [Google Scholar]