Abstract
Objective:
To test an air cleaner and health coach intervention to reduce secondhand smoke exposure compared with air cleaners alone or no air cleaners in reducing particulate matter (PM), air nicotine, and urine cotinine concentrations and increasing symptom-free days in children with asthma residing with a smoker.
Design:
Randomized controlled trial, with randomization embedded in study database.
Settings:
The Johns Hopkins Hospital Children’s Center and homes of children.
Participants:
Children with asthma, residing with a smoker, randomly assigned to interventions consisting of air cleaners only (n=41), air cleaners plus a health coach (n=41), or delayed air cleaner (control) (n=44).
Main Outcome Measures:
Changes in PM, air nicotine, and urine cotinine concentrations and symptom-free days during the 6-month study.
Results:
The overall follow-up rate was high (91.3%). Changes in mean fine and coarse PM (PM2.5 and PM2.5–10) concentrations (baseline to 6 months) were significantly lower in both air cleaner groups compared with the control group (mean differences for PM2.5 concentrations: control, 3.5 μg/m3; air cleaner only, −19.9 μg/m3; and air cleaner plus health coach, −16.1 μg/m3; P=.003; and PM2.5–10 concentrations: control, 2.4 μg/m3; air cleaner only, −8.7 μg/m3; and air cleaner plus health coach, −10.6 μg/m3; P=.02). No differences were noted in air nicotine or urine cotinine concentrations. The health coach provided no additional reduction in PM concentrations. Symptom-free days were significantly increased in both air cleaner groups compared with the control group (P=.03).
Conclusion:
Although the use of air cleaners can result in a significant reduction in indoor PM concentrations and a significant increase in symptom-free days, it is not enough to prevent exposure to secondhand smoke.
MORE THAN 30% OF US children are exposed to secondhand smoke (SHS) in their homes,1,2 with rates as high as 40% to 46% of children living in poverty.3 Despite parental awareness that SHS exacerbates asthma, 40% to 67% of inner-city children with asthma reside in a household with at least 1 smoker.4,5 Accordingly, avoidance of SHS exposures is a key recommendation of national and international asthma guidelines.6 Smoking is the dominant contributor to indoor particulate matter (PM) levels, increasing fine PM concentrations (PM2.5) by up to 25 to 45 μg/m3, compared with the 3- to 6-μg/m3 increase associated with indoor sweeping or cooking.7–9 Tobacco smoke is a complex mixture consisting of a gas-vapor phase and a particulate phase containing more than 4000 individual chemical constituents.10,11 Reduction in PM concentrations of SHS exposures with the use of air cleaners has been reported12–15; however, the data have been deemed insufficient to recommend the use of indoor air-cleaning devices to alleviate asthma symptoms.16
Total home smoking bans are difficult to sustain in inner-city families.4 Moreover, inner-city children often reside in multiunit housing that may predispose them to higher SHS exposure via shared common spaces and ventilation systems with households with smokers.17 Based on the success of a behavioral SHS reduction intervention that reduced air nicotine levels18 and previous reports of reduction in PM concentration with the use of air cleaners,12–15 we hypothesized that the combination of air cleaners with a behavioral intervention promoting home smoking bans would reduce levels of PM, air nicotine, and urine cotinine and reduce asthma morbidity in inner-city children with asthma who reside with a smoker compared with children receiving air cleaners alone or a control condition of no air cleaners or behavioral intervention.
METHODS
STUDY DESIGN
This randomized 3-arm controlled trial, the Particulate Reduction Education in City Homes (PREACH) study, was reviewed and approved by The Johns Hopkins Medical Institutional Review Board and registered with clinicaltrials.gov (NCT00466024). Written informed consent was obtained from the child’s primary caregiver. All clinic and laboratory staff were masked to group assignment during recruitment and follow-up. Participants were randomized in a 1:1:1 ratio with random block sizes. Randomization was performed by the study coordinator, who activated a randomization function embedded in the study database. All study staff, including all investigators, were blinded to subsequent group assignment. All participants agreed to attend 2 clinic and home visits for data collection at baseline and 6-month follow-up. During each clinic visit, the caregiver was administered a questionnaire, and urine samples were obtained from each child for cotinine analysis as a biomarker of SHS exposure. Home indoor air quality assessments were conducted by trained home indoor monitoring technicians within 2 weeks of the child’s baseline and 6-month follow-up clinic visits. Laboratory staff who processed biological and environmental samples were blinded to study assignments.
SAMPLE
The names of 1462 potentially eligible children diagnosed as having asthma were obtained from patient rosters of 1 urban pediatric emergency department and 2 community pediatric practices from October 1, 2006, through December 31, 2008. Letters were mailed to caregivers of children with asthma to set up screening appointments. Owing to inaccurate diagnoses and inaccurate age, address, and telephone information noted in medical records, only 189 children were available for screening and recruitment, and 126 children (66.7%) were enrolled and randomized. Most children were recruited during the fall season with no differences noted by group for season of recruitment. Eligibility criteria included child age of 6 to 12 years; physician-diagnosed asthma, symptom frequency, and/or controller medication use signifying persistent asthma6; a smoker in the home who smoked more than 5 cigarettes per day and resided in the home at least 4 days per week; and residence in the Baltimore metropolitan area. Several attempts were made to contact all potentially eligible participants by telephone, with at least 10 attempts made at varying times and days.
STUDY GROUP DESCRIPTIONS
Control Group
Families randomized to the control group received asthma education during 4 nurse home visits as an attention control group. Asthma education included review of asthma medications, spacer and peak flow techniques, development of an asthma action plan, and provision of written asthma education materials. Two high-efficiency particle air (HEPA) cleaners were placed in the child’s home (bedroom and living room) after the final follow-up home-monitoring visit. The HEPA air cleaners (Holmes Harmony Air Purifier HAP650; Holmes, a subsidiary of Jarden Corporation, Rye, New York) were 48 × 27 × 61-cm (19×10.63×24-in) units with an activated carbon filter, a pleated HEPA filter, 4 speeds, a clean air delivery rate of 225, and a recommended cleaning area of 10.8 m2 (342 ft2) (a room 5.4×5.7 m [18×19 ft]). The mean (SD) area of the study homes was 54.9 (18.6) m2 (610 [207] ft2), and the average bedroom area was 10.8 m2 (120 ft2) (3.0×3.6 m [10×12 ft]). Families were instructed to run the air cleaners continuously using the medium speed.
Air Cleaner Group
Families randomized into the air cleaner group received 2 air cleaners and the 4 asthma education sessions described in the previous section. Air cleaners were placed in the bedroom where the child slept 4 or more nights per week and in the family television or living room. Families who relocated during the study intervention underwent reevaluation for indoor air quality at the new residence.
Air Cleaner Plus Health Coach Group
Families randomized to the air cleaner plus health coach behavioral intervention group received the 2 air cleaners and four 30- to 45-minute nurse health coach home visits that included the asthma education described in the previous sections and a behavioral intervention. All health coach visits were completed within 2 months of randomization. The SHS behavioral intervention was a modified motivational health coach SHS reduction program for low-income families18 with the following 5 core components: (1) identify the child’s SHS exposure risk, (2) assess the caregiver’s motivation and readiness for behavior change, (3) set an SHS–home smoking ban goal with the caregiver for which the caregiver signs a contingency contract for established behavior change, (4) encourage and monitor the use of air cleaners, and (5) teach the child SHS avoidance techniques. The nurse interventionist received ongoing weekly supervision to review successes and difficulties in implementing the health coach protocol.
MEASURES
Child SHS Exposure
The child’s SHS exposure in the home was based on the care-giver’s self-report of smoking frequency and location in the home, number of cigarettes smoked inside and outside the home, and the number of quit attempts during the caregiver’s lifetime. Exposure to SHS was limited to the child’s primary household of 5 or more days each week. The caregiver’s report of success in keeping the child away from cigarette smoke was measured using a 4-point Likert scale ranging from not at all to very successful. The total number of hours spent indoors per day during the past 7 days was based on the caregiver’s report.
Urine Cotinine Level
Urine cotinine has a half-life of 16 to 20 hours in children,19 reflecting SHS exposure up to 24 hours after exposure.20 Urine samples (30 mL) were obtained from each child at baseline and 6 months and sent to the Centers for Disease Control and Prevention laboratories for analysis. Urine aliquots were fortified with trideuterated cotinine and hydrolyzed overnight with β-glucuronidase, after which the samples were extracted and the total cotinine concentration was measured by liquid chromatography/atmospheric pressure ionization and tandem mass spectrometry.19,20 All reported data are from runs confirmed as being in statistical control based on standard criteria.21 Coti-nine results are reported as nanograms per milliliter with a limit of detection (LOD) of 0.036 ng/mL. All cotinine values were above the LOD. Cotinine values of greater than 6.2 ng/mL were considered positive for SHS exposure.22
Indoor Air Quality Assessment
Environmental assessment of indoor air quality, the primary outcome, consisted of air sampling for fine and coarse PM (PM2.5 and PM 2.5–10, respectively) and air nicotine concentrations. Air sampling was conducted in the child’s bedroom and living room or television room because these rooms represent an indoor environment where the child spends a substantial portion of time. Continuous air sampling was conducted during the 7 days, within 2 weeks of clinic visit, using PM10 and PM2.5 4-L/min impactors (MSP Corp, St Paul, Minnesota) loaded with 37-mm, 2.0-μm pore size, Teflon polytetrafluoroethylene membrane filters with polypropylene support rings (Pall Corporation, Ann Arbor, Michigan). The PM2.5 concentrations reflect particles with an aerodynamic diameter of less than 2.5 μm that are capable of deposit in the lower airways. The 24-hour US Environmental Protection Agency (EPA) ambient PM2.5 air quality standard23 is 35 μg/m3. The PM2.5–10 fraction, coarse PM, was calculated as the difference between particles with an aerodynamic diameter of 10 and 2.5 μm, as a measure of particles deposited primarily in the upper and larger airways.24 The EPA does not regulate coarse PM fraction, and no threshold is available.
Air Nicotine Level
A passive sampling badge was placed in the child’s bedroom at 0.9 to 1.5 m (3–5 ft) above the floor. The passive air samplers consist of a sodium bisulfate–treated filter contained in a 37-mm polystyrene cassette covered with a polycarbonate filter diffusion screen.25 Nicotine content was analyzed using gas chromatography with a nitrogen phosphate detector. The LOD for the passive air nicotine badges was 0.003 μg/m3. All nicotine levels were above the LOD. We defined air nicotine levels greater than the LOD as positive for indoor SHS exposure.
Asthma Morbidity and Health Care Utilization
Frequency of symptom days and nights were based on care-giver responses to the items “In the past 2 weeks, how many days did [child] have wheezing, coughing, shortness of breath, or tightness in the chest?” and “In the past 2 weeks, how many nights did [child] wake up with cough, wheeze, shortness of breath, or chest tightness?” A response of greater than 0 on either question was counted as a symptom day. In addition, the number of slowed-activity days owing to asthma was ascertained at the baseline and 6-month interviews. Asthma severity was based on day and night symptom frequency during the past 2 weeks and the number of emergency department visits and hospitalizations in the past 6 months.6 Acute health care utilization was based on report of any emergency department or urgent care visit or hospitalization at baseline or the 6-month follow-up visit.
Adherence to Air Cleaner Use
Adherence to HEPA air cleaner use was measured in a subset of 13 households using data loggers or current meters (HOBO; MicroDAQ.com, LTD, Contoocook, New Hampshire). The meters, inserted inside the air cleaner to avoid child tampering, sense the change in electric current associated with turning the air cleaners on and off. The data loggers recorded the time and date for each on and off event. Families with adherence monitors were informed that air cleaner use was monitored.
Sample Size
Sample size estimates indicated that 40 participants in each of the 3 groups would provide 80% power at an α of .05 to detect a 50% difference in PM concentrations between any pair of groups.
STATISTICAL ANALYSIS
Baseline characteristics were compared across the groups using χ2 tests for categorical variables, the Kruskal-Wallis test for non-normally distributed continuous variables, and analysis of variance for age, which was normally distributed. Differences in exposure outcomes from baseline to 6 months were calculated and compared across the 3 treatment groups using the Kruskal-Wallis test because the differences in the exposure outcomes were right-skewed and not normally distributed. We then combined both air cleaner groups for comparison with the control group and used the Mann-Whitney test for comparison between these 2 groups. Symptom-free days (SFDs) were calculated for the baseline and 6-month measurements by subtracting the number of days of asthma symptoms during a 2-week period from 14 days. The change in SFDs from baseline to 6 months was calculated and compared across the 3 treatment groups using paired, 2-tailed t tests because the data were normally distributed. Days without slowed activity due to asthma were examined using the same approach used for SFDs. Logistic regression was used to model the relationship between acute asthma health care utilization and treatment group. A 2-sidedα<.05 was considered statistically significant. All analyses were performed using commercially available software (Stata version 11.0; StataCorp, College Station, Texas).
RESULTS
BASELINE SAMPLE CHARACTERISTICS
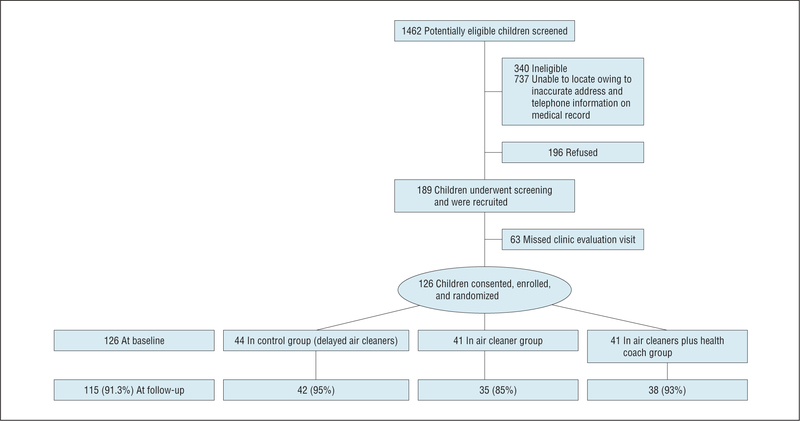
Of the 189 families screened and recruited, 126 (66.7%) consented to participate. All 126 (100.0%) completed the baseline questionnaire and were randomly assigned to the control, air cleaner, or air cleaner plus health coach groups (Figure 1). At the 6-month follow-up, 115 families (91.3%) completed questionnaire data, and high rates of interpretable air monitoring and urine cotinine data were available (PM2.5 levels, 83.3%; PM2.5–10 levels, 80.1%; air nicotine levels, 90.4%; urine cotinine levels, 96.0%). Most children were male (54.8%), African American(96.8%), and enrolled in Medicaid (89.7%) and lived with their biological mother (81.0%) (Table 1). The mean age of the children was 9.1 years. Asthma severity was high, with 79.4% children categorized as having persistent asthma (mild, 16.7%; moderate, 31.7%; and severe, 31.0%). Most children reported albuterol use within the past 2 weeks. There were no group differences for sociodemographic or health characteristics, with the exception of a slightly lower percentage of African American children in the control group and a fewer number of SFDs for the air cleaners plus health coach group (Table 1). There were no differences by child age, race/ethnicity, sex, or Medicaid status between the participants completing the follow-up and those unavailable for follow-up. Baseline mean PM2.5, air nicotine, and urine cotinine concentrations are given in Table 1.
Figure 1.
Participant recruitment and retention flowchart.
Table 1.
Baseline Sociodemographic, Health, and Environmental Characteristics by Groupa
| Control Group (n=44) |
Air Cleaner Group (n=41) |
Air Cleaner Plus Health Coach Group (n=41) |
|
|---|---|---|---|
| Sociodemographic characteristics | |||
| Male sex | 22 (50) | 24 (59) | 23 (56) |
| Child age, mean (SD), y | 9.2 (2.2) | 9.0 (1.9) | 8.9 (1.5) |
| African American raceb | 41 (93) | 41 (100) | 40 (98) |
| Child’s health insurance | |||
| Medicaid or public insurance | 39 (89) | 36 (88) | 38 (93) |
| Private | 4 (9) | 4 (10) | 3 (7) |
| Other | 1 (2) | 1 (2) | 0 |
| Caregiver | |||
| Birth mother | 36 (82) | 32 (78) | 34 (83) |
| Birth father | 1 (2) | 2 (5) | 2 (5) |
| Grandmother/legal guardian/other | 7 (16) | 7 (17) | 5 (12) |
| Marital status, caregiver | |||
| Single | 30 (68) | 31 (78) | 29 (71) |
| Married | 9 (22) | 8 (20) | 10 (24) |
| Separated/divorced/widowed | 5 (11) | 1 (3) | 2 (5) |
| Caregiver educational status | |||
| <High school degree | 18 (41) | 13 (33) | 12 (30) |
| High school graduate/GED | 20 (45) | 22 (55) | 22 (55) |
| Some college/college graduate/vocational | 6 (14) | 5 (13) | 6 (15) |
| Caregiver employed full- or part-time | 16 (36) | 23 (58) | 19 (48) |
| Health characteristics | |||
| Asthma severity | |||
| Intermittent | 11 (25) | 8 (20) | 7 (17) |
| Mild persistent | 7 (16) | 8 (20) | 6 (15) |
| Moderate persistent | 12 (27) | 13 (32) | 15 (37) |
| Severe persistent | 14 (32) | 12 (29) | 13 (32) |
| Any acute health care event in past 6 moc | 25 (57) | 28 (68) | 27 (66) |
| SFDs in past 14 d, mean (SD) | 12.3 (2.0) | 11.1 (3.5) | 10.6 (3.5) |
| Slowed-activity SFDs in past 14 d, mean (SD) | 11.9 (3.3) | 10.1 (5.1) | 10.3 (4.4) |
| Symptom-free nights in past 14 d, mean (SD) | 12.3 (3.5) | 11.7 (4.3) | 12.0 (2.9) |
| Indoor air components, mean (SD) | |||
| PM2.5 level, μg/m3 | 39.5 (24.1) | 33.9 (26.4) | 45.4 (34.7) |
| PM2.5–10 level, μg/m3 | 17.5 (13.7) | 18.8 (16.2) | 21.5 (13.4) |
| Air nicotine concentration, μg/m3 | 1.8 (2.8) | 1.1 (1.6) | 1.4 (1.7) |
| Urine cotinine concentration, ng/mL | 26.0 (30.4) | 20.0 (27.5) | 22.1 (20.2) |
Abbreviations: GED, General Educational Development; PM2.5, particulate matter with an aerodynamic diameter of less than 2.5 μm; PM2.5–10, particulate matter with a difference between particles with an aerodynamic diameter of 10 and 2.5 μm; SFD, symptom-free day.
Kruskal-Wallis tests were used to compare continuous variables between groups with the exception of age, which was normally distributed. Analysis of variance was performed for differences by group for age, and χ2 tests were used to compare categorical variables between groups. Unless otherwise indicated, data are expressed as number (percentage) of 126 children. Percentages have been rounded and might not total 100.
Differences between groups was P=.05. For all other differences, P>.05.
Based on report of any emergency department or urgent care visit or hospitalization.
COMPARISON OF HOUSEHOLD SMOKING BEHAVIOR AT BASELINE AND FOLLOW-UP BY GROUP
The caregiver was the predominant household smoker at baseline (68.3%) and follow-up (60.9%), a finding that did not differ by group. Children randomized into the control group had caregivers who smoked significantly more cigarettes at baseline and follow-up compared with children in either air cleaner group. Caregivers reported a median of 2 quit attempts during their lifetime at baseline, and attempts did not differ by air cleaner group. Almost one-half (46.0%) of caregivers reported smoking in their bedroom at baseline, which decreased to 30.4% at follow-up but did not differ by group (Table 2). Children spent most time indoors (mean, 20.3 h/d), and differences of time spent indoors between baseline and 6 months did not differ by group (P=.90). Success in keeping their child away from cigarette smoke was reported by a significantly higher number of caregivers in the air cleaner groups at follow-up (Table 2). Almost all caregivers reported at baseline and follow-up that they tried keeping their child away from cigarette smoke (baseline, 98.4%; follow-up, 100.0%).
Table 2.
Comparison of Differences in Household Smoking Characteristics Between Baseline and Follow-up by Group
| Household Smoking Characteristic | Baseline (n=126) |
Follow-up (n=115) |
P Valuea | |
|---|---|---|---|---|
| Caregiver is smoker,b No. (%) | ||||
| Control group | 33 (75) | 28 (67) | ||
| Air cleaner group | 23 (56) | 18 (51) | .73 | |
| Air cleaner plus health coach group | 30 (73) | 24 (63) | ||
| No. of cigarettes smoked by caregiver per day,c median (IQR) | ||||
| Control group | 10 (5–12) | 10 (5–10) | ||
| Air cleaner group | 6 (3–10) | 7 (5–10) | .05 | |
| Air cleaner plus health coach group | 7 (3–10) | 5 (3–7) | ||
| No. of cigarettes smoked in the home,c median (IQR) | ||||
| Control group | 6 (3–10) | 4.5 (2–5.5) | ||
| Air cleaner group | 3 (2–6) | 2 (0–5) | .34 | |
| Air cleaner plus health coach group | 3 (2–5) | 1 (0–4) | ||
| Smoking in caregiver bedroom,b No. (%) | ||||
| Control group | 24 (55) | 17 (40) | ||
| Air cleaner group | 14(34) | 9 (26) | .13 | |
| Air cleaner plus health coach group | 20 (49) | 9 (24) | ||
| Caregiver report successful or very successful in keeping child away from cigarette smoke,b No. (%) | ||||
| Control group | 31 (70) | 33 (79) | ||
| Air cleaner group | 30 (73) | 33 (94) | .47 | |
| Air cleaner plus health coach group | 31 (76) | 37 (97) |
Abbreviation: IQR, interquartile range.
Based on differences between baseline and follow-up.
Based on χ2 test.
Kruskal-Wallis rank sum tests were used to compare variables among the 3 groups.
INDOOR AIR QUALITY AND URINE COTININE ASSESSMENTS
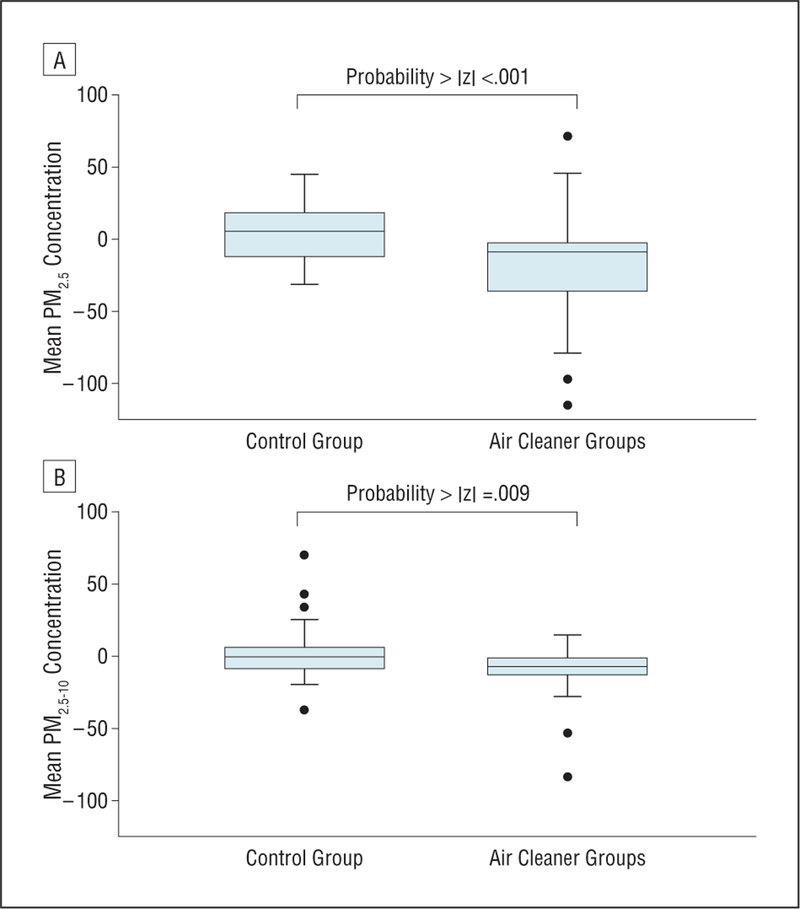
At follow-up, both air cleaner groups had significant decreases in mean differences in PM2.5 and PM2.5–10 concentrations, whereas the control PM concentrations remained unchanged (Table 3). The health coach provided no additional reduction in PM concentrations when we compared the 2 air cleaner groups (Table 3). Comparison of the combined air cleaner groups and the control group indicated that the combined air cleaner groups had significant mean differences in PM2.5 and PM2.5–10 levels from baseline to follow-up (mean differences for PM2.5: control, 3.5 [SD, 20.0]; combined air cleaner groups, −18.0 [SD, 33.2; P<.001]; and for PM2.5–10: control, 2.4 [SD,20.8]; combined air cleaner groups, −9.6 [SD, 16.0; P=.009]) (Figure 2). No significant differences were noted in air nicotine or urine cotinine concentrations between baseline and follow-up by group (Table 3). Adherence to air cleaner use was moderate, with air cleaner use logged at a mean of 106.7 (SD, 52.5) of 180 days (59.3%) in the subset of households with data loggers.
Table 3.
Follow-up Air Quality Measurements by Group
| Measure | Control Group (n=42) |
Air Cleaner Group (n=35) |
Air Cleaner Plus Health Coach Group (n=38) |
P Value | |
|---|---|---|---|---|---|
| PM2.5 level, μg/m3 | |||||
| Mean(SD) (n = 96) | 38.9 (25.0) | 17.9 (15.2) | 32.2 (30.1) | .003 | |
| Differencea (n = 86) | 3.5 (20.0) | −19.9 (28.2) | −16.1 (38.2) | ||
| PM2.5–10 level, μg/m3 | |||||
| Mean(SD) (n = 92) | 18.0 (15.8) | 11.0 (7.4) | 13.5 (10.1) | .02 | |
| Differencea (n = 78) | 2.4 (20.8) | −8.7 (17.4) | −10.6 (14.7) | ||
| Air nicotine concentration, μg/m3 | |||||
| Mean(SD) (n = 103) | 1.4 (2.04) | 0.9 (1.7) | 0.9 (1.1) | .94 | |
| Differencea (n = 93) | −0.4 (2.31) | −0.3 (1.9) | −0.6 (1.8) | ||
| Urine cotinine concentration, ng/mL | |||||
| Mean(SD)(n = 115) | 24.3 (27.4) | 18.8 (24.1) | 22.0 (28.9) | .85 | |
| Differencea (n = 110) | −2.0 (26.6) | −2.4 (35.4) | −1.4 (25.6) |
Abbreviations: PM2.5, particulate matter with an aerodynamic diameter of less than 2.5 μm; PM2.5–10, particulate matter with a difference between particles with an aerodynamic diameter of 10 and 2.5 μm.
Indicates mean 6-month concentration minus the baseline concentration. Kruskal-Wallis tests were used to compare differences among the 3 groups.
Figure 2.
Box plots for mean differences in fine (aerodynamic diameter of <2.5 μm) and coarse (difference between particles with an aerodynamic diameter of 10 and 2.5 μm) particulate matter (PM2.5 and PM2.5–10, respectively) concentrations from the 6-month follow-up, minus the baseline concentrations in the control compared with both air cleaner groups. We used the Mann-Whitney test to compare the change in PM concentrations between groups. The horizontal line in the middle of each box indicates the median, while the top and bottom borders of the box mark the 75th and 25th percentiles, respectively. The whiskers above and below the box mark the maximum and minimum values or 1.5 times the interquartile range. The points beyond the whiskers are outliers.
COMPARISON OF ASTHMA MORBIDITY AND HEALTH CARE UTILIZATION
The air cleaner plus health coach group reported the highest increase in SFDs between baseline and 6 months, although this did not reach statistical significance (P=.09) (Table 4). Differences in SFDs for slowed activity or night symptoms did not differ by group between baseline and follow-up. After combining the air cleaner groups, children assigned to those groups had a significant increase in SFDs during the past 2 weeks (1.36 SFDs) compared with 0.24 SFDs for control group children from baseline to follow-up. A trend of having an increase in slowed-activity SFDs was noted in the air cleaner groups compared with the control group (air cleaner groups, 1.76 SFDs; control group, 0.25 SFDs [P=.06]). There were no differences between the combined air cleaner groups compared with the control group at follow-up for symptom-free nights (P=.14) or for any acute asthma health care event during the past 6 months (odds ratio, 1.3; 95% confidence interval, 0.6–2.9).
Table 4.
Differences in SFDs, Slowed-Activity Days, and Symptom-Free Nights During Past 2 Weeks by Group
| Symptom | Differencea in SFDs During Past 2 wk, Mean (SD) | P Value | |
|---|---|---|---|
| Daytime wheeze, cough, chest tightnessb | |||
| Control group | −0.24 (3.0) | ||
| Air cleaner group | 1.06 (3.4) | .09 | |
| Air cleaner plus health coach group | 1.63 (4.8) | ||
| Slowed-activity daysb | |||
| Control group | 0.25 (3.2) | ||
| Air cleaner group | 2.24 (5.2) | .12 | |
| Air cleaner plus health coach group | 1.32 (5.2) | ||
| Nocturnal wheeze, cough, chest tightnessb | |||
| Control group | −0.03 (4.3) | ||
| Air cleaner group | 1.21 (4.5) | .34 | |
| Air cleaner plus health coach group | 1.25 (3.9) |
Abbreviation: SFDs, symptom-free days.
Indicates mean 6-month concentration minus the baseline concentration.
Analysis of variance was used to compare mean differences in SFDs.
COMMENT
Use of air cleaners in the homes of children with asthma residing with a household smoker significantly diminished fine and coarse PM concentrations compared with homes with no air cleaners. Moreover, children residing in homes with air cleaners experienced a significant increase in SFDs (1.36 in 2 weeks), yielding an additional 33 SFDs per year. Because smoking is a dominant contributor to indoor fine PM levels26 and increases PM2.5 levels by 25 to 45 μg/m3, 7,8,26 the reduction of 16 to 20 μg/m3 in PM2.5 levels in homes with air cleaners at 6 months indicates a significant reduction in fine particles in these homes, although not to the concentrations reported in children residing in homes without smokers27 or below the 24-hour EPA standards for outdoor air quality (35 μg/m3).23 However, our reductions in PM2.5 concentrations were similar to those of other studies of inner-city homes of children with asthma exposed to SHS.28,29
The addition of an intensive health coach intervention provided no additional reduction in PM concentrations or health effects compared with the air cleaner-only group and is in contrast to previous randomized controlled trials of behavioral SHS reduction interventions.17,30–32 Our primary focus for the health coach was tailoring the SHS reduction intervention to the parents’ readiness and motivation for SHS reduction in the home. However, many caregivers reportedly fail to achieve smoking cessation.18 Moreover, caregivers in the control and air cleaner plus health coach groups had a poor perception of their child’s exposure to SHS, based on the discordance between caregiver report of high success in keeping their child away from SHS and the follow-up PM concentrations at or above US EPA 24-hour standards.
Use of the air cleaners was not associated with significant reductions in air nicotine or urine cotinine concentrations, although mean concentrations were high (air nicotine, >0.003 μg/m3; urine cotinine, >6.2 ng/mL). The air cleaners may have been less effective in reducing the gas-vapor nicotine than they were in reducing PM. Although the air filters used in this study included a charcoal filter to remove certain gaseous contaminants and a HEPA filter to remove particulate contaminants, charcoal has been suggested to be a poor nicotine absorbent.33,34 Thus, the improvement in symptoms was most likely associated with the reduction in PM concentrations rather than with the reduction in nicotine exposure, consistent with other reports35 suggesting that the nonnicotine particle-bound components of tobacco smoke are the major contributors to increased risk of systemic inflammatory diseases.
Furthermore, the significant improvement in health effects was most likely associated with the significant reduction in PM levels owing to air cleaner placement compared with a change in household smoking behavior. McCormack et al36 noted a 6% increase in the number of days of cough, wheeze, or chest tightness for every 10-μg/m3 increase in indoor coarse PM levels in a comparable sample of preschool children with asthma. Deposition of coarse PM in the airways and subsequent bronchial hyperreactivity may be the underlying mechanism for respiratory symptoms.26,36 Our rate of increase of 33 SFDs/y was comparable to the number of SFDs reported in previous inner-city asthma studies that also used HEPA air cleaners in homes with smokers, pets, or mold problems37 but higher than the number of SFDs achieved in a clinic- and home-based asthma educational and family support intervention.38 The 14% to 18% increase in SFDs observed in our study is similar to the 20% increase seen in a clinical trial39 of leukotriene modifiers but less costly. Our data suggest that use of 2 HEPA air cleaners at a retail cost of approximately $200 to $400 may have an efficacy similar to that of leukotriene modifiers, at an approximate cost of $1200 to $1500 per year.40
Our study has a number of limitations. Room size, number of windows, air volume, and ventilation of the household were not measured and may have influenced the follow-up PM and air nicotine levels. Adherence to air cleaner use was not objectively measured in all homes, but in a subset, air cleaner use was moderate at more than half the study days. In addition, we were unable to account for all SHS exposures outside the home. We purposely enrolled low-income urban children with asthma who live in homes with adult smokers to detect a difference between intervention groups. However, this limits the generalizability of results to nonurban children or children living in nonsmoking homes. In addition, the modest sample size may limit our findings. Finally, the 6-month follow-up does not allow long-term evaluation of reduction in indoor PM concentrations or the sustainability of air cleaner use in inner-city families.
CONCLUSIONS
Use of air cleaners in homes of children with asthma was associated with a significant reduction in indoor PM concentrations and increase in SFDs. However, the reduced indoor PM levels were not sufficiently decreased to meet EPA standards for outdoor air quality. Although our results indicate that air cleaners are effective at lowering PM concentrations, they are not 100% effective. There is no known threshold for PM-inducing health effects in children with asthma. In addition, it is a tenet of public health practice that eliminating a source of contaminant is better than reducing it through an engineering control. As a result, implementing a smoke-free home policy should be considered, particularly in the homes of children with asthma.
Acknowledgments
Financial Disclosure: None reported.
Funding/Support: This study was supported by grant E09606 from the National Institute of Environmental Health Science, National Institutes of Health; by grant P01 R-826724 from the Environmental Protection Agency; and by The Johns Hopkins Center for Childhood Asthma in the Urban Environment.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Trial Registration: clinicaltrials.gov Identifier: NCT00466024
REFERENCES
- 1.Schuster MA, Franke T, Pham CB. Smoking patterns of household members and visitors in homes with children in the United States. Arch Pediatr Adolesc Med. 2002;156(11):1094–1100. [DOI] [PubMed] [Google Scholar]
- 2.Winickoff JP, Berkowitz AB, Brooks K, et al. ; Tobacco Consortium, Center for Child Health Research of the American Academy of Pediatrics. State-of-the-art interventions for office-based parental tobacco control. Pediatrics. 2005;115(3):750–760. [DOI] [PubMed] [Google Scholar]
- 3.Delva J, Tellez M, Finlayson TL, et al. Cigarette smoking among low-income African Americans: a serious public health problem. Am J Prev Med. 2005;29(3): 218–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berman BA, Wong GC, Bastani R, et al. Household smoking behavior and ETS exposure among children with asthma in low-income, minority households. Addict Behav. 2003;28(1):111–128. [DOI] [PubMed] [Google Scholar]
- 5.Oddoze C,Dubus JC,Badier M,et al. Urinarycotinineandexposuretoparentalsmoking in a population of children with asthma. Clin Chem. 1999;45(4):505–509. [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services. National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program, Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health; 2007. NIH publication 07–4051. [Google Scholar]
- 7.Abt E, Suh HH, Allen G, Koutrakis P. Characterization of indoor particle sources: a study conducted in the metropolitan Boston area. Environ Health Perspect. 2000; 108(1):35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wallace LA, Mitchell H, O’Connor GT, et al. ; Inner-City Asthma Study. Particle concentrationsininner-cityhomesofchildrenwithasthma:theeffectofsmoking, cooking, and outdoor pollution. Environ Health Perspect. 2003;111(9):1265–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thatcher TL, Layton DW. Deposition, resuspension and penetration of particles within a residence. Atmos Environ. 1995;29(12):1487–1497. [Google Scholar]
- 10.Church DF, Pryor WA. Free-radical chemistry of cigarette smoke and its toxico-logical implications. Environ Health Perspect. 1985;64(12):111–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scian MJ, Oldham MJ, Miller JH, Kane DB, Edmiston JS, McKinney WJ. Chemical analysis of cigarette smoke particulate generated in the MSB-01 in vitro whole smoke exposure system. Inhal Toxicol. 2009;21(12):1040–1052. [DOI] [PubMed] [Google Scholar]
- 12.Batterman S, Godwin C, Jia C. Long duration tests of room air filters in cigarette smokers’ homes. Environ Sci Technol. 2005;39(18):7260–7268. [DOI] [PubMed] [Google Scholar]
- 13.Hacker DW, Sparrow EM. Use of air-cleaning devices to create airborne particle-free spaces intended to alleviate allergic rhinitis and asthma during sleep. Indoor Air. 2005;15(6):420–431. [DOI] [PubMed] [Google Scholar]
- 14.Cheng YS, Lu JC, Chen TR. Efficiency of a portable indoor air cleaner in removing pollens and fungal spores. Aerosol Sci Technol. 1998;29(2):92–101. doi: 10.1080/02786829808965554. [DOI] [Google Scholar]
- 15.Myatt TA, Minegishi T, Allen JG, MacIntosh D. Control of asthma triggers in indoor air with air cleaners: a modeling analysis. Environ Health. 2008;7:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Society of Heating, Refrigerating and Air-Conditioning Engineers. Environmental tobacco smoke: position document approved by ASHRAE Board of Directors. June 2005. http://www.ashrae.org/pressroom. Accessed November 23, 2010. [Google Scholar]
- 17.Wilson KM, Klein JD, Blumkin AK, Gottlieb M, Winickoff JP. Tobacco-smoke exposure in children who live in multiunit housing. Pediatrics. 2011;127(1):85–92. [DOI] [PubMed] [Google Scholar]
- 18.Emmons KM, Hammond SK, Fava JL, Velicer WF, Evans JL, Monroe AD. A randomized trial to reduce passive smoke exposure in low-income households with young children. Pediatrics. 2001;108(1):18–24. [DOI] [PubMed] [Google Scholar]
- 19.Bernert JT Jr, Turner WE, Pirkle JL, et al. Development and validation of sensitive method for determination of serum cotinine in smokers and nonsmokers by liquid chromatography/atmospheric pressure ionization tandem mass spectrometry. Clin Chem. 1997;43(12):2281–2291. [PubMed] [Google Scholar]
- 20.Bernert JT, Harmon TL, Sosnoff CS, McGuffey JE. Use of continine immunoassay test strips for preclassifying urine samples from smokers and nonsmokers prior to analysis by LC-MS-MS. J Anal Toxicol. 2005;29(8):814–818. [DOI] [PubMed] [Google Scholar]
- 21.Caudill SP, Schleicher RL, Pirkle JL. Multi-rule quality control for the age-related eye disease study. Stat Med. 2008;27(20):4094–4106. [DOI] [PubMed] [Google Scholar]
- 22.Repace JL, Lowrey AH. An enforceable indoor air quality standard for environmental tobacco smoke in the workplace. Risk Anal. 1993;13(4):463–475. [DOI] [PubMed] [Google Scholar]
- 23.US Environmental Protection Agency. National Ambient Air Quality for Standards for PM2.5 (NAAQS). 2007. http://www.epa.gov/air/data. Accessed May 14, 2011. [Google Scholar]
- 24.Brunekreef B, Forsberg B. Epidemiological evidence of effects of coarse airborne particles on health. Eur Respir J. 2005;26(2):309–318. [DOI] [PubMed] [Google Scholar]
- 25.Hammond SK, Leaderer BP. A diffusion monitor to measure exposure to passive smoking. Environ Sci Technol. 1987;21(5):494–497. [DOI] [PubMed] [Google Scholar]
- 26.Breysse PN, Diette GB, Matsui EC, Butz AM, Hansel NN, McCormack MC. Indoor air pollution and asthma in children. Proc Am Thorac Soc. 2010;7(2):102–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Deusen A, Hyland A, Travers MJ, et al. Secondhand smoke and particulate matter exposure in the home. Nicotine Tob Res. 2009;11(6):635–641. [DOI] [PubMed] [Google Scholar]
- 28.Simons E, Curtin-Brosnan J, Buckley T, Breysse P, Eggleston PA. Indoor environmental differences between inner city and suburban homes of children with asthma. J Urban Health. 2007;84(4):577–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eggleston PA, Butz A, Rand C, et al. Home environmental intervention in inner-city asthma: a randomized controlled clinical trial. Ann Allergy Asthma Immunol. 2005;95(6):518–524. [DOI] [PubMed] [Google Scholar]
- 30.Wahlgren DR, Hovell MF, Meltzer SB, Hofstetter CR, Zakarian JM. Reduction of environmental tobacco smoke exposure in asthmatic children: a 2-year follow-up. Chest. 1997;111(1):81–88. [DOI] [PubMed] [Google Scholar]
- 31.Hovell MF, Zakarian JM, Matt GE, Hofstetter CR, Bernert JT, Pirkle J. Effect of counselling mothers on their children’s exposure to environmental tobacco smoke: randomised controlled trial. BMJ. 2000;321(7257):337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hovell MF, Meltzer SB, Wahlgren DR, et al. Asthma management and environmental tobacco smoke exposure reduction in Latino children: a controlled trial. Pediatrics. 2002;110(5):946–956. [DOI] [PubMed] [Google Scholar]
- 33.Wampler DA, Miller-Leiden S, Nazaroff WW, et al. Effectiveness of smokeless ashtrays. J Air Waste Manag Assoc. 1995;45(6):494–500. [DOI] [PubMed] [Google Scholar]
- 34.Coggins CR, Gaworski CL. Could charcoal filtration of cigarette smoke reduce smoking-induced disease? a review of the literature. Regul Toxicol Pharmacol. 2008;50(3):359–365. [DOI] [PubMed] [Google Scholar]
- 35.Carlens C, Hergens MP, Grunewald J, et al. Smoking, use of moist snuff, and risk of chronic inflammatory diseases. Am J Respir Crit Care Med. 2010;181(11):1217–1222. [DOI] [PubMed] [Google Scholar]
- 36.McCormack MC, Breysse PN, Matsui EC, et al. ; Center for Childhood Asthma in the Urban Environment. In-home particle concentrations and childhood asthma morbidity. Environ Health Perspect. 2009;117(2):294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kattan M, Stearns SC, Crain EF, et al. Cost-effectiveness of a home-based environmental intervention for inner-city children with asthma. J Allergy Clin Immunol. 2005;116(5):1058–1063. [DOI] [PubMed] [Google Scholar]
- 38.Krieger J, Takaro TK, Song L, Beaudet N, Edwards K. A randomized controlled trial of asthma self-management support comparing clinic-based nurses and in-home community health workers: the Seattle-King County Healthy Homes II Project. Arch Pediatr Adolesc Med. 2009;163(2):141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sorkness CA, Lemanske RF Jr, Mauger DT, et al. ; Childhood Asthma Research and Education Network of the National Heart, Lung, and Blood Institute. Long-term comparison of 3 controller regimens for mild-moderate persistent childhood asthma: the Pediatric Asthma Controller Trial. J Allergy Clin Immunol. 2007; 119(1):64–72. [DOI] [PubMed] [Google Scholar]
- 40.Estimated cost of 30 day supply of Singulair. https://online.epocrates.com/noFrame/showPage.do?method=drugs&MonographId=1238&ActiveSectionId=6. Accessed April 12, 2011. [Google Scholar]