Abstract
The purpose of the present study was to investigate the influence of intermittent pneumatic compression (IPC) boot use between submaximal cycling trials on heart rate (HR) and blood lactate concentrations. Ten healthy participants (9M; 1F) performed two consecutive 60 minute rides at 60% of functional threshold power with a 30 minute rest between rides. The rest period was spent in a supine position using IPC boots (BOOT) or sitting in a similar position without boots (CON). HRs were collected every 15 minutes during cycling rides, and lactate was measured at the 30-minute mark during both rides. An identical trial was performed 7 days later with conditions (BOOT or CON) crossed. There were no between-trial differences (p > 0.05) in HR; between-trial differences were found for lactate concentrations during the second ride (3.9 ± 1.0 mmol/L BOOT vs. 2.7 ± 1.5 mmol/L CON, p < 0.05). The use of IPC boots between cycling trials as compared to laying in a supine position did not affect heart rate responses but did stimulate higher lactate concentrations during subsequent exercise.
Keywords: Cycling, heart rate drift, recovery
INTRODUCTION
Intermittent pneumatic compression (IPC) boots are currently marketed to athletic populations for the purposes of enhancing recovery responses. While mechanical compression devices have been shown to improve various clinically oriented outcomes, particularly in regard to prevention of deep vein thrombosis (15), there is limited evidence that they are of potential use in healthy or athletic populations.
Lactate concentrations were lower using IPC boots 20 minutes after a Wingate test as compared to a passive recovery (6), although no differences were found between boot use and an active recovery. Lactate was also significantly lower at 25 and 35 minutes post-repeated anaerobic exercise as compared to a sham condition, but not at 5 and 15 minute post-exercise time points (11). Conversely, no differences were reported in post-exercise lactate responses for up to 25 minutes between IPC boot use and a passive recovery following a 90-minute cycling bout designed to cause glycogen depletion (7). Also, preconditioning with IPC devices does not influence anaerobic performance or lactate during recovery (12).
Two separate investigations report that IPC boots do not enhance recovery from eccentrically biased exercise as determined by performance based indirect indicators of muscle damage (2, 3) despite a reduction in the post-eccentric exercise swelling response (2). It is worth noting that correctly sized compression wear caused a non-significant trend (p = 0.06) for decreasing cardiovascular drift during cycling exercise (10), although the modality is distinct from IPC devices.
There is indirect evidence that massage may play a role in enhancing a variety of recovery mechanisms (19), so IPC boots may act as a mechanical modality to mimic such a response. But since post-exercise lactate accumulation causes no muscular harm as previously thought, there is limited purpose in investigating means (e.g., massage) to hasten lactate removal (14) unless the modalities occur between chronologically proximal bouts of exercise. There is cause to investigate short-term outcomes related to IPC devices as criterium and track cycling racers may perform multiple exercise bouts in a single day with races occurring within an hour or less of each other.
The present study was designed to assess whether IPC boot use immediately post-cycling exercise has influence over performance related variables (e.g., heart rate drift and lactate) during a subsequent ride. It was hypothesized that IPC boot use may attenuate a predicted rise in heart rate during the second ride by minimizing the pooling of blood in the interstitial space during the rest period, although logistically blood volume alterations were unable to be measured. Likewise, lower lactate levels during the second ride after IPC boot use as compared to a control trial were expected due to greater central blood volume maintenance.
METHODS
Participants
Twelve (11 M, 1 F) trained participants were recruited for the present study from a local cycling training facility. Sample size estimation was based effect sizes reported by Hanson et al. (6) Criteria for participation included an age range of 16–60 years and an absence of signs or symptoms suggestive of cardiovascular, pulmonary, or metabolic disease as outlined by the American College of Sports Medicine. Additionally, all participants were at minimum a Category V (male) or IV (female) cyclist as defined by USA cycling. All participants provided informed consent before participating in this study, and all protocols were approved by the Sacred Heart University Institutional Review Board.
Protocol
After participants provided their age, gender, health history, and had their bodyweight accessed via a standard physician’s scale, a functional threshold power (FTP) test was performed. FTP tests are a commonly utilized, maximal effort field test and are a valid prediction tool for cycling performance (13). FTP is calculated as 95% of the mean wattage over the 20 minute testing period. All testing was performed on participants’ own bikes; they were instructed to not make any adjustments affecting their orthopedic positioning throughout the duration of the study. Testing was conducted using an indoor computerized training system (CompuTrainer, RacerMate One, version 4.0.7, Seattle, WA) calibrated with a 2.10 calibration ratio. Participants were requested to fast for four hours prior to the FTP test, and avoid any caffeine-containing beverages or products for 24 hours prior to testing.
At least seven days after the FTP test and 48 hours after any physically strenuous activity, participants returned to perform two 60 minute, steady-state rides with the rest period in between. The rest period was a 30 minute recovery period between rides in which participants either sat in a supine position (CON) or in a similar position using IPC boots (BOOT). Due to length of time required to ensure proper set-up and initiation of the IPC device, the treatment was initiated 5 minutes following the first ride. The IPC boot device (NormaTec, Newton Center, MA, USA) was set at the highest intensity of compression, equivalent to a maximum of 80 pounds of pressure in each of the various compartments. 30 seconds of pulse time per compartment were used, similar to Hanson et al. (6)
Steady-state rides were performed at 60% of FTP; wattage corresponding was held constant by the computerized training system. Participants were instructed to maintain a cadence between 90–99 revolutions per minute (RPM) and were provided continuous visual feedback for assistance. Sixty percent of FTP was the chosen intensity as professional cyclists spend the greatest duration of stage races in a moderately high intensity (50–70% VO2 max as determined by HR responses) (5). While 60% FTP does not correspond to a 60% VO2max workload, the intensity was used to ensure all rides would successfully complete both steady-state rides while displaying progressive elevations in heart rate during the second ride. Given the trained status of the participant pool, a 60% FTP workload would be approximately comparable to 60% of lactate threshold (18).
HRs were collected every 15 min during cycling rides, and lactate was measured at the 30 min mark during both rides. Heart rate (HR) was collected using a standard heart rate monitor (Polar Electro, Kempele, Finland) and lactate was measured via a Lactate Plus analyzer (Nova Biomedical Corporation, Waltham, MA, USA). Blood was drawn via finger pricks; universal precautions were employed for all blood draws. For each puncture, the site was cleaned with an alcohol swab to prevent contamination of data. The first drop of blood was also cleaned and discarded, with the second drop being used for analysis.
A second trial, performed 7 days later, was identical in design except the conditions (BOOT or CON) were reversed. As a crossover design was utilized, direct measures of performance were not assessed as a blinded condition was not logistically feasible.
As impaired plasma volume status affects both HR and lactate responses to exercise, a hydration protocol based on the National Association of Athletic Trainers’ position statement (1) was established. The night before testing, participants were instructed to consume 500 ml of water four hours prior to their expected bedtime. If they did not urinate within two hours, they were instructed to repeat the dosage. These steps were taken to attempt assurance of euhydration prior to testing the following day.
On the testing day, food or drink ingestion was prohibited after 0700 hours, with testing commencing at 0800 hours. Participants were instructed to note their pre-exercise food and beverage choices, if applicable, and mimic them to the best of their ability a week later for the alternate trial. Caffeine-containing products were not permitted during the morning of the ride until all testing procedures were complete. Participants consumed 500 ml of water during both Ride 1 and Ride 2; during the 30 minute rest period, participants consumed 250 ml of water.
Statistical Analysis
All dependent variables (i.e., HR, lactate, cadence) were tested for normality using a Shapiro-Wilk test. If data were normally distributed, a repeated measures ANOVA with a Fisher’s LSD post hoc was used to detect any significant differences. Condition order was used as a covariate. If any variable within a data set was not normally distributed, a Mann-Whitney U test was used for between-trial comparisons and Wilcoxon signed-rank tests for within-trial comparisons. Level of significance was set a priori at p < 0.05. All data were analyzed via SPSS V23.0 (IBM; Armonk, NY).
RESULTS
Ten participants (9 M, 1 F) (35 ± 13 years of age, 72.8 ± 14.2 kg) completed all testing procedures; data for the two participants who did not complete all procedures were not included in the analysis.
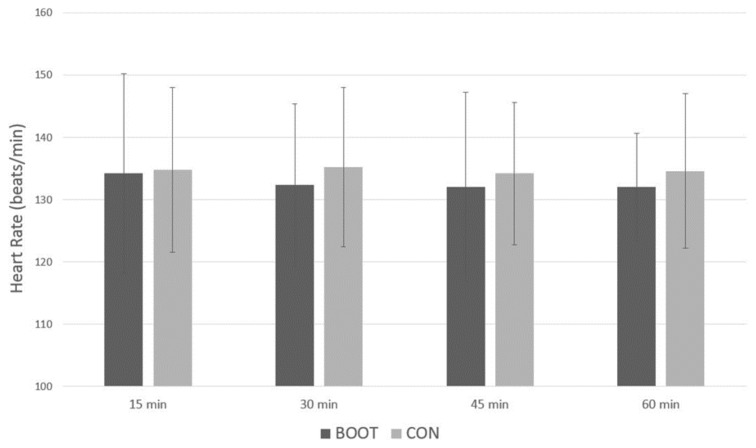
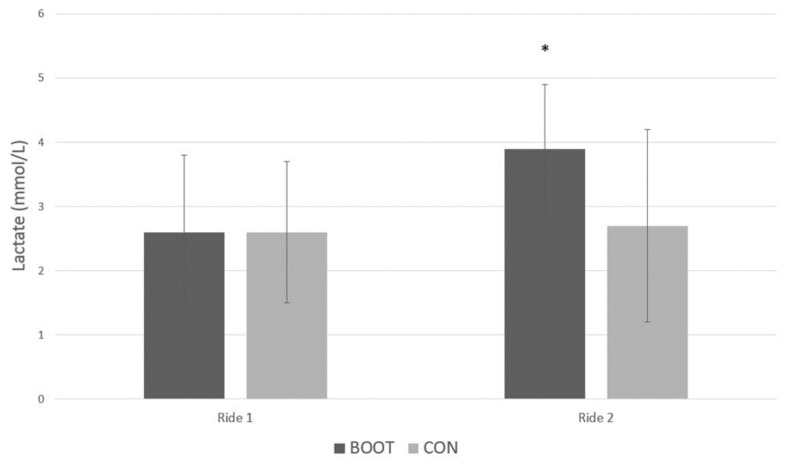
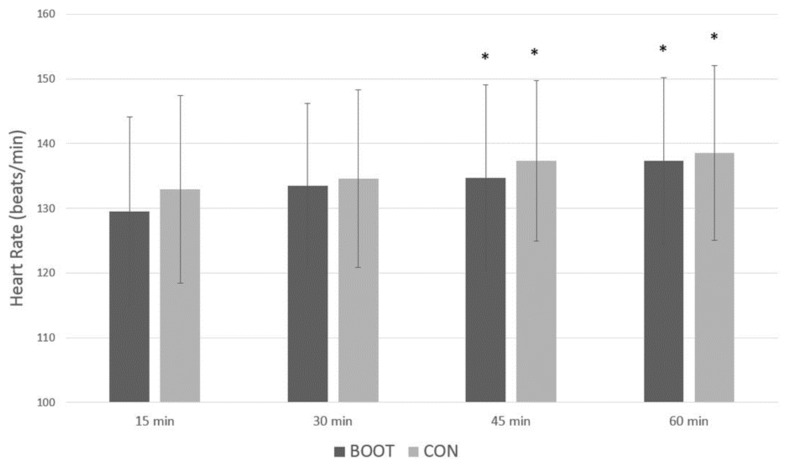
There were no significant differences (p > 0.05) in cadence between conditions or rides (BOOT Ride 1: 95.5 ± 4.6, Ride 2: 95.5 ± 3.7; CON Ride 1: 95.5 ± 4.4, Ride 2: 94.8 ± 4.4 RPM). Likewise, there were no between or within-trial differences (p > 0.05) for Ride 1 in regards to HR (Figure 1) and no between-trial difference for lactate (Figure 3). However, during Ride 2, within-trial differences occurred (p < 0.05) for HR (Figure 2) for both conditions, and a significant elevation [Z = -2.040, p = 0.041] in lactate was found (Figure 3) in the BOOT condition.
Figure 1.
Ride 1 Heart Rate Mean ± Standard Deviation. BOOT = intermittent pneumatic compression boot condition; CON = control condition; min = minute.
Figure 3.
Lactate Mean ± Standard Deviation at the 30 minute mark. BOOT = intermittent pneumatic compression boot condition; CON = control condition; * between-trial significant difference (p < 0.05) vs. Ride 1.
Figure 2.
Ride 2 Heart Rate (HR) Mean ± Standard Deviation. BOOT = intermittent pneumatic compression boot condition; CON = control condition; min = minute; * within-trial significant difference (p < 0.05) vs. 15 minute time point.
DISCUSSION
The current investigation demonstrated that use of IPC boots during rest between moderately high intensity bouts of cycling did not influence HR versus a control condition. Between-trial differences in HR and lactate would not be expected during Ride 1, and provides support of a successful control trial. The protocol was designed to ensure an upward heart rate drift during Ride 2 despite a constant workload; this intention was achieved. Furthermore, the moderate effect size (partial eta squared) of only 0.1 for between-trial differences in HR during Ride 2 suggest that a type II error did not occur in the present study despite the small sample size. As highly trained cyclists were used, clinicians should use caution when applying results from the current study to untrained populations.
Heart rate drift may have been observed in Ride 1 had HRs been collected prior to the 15-minute mark, as drift has been observed prior to 15 minutes of exercise (20); logistical constraints during data collection limited HR collection time points, providing an overall limitation to the study. Traditionally, heart rate drift is hypothesized to be the result of increased cutaneous blood flow (16). However, there is a contention that heart rate drift is due to increased HR per se as opposed to a response to a loss of central blood volume (4); if this is the case, any assistance provided by IPC devices in preventing blood pooling may not be evident in HR data during a subsequent ride.
An intriguing result was that IPC boot use promoted either an increase in lactate production or an impairment in clearance during a subsequent exercise bout. These findings are discordant from Martin et al. (12) potentially due to the differing cycling intensities employed or the limited blood sampling in the current protocol, another limitation to the present study. Lactate was not measured during the recovery period as it was deemed not only unfeasible a priori due to lack of logistical support, but also practically meaningless if a reduction in blood lactate did not carry over in some magnitude to the subsequent exercise bout itself. Investigations using more thorough temporal analysis of blood metabolites during exercise (as opposed to during recovery) following IPC use are needed.
It is uncertain why lactate was elevated during Ride 2 in the BOOT condition, but this finding is supported by a recent investigation showing higher lactate measurements during recovery from a loaded running time trial with use of compression garments (9). Greater sympathetic nervous system activation causes an increase lactate production (8). If the IPC device stimulated Group III muscle afferents (unmeasured), sympathetic drive may be upregulated in the subsequent exercise bout (17). Likewise, respiratory exchange ratios are elevated while running in compression garments without differences in core body temperature (9), indicating that compression alone may stimulate the sympathetic nervous system. To our knowledge, no study has examined autonomic function in relation to IPC use, and therefore it is ultimately unknown whether the elevation in lactate was autonomically influenced.
In conclusion, limited research demonstrates that IPC use influences performance or recovery from exercise. Our data suggest IPC use has no effect on chronotropic influences governing HR but does support the contention that use affects lactate metabolism, albeit in a different manner than often reported; more detailed temporal research is needed to better delineate hemodynamic and lactate responses during exercise following IPC use.
Many coaches or sports dieticians struggle to emphasize and implement appropriate rest and/or nutrition-related recovery strategies with certain athletes. Until further research better defines worthwhile uses of IPC devices, effectively immobilizing an athlete post-exercise via IPC boots may serve as an ideal setting to enforce recommended nutrient strategies or simply to ensure a passive recovery.
REFERENCES
- 1.Casa DJ, Armstrong LE, Hillman SK, Montain SJ, Reiff RV, Rich BS, Roberts WO, Stone JA. National athletic trainers' association position statement: fluid replacement for athletes. J Athletic Train. 2000;35:212–224. [PMC free article] [PubMed] [Google Scholar]
- 2.Chleboun GS, Howell JN, Baker HL, Ballard TN, Graham JL, Hallman HL, Perkins LE, Schauss JH, Conatser RR. Intermittent pneumatic compression effect on eccentric exercise-induced swelling, stiffness, and strength loss. Arch Phys Med Rehab. 1995;76:744–749. doi: 10.1016/s0003-9993(95)80529-x. [DOI] [PubMed] [Google Scholar]
- 3.Cochrane DJ, Booker HR, Mundel T, Barnes MJ. Does intermittent pneumatic leg compression enhance muscle recovery after strenuous eccentric exercise? Int J Sports Med. 2013;34:969–974. doi: 10.1055/s-0033-1337944. [DOI] [PubMed] [Google Scholar]
- 4.Coyle EF, Gonzalez-Alonso J. Cardiovascular drift during prolonged exercise: new perspectives. Exerc Sport Sci Rev. 2001;29:88–92. doi: 10.1097/00003677-200104000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez-Garcia B, Perez-Landaluce J, Rodriguez-Alonso M, Terrados N. Intensity of exercise during road race pro-cycling competition. Med Sci Sports Exerc. 2000;32:1002–1006. doi: 10.1097/00005768-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Hanson ESK, Li R, Thomas A. An intermittent pneumatic compression device reduces blood lactate concentrations more effectively than passive recovery after Wingate testing. J Athletic Enhancement. 2013;2 [Google Scholar]
- 7.Keck NA, Cuddy JS, Hailes WS, Dumke CL, Ruby BC. Effects of commercially available pneumatic compression on muscle glycogen recovery after exercise. J Strength Cond Res. 2015;29:379–385. doi: 10.1519/JSC.0000000000000772. [DOI] [PubMed] [Google Scholar]
- 8.Len'kova NA, Rodionov IM, Studitskaia OA. [Increase in lactic acid production in resting skeletal muscle in the presence of vasodilating sympathetic influences]. Biull Eksperimental Biol Med. 1968;66:32–34. [PubMed] [Google Scholar]
- 9.Leoz-Abaurrea I, Santos-Concejero J, Grobler L, Engelbrecht L, Aguado-JimEnez R. Running performance while wearing a heat dissipating compression garment in male recreational runners. J Strength Cond Res. 2016;30(12):3367–3372. doi: 10.1519/JSC.0000000000001467. [DOI] [PubMed] [Google Scholar]
- 10.MacRae BA, Laing RM, Niven BE, Cotter JD. Pressure and coverage effects of sporting compression garments on cardiovascular function, thermoregulatory function, and exercise performance. Eur J Appl Physiol. 2012;112:1783–1795. doi: 10.1007/s00421-011-2146-2. [DOI] [PubMed] [Google Scholar]
- 11.Martin JS, Friedenreich ZD, Borges AR, Roberts MD. Acute effects of peristaltic pneumatic compression on repeated anaerobic exercise performance and blood lactate clearance. J Strength Cond Res. 2015;29(10):2900–2906. doi: 10.1519/JSC.0000000000000928. [DOI] [PubMed] [Google Scholar]
- 12.Martin JS, Friedenreich ZD, Borges AR, Roberts MD. Preconditioning with peristaltic external pneumatic compression does not acutely improve repeated Wingate performance nor does it alter blood lactate concentrations during passive recovery compared with sham. Appl Physiol Nutr Metab. 2015;40:1214–1217. doi: 10.1139/apnm-2015-0247. [DOI] [PubMed] [Google Scholar]
- 13.Miller M. Validity of using functional threshold power and intermittent power to predict cross-country mountain bike race outcome. J Sci Cycling. 2014;3 [Google Scholar]
- 14.Moraska A. Massage and lactate clearance. Med Sci Sports Exerc. 2011;43:738. doi: 10.1249/MSS.0b013e3182078709. author reply 739. [DOI] [PubMed] [Google Scholar]
- 15.Morris RJ, Woodcock JP. Intermittent pneumatic compression or graduated compression stockings for deep vein thrombosis prophylaxis? A systematic review of direct clinical comparisons. Ann Surgery. 2010;251:393–396. doi: 10.1097/SLA.0b013e3181b5d61c. [DOI] [PubMed] [Google Scholar]
- 16.Rowell LB, Murray JA, Brengelmann GL, Kraning KK., 2nd Human cardiovascular adjustments to rapid changes in skin temperature during exercise. Circulation Res. 1969;24:711–724. doi: 10.1161/01.res.24.5.711. [DOI] [PubMed] [Google Scholar]
- 17.Tsuchimochi H, Hayes SG, McCord JL, Kaufman MP. Both central command and exercise pressor reflex activate cardiac sympathetic nerve activity in decerebrate cats. Am J Physio. 2009;296:H1157–1163. doi: 10.1152/ajpheart.01219.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valenzuela PL, Morales JS, Foster C, Lucia A, de la Villa P. Is the functional threshold power (FTP) a valid surrogate of the lactate threshold? Int J Sports Physiol Perform. 2018;13(10):1293–1298. doi: 10.1123/ijspp.2018-0008. [DOI] [PubMed] [Google Scholar]
- 19.Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35:235–256. doi: 10.2165/00007256-200535030-00004. [DOI] [PubMed] [Google Scholar]
- 20.Wingo JE, Ganio MS, Cureton KJ. Cardiovascular drift during heat stress: implications for exercise prescription. Exerc Sport Sci Rev. 2012;40:88–94. doi: 10.1097/JES.0b013e31824c43af. [DOI] [PubMed] [Google Scholar]