Abstract
The human papillomavirus (HPV) is a sexually transmitted infection and causes most oropharyngeal (e.g., throat) and anogenital (e.g., anal, cervical) cancers. Research indicates low knowledge about the link between HPV and cancer among the general population, and similar low knowledge of HPV among individuals diagnosed with HPV-associated cancers. This is important because HPV status can have implications for treatment, prognosis, and future sexual decisions. Using a health literacy framework, this study explored how patients diagnosed with HPV-associated cancers accessed, understood, appraised, and applied HPV information. We conducted 27 in-depth interviews with patients seeking care at a comprehensive cancer center; and data were analyzed using applied thematic analysis. Findings revealed that patients’ primary source of HPV information was medical providers (access); and many patients exhibited limited understanding of HPV and its role in their cancer diagnosis (understand). Most patients (17 of 27) did not mention HPV as the cause of their cancer. Many patients displayed difficulty connecting HPV with their lifestyles (appraise); and few discussed plans to engage in HPV prevention practices going forward (apply). Future research should focus on strategies to improve understanding of HPV which could increase vaccine uptake, reduce stigma, and enhance informed decision-making among HPV-associated cancer patients.
Introduction
The human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States (US) (Satterwhite et al., 2013), and is known to cause most oropharyngeal (including throat and base of tongue) and anogenital (including anal, vulvar, vaginal, cervical, and penile) cancers (Chaturvedi et al., 2011; Jemal et al., 2013; & Markowitz et al., 2014). In the US, over 30,000 cancers are attributed to HPV annually (Viens et al., 2016). Moreover, the estimated HPV-associated cancer incidence increased from 10.8 per 100,000 during 2004–2008 to 11.7 per 100,000 during 2008–2012 (Viens et al., 2016; Wu et al., 2012).
Currently, the HPV vaccine is a recommended prevention mechanism for most of these cancers (National Center for Immunization and Respiratory Diseases, 2017). Recent promotion of the HPV vaccine has resulted in increased media coverage about the link between HPV and cancer (Shepherd & Gerend, 2014), mainly cervical cancer. However, only 62% of the American public reports know about the causal link between HPV and cervical cancer (Blake et al., 2015). Additionally, a recent systematic review found that the general public showed relatively low knowledge about the connection between HPV and head and neck cancer (Dodd, Waller, & Marlow, 2016). Furthermore, research using national data indicates that among the general population, knowledge of the association between HPV and other HPV-associated cancers was even lower than knowledge of the link between HPV and cervical cancer (McBride & Singh, 2017).
Limited knowledge about the link between HPV and cancer also exists among individuals diagnosed with HPV-associated cancers. A patient’s HPV status can have implications for their cancer treatment plan and/or prognosis in certain cancer types (Marur, D’Souza, Westra, & Forastiere, 2010). For example, HPV-associated oropharyngeal cancers are significantly more responsive to certain treatment regimens compared to tobacco-associated oropharyngeal cancers (Rutter, Husain, & Burtness, 2015). Additionally, patients should be aware of their HPV status as it may influence future sexual health decisions for themselves and their families, including conversations with current sexual partners (Dodd, Marlow, & et al., 2016b). For these reasons, it is imperative that medical providers involved in the diagnosis and treatment of HPV-associated cancers be prepared to discuss HPV status with patients. A pilot study conducted by Pils et al. (2014) found that in comparison to women with non-HPV related cancers, women with HPV-associated cancers (i.e., cervical, vulvar or vaginal) reported similar low knowledge of the term “HPV” (Pils et al., 2014). Among a sample of oral cancer patients, less than half reported that their oncologist had discussed HPV with them, and 37% said they desired more information about HPV (Milbury, Rosenthal, El-Naggar, & Badr, 2013). One study indicated that some medical providers found it difficult to discuss HPV with patients, and described it as opening a “can of worms” (McSherry et al., 2012). Furthermore, much of the educational material about HPV is focused on cancer prevention and is not targeted toward individuals who already have an HPV-associated cancer (Hendry et al., 2017). To date, very little research has been conducted to explore how patients diagnosed with an HPV-associated cancer understand the link between HPV and their cancer diagnosis.
Theoretical Framework
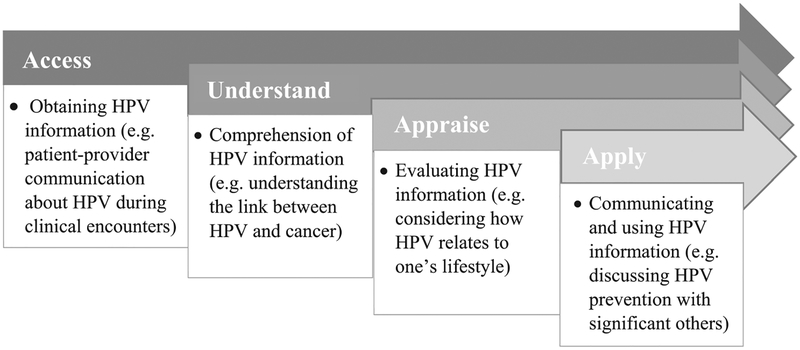
As indicated previously, research has pointed to a lack of knowledge about the link between HPV and cancer among the general population and those diagnosed with an HPV-associated cancer (Inglehart et al., 2016; Milbury et al., 2013). In addition to limited HPV knowledge, there is also a need to explore how HPV information is used to make informed decisions about health and healthcare (e.g., using condoms during sexual encounters). Thus, we consulted Sørensen et al.’s (2012) Health Literacy Model to help organize emergent themes related to patients’ understanding about the role of HPV in their cancer diagnosis. Health literacy can be defined as “people’s knowledge, motivation and competences to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course” (Sørensen et al., 2012, p. 9).
Sørensen et al.’s (2012)Health Literacy Model was chosen because it synthesizes other definitions and components of various health literacy definitions. Within this health literacy framework, access “refers to the ability to seek, find and obtain health information” (Sørensen et al., 2012, p. 9). Once individuals access health information, the next domain of health literacy involves a person’s ability to understand or comprehend that information (Sørensen et al., 2012). Next, this model indicates the importance of information appraisal, which refers to an individual’s “ability to interpret, filter, judge and evaluate the health information” (Sørensen et al., 2012, p. 9). Finally, application of health information refers to a person’s “ability to communicate and use” pertinent information to make informed health-related decisions (Sørensen et al., 2012, p. 9). In the present study, patients’ perspectives about how they accessed, understood, appraised, and applied HPV information in relation to their cancer diagnoses are explored. Figure 1 (adapted from Sørensen et al., 2012; Best et al., 2017) illustrates how Sørensen’s Health Literacy Model may be applied in the context of HPV-associated cancer information.
Figure 1.
Application of a health literacy framework to HPV-associated cancer information.
Methods
Participants and Recruitment
This study used a qualitative approach, employing one-on-one in-depth interviews among the target population. The study protocol was approved by the Institutional Review Board at the University of South Florida and the Scientific Review Committee at the Moffitt Cancer Center. From September 2016 to May 2017, 27 participants were recruited from several outpatient oncology clinics within a large NCI-designated cancer center located in a metropolitan area. Clinics included Head and Neck, Gastrointestinal, and Gynecologic Oncology. Eligible participants included men and women who were (1) 18 years of age and older; (2) diagnosed with an HPV-positive oropharyngeal (i.e., throat and base of tongue) or anogenital (i.e., anal, vulvar, cervical, and penile) cancer; (3) undergoing active definitive treatment (with curative intent); (4) able to speak and understand English, as survey instruments were available only in English; (5) never diagnosed with severe cognitive impairment; and (6) able to provide informed consent.
Potential participants were identified through an electronic health record system with permission of their treating provider; and research assistants (credentialed through the cancer center) were available in clinics to approach patients after gaining approval from their treating provider. Interested participants were provided with study details, systematically screened for eligibility, and either interviewed in-person or scheduled for a phone interview after providing consent. Interviews took an average of 39 min to complete, and ranged from 25 to 55 min. Participants were provided with a $50.00 gift card for their time.
Study Measures
Socio-demographic data were collected from each interviewed participant using a brief paper-and-pencil questionnaire, which was verbally administered by a research assistant. Socio-demographic variables included participants’ age, education level, household income, gender, sexual orientation, and marital status. A semi-structured interview guide was developed by the research team based on literature (Milbury et al., 2013; Pils et al., 2014) and input from clinicians to explore patients’ understanding of the link between HPV and their cancer diagnosis. Clinicians providing input on instrument development included oncologists practicing in the following specialties: head and neck, gynecology, and gastrointestinal (specializing in anal cancer).
Interviewers did not use the term “HPV” unless the participant used it (or a related term) first. This was decided by the research team for two main reasons: (1) researchers and clinicians felt that initiating the term could further stigmatize an already vulnerable group; and (2) in the event that a provider had not adequately discussed the patient’s HPV status with them (e.g., due to provider discomfort), the research team felt that introducing the term in the interview could prompt questions from the patient that the interviewer should not ethically answer. Therefore, the interview guide included questions designed to elicit the patients’ perspectives of what caused their cancer, and their recollections of conversations with providers about potential causes. If patients mentioned HPV (or a related term), interviewers probed more specifically about how they received information about HPV, what specifically they were told about HPV, how they felt about having an HPV-associated cancer, etc. Some pertinent questions and probes from the interview guide included: Some people report that they spend a lot of time thinking about what caused their cancer. What are some of the thoughts you have had? How do these thoughts about what caused your cancer affect how you feel about yourself? Has a medical provider ever talked to you about what may have caused your cancer? If yes, what did she/he say about it? A copy of the interview guide is included in Appendix.
Data Analysis
All interview data were digitally recorded and transcribed verbatim. The research team used the applied thematic analysis framework (Fereday & Muir-Cochrane, 2006) to analyze data. Codebook development took place using several rounds of team-based transcript analysis to ensure consensus among a primary coder and the rest of the research team (Guest, MacQueen, & Namey, 2012). The final codebook included a-priori and emergent codes based on the study’s research aims and the health literacy framework (which was incorporated after health literacy themes began to emerge). Coding decisions were discussed and finalized during research team debriefings. The primary coder kept track of all changes, rationale for changes, results of discussion, and actions taken throughout codebook revision; and the codebook was continually updated during this iterative process (Guest, MacQueen, & Namey, 2012). Data were managed using MAXQDA qualitative analysis software, version 12 (Verbi, 2017). Lastly, univariate analyses including frequencies, means, and standard deviations were conducted using SPSS version 24 (IBM Corporation, 2016) to describe socio-demographic characteristics of the sample, as well as to examine knowledge of HPV by cancer type.
Results
Demographic characteristics of the study sample are included in Table 1. Study participants ranged from age 29–79 years (M = 54.8), with over half of participants being female (55.6%). Approximately 78% of participants self-identified as non-Hispanic White or Caucasian, 15% identified as non-Hispanic Black or African-American, and 7% identified as Hispanic or Latino. The majority of the participants had some college education (30.8%) or a bachelor’s degree (26.9%). Most of the sample described themselves as straight or heterosexual in terms of sexual orientation (85.2%), while four participants (14.8%) described themselves as gay, lesbian, or homosexual. Over half of participants were either married or living with a partner (63.0%). With regard to cancer type, seven patients were diagnosed with oropharyngeal cancer (e.g., throat, base of tongue) (26.0%), 11 patients were diagnosed with anal cancer (41.0%), and nine patients were diagnosed with gynecologic cancer (i.e., cervical or vulvar) (33.0%).
Table 1.
Demographic characteristics (N = 27) *
| Characteristic | M (SD) | N (%) |
|---|---|---|
| Age (years) | 54.8(11.5) | |
| Gender | ||
| Female | 15(55.6) | |
| Male | 12(44.4) | |
| Race/ethnicity | ||
| White/Caucasian | 21(77.8) | |
| Black/African-American | 4(14.8) | |
| Hispanic/Latino | 2 (7.4) | |
| Marital status | ||
| Married/living with partner | 17(63.0) | |
| Single | 3(11.1) | |
| Divorced | 3(11.1) | |
| Widowed | 4(14.8) | |
| Sexual orientation | ||
| Straight/heterosexual | 23(85.2) | |
| Gay/lesbian/homosexual | 4(14.8) | |
| Education | ||
| High school or equivalent | 9(34.6) | |
| Some college | 8(30.8) | |
| Bachelor’s degree or higher | 9(34.6) | |
| Income (US dollars) | ||
| ≤$20,000 | 11(40.7) | |
| $20,001–40,000 | 8(29.6) | |
| >$40,001 | 8(29.6) | |
| Cancer type | ||
| Anal | 11(41.0) | |
| Gynecological | 9(33.0) | |
| Oropharyngeal | 7(26.0) | |
Missing data are not included; percentages may not total 100
Major themes which emerged during data analysis are reported within the context of the health literacy framework. Specifically, findings outline patients’ perspectives about how they accessed, understood, appraised, and applied HPV information in relation to their cancer diagnosis.
Access
Most patients in this study talked about medical providers as their main source of accessing information related to their cancer diagnosis. Very few patients mentioned following up with other sources for additional information. Only 14 of 27 patients reported having received information about the cause of their cancer from a medical provider. Among those who recalled receiving information on the cause of their cancer, only nine recalled being told about HPV. Proportionately, oropharyngeal cancer patients more frequently indicted that their medical providers talked to them about the cause of their cancer (5 of 7 or 71%). With regard to medical providers acting as a source of information about potential cancer causes, many patients reported either being unclear about the information shared, or believed providers were unsure of the cause. As a 53-year-old female patient with anal cancer described, “They don’t really have too much of an idea about how it happens either.” These patients perceived that there was little to no information available to providers regarding the cause of their cancer. A few patients reported no desire to seek information about the cause of their cancer. Only two patients reported information-seeking beyond discussion with a medical provider to learn about potential causes. For example, a 44-year-old female stated “I just typed it in. I just typed in ‘cervical cancer’ and any website out there that had anything I can read, I read.”
Understand
Many study participants mentioned feeling confused following a medical provider’s explanation of potential causes of their cancer. Seventeen of the 27 study patients reported either not knowing what caused their cancer, or they mentioned causes other than HPV. Table 2 displays the number of patients who mentioned HPV as a potential cause for their cancer by cancer type. None of the oropharyngeal cancer patients (0 of 7) mentioned the term “HPV”; and many oropharyngeal cancer patients who did speculate a potential cause mentioned smoking. Some examples of other non-HPV related causes mentioned included: genetics; diet; toothpaste; toilet seats; and occupational or outdoor exposures such as the sun and animal excrement. For example, a 56-year-old male patient diagnosed with oropharyngeal cancer reported the following:
Table 2.
Patients who mentioned HPV by cancer type
| Cancer Type | n (%) |
|---|---|
| Anal (n = 11) | 6(55) |
| Gynecological (n = 9) | 4(44) |
| Oropharyngeal (n = 7) | 0(0) |
Different things like working my head up trees—tree trailing business—probably it was something maybe from the trees or when the birds are migrating they [piss] a lot in the trees and I thought maybe being exposed to that but they said that no, that was unlikely. Because I’ve wondered different things but never have got any answer.
Even when patients knew their cancer was related to HPV, some were still unclear about the transmission of HPV, and had difficulty making the connection between HPV and sexual activity. As a 44-year-old female anal cancer patient stated,
A doctor I was sent to said, “you got cancer,” and I said, “What type of cancer?” You know, and he was telling me and then he was like, “well, you get it off toilet seats and sitting on toilets.” I’m like, “I never heard of that.” I was just kinda shocked.
Additionally, a 45-year-old cervical cancer participant said, “You don’t have to have STDs or anything to get it. It’s from a virus that everybody can get, even boys can get it. It’s kind of like almost in your body.”
Appraise
Many patients who were aware of HPV also knew that it was spread through sexual contact. However, some patients learned that their cancer was linked to sexual activity, but still did not connect that to HPV. For instance, a 54year-old female anal cancer patient described that her diagnosis was linked to sexual activity; however, she never mentioned HPV specifically, and she had difficulty understanding how she acquired this cancer through sexual activity since she had always been faithful to her spouse and assumed his fidelity to her as well. Similarly, another participant mentioned lack of certainty about her HPV status, but stated that she “didn’t have a lot of sexual partners so it couldn’t have been that.” Patients who were married or in committed relationships expressed negative thoughts regarding potential cheating or being perceived as promiscuous. A 44-year-old female described her diagnosis of anal cancer as something “homosexuals” acquired, and did not connect the disease with her lifestyle because she “never had sex back there.” Two patients, who were also positive for the human immunodeficiency virus (HIV), found it possible they were affected by HPV due to their weakened immune systems or other health complications.
Many patients that had a history of tobacco use reported being told that their cancer was caused from smoking; however, most of these patients were skeptical. These patients rejected smoking as the cause of their cancer and presented alternate explanations such as cleaning swimming pools or heavy sun exposure. A 45-year-old cervical cancer patient stated, “I know people say ‘Oh, smoking causes cancer.’ Well, you know what? I know people that have never smoked a cigarette, never tried alcohol a day in their life and had lung cancer.”
Apply
Most patients in this study did not make the connection between HPV and their cancer diagnosis; thus, there was limited discussion about how they may communicate HPV information to family and/or significant others, or how they may use this information in future health decision-making. One anal cancer patient stated that, due to “embarrassment,” he did not plan to disclose his HPV status to the person he was dating. This decision may have been unintentionally exacerbated by conversations with medical staff about HPV, in which the patient recalls, “the nurse told me, ‘don’t worry about it because’ she said ‘everyone, everyone,’ even the doctor just now said ‘virtually everyone walking the planet is exposed.’” A few female patients recalled a history of abnormal Pap tests, yet not being aware of the significance of abnormal Pap test results at the time; therefore, they were not able to apply this information to cancer prevention practices such as further testing and/or increased screening. Two patients mentioned the HPV vaccine in their description of the virus. These patients regretted that the HPV vaccine was not available to them prior to becoming infected.
Discussion
Guided by a health literacy framework (Sørensen et al., 2012), the goal of this study was to identify gaps in patients’ ability to access, understand, appraise, and apply HPV information in the context of their cancer diagnosis. Overall, findings revealed that many patients diagnosed with HPV-positive oropharyngeal and anogenital cancers exhibited limited understanding of HPV, and uncertainty about the role of HPV in their cancer diagnosis. Specifically, most patients reported limited recollection of their medical providers talking to them about HPV (access); and many displayed confusion about the cause of their cancer, or about HPV in general (understand). Moreover, some patients who did mention HPV displayed difficulty making a connection between HPV and their lifestyles (appraise). Finally, because most patients in this study did not make the connection between HPV and their cancer diagnosis, there was limited discussion about future HPV prevention practices or promotion of HPV prevention among family and friends (apply). These findings coincide with existing research in which only 35% of a sample of HPV-associated oropharyngeal cancer patients knew that HPV was the cause of their type of cancer (Milbury et al., 2013). Patients with cancer who are aware of and understand their HPV status may use this information to initiate conversations with current sexual partners, encourage eligible family members to get the HPV vaccine, and/or use condoms during future sexual encounters.
Our findings indicate that patients’ understanding of cancer in general was limited, and this may contribute to confusion when speculating cause. Throughout interviews, patients spoke in general terms about cancer without distinguishing their specific cancer type. This was particularly common when patients described potential causes—anything is a potential cause of their cancer since there is so much uncertainty about cancer in general. In addition to confusion about the link between HPV and cancer, some patients also exhibited an inability to connect HPV to their own lifestyles (e.g., sexual behavior, monogamy, etc.). For example, many patients expressed disbelief about having an STI due to limited sexual partners and/or being in a monogamous relationship. Despite confusion, most patients did not report seeking further explanation on the role of HPV in their cancer diagnosis, and chose to focus only on treatment going forward. It is possible that newly diagnosed cancer patients receive so much information (mostly related to treatment and prognosis), that HPV information is lost or forgotten. Given that less intensive treatment may be recommended for some HPV-associated cancers (e.g., oropharyngeal), these patients are at reduced risk for long-term effects and are more likely to return to normal activities after treatment compared to those diagnosed with non-HPV associated cancers (Rutter et al., 2015). Therefore, ensuring that these patients are aware of and understand the implications of their HPV status is critical.
Several patients used language such as “everyone has it” without ever mentioning HPV; and in many cases, this language was used in reference to cancer. This miscommunication appears to be related to providers’ description of the pervasiveness of HPV, while some patients interpret this to mean everyone has cancer. Health literacy techniques such as AskMe3 (National Patient Safety Foundation, 2016) could be incorporated into to clinical visits in which patients are encouraged to prepare questions specifically related to HPV in advance, which could help foster more effective patient–provider communication.
Healthcare providers’ communication approaches that aim not to stigmatize patients appear to contribute to confusion. There is often stigma associated with HPV from the patient’s perspective (Daley, Vamos, Wheldon, Kolar, & Baker, 2013), coupled with medical providers’ reported difficulty discussing HPV with patients (Dodd, Marlow, et al., 2016b; McSherry et al., 2012). In an effort to not stigmatize patients, oncology providers may forgo sharing specific STI-related information. This phenomenon could also be related to some oncology providers’ discomfort discussing sex and sexual behavior with patients (McSherry et al., 2012). Effective tools to reduce discomfort during these sensitive patient–provider interactions are necessary. Presently, there are a limited number of resources available to assist oncology and other healthcare providers with discussing HPV and its association with cancer and other health conditions.
Recent research conducted by a team at Bangor University in the United Kingdom resulted in the development of various “consultation guides” to assist clinicians in discussing HPV with patients diagnosed with a range of HPV-associated cancers (Hendry et al., 2017). However, to our knowledge, there have been no studies conducted in United States involving development and rigorous testing of messages to assist with patient–provider communication about HPV and cancer. Also, resources used to train reproductive and sexual health providers may be helpful and could be adapted for oncology providers involved in diagnosis and treatment of HPV-associated cancers, as well as for other healthcare providers who have important roles in educating the general public about HPV. Future research building directly on this study should explore perceptions of oncology providers’ role in educating patients on HPV in general and its role as a causative agent of cancer.
Researchers have found that among patients with lung, breast, colorectal and prostate cancers, higher levels of health literacy corresponded with better quality of life (Halverson et al., 2015). Additionally, cancer patients with lower health literacy tend to spend less time engaging in health information-seeking behaviors, which could subsequently lead to fewer health promoting behaviors (Morris et al., 2013). Therefore, continued effort to extend our understanding of health literacy among cancer survivors is critical to improving their health and well-being. Moreover, our qualitative findings suggest that patients may struggle to understand, appraise and apply HPV-related health information; thus future research should include quantitative measures such as a cancer health literacy scale to more adequately measure health literacy among HPV-associated cancer patients (Dumenci et al., 2014).
Findings from this study should be considered within the context of certain limitations. In particular, the majority of study participants were non-Hispanic White (78%) and college educated (65%), which limits study generalizability. It is important to note that even among this highly educated sample, understanding of HPV and its connection with cancer was low. This reinforces the need for a “universal precautions” approach to health communication in which we assume that all patients may have difficulty understanding health information (Brega et al., 2015). Additionally, the sample included a number of different HPV-associated cancer types, which could be viewed as both a strength and a limitation. Given the small sample size (N = 27), variability in cancer types precludes in-depth exploration of potential differences in HPV understanding between cancer types. However, findings show that among a group of patients diagnosed with varying HPV-associated cancers, themes of confusion and miscommunication were prevalent. Finally, this study explored the issue of HPV and cancer- related health literacy from the patient’s perspective; however, additional information is required from the providers’ perspective to fully understand how to address this issue. Future research should explore perspectives about healthcare providers’ role in educating patients about HPV, and perceived facilitators and barriers to discussing HPV with cancer patients.
Conclusion
Findings from the present study highlight that patients’ primary (and often only) sources of HPV-related health information are their medical providers. Thus, it is imperative that healthcare providers should be equipped to deliver this information in a way that patients can use to make informed health decisions. Future research should involve development of resources to assist with patient–provider communication to help facilitate health literacy and informed decision-making among patients diagnosed with HPV-associated cancers. Additionally, more research is needed to develop strategies to improve patient–provider communication about HPV among the general population which could increase HPV vaccine uptake and reduce HPV-related stigma.
Funding
This work was supported by the Institutional Research from American Cancer Society [grant number 14-189-19].
APPENDIX
Interview guide
Introduction to the interview
Good morning/afternoon. My name is _____________ and I am a research assistant at the University of South Florida. First, I would like to thank you for taking the time to conduct this interview with me. Before we begin, how should I address you during this interview? Ms./Mrs._____________, or by your first name? Thank you!
We would like to understand your experiences being diagnosed with cancer and we will be asking you some questions to explore topics such as how cancer has affected you and your loved ones, and the role of religion and spirituality in your journey. This interview should take no more than one hour. Everything you share with me as well as your identity will be kept confidential. I want you to know that if you wish to stop the interview at any time, you are free to do so. We will also be audio recording this interview. Do we have your permission to record? Thank you! Do you have any questions before we begin? Great, let’s begin.
Opening Query
-
1
Question: Can you tell me a little bit about yourself?
Probe: How about your family?
Explore the psychosocial impact of oropharyngeal and anogenital cancers
-
2
Question: Tell me about your experience being diagnosed with cancer.
Probe: When were you first diagnosed with cancer?
-
3
Question: How did being diagnosed with *insert cancer type* cancer make you feel?
Probe: Anger, sadness, guilt, embarrassment, stigma [hone in on any reference to these types of feelings, and ask participant to elaborate.]
Explore the patients’ understanding of the association between HPV and cancer
-
4
Question: Some people report that they spend a lot of time thinking about what caused their cancer. What are your thoughts on the causes of your cancer?
Probe: How do these thoughts about what caused your cancer make you feel?
Probe: Has a medical provider ever talked to you about what may have caused your cancer? If yes, what did she/he say about it?
If participant mentions HPV:
Probe: How did you first receive information about HPV?
Probe: Has a medical provider ever talked to you about HPV, specifically? If yes, what did she/he say about it?
Probe: What other information have you been told/given about HPV?
Probe: How did receiving information about HPV make you feel?
Explore perceived social support and interpersonal communication
-
5
Question: Some people with *insert cancer type* cancer report problems talking about their illness with family and friends because they fear being judged. Can you describe any problems talking about your cancer?
Probe: How did your family, friends, and co-workers respond to your cancer diagnosis?
Probe: Do you have a significant other? [If yes] How did he/she respond to your diagnosis?
Probe: How do other people’s questions about or reactions to your cancer affect you?
-
6
Question: Who do you consider to be your main source of support through your experience with cancer? This could be a person or group of people.
Probe: In what ways does this person [or this group] provide support?
Probe: Is this the person [or group] you talk with most about your cancer?
Probe: Who else have you shared your diagnosis with?
-
7
Question: Is there anyone who you would not tell about your cancer? Why?
Probe: How did you decide who to tell and who not to tell? Can you walk me through that process?
Probe: If you had a different cancer (for example, breast cancer), would this still apply?
Probe: Can you describe how not talking about your cancer made you feel? [Note: You are looking for the impact of topic avoidance with this probe]
-
8
Question: Since your cancer diagnosis, can you share with me how any of your relationships may have changed?
Probe: How has your relationship with your significant other been affected by your diagnosis?
Probe: What about your friends?
Probe: What about your family?
Explore the role of religion and spirituality in coping with cancer
-
9
Question: Do you consider yourself to be spiritual, religious, both, or neither?
-
10
Question: What is the role of [use the term participant uses] in your life in general?
-
11
Question: What is the role of religion and/or spirituality in coping with *insert cancer type* cancer specifically?
Probe: In what ways have your religious/spiritual beliefs impacted the way you feel about having *insert cancer type* cancer?
Probe: Are these feelings about cancer in general or are they specific to *insert cancer type* cancer?
Probe: Have you received support from your religious organization (such as church members, pastor, etc.) as it relates to your cancer?
Probe: Do you normally seek support for problems from your religious organization? If yes, can you share with me about that?
Probe: *insert cancer type* cancer may be a sensitive topic. Is there any reason you may avoid talking with your church members or pastor about your cancer diagnosis? [If participants mention topic avoidance, ask how this avoidance makes them feel.]
Final Questions
-
12
Question: What other things do you feel are important to help other people like you deal with *insert cancer type* cancer?
-
13
Question: Is there anything else you would like to share with me before we end our discussion?
Conclusion
Thank you so much, (insert name), for taking the time to talk with me about your cancer journey. I know it may not have been easy and we really appreciate the effort you took to share with us. We will be sending you a gift card for $50. Can you confirm for me the spelling of your name and the address/number where we should send your gift card? Thank you again!
Footnotes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/uhcm.
References
- Best AL, Vamos CA, Choi SK, Thomas EL, Daley EM, & Friedman DB (2017). Increasing routine cancer screening among underserved populations through effective communication strategies: Application of a health literacy framework. Journal of Cancer Education. doi: 10.1007/s13187-017-1194-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake KD, Ottenbacher AJ, Finney Rutten LJ, Grady MA, Kobrin SC, Jacobson RM, & Hesse BW (2015). Predictors of human papillomavirus awareness and knowledge in 2013: Gaps and opportunities for targeted communication strategies. American Journal of Preventive Medicine, 48(4), 402–410. doi: 10.1016/j.amepre.2014.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brega AG, Barnard J, Mabachi NM, Weiss BD, DeWalt DA, Brach C, & West DR (2015). AHRQ health literacy universal precautions toolkit. (2nd ed.). Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Chaturvedi A, Engels E, Pfeiffer R, Hernandez BY, Xiao W, Kim E, … Gillison ML (2011). Human papillomavirus and rising oropharyngeal cancer incidence in the United States. Journal of Clinical Oncology, 29(32), 4294–4301. doi: 10.1200/JCO.2011.36.4596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley E, Vamos C, Wheldon C, Kolar S, & Baker E (2013). Negative emotions and stigma associated with a human papillomavirus test result: A comparison between human papillomavirus–Positive men and women. Journal of Health Psychology, 20, 1073–1082. doi: 10.1177/1359105313507963 [DOI] [PubMed] [Google Scholar]
- Dodd R, Waller J, & Marlow L (2016). Human papillomavirus and head and neck cancer: Psychosocial impact in patients and knowledge of the link–A systematic review. Clinical Oncology, 28(7), 421–439. doi: 10.1016/j.clon.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodd RH, Marlow LA, & Waller J (2016). Discussing a diagnosis of human papillomavirus oropharyngeal cancer with patients: An exploratory qualitative study of health professionals. Head & Neck, 38(3), 394–401. doi: 10.1002/hed.23916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumenci L, Matsuyama R, Riddle DL, Cartwright LA, Perera RA, Chung H, & Siminoff LA (2014). Measurement of cancer health literacy and identification of patients with limited cancer health literacy. Journal of Health Communication, 19(Sup2), 19, 205–224. doi: 10.1080/10810730.2014.943377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fereday J, & Muir-Cochrane E (2006). Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods, 5(1), 80–92. doi: 10.1177/160940690600500107 [DOI] [Google Scholar]
- Guest G, MacQueen KM, & Namey EE (2012). Applied thematic analysis. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Halverson JL, Martinez-Donate AP, Palta M, Leal T, Lubner S, Walsh MC, … Trentham-Dietz A (2015). Health literacy and health-related quality of life among a population-based sample of cancer patients. Journal of Health Communication, 20(11), 1320–1329. doi: 10.1080/10810730.2015.1018638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendry M, Pasterfield D, Gollins S, Adams R, Evans M, Fiander A, & Wilkinson C (2017). Talking about human papillomavirus and cancer: Development of consultation guides through lay and professional stakeholder coproduction using qualitative, quantitative and secondary data. BMJ Open Access, 7, e015413. doi: 10.1136/bmjopen-2016-015413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corporation. (2016). IBM SPSS statistics for windows, version 24.0. Armonk, NY: IBM Corp. [Google Scholar]
- Inglehart R, Taberna M, Pickard R, Hoff M, Fakhry C, Ozer E, … Gillison ML (2016). HPV knowledge gaps and information seeking by oral cancer patients. Oral Oncology, 63, 23–29. doi: 10.1016/j.oraloncology.2016.10.021 [DOI] [PubMed] [Google Scholar]
- Jemal A, Simard E, Dorell C, Noone A, Markowitz L, Kohler B, … Saslow D (2013). Annual report to the nation on the status of cancer, 1975–2009, featuring the burden and trends in human papillomavirus (hpv)–associated cancers and Hpv vaccination coverage levels. Journal of the National Cancer Institute, 105(3), 175–201. doi: 10.1093/jnci/djs491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz L, Dunne E, Saraiya M, Chesson H, Curtis C, Gee J, … Unger E (2014). Human papillomavirus vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recommendations and Reports, 63, 1–30. [PubMed] [Google Scholar]
- Marur S, D’Souza G, Westra WH, & Forastiere AA (2010). HPV-associated head and neck cancer: A virus-related cancer epidemic. Lancet Oncology, 11(8), 781–789. doi: 10.1016/S1470-2045(10)70017-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride K, & Singh S (2017). Predictors of adults’ knowledge and awareness of HPV, HPV-Associated cancers, and the HPV vaccine: Implications for health education. Health Education & Behavior. doi: 10.1177/1090198117709318 [DOI] [PubMed] [Google Scholar]
- McSherry LA, Dombrowski SU, Francis JJ, Murphy J, Martin CM, O’Leary JJ, & Sharp L (2012). ‘It’s a can of worms’: Understanding primary care practitioners’ behaviours in relation to HPV using the theoretical domains framework. Implementation Science, 7, 73. doi: 10.1186/1748-5908-7-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milbury K, Rosenthal DI, El-Naggar A, & Badr H (2013). An exploratory study of the informational and psychosocial needs of patients with human papillomavirus-associated oropharyngeal cancer. Oral Oncology, 49(11), 1067–1071. doi: 10.1016/j.oraloncology.2013.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris NS, Field TS, Wagner JL, Cutrona SL, Roblin DW, Gaglio B, … Mazor KM (2013). The association between health literacy and cancer-related attitudes, behaviors, and knowledge. Journal of Health Communication, 18(sup1), 223–241. doi: 10.1080/10810730.2013.825667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Immunization and Respiratory Diseases. (2017, August 24). HPV vaccines: vaccinating your preteen or teen. Retrieved from https://www.cdc.gov/hpv/parents/vaccine.html [Google Scholar]
- National Patient Safety Foundation. (2016, July 7). Ask me 3: good questions for your good health.Retrieved from http://www.npsf.org/?page=askme3. [Google Scholar]
- Pils S, Joura E, Winter M, Shrestha A, Jaeger-Lansky A, & Ott J (2014). What do women with gynecologic cancer know about HPV and their individual disease? A pilot study. BMC Cancer, 14, 388. doi: 10.1186/1471-2407-14-388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter CE, Husain ZA, & Burtness B (2015). Treatment de-intensification for locally advanced HPV-associated oropharyngeal cancer. American Journal of Hematology/Oncology, 11(5), 13–17. [Google Scholar]
- Satterwhite C, Torrone E, Meites E, Dunne EF, Mahajan R, Bañez Ocfemia C, & Weinstock H (2013). Sexually transmitted infections among US women and men: Prevalence and incidence estimates, 2008. Sexually Transmitted Diseases, 40(3), 187–193. doi: 10.1097/OLQ.0b013e318286bb53 [DOI] [PubMed] [Google Scholar]
- Shepherd MA, & Gerend M (2014). The blame game: Cervical cancer, knowledge of its link to human papillomavirus and stigma. Psychology & Health, 29(1), 94–109. doi: 10.1080/08870446.2013.834057 [DOI] [PubMed] [Google Scholar]
- Sørensen K, Van Den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, & Brand H (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12(1), 80. doi: 10.1186/1471-2458-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VERBI Software. (2017). MAXQDA 2018 [computer software]. Berlin, Germany: VERBI Software; Available from https://www.maxqda.com [Google Scholar]
- Viens LJ, Henley SJ, Watson M, Markowitz L, Thomas C, Thompson TD, … Saraiya M (2016). Human papillomavirus–associated cancers — United States, 2008–2012. MMWR Morbidity and Mortality Weekly Report, 65, 661–666. doi: 10.15585/mmwr.mm6526a1 [DOI] [PubMed] [Google Scholar]
- Wu X, Watson M, Wilson R, Saraiya M, Cleveland J, & Markowitz L (2012). Human papillomavirus-associated cancers-United States, 2004–2008. MMWR Morbidity and Mortality Weekly Report, 61, 258. [PubMed] [Google Scholar]