Abstract
Introduction
Disaster epidemiological studies indicate that Asia has the highest frequency of natural disasters. Rural communities are heavily impacted by natural disasters and have different healthcare needs to urban ones. Referencing Asian countries, this paper’s objective is to provide an overview of health impacts and the current evidence for designing programmes and policies related to rural health emergency and disaster risk management (health-EDRM).
Sources of data
This paper uses published English-only reports and papers retrieved from PubMed, Google Scholar, Embase, Medline and PsycINFO on rural disaster and emergency responses and relief, health impact and disease patterns in Asia (January 2000–January 2018).
Areas of agreement
Earthquakes are the most studied natural disasters in rural communities. The medical burden and health needs of rural communities were most commonly reported among populations of extreme age. Most of the existing research evidence for rural interventions was reported in China. There lacks published peer-reviewed reports of programme impacts on personal and community preparedness.
Areas of controversy
There is a lack of evidence-based health-EDRM interventions to evaluate implementation effectiveness in rural areas despite vast volumes of health-related disaster literature.
Growing points
Climate change-related disasters are increasing in frequency and severity. Evidence is needed for disaster risk reduction interventions to address the health risks specific to rural populations.
Areas timely for developing research
To support global policy development, urgent evidence is needed on the intervention effectiveness, long-term health outcomes, local and cultural relevance as well as sustainability of health relief produced by Health-EDRM programmes in rural areas.
Keywords: Disaster preparedness, disaster risk reduction, rural health, natural disasters, Asia, health-EDRM
Introduction
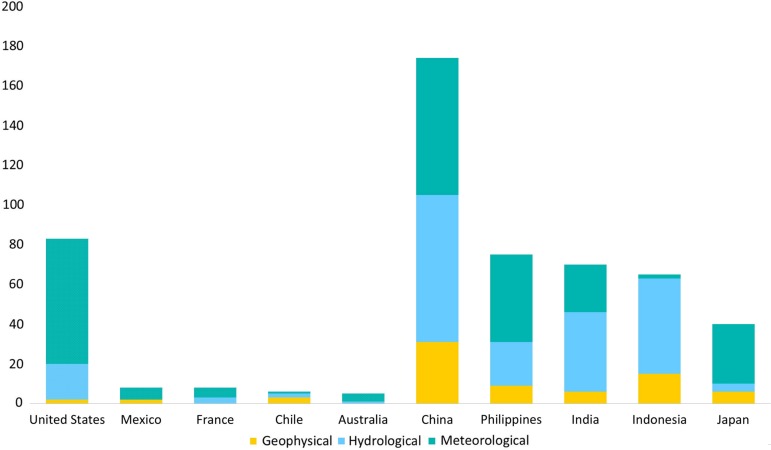
In recent years, most of the published disaster health literature concerns urban communities within high-income or developed countries. However, global disaster epidemiological patterns show that Asia has the highest frequency of natural disaster occurrences in floods, cyclones and earthquakes.1 In Asia, with the exception of the 2011 Great East Japan Earthquake, the majority of these large-scale disasters (the 2004 South Indian Ocean Tsunami, the 2005 Pakistan Kashmir Earthquake, the 2008 China Sichuan (Wenchuan) Earthquake, the 2013 Typhoon Haiyan and the 2015 Nepal earthquake) mostly affected rural communities in developing countries. Among the Asian countries, China has the highest cumulative number of natural disasters over the past decade (Fig. 1). In 2016 alone, it experienced 34 natural disasters, four of which ranked in the top 10 largest disasters worldwide in 2016.2 The year 2016–17 also saw Vietnam experience its worst drought in 90 years; a torrential monsoon in Bangladesh, India and Nepal, which killed over 900 people; and a 6.7 magnitude earthquake in the Philippines that impacted over 53 000 people.1
Fig. 1.
Top 5 Asian and non-Asia countries by number of reported Geophysical, Hydrological and Meteorological Disasters between 2012 and 2016, adopted from Annual Disaster Statistical Review 2012–16.3
Health-EDRM specifically refers to the systematic analysis and management of health risks surrounding emergencies and disasters by reducing the hazards and vulnerability along with extending preparedness, response and recovery measures.4 This encompasses both top-down and bottom-up interventions such as accessing early warning systems, timely deployment of relief workers, and the provision of suitable drugs and medical equipment to lessen the events’ impact during all stages of the disaster management cycle (prevention and mitigation, preparedness, response and recovery).5,6
The rural population is defined as people who are not living in cities and towns. Demography in rural communities are often characterized by populations of extreme ages, living in remote areas with endemic poverty and had low levels of education.7–9 In a number of Asian countries, many rural communities are transitional communities, which are reflected by their migratory nature and high demographic proportions of the very old and the very young. Specific health risks in their communities include respiratory issues from energy poverty which leads to indoor waste burning for food and warmth,10 the re-emergence of infectious diseases as a result of low vaccination coverage and gastrointestinal problems from unregulated waste management.11 Rural communities present with different healthcare needs and disease patterns from their urban counterparts. Referencing Asian countries, the objective of this paper is to examine the physical and mental health impact of natural disasters. Scientific evidence of potential health-EDRM interventions which might address health risks associated with geophysical, hydrological and meteorological disasters will be reviewed. Research and evidence gaps in the designing and planning of programmes and policies related to rural health-EDRM are identified. By applying disaster risk reduction (DRR) principles to guide health-EDRM, as stated in the Sendai Framework for Disaster Risk Reduction 2015–30,12 the adverse human health impact can be mitigated in rural communities (Table 1).
Table 1.
UNISDRa guiding principles from the Sendai Framework on Disaster Risk Reduction 2015–30 that may be applied to health-EDRM
| 1. Shared responsibility between central Governments and national authorities, sectors and stakeholders as appropriate to national circumstances |
| 2. Engagement from all of society |
| 3. Coherence of disaster risk reduction and sustainable development policies, plans, practices and mechanisms, across different sectors |
| 4. Decision-making to be inclusive and risk-informed while using a multi-hazard approach |
| 5. The quality of global partnership and international cooperation to be effective, meaningful and strong |
aUNISDR, the United Nations Office for Disaster Risk Reduction.
Search strategy
English-only articles and reports published between from January 2000 to January 2018 were included on health outcome, disaster management and impact of natural disasters in rural Asian communities. PubMed, Google Scholar, Embase, Medline and PsycINFO were used. The following keywords were searched for in peer-reviewed articles published in and after 2000: ‘rural’, ‘non-urban based’, ‘health-EDRM’, ‘disaster’, ‘disaster risk reduction (DRR)’, ‘natural disaster’, ‘earthquake’, ‘typhoon’, ‘cyclone’, ‘flood’, ‘response’, ‘relief’, ‘individual preparedness’, ‘household preparedness’, ‘community preparedness’, ‘policy-level preparedness’, ‘rural health’, ‘health impact’, ‘mental health’, ‘injury’, ‘non-communicable disease (NCD)’, ‘communicable disease’, ‘disease outbreak’, ‘disease pattern’, ‘Asia’, ‘China’, ‘India’, ‘Indonesia’, ‘Japan’, ‘Nepal’, ‘Pakistan’, ‘the Philippines’ and ‘Vietnam’. The snowballing search methodology was also used.
The top 10 countries by the number of reported disaster events in 2016 (CRED), if in Asia, were included in the keyword search.3 Geophysical, hydrological and meteorological disasters were reviewed as they are the most frequently reported disasters in Asia. Published papers reported in this study must include any of the keywords mentioned above in main text and describes the rural context. This paper will first discuss the physical and mental impact of selected natural disasters, followed by their health-EDRM interventions, and subsequent gaps in the keyword research.
Geophysical (Earthquakes)
Overall, earthquakes are caused by the ground shaking due to seismic waves and mainly occur along the Pacific Rim.13 Mortality is commonly caused by collapsed buildings and injuries often consist of fractures and soft-tissue trauma of the extremities. Specific mortality risk factors include physical disability, being indoors, distance from the epicentre and availability of hospital beds.13 The female gender and those with lower education level, or who had witnessed deaths, experienced bereavement, household damage or personal injury were more likely to develop Post-Traumatic Stress Disorder (PTSD).14
Physical health impact
Different populations, such as those of extreme ages, present disproportionate needs. In one report, 40% of the patients at a triage site were elderly yet chronic health needs were frequently overlooked.15 In the case of the Sichuan earthquake, 77% of admitted patients were reported with at least one NCD. Hypertension (47%) and diabetes (24%) made up the majority of burden. Rural infants who were provided with the equivalent nutritional provision intake as adults after the same earthquake showed signs of acute malnutrition, stunted growth and wasting 2 years later.16
Most of the literature reviewed in the search on natural disaster epidemiology focused on earthquakes, particularly the 2008 Sichuan earthquake and the 2004 Indian Ocean Tsunami. These disasters claimed 70 000 lives in China17 and 165 000 lives in Indonesia, respectively.18 Specific morbidities included crush syndrome, slips and falls.19–21
Although infrequent, infectious disease outbreaks tend to occur after the initial response phase and cases of respiratory infections, diarrhea and urinary tract infections were seen in China and Iran.22,23 Cramped conditions in temporary shelters were also linked to communicable disease outbreaks. Nepal saw an 80% increase in water-borne infections within the first 6 months of the 2015 earthquake24 and in the wake of the 2005 Pakistan earthquake, there were more than 400 cases of measles and outbreaks of meningitis, which are particularly fatal to children.25 While after the 2008 Sichuan earthquake, 2.41% of the victims were suspected of being afflicted with gas gangrene.26 In Sri Lanka, the influx of highly saline water and the chaotic distribution of waste due to the backwash of waves from the Indian Ocean Tsunami led to water-borne health issues. Anecdotal reports suggested surface water bodies and shallow wells were contaminated by decaying municipal solid waste and people reported skin irritation after contact with the waves. Samples taken later showed arsenic levels above the WHO’s 10 ppm safety level.27
There were also significant discrepancies in delivery of care for chronic health issues between rural mobile clinics and urban stationary clinics after the 2005 Kashmir Earthquake in Pakistan, leading to a higher prevalence of pneumonia in rural areas.28 In 2001, the Gujarat earthquake destroyed the majority of healthcare facilities and hospitals near the quake’s epicentre, directly affecting medical triage and the well-being of existing in-patients. Over 65% of soft-tissue injuries became infected and/or contaminated as treatment was limited to outdoor or first-aid techniques due to overcrowded hospitals and scarce resources.21
Mental health impact
Tsunamis, including the 2004 Indian Ocean Tsunami and the 2006 Pangandaran Tsunami, gravely affected Indonesia, especially its smaller offshore islands. PTSD surveys conducted after the Indian Ocean Tsunami found that 24% of survivors in field hospitals displayed four out of seven of the PTSD symptoms. Those with the most severe symptoms were associated with loss of kin, property damage and exposure to traumatic events. Prior traumatic events were prevalent in Indonesia at the time due to the then ongoing civil conflict.29,30 Men had a higher prevalence of depression, anxiety and somatic symptoms compared to women. Adolescents and adults in the Aceh region of Indonesia and who lived in camps for displaced people were three times more likely to suffer from tsunami-related fears compared to those living in villages. Existing mental illnesses such as schizophrenia—which accounts for 92% of the Indonesians admitted to mental hospitals30—also need to be addressed in disaster management as they require long-term drug treatment.
Cultural context is routinely mentioned in disaster management but specifics are rarely given. In China, there were discrepancies in the literature on whether members of the majority Han ethnic majority were at higher risk of developing PTSD when compared to various ethnic minorities. The notion of ethnic minority resilience suggests that the cultural worldview of minority communities play an important role in how they interpret and react to acute stress reactions, leading to a lower prevalence of PTSD symptoms compared to the Han Chinese.31,32 Inadequate mental health support in China also saw 49% of soldiers involved in relief work suffering from mental health problems during the rescue phase of the Sichuan earthquake; 6.53% of these soldiers subsequently suffered from PTSD 6 months later.17,33 Junior middle school students, especially girls and those who were delayed in evacuation, or whose houses had been destroyed were at also at high risk of PTSD and/or depression 10 months after the Sichuan earthquake.34
Qu, et al. found Chinese women from the Qiang ethnic minority who worked on farms were at higher risk for PTSD than non-farm workers. This indicates loss of farmland or agricultural work may be an indirect but distinct cause for distress among rural populations.35,36 A greater proportion of those who died in the Indian Ocean Tsunami were women because they were by the coastline when the waves hit, while the men were out at sea.37 Other indirect health risks for women and girls include vulnerability to human trafficking during post-disaster mass displacements through being kidnapped or tricked by promises of migrant work.38,39
Health-EDRM interventions
For individual preparedness of health-EDRM, knowledge and previous experience with disasters was not found to be associated with greater disaster preparedness unless individuals or affected households had sustained direct serious impact during a previous disaster.40 A study on Indonesian islands which had embedded the experiences of historical tsunamis and floods into their local culture showed that communities with repeatedly exposed to disasters recognized hazard signs (e.g. receding tide) and took relevant actions to prevent injury (e.g. retreating to higher ground).18 In general, women, socially active people and people with mobility issues were associated with a greater uptake of preventive actions. While studies on health education interventions in China and Thailand showed that even when villagers had experienced some form of previous disaster event, only around 30% possessed disaster or emergency kits.8,40 Through studying intentions for disaster preparedness, one of the major reasons identified for the lack of such kits was uncertainty about what might be needed and a lack of skills. For example, many villagers living in disaster-prone areas in rural China expressed interest in preparing disaster kits but most were unsure of what the contents should be41,42 and did not know the skills required for self-rescue.19 They were also unsure if disaster kits would be useful during an earthquake. For Tsunamis, although water-borne health risks are prominent, and interventions such as bottled water, water purification vehicles and mountain spring water have proved to be effective in Sri Lanka, household health-EDRM practices such as boiling water also need regular reinforcement as the behavioral pattern might not be sustained (water contamination is often invisible to the naked eye).43
At the community level, research on the knowledge and skills of relief and military rescue workers suggested that a significant proportion of frontline rescue workers were not trained specifically for rural environments or even for disasters. Surveys on disaster education conducted after the Sichuan earthquake showed 89.8% of Chinese health professionals wanted disaster management to be included in the medical training curriculum. Most respondents preferred online training for convenience and flexibility.44 While short term training programmes were developed through recommended technical frameworks8,22,42 (e.g. based on ICN Framework of Disaster Nursing Competencies 2009), the long-term effectiveness and clinical impact of such training has not been tested.45 Major logistical issues also arose during the 2015 Nepal Earthquake as medical relief teams failed to reach some of the remote rural areas even after 4 days and local health facilities were non-existent.46 A number of articles pointed out that NCDs, which often represent the underlying epidemiological profile of the affected communities, were often ignored in protocol and planning due to a lack of awareness, the absence of diagnostic tools, inability to afford medication and not having stock of medication. This potentially leads to an absence of medication during evacuation and the untreated symptoms may cause medical/surgical complications.47 On a policy level, Iran has set up a communicable diseases surveillance system for detecting and monitoring 19 diseases/syndromes that was used after the 2012 East Azerbaijan Earthquakes. However, there were communication issues with the rural health houses (rural health centres) and disagreement on the case definitions.23 To combat vector-bone diseases, the Health and Family Planning Commission of Yunnan Province, China, took measures to prevent outbreaks of malaria (e.g. sanitation and immunization) in rural villages and other high risk areas such as temporary shelters after the 2014 earthquakes.48
Meteorological (cyclones, storms and typhoons)
A cyclone is defined as a non-frontal storm with spirals of strong winds and rain, with various nomenclatures given to indicate their location and strength.49 A literature review has found that mortality was directly caused by drowning followed by trauma; or indirectly through causes such as motor-vehicle injury, fire burns and electrocution, all associated with winds exceeding 155 miles/h, storm surges above 10 m, and torrential rain.49
Physical health impact
Cyclones, storms and typhoons are frequent disasters in Asia and will likely increase in frequency due to climate change. Yet, the rural populations often have the lowest level of awareness of their own health impact and associated health risks.50 Injury prevalence was an amalgamation of lacerations, wounds, contusions and blunt force trauma, the majority of which could be treated in an outpatient facility. Cascading hazards in the aftermath of cyclones include floods, as seen with Cyclone Gorky (Bangladesh) in 1991 and Cyclone Nargis (Myanmar) in 2008. Together, they account for two-thirds of all cyclone-related deaths reviewed in 30 years.49,51 There is currently no study specific to the demographic variability of physical impacts from cyclones and typhoons.
Studies reviewed in the search indicated water security is a huge concern as many typhoon-stricken areas are coastal regions, putting an estimated 25 million people at risk of drinking water contaminated by sea water. A study on southeast Asia reported that over 30% of those who had consumed over half of their sodium intake just through drinking water may be at risk for hypertension.52 Tropical cyclones also pose risks for communicable diseases such as upper-tract respiratory infections, gastroenteritis and vector-borne diseases such as dengue fever and malaria from pools of stagnant water (China and the Philippines).50,53
Mental health impact
A number of mental health studies were published after Typhoon Haiyan in the rural Philippines. These studies observed high rates of PTSD and reported stigmatization of mental illness, which made identification and treatment difficult. Furthermore, people with existing psychiatric issues were left untreated as they ceased to receive medication.54 Excessive alcohol use has been associated as a negative coping mechanism for disasters, which may have exacerbated the already existing high-alcohol consumption in the Philippines.55 A study in South Korea after Typhoon Rusa (2002) found primary school-aged children reported mild anxiety (60%) and moderate to severe PTSD symptoms, which was associated with fear and separation from parents.56
Health-EDRM interventions
Despite the low self-perception of health risks, studies indicated disaster affected communities regard disaster education on health risks as necessary. About 89% of study participants from rural China thought typhoon disaster education was needed but only around 50% knew about keeping emergency food and drugs, and checking electrical circuits. Findings indicated non-actions were associated with the lack of technical know-how.57 Meteorological disasters also affect the availability of drugs. In 2013, Typhoon Haiyan caused massive disruption for tuberculosis (TB) drug treatment in the Philippines. Despite its endemic status and potential implication for multiple-drug resistant TB development, TB was not included in the ‘Surveillance in Post Extreme Emergency and Disasters’ system and most of the case records were lost. In some regions, it took 6–8 weeks for all the treatment and diagnosis facilities to reopen.58 Systematic backup of health records and treatment plans are crucial for allocation of resources for uninterrupted disease management. Research on disaster-related knowledge in China and the Philippines showed individuals had a good knowledge about cyclone occurrences and its related protective behaviors, which were associated with sociodemographic characteristics, but many did not adhere to warnings or carry out protective behaviors.57,59 Local and indigenous knowledge for identifying early predictors of typhoons and floods (e.g. a prolonged strong smell of fish from the sea and the appearance of black and white striped sea snakes) allowed residents on Rapu-rapu Island in the Philippines, to be prepared for pending disasters.60 At the systems level, when early warning systems are comprised of effective global partnerships, such as the ESCAP/WMO Typhoon Committee, it appears to be effective in facilitating time-sensitive data exchange to minimize blind spots during typhoon tracking. In 2016, Typhoon Meranti (peak = 305 km/h) caused minimum damage due to precise tracking of its speed, intensity and movement.1
Hydrological (floods, wet mass movements)
Flooding is the result of a significant rise in water levels, whether it is from storm surges, sea-level rising, torrential rainfall/monsoons or melting snow. Over 63% of all floods involve mortality, most from drowning, but characteristics associated with drowning have not been made clear. Other common causes of death include electrocution, heart attacks, hypothermia and trauma.51 Females, the elderly, children and males aged 10–29 are at greater risk for mortality.61 Carbon monoxide poisoning is also an indirect cause of mortality but it has only been recorded in urban areas and middle-high income countries.62
Physical health impact
From the search, almost no published paper had reported rural flood epidemiology patterns in Asia. Mortality associated risks include the storm course, timing of warning systems and the summer months.51 High mortality is usually associated with flash floods, and rapid urbanization has eroded the natural and historical methods of flood prevention.63 Over half the households in Thailand reported acute health problems such as skin infections and cold symptoms during floods, in addition to hypertension and diabetes.64 The handful of papers on rural health discussed an increase in fires and snake bites. Extreme ages are also highlighted such as in rural Hainan, China, where gender and ethnicity impacted the self-reported health outcomes of elderly people (age ≤ 50).65 Nutritional outcomes were also reported in affected communities. In rural Odisha, India, wasting among children under 5-years-old was 1.94–2.3 times higher in communities that were flooded in comparison to non-flooded communities. Severe wasting was even more prevalent in communities that experienced repeated floods.66
The effects of climate change saw an increase in floods and typhoons in Vietnam.63 Flash floods were found more frequently in the mountainous Himalayan regions of Pakistan, a country that already has a high prevalence of malaria, TB and polio. The most immediate incident cases of infectious disease was of acute diarrhea, followed by incidences of acute respiratory infections increasing two weeks later.67 Looking specifically at the effect of flooding in China, a study noted that previously eliminated infectious diseases had also re-emerged.68
Mental health impact
Mental health impact post-flooding varies in context. In China, PTSD was repeated to be prevalent in all ages, especially for people with low social support.69,70 However for Thailand, specific mental health problems were associated with economic losses in farm production and food insecurity.64 In Uttar Pradesh, India, negative effects of repeated exposure to floods included symptoms of anxiety and depression compared to individuals not affected by floods. Of note, same study also found no relationship between mental health outcomes and physical health.71,72
Health-EDRM interventions
Floods often reoccur in the same area, therefore system-level post-disaster recovery and rehabilitation efforts should also take into account of future disaster preparedness and resilience building. Nevertheless, for community protection, individual level of preparedness in Asian communities was low. Studies indicated that up to 72.5% of respondents from rural China with disaster experience did not have any form of preparedness. Major knowledge gaps include geographic locations, populations at risk from natural disaster and what is the risk factors for displacement.51,73 Health intervention that targets knowledge enhancement in disaster kit preparedness and homemade oral rehydration solution (ORS) were retained 12 months after the intervention, which shows health-EDRM interventions were well-received.41 Effects of community-level preparedness was reported from local and indigenous coastal areas and small islands. For example, in Sayung, Indonesia, stilt houses were used to combat coastal flooding.60 However, at the community level, the discrimination against people from a lower social hierarchy or caste in India created direct barriers to disaster preparedness and mitigation as lower caste people were turned away from shelters.74 In addition, on a policy-level, there is generally an emphasis on response rather than preparedness. For example, in Vietnam, training for health-related emergencies did not meet the actual needs and the role of primary healthcare workers in emergency response was not defined.75
Intervention for health, emergency and disaster risk reduction
In addition to the review of health-EDRM in specific disaster sub-types, scientific evidence associated with generalized health-EDRM interventions can be conceptualized and examined according to primary, secondary and tertiary hierarchy levels, to prevent, minimize and mitigate health risks before the onset of disasters, immediately after the occurrence of disasters, and those already affected by the disaster (Table 2).
Table 2.
The current evidence on the various levels of Health-EDRM Interventions for monitoring and evaluation in rural Asia (from reviewed materials)
| Mentioned health-EDRM interventions (as of January 2018)2 | ||||
|---|---|---|---|---|
| Primary | Secondary | Tertiary | ||
| Measures aim to prevent the onset of disaster or minimize the risks that might contribute to the occurrence of emergency and disasters risks | Aims to prevent potential harm and health risks associated immediately after the occurrence of a disaster | Aims to minimize the impact and damage after disaster. Targets specifically at people who might already suffered from the disaster impact | ||
| Levels of Preparedness1 | Individual/Household |
|
|
|
| Community |
|
|
|
|
| System/Policy |
Health and disaster risk literacy
|
Health risk management
|
Health response | |
1,2 Levels of disaster preparedness and health interventions categorized from ‘Public Health Humanitarian Responses to Natural Disasters’ adapted from Chan 20 17.6
aStudies that evaluated disaster preparedness interventions in Asia.
Review indicated although efficacies of primary interventions, such as vaccinations, have been examined in the context of armed conflicts and displaced populations, effectiveness of disease vaccination prevention was rarely examined in natural disasters. Low tetanus vaccination rates were reported in multiple Asian countries, especially among elders,15 but only one study in China looked at the implementation of emergency immunizations and it was deemed unreliable by local hygiene professionals.43 The lack of baseline information for vaccination coverage is likely to create an opportunity for an otherwise preventable disease outbreak. Multisectoral coordination mechanisms have to be set up to ensure there is accountability and validity of relief actions, such as mass vaccination campaigns.
Secondary intervention studies that were published which align with DRR concepts and health-EDRM principles include evacuating to a safe place, owning disaster kits and awareness of disaster risks. The approaches aim to lessen the disaster impact, but the risk reduction practices have not been quantified or evaluated beyond knowledge assessments of selected rural villages.8,41 Except in hospital settings, no randomized control trials have been published in other care settings.89 The optimal channels to use for communication (television, word of mouth)57,79,85 have been surveyed along with the need for first-aid training77 and disaster kit preparedness90 for laypeople, but no studies have evaluated whether those interventions in rural Asian communities were actually beneficial during a disaster.
Tertiary interventions in health-EDRM, which typically revolve around medical treatment and recovery include field medical teams, hospitals, and clinics in patient management and disease control. Assessment quality varies as data on morbidity and mortality rates were found not to be disaggregated by demography or diagnosis, especially in floods and cyclones. PTSD overwhelmingly dominates the mental health research field but no treatment options were reported let alone assessed. Of the systematic literature reviews Doocy, et al. did on thirty years of natural disasters, fewer than 50% of papers reported injuries, and an even smaller fraction gave specifications. The need for better clinical management and deployment of other medical disciplines remain mere suggestions and are not standard practice due to the lack of evidence-based support in Asia.
Discussion
Overall, this review indicated most evidence-based research was related to earthquakes. Most published evidence highlights disaster recovery with the occasional clinical outcomes. Few publications highlighted the impacts and health risks associated with floods and cyclones although these cause the most global natural disaster-related deaths. Although studies on physical and mental health were reported, indirect health risks such as infectious diseases and contaminated water sources were only occasionally found. Crosscutting themes emerged such as the difference in PTSD prevalence for age subgroups, and the lack of disaster-specific knowledge in relief workers and at-risk communities, and evidence-based interventions to engage in various levels of health-EDRM. Notably for health protection, no published reports were identified by the current search algorithm associated with post-disaster food safety, injury, the occupational safety of responders or cost-effectiveness/cost-benefit analysis of health-EDRM interventions in comparison with other post-disaster programmes. Although various health education and promotion interventions were reportedly implemented on an individual and community-level, there is a lack of scientific evidence on whether these education interventions were accepted, utilized or demonstrated their intended effectiveness. In addition, there were only nine published journal articles and reports that used the term ‘health-EDRM’, ‘H-EDRM’ and ‘EDRM-H’ which reflects a research gap and the inconsistent use of the phrase, as of January 2018 (Table 3). This also shows health-EDRM as a research topic is still in its infancy, as only three of the studies were on rural health.
Table 3.
Published articles and reports which mentions health-EDRM (as of January 2018)
| Paper | Publication type | Journal | Author | Date published | Location | Term variation |
|---|---|---|---|---|---|---|
| Health Emergency and Disaster Risk Management (Health-EDRM): Developing the Research Field within the Sendai Framework Paradigm | Short Article | International Journal of Disaster Risk Science | S. Lo, E. Chan, G. Chan, et al. | 2017 | Non-specific | Health-EDRM |
| Health Emergency and Disaster Risk Management (Health- EDRM) in Remote Ethnic Minority Areas of Rural China: The Case of a Flood-Prone Village in Sichuan | Short Article | International Journal of Disaster Risk Science | E. Chan, C. Guo, P. Lee, S. Liu, C. Mark | 2017 | China | Health-EDRM |
| Health Emergency and Disaster Risk Management (H-EDRM): Developing the Research Field within the Sendai Framework Paradigm | Supplement 1 | Prehospital and Disaster Medicine | C. Guo, S. Lo, E. Chan, G. Chan, et al. | 2017 | Non-specific | Health-EDRM |
| What are the health research needs for the Sendai Framework? | Comment | The Lancet | E Chan, V. Murray | 2017 | Non-specific | Health-EDRM |
| Health and Risks: Integrating Health into Disaster Risk Reduction, Risk Communication, and Building Resilient Communities | Editorial | International Journal of Disaster Risk Science | E. Chan, P. Shi | 2017 | Non-specific | H-EDRM |
| Medical and health risks associated with communicable diseases of Rohingya refugees in Bangladesh 2017 | Article | International Journal of Infectious Disease | E. Chan, C. Chiu, G. Chan | 2017 | Bangladesh | H-EDRM |
| Building National Resilience for Sexual and Reproductive Health: Learning from Current Experiences | Report | Women’s Refugee Commission | Women’s Refugee Commission | 2016 | Eastern Europe, Central Asia | EDRM-H |
| The Role of Public Health Within the United Nations Post-2015 Framework for Disaster Risk Reduction | Article | International Journal of Disaster Risk Science | V. Murray, A. Aitsi-Selmi | 2015 | Non-specific | EDRM-H |
| Reducing risks to health and well-being at mass gatherings: the role of the Sendai Framework for Disaster Risk Reduction | Article | International Journal of Infectious Disease | A. Aitsi-Selmi, V. Murray, D. Heymann, B. McCloskey, et al. | 2015 | Non-specific | EDRM-H |
Key findings on Asian rural disasters were mostly published from China, consistent with Elsevier’s recent global report on disaster science,87 followed by Japan, the Philippines, Indonesia and Bangladesh. Between 2012–16, the report mentioned above found 6301 papers published by China on disaster science. Using the same time frame, our review only found 27 papers that wrote specifically about health and rural populations. In fact, it is difficult to review papers on rural populations as the urban/rural demography is not specified in most of the disaster literature. Research articles about Asia also tend to be in a non-English language. A huge selection bias likewise exists where research is given preference to ‘famous’ disasters which tend to be earthquakes and tsunamis.
Of the few DRR and health-EDRM prevention interventions documented, there is an absence of evaluations of whether the same intervention under different disaster categories would have the same outcome. For example, is household ORS more widely used in floods, cyclones or earthquakes, and does it actually prevent or mitigate the symptoms of diarrheal diseases in different settings? As urbanization is a growing trend, changing economic, social and demographic patterns also need to be addressed. With a growing migrant population, it is presumptive to assume that migrants’ disaster risk profiles should be assessed using one static location. The risks should account for dynamic migratory patterns in multiple locations, especially as rural and urban settings carry different risks. Of note, there was also no study available on the actual awareness of the occupational hazards which frontline workers have to face and their mental health protection apart from one semi-structured interview. It assessed the pre-deployment preparation of internationally deployed relief workers and found that honesty and realistic expectations of the working environment were deemed helpful.78 One other study gave suggestions on self-care for frontline workers but did not assess their actual practice.91
The frequency and severity of natural disasters are increasing and the lack of DRR and health-EDRM interventions in rural Asian communities is the major evidence gap. Earthquake-related community-level clinical interventions and system-level hospital disaster training have been recommended, but no effectiveness studies on practices were found in the literature. The 2011 Great East Japan earthquake is an example where flooding was unprecedented and many people perished despite following evacuation plans.92 Except for personal disaster preparedness, there is almost no published health-EDRM research concerning floods. For cyclones, early warning systems were found to be effective at a policy level but not at a household/individual level as many people did not adhere to the warnings. Health risks such as vector-borne diseases and hypertension from saline-contaminated water were identified but no study actually examined if subsequent high salt intake caused hypertension.
Even with the plethora of recommendations, there are still gaps and inconsistencies for the efficacy of homemade ORS,93 disaster kits, warning and evacuation drills, psychological first-aid94 and disaster health literacy. Only cross-sectional studies and immediate pre/post education surveys have been published on those topics for rural areas. Furthermore, Health-EDRM during pre-disasters (i.e. the prevention and mitigation phase) is also important to maintain a robust health status at baseline. As technology progresses and is being integrated into disaster management, the preferred type of communication strategy (e.g. face-to-face, mobile app, the internet)80,95 should likewise be addressed. From the scope of this review, no published studies have examined the cost-effectiveness and cost-benefits of different Health-EDRM interventions. The previous paradigm on health-EDRM relied upon government-level responses to save lives, which may be insufficient. An all-of-society engagement approach is needed to reveal the hidden gaps between the delivery of disaster interventions and the targeted recipients. Contingency plans must factor in vulnerabilities of older people, ethnic minorities, illiterate populations, people with disabilities and NCDs, those who face gender-based discrimination, and other marginalized communities. An all-hazards approach also needs to be considered as disasters have cascading risks and are rarely single events, for example, many typhoons also cause flooding.88
Limitations of this review include the exclusion of non-English, non-electronic, and grey literature such as public, governmental and non-governmental organizations (NGO) reports. Country-specific searches only included the top 10 countries with a focus on rural outcomes. Furthermore, only three disaster categories were discussed, mostly from observational studies, which potentially excluded location-specific disasters such as infectious disease outbreaks, droughts and armed-conflicts. The time frame of this review (2000–18) has also left out major disaster events before the millennium. However, our review does present the gaps in health-EDRM research, especially through looking at current health impacts and risk reduction efforts of earthquakes, cyclones and floods in rural Asia. By breaking health-EDRM down into individual/household, community and system/policy levels, this review identifies clear topics for future clinical and public health research.
Acknowledgements
The authors would like to thank the help of Ms Janice Ho, Ms Carol Wong, Dr Tony Yung, Ms Sophine Tsang and Mr Eugene Lo.
Conflict of interest statement
The authors have no potential conflicts of interest.
References
- 1. ESCAP Asia-Pacific Disaster Report 2017 Disaster Resilience for Sustainable Development. 2017.
- 2. Internal Displacement Monitoring Centre Global Report ON INTERNAL DISPLACEMENT. 2017.
- 3. Guha-Sapir D, Hoyois P, Wallemacq P, et al. Annual Disaster Statistical Review 2016 The numbers and trends. 2017.
- 4. Abrahams J. Disaster Risk Management for Health Advocating disaster risk management for health. World Heal Organ. 2011.
- 5. Wisner B, Adams J. Environmental health in emergencies and disasters A PRACTICAL GUIDE. 2002.
- 6. Chan EYY. Public health humanitarian responses to natural disasters, 1st ed New York: Routledge, 2017, p.259. [Google Scholar]
- 7. Liu N, Zeng L, Li Z, et al. Health-related quality of life and long-term care needs among elderly individuals living alone: a cross-sectional study in rural areas of Shaanxi Province, China. BMC Public Health 2013;13:2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chan EYY, Kim JH, Lin C, et al. Is previous disaster experience a good predictor for disaster preparedness in extreme poverty households in remote muslim minority based community in China? J Immigr Minor Heal 2014;16:466–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ning Y, Tao MX, Hu JF, et al. Status of household disaster preparedness and affected factors among the general public of four counties in Shaanxi. Chin J Prev Med 2013;47:347–50. [PubMed] [Google Scholar]
- 10. Zhang J, Mauzerall DL, Zhu T, et al. Environmental health in China: challenges to achieving clean air and safe water. Lancet 2010;375:265–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brown C, Milke M, Seville E. Disaster waste management: a review article. Waste Manag 2011;31:1085–98. [DOI] [PubMed] [Google Scholar]
- 12. Nations Office for Disaster Risk Reduction U Sendai Framework for Disaster Risk Reduction. 2015.
- 13. Doocy S, Daniels A, Packer C, et al. The human impact of earthquakes: a Historical Review of Events 1980 2009 and Systematic Literature Review. PLOS Curr Disasters 2013;5:1–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dai W, Chen L, Lai Z, et al. The incidence of post-traumatic stress disorder among survivors after earthquakes:a systematic review and meta-analysis. BMC Psychiatry 2016;16:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chan EYY. The untold stories of the Sichuan earthquake. Lancet 2008;372:359–62. [DOI] [PubMed] [Google Scholar]
- 16. Dong C, Ge P, Ren X, et al. Growth and anaemia among infants and young children for two years after the Wenchuan Earthquake. Asia Pac J Clin Nutr 2014;23:445–51. [DOI] [PubMed] [Google Scholar]
- 17. Zhang L, Liu X, Li Y, et al. Emergency medical rescue efforts after a major earthquake: lessons from the 2008 Wenchuan earthquake. Lancet 2012;379:853–61. [DOI] [PubMed] [Google Scholar]
- 18. Gaillard J-C, Clavé E, Océane A, et al. Ethnic groups; response to the 26 December 2004 earthquake and tsunami in Aceh, Indonesia. Nat Hazards 2008;47:17–38. [Google Scholar]
- 19. Qiu J, Liu G, Wang S, et al. Analysis of injuries and treatment of 3 401 inpatients in 2008 Wenchuan earthquake—based on Chinese Trauma Databank. Chinese J Traumatol English Ed 2010;13:297–303. [PubMed] [Google Scholar]
- 20. He Q, Wang F, Li G, et al. Crush syndrome and acute kidney injury in the Wenchuan Earthquake. J Trauma 2011;70:1213–7; discussion 1217–8. [DOI] [PubMed] [Google Scholar]
- 21. Phalkey R, Reinhardt JD, Marx M. Injury epidemiology after the 2001 Gujarat earthquake in India: a retrospective analysis of injuries treated at a rural hospital in the Kutch district immediately after the disaster. Glob Health Action 2011;4:7196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cartwright C, Hall M, Lee ACK. The changing health priorities of earthquake response and implications for preparedness: a scoping review. Public Health 2017;150:60–70. [DOI] [PubMed] [Google Scholar]
- 23. Babaie J, Fatemi F, Ardalan A, et al. Communicable diseases surveillance system in East Azerbaijan earthquake: strengths and weaknesses. PLoS Curr 2014;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Uprety S, Hong PY, Sadik N, et al. The effect of the 2015 earthquake on the bacterial community compositions in water in Nepal. Front Microbiol 2017;8:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kouadio IK, Aljunid S, Kamigaki T, et al. Anti-infective therapy infectious diseases following natural disasters: prevention and control measures. Expert Rev Anti Infect Ther 2014;10:95–104. [DOI] [PubMed] [Google Scholar]
- 26. Chen E, Deng L, Liu Z, et al. Management of gas gangrene in Wenchuan earthquake victims. J Huazhong Univ Sci Technolog Med Sci 2011;31:83–7. [DOI] [PubMed] [Google Scholar]
- 27. Pilapitiya S, Vidanaarachchi C, Yuen S. Effects of the tsunami on waste management in Sri Lanka. Waste Manag 2006;26:107–9. [DOI] [PubMed] [Google Scholar]
- 28. Chan EYY. Building Bottom-up Health and Disaster Risk Reduction Programmes, 1st ed Oxford: Oxford University Press, 2017, p368. [Google Scholar]
- 29. Musa R, Draman S, Jeffrey S, et al. Post tsunami psychological impact among survivors in Aceh and West Sumatra, Indonesia. Compr Psychiatry 2014;55:S13–6. [DOI] [PubMed] [Google Scholar]
- 30. Marthoenis M, Yessi S, Aichberger MC, et al. Mental health in Aceh—Indonesia: a decade after the devastating tsunami 2004. Asian J Psychiatr 2016;19:59–65. [DOI] [PubMed] [Google Scholar]
- 31. Cheung EYL, Chan EYY, Lam HP, et al. Post disaster mental health among ethnic minorities in rural China: results from qualitative studies. Prehosp Disaster Med 2011;26:s88–9. [Google Scholar]
- 32. Xu J, Zhang Y, Chan J, et al. A comparison of the acute stress reactions between the Han and Tibetan ethnic groups in responding to devastating earthquakes. Int J Psychiatry Med 2011;42:167–80. [DOI] [PubMed] [Google Scholar]
- 33. Wang H, Jin H, Nunnink SE, et al. Identification of post traumatic stress disorder and risk factors in military first responders 6 months after Wen Chuan earthquake in China. J Affect Disord 2011;130:213–9. [DOI] [PubMed] [Google Scholar]
- 34. Wang W, Fu W, Wu J, et al. Prevalence of PTSD and depression among Junior Middle School Students in a Rural Town Far from the Epicenter of the Wenchuan Earthquake in China. PLoS One 2012;7:41665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Qu Z, Wang X, Tian D, et al. Posttraumatic stress disorder and depression among new mothers at 8 months later of the 2008 Sichuan earthquake in China. Arch Womens Ment Health 2012;15:49–55. [DOI] [PubMed] [Google Scholar]
- 36. Liu Z, Zeng Z, Xiang Y, et al. A cross-sectional study on posttraumatic impact among Qiang women in Maoxian County 1 year after the Wenchuan Earthquake, China. Asia Pac J Public Health 2012;24:21–7. [DOI] [PubMed] [Google Scholar]
- 37. Oxfam The tsunami’s impact on women. 2005.
- 38. Gyawali B, Keeling J, Kallestrup P. Human trafficking in Nepal: post-earthquake risk and response. Disaster Med Public Health Prep 2017;11:153–4. [DOI] [PubMed] [Google Scholar]
- 39. Dutta PM. Natural disaster and vulnerability to trafficking of women and girls in India. Eur Sci J 2017;7881:54–69. [Google Scholar]
- 40. Witvorapong N, Muttarak R, Pothisiri W. Social participation and disaster risk reduction behaviors in Tsunami prone areas. PLoS One 2014;10:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ying Yang Chan E, Chunlan Guo B, Poyi Lee B, et al. Health Emergency and Disaster Risk Management (Health-EDRM) in Remote Ethnic Minority Areas of Rural China: the case of a Flood-Prone Village in Sichuan. Int J Disaster Risk Sci 2017;8:156–63. [Google Scholar]
- 42. Chan EYY. Health Education for Hui Ethnicity in a Disaster-Prone Rural Setting in Gansu Province, China. In: The 13th World Congress on Public Health. 2012. p. 9956.
- 43. Zeng G. Investigation and recommendations concerning prevention and treatment of infectious diseases and promotion of hygiene in earthquake-stricken areas. J Evid Based Med 2008;1:2–8. [DOI] [PubMed] [Google Scholar]
- 44. Huang B, Li J, Li Y, et al. Need for continual education about disaster medicine for health professionals in China—a pilot study. BMC Public Health 2011;11:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wang C, Xiang H, Xu Y, et al. Improving emergency preparedness capability of rural public health personnel in China. Public Health 2010;124:339–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sharma DC. Nepal earthquake exposes gaps in disaster preparedness. Lancet 2015;385:1819–20. [DOI] [PubMed] [Google Scholar]
- 47. Hung KK, Lam EC, Chan EY. Graham C a. Disease pattern and chronic illness in rural China: the Hong Kong Red Cross basic health clinic after 2008 Sichuan earthquake. EMA - Emerg Med Australas 2013;25:252–9. [DOI] [PubMed] [Google Scholar]
- 48. Feng J, Xia Z, Zhang L, et al. Risk Assessment of Malaria Prevalence in Ludian, Yongshan, and Jinggu Counties, Yunnan Province, After 2014 Earthquake Disaster. Am J Trop Med Hyg 2016;94:674–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Doocy S, Dick A, Daniels A, et al. The human impact of tropical cyclones: a historical review of Events 1980–2009 and Systematic Literature Review Citation Abstract Authors. PLOS Curr Disasters 2013;1:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dolhun E. Aftermath of Typhoon Haiyan: the imminent epidemic of waterborne illnesses in Leyte, Philippines. Disaster Med Public Health Prep 2013;7:547–8. [DOI] [PubMed] [Google Scholar]
- 51. Doocy S, Daniels A, Murray S, et al. The human impact of floods: a historical review of events and systematic literature review. PLOS Curr Disasters 2013;1:1–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hoque M a, Scheelbeek PFD, Vineis P, et al. Drinking water vulnerability to climate change and alternatives for adaptation in coastal South and South East Asia. Clim Change 2016;136:247–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zheng J, Han W, Jiang B, et al. Infectious diseases and tropical cyclones in southeast China. Int J Environ Res Public Health 2017;14:494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. McCall C. Scars of typhoon Haiyan still run deep 1 year on. Lancet 2014;384:1656–7. [DOI] [PubMed] [Google Scholar]
- 55. Zhao C, Wu Z, Xu J. The association between post-traumatic stress disorder symptoms and the quality of life among Wenchuan earthquake survivors: the role of social support as a moderator. Qual Life Res 2012;22:733–43. [DOI] [PubMed] [Google Scholar]
- 56. Lee I, Ha Y-S, Kim Y-A, et al. PTSD symptoms in Elementary School Children After Typhoon Rusa. J Korean Acad Nurs 2004;34:636–45. [DOI] [PubMed] [Google Scholar]
- 57. Zhang W, Wang W, Lin J, et al. Perception, knowledge and behaviors related to typhoon: a cross sectional study among rural residents in Zhejiang, China. Int J Environ Res Public Health 2017;14:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lew W, Vianzan R. Restarting the tuberculosis programme post-Haiyan. West Pacific Surveill Response 2015;6:96–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Jiang L-P, Yao L, Bond EF, et al. Risk perceptions and preparedness of typhoon disaster on coastal inhabitants in China. Am J Disaster Med 2011;6:119–26. [PubMed] [Google Scholar]
- 60. Hiwasaki L, Luna E, Syamsidik Marçal JA, et al. Local and indigenous knowledge on climate-related hazards of coastal and small island communities in Southeast Asia. Clim Change 2015;128:35–56. [Google Scholar]
- 61. Lowe D, Ebi KL, Forsberg B. Factors increasing vulnerability to health effects before, during and after floods. OPEN ACCESS Int J Environ Res Public Health 2013;10:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Waite T, Murray V, Baker D. Carbon monoxide poisoning and flooding: changes in risk before, during and after flooding require appropriate public health interventions. PLoS Curr 2014;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Tran P, Shaw R. Towards an integrated approach of disaster and environment management: a case study of Thua Thien Hue province, central Viet Nam. Environ Hazards 2007;7:271–82. [Google Scholar]
- 64. Srikuta P, Inmuong U, Inmuong Y, et al. Health vulnerability of households in flooded communities and their adaptation measures: case study in Northeastern Thailand. Asia-Pacific J Public Heal 2015;27:743–55. [DOI] [PubMed] [Google Scholar]
- 65. Chan EYY, Lin CLY, Lee PPY, et al. Preliminary results of post-flooding impacts on rural elderly in Hainan Province, China. Prehosp Disaster Med 2011;26:s41. [Google Scholar]
- 66. Rodriguez-Llanes J, Ranjan-Dash S, Mukhopadhyay A, et al. Flood-exposure is associated with higher prevalence of Child Undernutrition in Rural Eastern India. Int J Environ Res Public Health 2016;13:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Shabir O. A summary case report on health impacts and responses to Pakistan floods of 2010. PLOS Curr Disasters 2013;5:1–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wu X-H, Zhang S-Q, Xu X-J, et al. Effect of floods on the transmission of schistosomiasis in the Yangtze River valley, People’s Republic of China. Parasitol Int 2008;57:271–6. [DOI] [PubMed] [Google Scholar]
- 69. Feng S, Tan H, Benjamin A, et al. Social support and posttraumatic stress disorder among flood victims in Hunan, China. Ann Epidemiol 2007;17:827–33. [DOI] [PubMed] [Google Scholar]
- 70. Peng H. China’s health challenges after the Yushu Earthquake. Prehosp Disaster Med 2011;26:135–6. [DOI] [PubMed] [Google Scholar]
- 71. Wind TR, Joshi PC, Kleber RJ, et al. The Impact of Recurrent Disasters on Mental Health: A Study on Seasonal Floods in Northern India. 2018. [DOI] [PubMed]
- 72. Torti J. Floods in Southeast Asia: a health priority. J Glob Health 2012;2:020304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lee Poyi CU of HK Impact of Floods in China: An Update Literature Review. In: The 13th World Congress on Public Health. 2012. p. 10105.
- 74. Ray-Bennett NS. The influence of caste, class and gender in surviving multiple disasters: A case study from Orissa, India. Environ Hazards 2009;8:5–22. [Google Scholar]
- 75. Van Minh H, Tuan Anh T, Rocklöv J, et al. Primary healthcare system capacities for responding to storm and flood-related health problems: a case study from a rural district in central Vietnam. Glob Health Action 2014;7:23007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Chan EYY, Kim J. Chronic health needs immediately after natural disasters in middle-income countries: the case of the 2008 Sichuan, China earthquake. Eur J Emerg Med 2011;18:111–4. [DOI] [PubMed] [Google Scholar]
- 77. der Heide EA. The importance of evidence-based disaster planning. Ann Emerg Med 2006;47:34–49. [DOI] [PubMed] [Google Scholar]
- 78. Mäkinen TH, Miettinen SM, Kernohan WG. Mental well-being considerations in preparation for disaster health care: learning from deployment. Prehosp Disaster Med 2015;30:327–36. [DOI] [PubMed] [Google Scholar]
- 79. Hall S, Harris R, Diannitta Agustinawati B, et al. Awareness of Tsunami natural warning signs and intended evacuation behaviors in Java, Indonesia. Nat Hazards 2017;89:473–96. [Google Scholar]
- 80. Shklovski I, Palen L, Sutton J Finding community through information and communication technology in disaster response. In: Proceedings of the ACM 2008 conference on Computer supported cooperative work - CSCW’08. New York, New York, USA: ACM Press; 2008. p. 127.
- 81. Pascapurnama DN, Murakami A, Chagan-Yasutan H, et al. Prevention of tetanus outbreak following natural disaster in Indonesia: lessons learned from previous disasters. Tohoku J Exp Med 2016;238:219–27. [DOI] [PubMed] [Google Scholar]
- 82. Hall ML, Lee ACK, Cartwright C, et al. The 2015 Nepal earthquake disaster: lessons learned one year on. Public Health 2017;145:39–44. [DOI] [PubMed] [Google Scholar]
- 83. Abdulli MA, Samieifard R, Jalili Ghazi Zade M. Rural solid waste management. Int J Environ Res 2008;2:425–30. [Google Scholar]
- 84. Han Z, Liu D, Lei Y, et al. Characteristics and management of domestic waste in the rural area of Southwest China. Waste Manag Res 2015;33:39–47. [DOI] [PubMed] [Google Scholar]
- 85. Pan A. Study on mobility-disadvantage group’ risk perception and coping behaviors of abrupt geological hazards in coastal rural area of China. Environ Res 2016;148:574–81. [DOI] [PubMed] [Google Scholar]
- 86. Kun P, Tong X, Liu Y, et al. What are the determinants of post-traumatic stress disorder: age, gender, ethnicity or other? Evidence from 2008 Wenchuan earthquake. Public Health 2013;127:644–52. [DOI] [PubMed] [Google Scholar]
- 87. Tobin S. A Global Outlook on Disaster Science. 2018.
- 88. Aitsi-Selmi A, Murray V, Heymann D, et al. Reducing risks to health and wellbeing at mass gatherings: the role of the Sendai Framework for Disaster Risk Reduction. Int J Infect Dis 2016;47:101–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Houston KA, Gibb JG, Maitland K, et al. Oral rehydration of malnourished children with diarrhoea and dehydration: a systematic review [version 3; referees: 2 approved]. Wellcome Open Res 2017;1:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Heagele TN. Lack of evidence supporting the effectiveness of disaster supply kits. Am J Public Health 2016;106:979–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Quevillon RP, Gray BL, Erickson SE, et al. Helping the helpers: assisting staff and volunteer workers before, during, and after disaster relief operations. J Clin Psychol 2016;72:1348–63. [DOI] [PubMed] [Google Scholar]
- 92. Mimura N, Yasuhara K, Kawagoe S, et al. Damage from the Great East Japan Earthquake and Tsunami—a quick report. Mitig Adapt Strateg Glob Chang 2011;16:803–18. [Google Scholar]
- 93. Ansari M. A survey of mothers’ knowledge about childhood diarrhoea and its management among a marginalised community of Morang, Nepal. Australas Med J 2011;4:474–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Fox JH, Burkle FM, Bass J, et al. The effectiveness of psychological first aid as a disaster intervention tool: research analysis of peer-reviewed literature from 1990–2010. Disaster Med Public Heal Prep 2012;6:247–52. [DOI] [PubMed] [Google Scholar]
- 95. Yarali A, Ahsant B, Rahman S Wireless Mesh Networking: A Key Solution for Emergency & Rural Applications. In: 2009 Second International Conference on Advances in Mesh Networks. IEEE; 2009. p. 143–9.