Abstract
Objective:
The Diabetes Early Re-admission Risk Indicator (DERRI™) was previously developed and internally validated as a tool to predict the risk of all-cause re-admission within 30 days of discharge (30-day re-admission) of hospitalized patients with diabetes. In this study, the predictive performance of the DERRI™ with and without additional predictors was assessed in an external sample.
Methods:
We conducted a retrospective cohort study of adult patients with diabetes discharged from two academic medical centers between January 1, 2000 and December 31, 2014. We applied the previously developed DERRI™, which includes admission laboratory results, sociodemographics, a diagnosis of certain comorbidities, and recent discharge information, and evaluated the effect of adding metabolic indicators on predictive performance using multivariable logistic regression. Total cholesterol (TC) and hemoglobin A1c (A1c) were selected based on clinical relevance and univariate association with 30-day re-admission.
Results:
Among 105,974 discharges, 19,032 (18.0%) were followed by 30-day re-admission for any cause. The DERRI™ had a C-statistic of 0.634 for 30-day re-admission. TC was the lipid parameter most strongly associated with 30-day re-admission. The DERRI™ predictors A1c and TC were significantly associated with 30-day re-admission; however, their addition to the DERRI™ did not significantly change model performance (C-statistic, 0.643 [95% confidence interval, 0.638 to 0.647]; P = .92).
Conclusion:
Performance of the DERRI™ in this external cohort was modest but comparable to other re-admission prediction models. Addition of A1c and TC to the DERRI™ did not significantly improve performance. Although the DERRI™ may be useful to direct resources toward diabetes patients at higher risk, better prediction is needed.
Keywords: diabetes, hospital, readmission risk prediction
INTRODUCTION
Hospital re-admission within 30 days of discharge (30-day re-admission) is a high-priority healthcare quality measure and target for cost reduction (1–3). More than a quarter of hospital expenditures in the United States are incurred by patients with diabetes (4). In this population, up to 20% of hospitalizations are followed by a 30-day re-admission (5–10), corresponding to nearly 2 million discharges annually (11).
Interventions aimed at reducing the risk of 30-day re-admission of various populations tend to be more effective when focused on higher-risk patients (12,13); however, approaches tailored to patients with diabetes are needed (14). We therefore previously developed and internally validated the Diabetes Early Re-admission Risk Indicator (DERRI™) (10), a model to predict the risk of all-cause 30-day re-admission in hospitalized patients with diabetes based on easily obtained clinical and sociodemographic information available before hospital discharge. The DERRI™ identifies patients with diabetes at higher risk for 30-day re-admission, providing guidance for a targeted approach to interventions and enabling more efficient use of resources.
An important step in evaluating the generalizability of a predictive model is to test the model in a sample different from the one used to develop the model (i.e., external validation) (15). Herein, we present an external validation of the DERRI™ tool. In addition, we examined the effect of adding metabolic parameters (hemoglobin A1c [A1c] and cholesterol levels) on predictive performance. These parameters, which were not available in the data for the development of the DERRI™, are routinely collected on patients with diabetes, yet their association with re-admission is unclear for A1c (conflicting studies) (16,17) and unknown for cholesterol.
METHODS
Study Sample
The methods used to select the cohort (external validation sample), define variables, and analyze the data were similar to those used to develop the DERRI™ (10). A total of 105,960 hospital discharges were retrospectively selected from the electronic medical records of 42,800 patients hospitalized at two urban academic medical centers in Boston, Massachusetts (Massachusetts General Hospital and Brigham and Women’s Hospital) between January 1, 2000, and December 31, 2014, the time period for which data were available. Patients were included based on a diagnosis of diabetes defined by an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code of 250.xx associated with a hospital discharge and receiving a diabetes-specific medication during that hospitalization. Index discharges of these patients were included based on a diagnosis of diabetes (ICD-9-CM code 250.xx) associated with hospital discharge or the presence of a diabetes-specific medication on the pre-admission medication list. Index discharges were excluded for patients aged less than 21 years on the date of admission, discharge by transfer to another hospital, discharge from an obstetric service (indicating pregnancy), inpatient death, outpatient death within 30 days of discharge, incomplete data or lacking 30 days of follow-up after discharge (discharged after December 1, 2014). All eligible index discharges were included in the analysis. Data from nonindex hospitalizations at three local community hospitals in the Partners HealthCare network were included in the assessment of covariates and re-admissions.
The Partners HealthCare and Temple University Institutional Review Boards approved the protocol. A waiver of informed consent was obtained for this large retrospective study.
Definition of Variables
The outcome to be predicted by the model was all-cause re-admission within 30 days of an index discharge. A total of 15 variables were evaluated as predictors of the outcome. The current dataset includes data on all 10 variables in the DERRI™, which were having a home zip code less than 5 miles from the hospital, employment status, pre-admission insulin use (yes or no), a diagnosis of one or more macrovascular diabetes complications, a diagnosis of anemia, admission hematocrit level, serum creatinine level, serum sodium level, having a discharge within 90 days before admission, and most recent discharge status up to 1 year before admission (discharge against medical advice, home, home with nursing care, to a subacute facility, or no discharge) (10). In addition to these 10 variables, total cholesterol, high-density-lipoprotein cholesterol (HDL-C), low-density-lipoprotein cholesterol (LDL-C), triglycerides, and A1c levels were evaluated for association with re-admission. For these new variables, the value closest to the admission date between 1 year before admission and up to discharge was used. In order to capture nonlinear associations with re-admission, the new variables were categorized into normal, high, and low values. Variables based on ICD-9-CM codes (current or prior diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome, microvascular complications, macrovascular complications, schizophrenia or mood disorder, gastroparesis, pancreatitis, hypertension, chronic obstructive pulmonary disease or asthma, cardiac dysrhythmia, malignant neoplasm, and anemia) were considered for ever occurrence (during or before the index hospitalization) or current occurrence during the index hospitalization.
Statistical Analysis
Summaries of continuous variables included means and standard deviations or medians and interquartile ranges, while counts and percentages were used for categorical variables. To account for clusters of multiple hospitalizations per patient, univariate logistic regression with the generalized estimating equations (GEE) approach was used to model the association of each predictor with 30-day re-admission (18). In addition, distributions of characteristics of the external validation sample were compared to the previously published internal validation sample using univariate logistic regression with GEE (10). A1c, total cholesterol, HDL-C, LDL-C, and triglycerides were categorized by clinically relevant cut-points and analyzed for univariate association with 30-day re-admission by chi-square. Total cholesterol was found to have the strongest association with re-admission among the lipid parameters and therefore selected for multivariable modeling. A1c was selected for multivariable modeling based on univariate statistical significance as well as clinical relevance.
Multivariable logistic regression with GEE was performed to determine the adjusted associations of the variables with all-cause 30-day re-admission. Data generated by three multivariable models are presented. The first is the previously published DERRI™, which was applied to the current external validation sample. The second is a model developed in the current study sample using the 10 DERRI™ variables to directly assess the effect of adding additional variables on model performance. The third model, also developed in the current sample, uses the DERRI™ variables plus total cholesterol and A1c.
Comparative performance of the models in the external and internal validation samples was assessed by discrimination, the ability of the model to distinguish high-risk from low-risk individuals (15). Discrimination was evaluated using the C-statistic (equivalent to the area under the receiver operating characteristic curve), a standard measure of the predictive accuracy of a logistic regression model, where higher values represent better discrimination (19). In addition, patients were stratified into quintiles of 30-day re-admission risk using the models to predict each patient’s risk of re-admission as a number between 0 and 100%.
Because 46% of discharges were missing either total cholesterol or A1c values, a sensitivity analysis was performed only on discharges associated with complete A1c and cholesterol data.
SAS version 9.4 (SAS Institute, Cary, NC) was used for all analyses. A P value less than .05 was considered statistically significant.
RESULTS
There were 105,960 discharges in this external validation sample, of which 19,032 (18.0%) were associated with 30-day re-admission for any cause. Characteristics of the cohort are presented in Table 1. With the exception of gender, English fluency, and insurance status, most of the variables were associated with 30-day re-admission in univariate analysis. The most common reasons for re-admission were cardiovascular disease, infection, and diabetes (Table 2).
Table 1.
Characteristics of Hospitalized Patients With Diabetes in External Validation Sample by 30-Day Re-admission
| Variable | All discharges N = 105,960 | Followed by re-admission n = 19,032 | No re-admission n = 86,928 | P value |
|---|---|---|---|---|
| Age | <.0001 | |||
| <50 years | 6,857 (6.5) | 1,465 (7.7) | 5,392 (6.2) | |
| 50–59 years | 12,971 (12.2) | 2,646 (13.9) | 10,325 (11.9) | |
| 60–69 years | 25,989 (24.5) | 5,076 (26.7) | 20,913 (24.1) | |
| 70+ years | 60,143 (56.8) | 9,845 (51.7) | 50,298 (57.9) | |
| Gender | .55 | |||
| Female | 47,940 (45.2) | 8,554 (45.0) | 39,386 (45.3) | |
| Male | 58,020 (54.8) | 10,478 (55.1) | 47,542 (54.7) | |
| Weight, kg, mean (SD) | 85.9 (20.41) | 85.0 (20.78) | 86.1 (20.32) | <.0001 |
| Marital status | .02 | |||
| Married | 49,165 (46.4) | 8,605 (45.2) | 40,560 (46.7) | |
| Single | 52,716 (49.8) | 9,730 (51.1) | 42,986 (49.5) | |
| Other or not recorded | 4,079 (3.9) | 697 (3.7) | 3,382 (3.9) | |
| Race/ethnicity | .001 | |||
| Black | 11,330 (10.7) | 2,083 (10.9) | 9,247 (10.6) | |
| Hispanic | 5,914 (5.6) | 1,238 (6.5) | 4,676 (5.4) | |
| White | 78,000 (73.6) | 13,785 (72.4) | 64,215 (73.9) | |
| Other | 5,951 (5.6) | 1,135 (6.0) | 4,816 (5.5) | |
| Not recorded | 4,765 (4.5) | 791 (4.2) | 3,974 (4.6) | |
| English speaking | .35 | |||
| Yes | 92,887 (87.7) | 16,624 (87.4) | 76,263 (87.7) | |
| No | 13,073 (12.3) | 2,408 (12.7) | 10,665 (12.3) | |
| Insurance status | .22 | |||
| Medicaid | 1,834 (1.7) | 332 (1.7) | 1,502 (1.7) | |
| Medicare | 52,913 (49.9) | 9,445 (49.6) | 43,468 (50.0) | |
| None | 12,150 (11.5) | 2,295 (12.1) | 9,855 (11.3) | |
| Private | 39,063 (36.9) | 6,960 (36.6) | 32,103 (36.9) | |
| Home zip code | <.0001 | |||
| ≥5 miles from hospital | 73,372 (69.2) | 12,662 (66.5) | 60,710 (69.8) | |
| <5 miles from hospital | 32,588 (30.8) | 6,370 (33.5) | 26,218 (30.2) | |
| Educational level | .026 | |||
| Less than high school | 12,575 (11.9) | 2,361 (12.4) | 10,214 (11.8) | |
| Any high school | 28,047 (26.5) | 5,209 (27.4) | 22,838 (26.3) | |
| Some College | 4,324 (4.1) | 748 (3.9) | 3,576 (4.1) | |
| College Graduate | 19,156 (18.1) | 3,277 (17.2) | 15,879 (18.3) | |
| Not recorded | 41,858 (39.5) | 7,437 (39.1) | 34,421 (39.6) | |
| Employment | <.0001 | |||
| Disabled | 14,446 (13.6) | 3,291 (17.3) | 11,155 (12.8) | |
| Employed | 18,218 (17.2) | 2,787 (14.6) | 15,431 (17.8) | |
| Retired | 40,057 (37.8) | 7,099 (37.3) | 32,958 (37.9) | |
| Unemployed | 6,755 (6.4) | 1,419 (7.5) | 5,336 (6.1) | |
| Other or not recorded | 26,484 (25.0) | 4,436 (23.3) | 22,048 (25.4) | |
| Pre-admission sulfonylurea use | <.0001 | |||
| Yes | 15,722 (14.8) | 2,419 (12.7) | 13,303 (15.3) | |
| No | 90,238 (85.2) | 16,613 (87.3) | 73,625 (84.7) | |
| Pre-admission metformin use | <.0001 | |||
| Yes | 21,355 (20.2) | 3,067 (16.1) | 18,288 (21.0) | |
| No | 84,605 (79.9) | 15,965 (83.9) | 68,640 (79.0) | |
| Pre-admission thiazolidinedione use | <.0001 | |||
| Yes | 2,848 (2.7) | 375 (2.0) | 2,473 (2.8) | |
| No | 103,112 (97.3) | 18,657 (98.0) | 84,455 (97.2) | |
| Pre-admission insulin use | <.0001 | |||
| Yes | 37,851 (35.7) | 7,306 (38.4) | 30,545 (35.1) | |
| No | 68,109 (64.3) | 11,726 (61.6) | 56,383 (64.9) | |
| Pre-admission glucocorticoid use | <.0001 | |||
| Yes | 11,793 (11.1) | 2,598 (13.7) | 9,195 (10.6) | |
| No | 94,167 (88.9) | 16,434 (86.4) | 77,733 (89.4) | |
| Current or prior DKA or HHS | .0043 | |||
| Yes | 4,247 (4.0) | 903 (4.7) | 3,344 (3.9) | |
| No | 101,713 (96.0) | 18,129 (95.3) | 83,584 (96.2) | |
| Microvascular complicationsa | <.0001 | |||
| 0 | 74,613 (70.4) | 12,029 (63.2) | 62,584 (72.0) | |
| 1 | 18,499 (17.5) | 3,769 (19.8) | 14,730 (17.0) | |
| 2 | 7,952 (7.5) | 1,962 (10.3) | 5,990 (6.9) | |
| 3 | 4,896 (4.6) | 1,272 (6.7) | 3,624 (4.2) | |
| Macrovascular complicationsb | <.0001 | |||
| 0 | 37,233 (35.1) | 6,192 (32.5) | 31,041 (35.7) | |
| 1 | 31,312 (29.6) | 5,030 (26.4) | 26,282 (30.2) | |
| 2 | 25,683 (24.2) | 4,986 (26.2) | 20,697 (23.8) | |
| 3 | 9,285 (8.8) | 2,201 (11.6) | 7,084 (8.2) | |
| 4 | 2,447 (2.3) | 623 (3.3) | 1,824 (2.1) | |
| Pre-admission BP meds | <.0001 | |||
| None | 45,840 (43.3) | 8,230 (43.2) | 37,610 (43.3) | |
| ACE-i or ARB | 38,371 (36.2) | 6,319 (33.2) | 32,052 (36.9) | |
| Non-ACE or ARB | 21,749 (20.5) | 4,483 (23.6) | 17,266 (19.9) | |
| Pre-admission statin use | .0024 | |||
| Yes | 45,183 (42.6) | 7,856 (41.3) | 37,327 (42.9) | |
| No | 60,777 (57.4) | 11,176 (58.7) | 49,601 (57.1) | |
| White blood cell count | <.0001 | |||
| Low <4 K/μL | 4,141 (3.9) | 961 (5.1) | 3,180 (3.7) | |
| Normal 4–11 K/μL | 68,237 (64.4) | 12,182 (64.0) | 56,055 (64.5) | |
| High >11 K/μL | 33,582 (31.7) | 5,889 (30.9) | 27,693 (31.9) | |
| Hematocrit, %, mean (SD) | 35.5 (5.63) | 34.5 (5.63) | 35.7 (5.61) | <.0001 |
| Serum sodium | <.0001 | |||
| Low <135 mmol/L | 27,048 (25.5) | 5,462 (28.7) | 21,586 (24.8) | |
| Normal 135–145 mmol/L | 77,703 (73.3) | 13,318 (70.0) | 64,385 (74.1) | |
| High >145 mmol/L | 1,209 (1.1) | 252 (1.3) | 957 (1.1) | |
| Serum potassium | <.0001 | |||
| Low <3.1 mmol/L | 1,866 (1.8) | 369 (1.9) | 1,497 (1.7) | |
| Normal 3.1–5.3 mmol/L | 96,074 (90.7) | 16,921 (88.9) | 79,153 (91.1) | |
| High >5.3 mmol/L | 8,020 (7.6) | 1,742 (9.2) | 6,278 (7.2) | |
| Creatinine, mg/dL, median (IQR) | 1.2 (0.9–1.7) | 1.3 (0.9–2.1) | 1.2 (0.9–1.7) | <.0001 |
| Discharged 90 days prior to index admission | <.0001 | |||
| Yes | 32,451 (30.6) | 8,970 (47.1) | 23,481 (27.0) | |
| No | 73,509 (69.4) | 10,062 (52.9) | 63,447 (73.0) | |
| Length-of-stay, days, median (IQR) | 5.0 (3.0–8.0) | 5.0 (3.0–9.0) | 5.0 (3.0–8.0) | <.0001 |
| Discharge status of index admission | <.0001 | |||
| Home | 21,424 (20.2) | 3,539 (18.6) | 17,885 (20.6) | |
| Home with nursing care | 38,789 (36.6) | 7,006 (36.8) | 31,783 (36.6) | |
| Sub-acute facility | 21,853 (20.6) | 3,990 (21.0) | 17,863 (20.6) | |
| Against medical advice | 803 (0.8) | 208 (1.1) | 595 (0.7) | |
| Other | 1,219 (1.2) | 203 (1.1) | 1,016 (1.2) | |
| No status recorded | 21,872 (20.6) | 4,086 (21.5) | 17,786 (20.5) | |
| Discharge 1 year prior to index admission | <.0001 | |||
| Home | 10,779 (10.2) | 2,503 (13.2) | 8,276 (9.5) | |
| Home with nursing care | 18,419 (17.4) | 4,531 (23.8) | 13,888 (16.0) | |
| Subacute facility | 10,016 (9.5) | 2,358 (12.4) | 7,658 (8.8) | |
| Against medical advice | 441 (0.4) | 129 (0.7) | 312 (0.4) | |
| No discharge recorded | 66,305 (62.6) | 9,511 (50.0) | 56,794 (65.3) | |
| Body mass index | <.0001 | |||
| <18.5 kg/m2 | 1,595 (1.5) | 361 (1.9) | 1,234 (1.4) | |
| 18.5–24.9 kg/m2 | 17,140 (16.2) | 3,593 (18.9) | 13,547 (15.6) | |
| 25.0–29.9 kg/m2 | 32,719 (30.9) | 5,688 (29.9) | 27,031 (31.1) | |
| ≥30.0 kg/m2 | 54,506 (51.4) | 9,390 (49.3) | 45,116 (51.9) | |
| Depression or psychosis ever | <.0001 | |||
| Yes | 22,506 (21.2) | 4,877 (25.6) | 17,629 (20.3) | |
| No | 83,454 (78.8) | 14,155 (74.4) | 69,299 (79.7) | |
| Gastroparesis ever | <.0001 | |||
| Yes | 3,415 (3.2) | 996 (5.2) | 2,419 (2.8) | |
| No | 102,545 (96.8) | 18,036 (94.8) | 84,509 (97.2) | |
| Pancreatitis ever | <.0001 | |||
| Yes | 4,482 (4.2) | 1,071 (5.6) | 3,411 (3.9) | |
| No | 101,478 (95.8) | 17,961 (94.4) | 83,517 (96.1) | |
| Hypertension ever | .03 | |||
| Yes | 74,179 (70.0) | 13,145 (69.1) | 61,034 (70.2) | |
| No | 31,781 (30.0) | 5,887 (30.9) | 25,894 (29.8) | |
| COPD or asthma ever | <.0001 | |||
| Yes | 16,325 (15.4) | 3,394 (17.8) | 12,931 (14.9) | |
| No | 89,635 (84.6) | 15,638 (82.2) | 73,997 (85.1) | |
| Cardiac dysrhythmias ever | <.0001 | |||
| Yes | 35,664 (33.7) | 7,090 (37.3) | 28,574 (32.9) | |
| No | 70,296 (66.3) | 11,942 (62.8) | 58,354 (67.1) | |
| Malignant neoplasm ever | <.0001 | |||
| Yes | 18,741 (17.7) | 4,279 (22.5) | 1,4462 (16.6) | |
| No | 87,219 (82.3) | 14,753 (77.5) | 72,466 (83.4) | |
| Anemia ever | <.0001 | |||
| Yes | 41,868 (39.5) | 9,239 (48.5) | 32,629 (37.5) | |
| No | 64,092 (60.5) | 9,793 (51.5) | 54,299 (62.5) | |
| Hemoglobin A1c | <.0001 | |||
| Low <6.5% (48 mmol/mol) |
21,338 (20.1) | 4,302 (22.6) | 17,036 (19.6) | |
| Controlled 6.5–8% (48–64 mmol/mol) |
32,459 (30.6) | 5,874 (30.9) | 26,585 (30.6) | |
| High >8.0% (65 mmol/mol) |
23,690 (22.4) | 4,178 (22.0) | 19,512 (22.5) | |
| Unknown | 28,473 (26.9) | 4,678 (24.6) | 23,795 (27.4) | |
| Total cholesterol | <.0001 | |||
| Low <150 mg/dL | 33,704 (31.8) | 6,893 (36.2) | 26,811 (30.8) | |
| Normal 150–200 mg/dL | 22,041 (20.8) | 3,844 (20.2) | 18,197 (20.9) | |
| High >200 mg/dL | 9,117 (8.6) | 1,621 (8.5) | 7,496 (8.6) | |
| Unknown | 41,098 (38.8) | 6,674 (35.1) | 34,424 (39.6) | |
| LDL-C | <.0001 | |||
| Low <70 mg/dL | 26,001 (24.5) | 5,352 (28.1) | 20,649 (23.8) | |
| Normal 70–100 mg/dL | 21,163 (20.0) | 3,788 (19.9) | 17,375 (20.0) | |
| High >100 mg/dL | 14,392 (13.6) | 2,568 (13.5) | 11,824 (13.6) | |
| Unknown | 44,404 (41.9) | 7,324 (38.5) | 37,080 (42.7) | |
| HDL-C | <.0001 | |||
| Low <70 mg/dL | 30,299 (28.6) | 5,895 (31.0) | 24,404 (28.1) | |
| Normal 70–100 mg/dL | 24,797 (23.4) | 4,471 (23.5) | 20,326 (23.4) | |
| High >100 mg/dL | 6,378 (6.0) | 1,181 (6.2) | 5,197 (6.0) | |
| Unknown | 44,486 (42.0) | 7,485 (39.3) | 37,001 (42.6) | |
| Triglycerides | <.0001 | |||
| Low <100 mg/dL | 20,722 (19.6) | 4,120 (21.7) | 16,602 (19.1) | |
| Normal 100–150 mg/dL | 18,969 (17.9) | 3,523 (18.5) | 15,446 (17.8) | |
| High >150 mg/dL | 25,657 (24.2) | 4,896 (25.7) | 20,761 (23.9) | |
| Unknown | 40,612 (38.3) | 6,493 (34.1) | 34,119 (39.3) | |
Abbreviations: ACE = angiotensin-converting enzyme; ACE-i = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker; BP = blood pressure; COPD = chronic obstructive pulmonary disease; DKA = diabetic ketoacidosis; HDL-C = high-density-lipoprotein cholesterol; HHS = hyperglycemic hyperosmolar syndrome; IQR = interquartile range; LDL-C = low-density-lipoprotein cholesterol.
Data are n, (%) unless otherwise noted.
Retinopathy, neuropathy, nephropathy.
Coronary artery disease, heart failure, stroke, peripheral vascular disease; ever = current or prior.
Table 2.
Most Common Reasons for Re-admission Based on Primary ICD-9-CM Code
| ICD-9-CM Codea | Description | n (% of re-admissions) |
|---|---|---|
| 414, 410, 440 | Chronic ischemic heart disease, acute myocardial infarction, atherosclerosis | 1,666 (8.8) |
| 599.xx, 486.xx, 682.xx, 0.38.xx, 008.xx | Urinary tract infection, pneumonia, cellulitis, abscess, septicemia, intestinal infection | 1,547 (8.1) |
| 428.xx | Heart failure | 1,443 (7.6) |
| 250.xx | Diabetes mellitus | 1,167 (6.1) |
| 996.xx | Complication or infection of device, implant, graft, or indwelling urinary catheter | 1,105 (5.8) |
| 998.xx, 997.49, 997.6x | Postoperative complication, including infection, bleeding, and disruption of surgical woundb | 677 (3.6) |
| 577.xx, 572.xx, 578.xx, 560.xx | Disease of pancreas, liver abscess, chronic liver disease, gastrointestinal hemorrhage, intestinal obstruction | 670 (3.5) |
| 584.xx, 403.xx | Acute kidney failure, hypertensive kidney disease | 576 (3.0) |
| V58.1 | Antineoplastic chemotherapy and immunotherapy | 496 (2.6) |
| 786.5x, 786.0x | Chest pain, shortness of breath | 370 (1.9) |
Abbreviation: ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification.
Listed in order of frequency.
Excludes 998.89, other postoperative or blood transfusion complications, which was 0.03% of re-admissions.
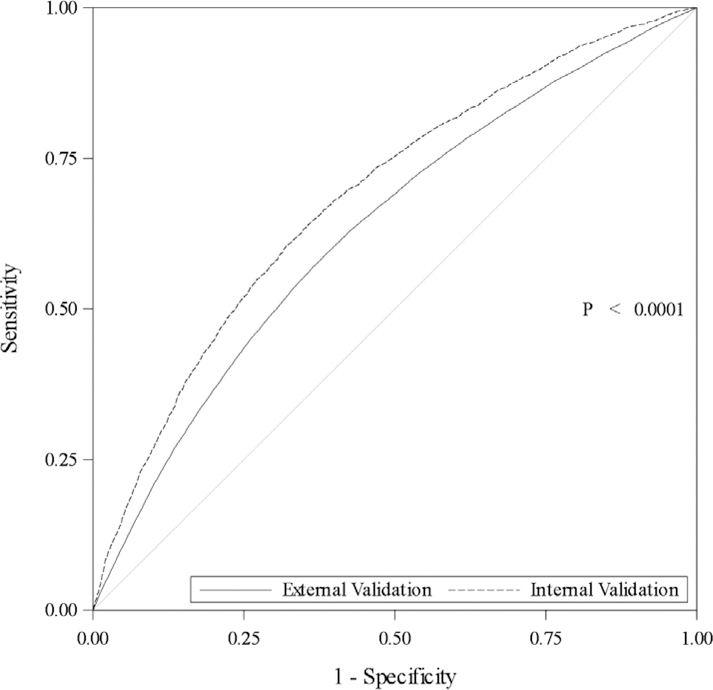
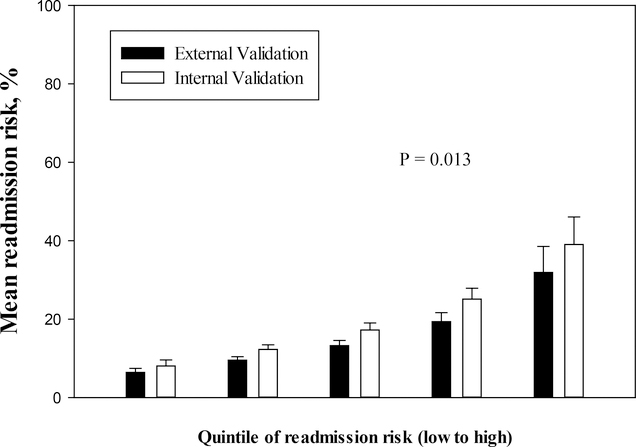
The C-statistic of the DERRI™ was 0.634 (95% confidence interval [CI], 0.629 to 0.638) in the external validation sample and 0.686 (95% CI, 0.677 to 0.696) in the previously published internal validation sample (P<.0001, Fig. 1 A) (10). Quintiles of mean predicted all-cause 30-day re-admission risk based on the DERRI™ were statistically significantly different between the external and internal validation samples (overall P = .013, Fig. 2 A). For example, the highest quintile had a 32 ± 7% risk of 30-day re-admission in the external validation sample and a 39 ± 7% risk in the internal validation sample.
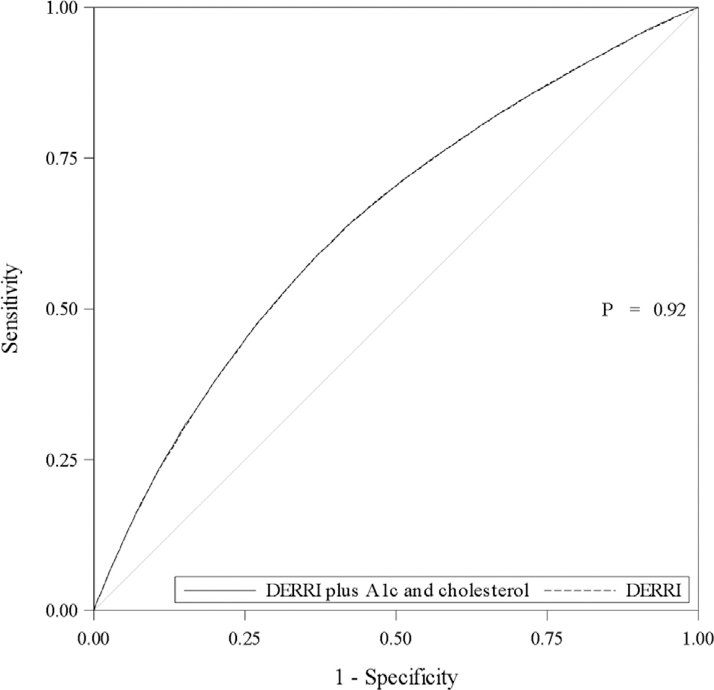
Fig. 1.
(A) Receiver operating characteristic (ROC) curves of all-cause 30-day re-admission predicted by the Diabetes Early Re-admission Risk Indicator (DERRI™) in internal and external validation samples. (B) ROC curves of all-cause 30-day re-admission predicted by the DERRI™ and DERRI™ plus hemoglobin A1c and total cholesterol in external validation sample.
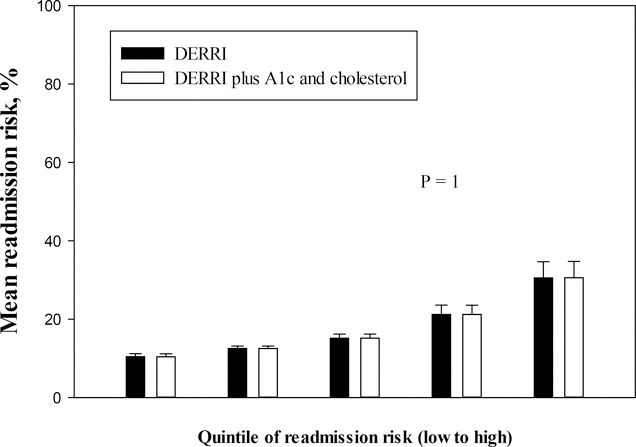
Fig. 2.
(A) Quintiles of all-cause 30-day re-admission risk predicted by the Diabetes Early Re-admission Risk Indicator (DERRI™) in internal and external validation samples. (B) Quintiles of all-cause 30-day re-admission risk predicted by the DERRI™ and DERRI™ plus hemoglobin A1c and total cholesterol in external validation sample.
Relationships of the DERRI™ predictors with 30-day re-admission were either attenuated or relatively unchanged by adding Alc and total cholesterol to the model (Table 3) (10). A hospital discharge within 90 days before the index admission remained the strongest predictor and was associated with nearly 2-fold greater odds of 30-day re-admission. Other relatively strong factors were status of the most recent prior hospital discharge and employment status. Unexpectedly, an A1c <6.5% (48 mmol/mol) and a total cholesterol <150 mg/dL were associated with higher odds of re-admission (1.06 [95% CI, 1.00 to 1.11] and 1.07 [95% CI, 1.01 to 1.12]). The only difference in the direction of associations generated by the model with Alc and total cholesterol versus the DERRI™ was found with the number of macrovascular complications. In the current model, having only one complication was associated with a 9% lower odds of re-admission and three or four complications with 9% or 14% higher odds of readmission, respectively, whereas in the DERRI™, an increasing number of macrovascular complications was associated with a progressively higher odds of re-admission.
Table 3.
Predictors of All-Cause 30-Day Re-admission According to DERRI™ Plus Hemoglobin A1c and Cholesterol in External Validation Sample
| Predictor | Odds ratio (95% CI) | P value |
|---|---|---|
| Home zip code <5 miles from hospital | 1.06 (1.02–1.11) | .0085 |
| Employment status (vs. employed) | ||
| Disabled | 1.36 (1.26–1.46) | <.0001 |
| Retired | 1.05 (0.99–1.12) | .093 |
| Unemployed | 1.35 (1.23–1.49) | <.0001 |
| Other or not recorded | 1.03 (0.96–1.10) | .39 |
| Pre-admission insulin use | 1.04 (1.00–1.09) | .041 |
| Macrovascular complicationsa, n (vs. 0) | ||
| 1 | 0.91 (0.86–0.96) | .0002 |
| 2 | 0.99 (0.94–1.04) | .67 |
| 3 | 1.09 (1.02–1.17) | .016 |
| 4 | 1.14 (0.99–1.30) | .067 |
| Admission hematocrit, per 5% | 0.91 (0.89–0.93) | <.0001 |
| Log (admission serum creatinine) | 1.19 (1.15–1.23) | <.0001 |
| Admission serum sodium (vs. normal) | ||
| Low, <135 mmol/L | 1.11 (1.06–1.15) | <.0001 |
| High, >145 mmol/L | 1.25 (1.08–1.45) | .0028 |
| Discharged within 90 days before admission | 1.89 (1.80–1.98) | <.0001 |
| Most recent discharge status up to 1 year before admission (vs. home) | ||
| Against medical advice | 1.23 (0.97–1.56) | .089 |
| Home with nursing care | 1.06 (1.00–1.14) | .068 |
| No discharge recorded | 0.87 (0.81–0.92) | <.0001 |
| Subacute facility | 0.96 (0.89–1.04) | .37 |
| Anemia, current or prior diagnosis | 1.12 (1.08–1.17) | <.0001 |
| Hemoglobin A1c (vs. 6.5–8.0%) | ||
| <6.5% | 1.06 (1.00–1.11) | .04 |
| >8.0% | 0.99 (0.94–1.05) | .84 |
| Unknown | 1.04 (0.99–1.10) | .14 |
| Total cholesterol (vs. 150–200 mg/dL) | ||
| <150 mg/dL | 1.07 (1.01–1.12) | .012 |
| >200 mg/dL | 1.04 (0.96–1.12) | .35 |
| Unknown | 1.00 (0.95–1.05) | .95 |
Abbreviation: DERRI™ = Diabetes Early Re-admission Risk Indicator.
Coronary artery disease, heart failure, stroke, peripheral vascular disease.
Addition of Alc and total cholesterol to the DERRI™ predictors did not significantly change model performance in terms of the C-statistic (0.643 [95% CI, 0.638 to 0.647]; P = .92, Fig. 1 B) or mean predicted 30-day re-admission risk (overall P>.999; Fig. 2 B). The highest quintile had a 31 ± 4% mean predicted risk of 30-day re-admission. In the sensitivity analysis performed using records with complete A1c or total cholesterol data, results were unchanged (data not shown). In a post-hoc exploratory analysis, pre-admission statin use was added to the model with A1c and total cholesterol. Neither the odds ratio for low total cholesterol nor the C-statistic changed.
Characteristics of the external and internal validation samples were statistically significantly different for most variables, including sociodemographics and clinical parameters (Table 4). The external validation sample was older, more married, more white, more privately insured, and lived further away from the index hospital than the internal validation sample. Among the 10 DERRI™ predictors, the distributions of seven predictors were statistically significantly different between the two samples.
Table 4.
Characteristics of Hospitalized Patients With Diabetes in Internal and External Validation Samples
| Variable | All discharges N = 123,761 | Internal validation n = 17,801 | External validation n = 105,960 | P value |
|---|---|---|---|---|
| Age | <.0001 | |||
| <50 years | 10,160 (8.2) | 3,303 (18.6) | 6,857 (6.5) | |
| 50–59 years | 17,190 (13.9) | 4,219 (23.7) | 12,971 (12.2) | |
| 60–69 years | 30,510 (24.7) | 4,521 (25.4) | 25,989 (24.5) | |
| 70+ years | 65,901 (53.3) | 5,758 (32.4) | 60,143 (56.8) | |
| Gender | <.0001 | |||
| Female | 56,951 (46.0) | 9,011 (50.6) | 47,940 (45.2) | |
| Male | 66,810 (54.0) | 8,790 (49.4) | 58,020 (54.8) | |
| Weight (kg), mean (SD) | 85.9 (20.41) | 85.0 (20.78) | 86.1 (20.32) | .0026 |
| Marital status | <.0001 | |||
| Married | 54,881 (44.3) | 5,716 (32.1) | 49,165 (46.4) | |
| Single | 64,458 (52.1) | 11,742 (66.0) | 52,716 (49.8) | |
| Other or not recorded | 4,422 (3.6) | 343 (1.9) | 4,079 (3.9) | |
| Race/ethnicity | <.0001 | |||
| Black | 19,269 (15.6) | 7,939 (44.6) | 11,330 (10.7) | |
| Hispanic | 8,572 (6.9) | 2,658 (14.9) | 5,914 (5.6) | |
| White | 84,032 (67.9) | 6,032 (33.9) | 78,000 (73.6) | |
| Other | 6,932 (5.6) | 981 (5.5) | 5,951 (5.6) | |
| Not recorded | 4,956 (4.0) | 191 (1.1) | 4,765 (4.5) | |
| English speaking | <.0001 | |||
| Yes | 107,258 (86.7) | 14,371 (80.7) | 92,887 (87.7) | |
| No | 16,503 (13.3) | 3,430 (19.3) | 13,073 (12.3) | |
| Insurance status | <.0001 | |||
| Medicaid | 5,914 (4.8) | 4,080 (22.9) | 1,834 (1.7) | |
| Medicare | 61,731 (49.9) | 8,818 (49.5) | 52,913 (49.9) | |
| None | 13,033 (10.5) | 883 (5.0) | 12,150 (11.5) | |
| Private | 43,083 (34.8) | 4,020 (22.6) | 39,063 (36.9) | |
| Home zip coded | <.0001 | |||
| ≥5 miles from hospital | 78,942 (63.8) | 5,570 (31.3) | 73,372 (69.2) | |
| <5 miles from hospital | 44,819 (36.2) | 12,231 (68.7) | 32,588 (30.8) | |
| Educational level | <.0001 | |||
| Less than high school | 15,115 (12.2) | 2,540 (14.3) | 12,575 (11.9) | |
| Any high school | 37,618 (30.4) | 9,571 (53.8) | 28,047 (26.5) | |
| Some college | 5,472 (4.4) | 1,148 (6.5) | 4,324 (4.1) | |
| College graduate | 21,960 (17.7) | 2,804 (15.8) | 19,156 (18.1) | |
| Not recorded | 43,596 (35.2) | 1,738 (9.8) | 41,858 (39.5) | |
| Employmentd | <.0001 | |||
| Disabled | 18,129 (14.7) | 3,683 (20.7) | 14,446 (13.6) | |
| Employed | 19,964 (16.1) | 1,746 (9.8) | 18,218 (17.2) | |
| Retired | 47,047 (38.0) | 6,990 (39.3) | 40,057 (37.8) | |
| Unemployed | 11,574 (9.4) | 4,819 (27.1) | 6,755 (6.4) | |
| Other or not recorded | 27,047 (21.9) | 563 (3.2) | 26,484 (25.0) | |
| Pre-admission sulfonylurea use | .039 | |||
| Yes | 18,580 (15.0) | 2,858 (16.1) | 15,722 (14.8) | |
| No | 105,181 (85.0) | 14,943 (83.9) | 90,238 (85.2) | |
| Pre-admission metformin use | <.0001 | |||
| Yes | 26,368 (21.3) | 5,013 (28.2) | 21,355 (20.2) | |
| No | 97,393 (78.7) | 12,788 (71.8) | 84,605 (79.9) | |
| Pre-admission thiazolidinedione use | <.0001 | |||
| Yes | 4,091 (3.3) | 1,243 (7.0) | 2,848 (2.7) | |
| No | 119,670 (96.7) | 16,558 (93.0) | 103,112 (97.3) | |
| Pre-admission insulin used | .30 | |||
| Yes | 44,382 (35.9) | 6,531 (36.7) | 37,851 (35.7) | |
| No | 79,379 (64.1) | 11,270 (63.3) | 68,109 (64.3) | |
| Pre-admission glucocorticoid use | .0034 | |||
| Yes | 13,472 (10.9) | 1,679 (9.4) | 11,793 (11.1) | |
| No | 110,289 (89.1) | 16,122 (90.6) | 94,167 (88.9) | |
| Current or prior DKA or HHS | <.0001 | |||
| Yes | 5,478 (4.4) | 1,231 (6.9) | 4,247 (4.0) | |
| No | 118,283 (95.6) | 16,570 (93.1) | 101,713 (96.0) | |
| Microvascular complicationsa | .19 | |||
| 0 | 86,979 (70.3) | 12,366 (69.5) | 74,613 (70.4) | |
| 1 | 21,853 (17.7) | 3,354 (18.8) | 18,499 (17.5) | |
| 2 | 9,329 (7.5) | 1,377 (7.7) | 7,952 (7.5) | |
| 3 | 5,600 (4.5) | 704 (4.0) | 4,896 (4.6) | |
| Macrovascular complicationsb,d | <.0001 | |||
| 0 | 44,973 (36.3) | 7,740 (43.5) | 37,233 (35.1) | |
| 1 | 36,540 (29.5) | 5,228 (29.4) | 31,312 (29.6) | |
| 2 | 29,242 (23.6) | 3,559 (20.0) | 25,683 (24.2) | |
| 3 | 10,337 (8.4) | 1,052 (5.9) | 9,285 (8.8) | |
| 4 | 2,669 (2.2) | 222 (1.3) | 2,447 (2.3) | |
| Pre-admission BP meds | <.0001 | |||
| None | 50,789 (41.0) | 4,949 (27.8) | 45,840 (43.3) | |
| ACE-i or ARB | 46,966 (38.0) | 8,595 (48.3) | 38,371 (36.2) | |
| Non-ACE or ARB | 26,006 (21.0) | 4,257 (23.9) | 21,749 (20.5) | |
| Pre-admission statin use | <.0001 | |||
| Yes | 53,754 (43.4) | 8,571 (48.2) | 45,183 (42.6) | |
| No | 70,007 (56.6) | 9,230 (51.9) | 60,777 (57.4) | |
| White blood cell count | <.0001 | |||
| Low <4 K/μL | 4,934 (4.0) | 793 (4.5) | 4,141 (3.9) | |
| Normal 4–11 K/μL | 81,937 (66.2) | 13,700 (77.0) | 68,237 (64.4) | |
| High >11 K/μL | 36,890 (29.8) | 3,308 (18.6) | 33,582 (31.7) | |
| Hematocritd, %, mean (SD) | 35.2 (5.63) | 33.7 (5.34) | 35.5 (5.63) | <.0001 |
| Serum sodiumd | <.0001 | |||
| Low <135 mmol/L | 29,061 (23.5) | 2,013 (11.3) | 27,048 (25.5) | |
| Normal 135–145 mmol/L | 93,298 (75.4) | 15,595 (87.6) | 77,703 (73.3) | |
| High >145 mmol/L | 1,402 (1.1) | 193 (1.1) | 1,209 (1.1) | |
| Serum potassium | .0003 | |||
| Low <3.1 mmol/L | 2,104 (1.7) | 238 (1.3) | 1,866 (1.8) | |
| Normal 3.1–5.3 mmol/L | 112,376 (90.8) | 16,302 (91.6) | 96,074 (90.7) | |
| High >5.3 mmol/L | 9,281 (7.5) | 1,261 (7.1) | 8,020 (7.6) | |
| Creatinined, mg/dL, median (IQR) | 1.1 (0.9–1.7) | 1.0 (0.7–1.4) | 1.2 (0.9–1.7) | .027 |
| Discharged 90 days prior to index admissiond | .12 | |||
| Yes | 38,112 (30.8) | 5,661 (31.8) | 32,451 (30.6) | |
| No | 85,649 (69.2) | 12,140 (68.2) | 73,509 (69.4) | |
| Length-of-stay, days, median (IQR) | 5.0 (3.0–8.0) | 3.7 (2.1–6.2) | 5.0 (3.0–8.0) | <.0001 |
| Discharge status of index admission | <.0001 | |||
| Home | 31,796 (25.7) | 10,372 (58.3) | 21,424 (20.2) | |
| Home with nursing care | 42,237 (34.1) | 3,448 (19.4) | 38,789 (36.6) | |
| Subacute facility | 25,307 (20.5) | 3,454 (19.4) | 21,853 (20.6) | |
| Against medical advice | 1,195 (1.0) | 392 (2.2) | 803 (0.8) | |
| Other | 1,352 (1.1) | 133 (0.8) | 1,219 (1.2) | |
| No status recorded | 21,874 (17.7) | 2 (0.01) | 21,872 (20.6) | |
| Discharge 1 year prior to index admissiond | <.0001 | |||
| Home | 17,198 (13.9) | 6,419 (36.1) | 10,779 (10.2) | |
| Home with nursing care | 20,781 (16.8) | 2,362 (13.3) | 18,419 (17.4) | |
| Sub-acute facility | 12,098 (9.8) | 2,082 (11.7) | 10,016 (9.5) | |
| Against medical advice | 723 (0.6) | 282 (1.6) | 441 (0.4) | |
| No discharge recorded | 72,961 (59.0) | 6,656 (37.4) | 66,305 (62.6) | |
| Body mass index | <.0001 | |||
| <18.5 kg/m2 | 2,017 (1.6) | 422 (2.4) | 1,595 (1.5) | |
| 18.5–24.9 kg/m2 | 20,147 (16.3) | 3,007 (16.9) | 17,140 (16.2) | |
| 25.0–29.9 kg/m2 | 37,644 (30.4) | 4,925 (27.7) | 32,719 (30.9) | |
| ≥30.0 kg/m2 | 63,953 (51.7) | 9,447 (53.1) | 54,506 (51.4) | |
| Depression or psychosis ever | <.0001 | |||
| Yes | 27,748 (22.4) | 5,242 (29.5) | 22,506 (21.2) | |
| No | 96,013 (77.6) | 12,559 (70.6) | 83,454 (78.8) | |
| Gastroparesis ever | .0042 | |||
| Yes | 4,319 (3.5) | 904 (5.1) | 3,415 (3.2) | |
| No | 119,442 (96.5) | 16,897 (94.9) | 102,545 (96.8) | |
| Pancreatitis ever | ||||
| Yes | 5,456 (4.4) | 974 (5.5) | 4,482 (4.2) | .021 |
| No | 118,305 (95.6) | 16,827 (94.5) | 101,478 (95.8) | |
| Hypertension ever | <.0001 | |||
| Yes | 87,421 (70.6) | 13,242 (74.4) | 74,179 (70.0) | |
| No | 36,340 (29.4) | 4,559 (25.6) | 31,781 (30.0) | |
| COPDc or asthma ever | <.0001 | |||
| Yes | 20,393 (16.5) | 4,068 (22.9) | 16,325 (15.4) | |
| No | 103,368 (83.5) | 13,733 (77.2) | 89,635 (84.6) | |
| Cardiac dysrhythmias ever | <.0001 | |||
| Yes | 39,828 (32.2) | 4,164 (23.4) | 35,664 (33.7) | |
| No | 83,933 (67.8) | 13,637 (76.6) | 70,296 (66.3) | |
| Malignant neoplasm ever | <.0001 | |||
| Yes | 20,459 (16.5) | 1,718 (9.7) | 18,741 (17.7) | |
| No | 103,302 (83.5) | 16,083 (90.4) | 87,219 (82.3) | |
| Anemia everd | .062 | |||
| Yes | 49,216 (39.8) | 7,348 (41.3) | 41,868 (39.5) | |
| No | 74,545 (60.2) | 10,453 (58.7) | 64,092 (60.5) | |
Abbreviations: ACE = angiotensin-converting enzyme; ACE-i = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker; BP = blood pressure; COPD = chronic obstructive pulmonary disease; DKA = diabetic ketoacidosis; HHS = hyperglycemic hyperosmolar syndrome; IQR = interquartile range.
Data are n, (%) unless otherwise noted.
Retinopathy, neuropathy, nephropathy.
Coronary artery disease, heart failure, stroke, peripheral vascular disease.
COPD, chronic obstructive pulmonary disease; Ever=current or prior.
Included in the Diabetes Early Re-admission Risk Indicator.
DISCUSSION
In this retrospective study of 105,960 discharges of patients with diabetes, we examined the external validity of the DERRI™, a previously developed and internally validated tool comprised of 10 parameters that predicts the 30-day re-admission risk of individual patients. In this sample, the DERRI™ had modest predictive performance based on a C-statistic of 0.634. Additionally, total cholesterol, HDL-C, LDL-C, triglycerides, and A1c levels were evaluated for association with re-admission. Although A1c and total cholesterol levels were independently associated with re-admission risk, inclusion of these variables with the DERRI™ predictors did not yield a model with significantly better predictive performance.
Discharges of patients with an Alc level <6.5% (48 mmol/mol) were at higher odds of re-admission than those with an Alc level between 6.5% (48 mmol/mol) and 8% (64 mmol/mol), whereas higher Alc levels were not associated with re-admission risk. Given the risk of hypoglycemia associated with lower A1c levels (20), it may be speculated that hypoglycemia is underlying the associated risk of re-admission. Unfortunately, data are not available in this retrospective cohort to explore this hypothesis. These findings add to the conflicting literature on the association of A1c with re-admission risk. One study reported higher re-admission risk associated with elevated Alc levels (16), while another study found that higher A1c levels were associated with lower risk of re-admission (17). Therefore, the association between Alc and re-admission risk remains quite unclear and requires additional study to clarify.
Similar to A1c, discharges of patients with total cholesterol levels <150 mg/dL were at higher odds of re-admission than those with levels of 150 to 200 mg/dL, and higher total cholesterol levels were not associated with re-admission risk. To our knowledge, there is no previously published literature that describes the association between re-admission risk and total cholesterol. The mechanism underlying this pattern of association is not immediately apparent. It may be speculated that the association of lower total cholesterol levels and re-admission risk is due to confounding by indication, where aggressive lipid lowering is achieved in patients at high risk for cardiovascular events and thus re-admission. An alternative hypothesis is that low total cholesterol may reflect malnutrition or poor fat absorption, which may be associated with comorbidities. Interestingly, total cholesterol was found to have the strongest association with re-admission among the lipid parameters and was selected for multivariable modeling. Of note, the association of low cholesterol with re-admission was not affected by adjustment for pre-admission statin use.
In the current study, the DERRI™ demonstrated less predictive accuracy than in the internal validation sample. This discrepancy may be accounted for by the substantial population differences between the internal validation and external validation samples. Because of these differences, there is likely to be variation in the relative importance of re-admission risk factors between the two samples. Despite the somewhat lower value, 0.634 is comparable to the C-statistics of other models predicting re-admission risk among diabetes patients, which range from 0.635 to 0.822 (6,8,17,21,22). A key difference, however, between these other models and the DERRI™ is that only the DERRI™ can be used for a patient before hospital discharge. The other models include variables obtained after discharge, such as hospital length-of-stay, discharge disposition, and outpatient follow-up. In addition, most of them contain the number of recent prior emergency department visits or hospitalizations, which is not easily obtainable if patients have had acute encounters at multiple hospitals. Furthermore, two of them include a comorbidity index that is scored according to all of a patient’s comorbidities (17,21). Such models are less practical for use at the point of care. Lastly, none of these other models were tested in an external validation sample, which tends to yield worse performance metrics than internal validation (15). Although performance of the DERRI™ is modest, evidence suggests that even moderately performing models tend to outperform clinical judgment (23,24).
Some limitations of our study should be acknowledged. Both the internal and external validation samples were drawn from urban academic medical centers in the Northeastern US; therefore, these findings may not be generalizable to hospitals with different characteristics. Despite these similarities between the academic medical centers, the external and internal validation samples were different for most variables, most notably age and race/ethnicity. It is unknown whether or not the DERRI™ would perform better in another population that is more similar to the internal validation population. Data on other potential predictors of 30-day re-admission, including diabetes type and duration, could not be obtained in this retrospective study. In addition, the analyses of A1c and cholesterol are limited by the substantial proportion of records missing these data. However, it is re-assuring that the sensitivity analysis restricted to discharges that had complete A1c and cholesterol data yielded similar results. Finally, we were unable to capture 30-day re-admissions that may have occurred at hospitals outside of the Partners HealthCare system. However, when compared to rates reported in the literature for patients with diabetes, the 30-day re-admission rate in our study is on the higher end of the range of 10.0 to 20.4% (5–10); therefore, it seems unlikely that a significant number of patients were re-admitted elsewhere.
These study limitations are balanced by a number of strengths. The subject cohort was comprised of a relatively large sample size drawn from patients hospitalized at two academic medical centers. Re-admissions were captured at all of the Partners HealthCare hospitals in the region during the study period, including three community hospitals. A total of 15 sociodemographic and clinical characteristics were examined as potential predictors of 30-day re-admission, expanding the existing body of literature (5,6,8,9,21,25,26). To our knowledge, the association between lipid parameters and 30-day re-admission risk has not been previously reported. Lastly, this is the first external validation study of a re-admission risk prediction model in diabetes patients.
Future research could explore ways to improve the prediction of re-admission risk for patients with diabetes. Larger studies drawn from diverse populations and settings would better address issues of generalizability. We are currently conducting a prospective study to gather data on previously untested potential re-admission predictors. In addition, we are conducting a pilot randomized controlled trial that uses the DERRI™ to identify patients at high risk of re-admission and explores the feasibility and efficacy of a re-admission risk-reduction intervention, the Diabetes Transition of Hospital Care (DiaTOHC) Program (ClinicalTrials.gov Identifier: NCT03243383).
CONCLUSION
In summary, performance of the DERRI™ in this external cohort to predict early re-admission risk of patients with diabetes was modest. Although lower A1c and total cholesterol levels were found to be associated with higher re-admission risk, these parameters do not add significant predictive power to the DERRI™. Additional research is needed to identify better predictors of re-admission among patients with diabetes.
ACKNOWLEDGMENT
We thank Neil Kondamuri for administrative support preparing the manuscript.D.R. was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K23DK102963. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the study design, data, writing the report, or submission for publication.
An abstract of this study was presented at the 77th Scientific Sessions of the American Diabetes Association in June, 2017, San Diego, California. The Partners HealthCare and Temple University Institutional Review Boards approved the protocol. A waiver of informed consent was obtained for this large retrospective study.
Abbreviations:
- A1c
hemoglobin A1c
- CI
confidence interval
- DERRI™
Diabetes Early Readmission Risk Indicator
- GEE
generalized estimating equation
- HDL-C
high-density-lipoprotein cholesterol
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- LDL-C
low-density-lipoprotein cholesterol
Footnotes
DISCLOSURE
The authors have no multiplicity of interest to disclose.
REFERENCES
- 1.Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305:504–505. [DOI] [PubMed] [Google Scholar]
- 2.Stone J, Hoffman G Medicare Hospital Readmissions: Issues, Policy Options and PPACA. Congressional Research Service; Penny Hill Press; 2010. [Google Scholar]
- 3.Epstein AM. Revisiting readmissions--changing the incentives for shared accountability. N Engl J Med. 2009;360:1457–1459. [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robbins JM, Webb DA. Diagnosing diabetes and preventing rehospitalizations: the urban diabetes study. Med Care. 2006;44:292–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennett KJ, Probst JC, Vyavaharkar M, Glover SH. Lower rehospitalization rates among rural Medicare beneficiaries with diabetes. J Rural Health. 2012;28:227–234. [DOI] [PubMed] [Google Scholar]
- 7.Chen JY, Ma Q, Chen H, Yermilov I. New bundled world: quality of care and readmission in diabetes patients. J Diabetes Sci Technol. 2012;6:563–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eby E, Hardwick C, Yu M, et al. Predictors of 30 day hospital readmission in patients with type 2 diabetes: a retrospective, case–control, database study. Curr Med Res Opin. 2015;31:107–114. [DOI] [PubMed] [Google Scholar]
- 9.Healy SJ, Black D, Harris C, Lorenz A, Dungan KM. Inpatient diabetes education is associated with less frequent hospital readmission among patients with poor glycemic control. Diabetes Care. 2013;36:2960–2967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rubin DJ, Handorf EA, Golden SH, Nelson DB, McDonnell ME, Zhao H. Development and validation of a novel tool to predict hospital readmission risk among patients with diabetes. Endocr Pract. 2016;22:1204–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.HCUP Nationwide Inpatient Sample (NIS) 2014. Agency for Healthcare Research and Quality (AHRQ) 2018. Available at: https://hcupnet.ahrq.gov/#setup. Accessed April 11, 2018. [Google Scholar]
- 12.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528. [DOI] [PubMed] [Google Scholar]
- 13.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334:1441–1447. [DOI] [PubMed] [Google Scholar]
- 14.Draznin B, Gilden J, Golden SH, et al. Pathways to quality inpatient management of hyperglycemia and diabetes: a call to action. Diabetes Care. 2013;36:1807–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altman DG, Vergouwe Y, Royston P, Moons KGM. Prognosis and prognostic research: validating a prognostic model. BMJ. 2009;338:1432–1435. [DOI] [PubMed] [Google Scholar]
- 16.Engoren M, Schwann TA, Habib RH. Elevated hemoglobin A1c is associated with readmission but not complications. Asian Cardiovasc Thorac Ann. 2014;22:800–806. [DOI] [PubMed] [Google Scholar]
- 17.Wei NJ, Wexler DJ, Nathan DM, Grant RW. Intensification of diabetes medication and risk for 30-day readmission. Diabet Med. 2013;30:e56–e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–375. [DOI] [PubMed] [Google Scholar]
- 19.Royston P, Moons KGM, Altman DG, Vergouwe Y. Prognosis and prognostic research: Developing a prognostic model. BMJ. 2009;338:b604. [DOI] [PubMed] [Google Scholar]
- 20.Cryer PE. Glycemic goals in diabetes: trade-off between glycemic control and iatrogenic hypoglycemia. Diabetes. 2014;63:2188–2195. [DOI] [PubMed] [Google Scholar]
- 21.Rico F, Liu Y, Martinez DA, Huang S, Zayas-Castro JL, Fabri PJ. Preventable readmission risk factors for patients with chronic conditions. J Healthc Qual. 2016;38:127–142. [DOI] [PubMed] [Google Scholar]
- 22.Collins J, Abbass IM, Harvey R, et al. Predictors of all-cause-30-day-readmission among Medicare patients with type 2 diabetes. Curr Med Res Opin. 2017;33:1517–1523. [DOI] [PubMed] [Google Scholar]
- 23.Ivanov J, Borger MA, David TE, Cohen G, Walton N, Naylor CD. Predictive accuracy study: comparing a statistical model to clinicians’ estimates of outcomes after coronary bypass surgery. Ann Thorac Surg. 2000;70:162–168. [DOI] [PubMed] [Google Scholar]
- 24.Loeb M, Walter SD, McGeer A, Simor AE, McArthur MA, Norman G. A comparison of model-building strategies for lower respiratory tract infection in long-term care. J Clin Epidemiol. 1999;52:1239–1248. [DOI] [PubMed] [Google Scholar]
- 25.Albrecht JS, Hirshon JM, Goldberg R, et al. Serious mental illness and acute hospital readmission in diabetic patients. Am J Med Qual. 2012;27:503–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ostling S, Wyckoff J, Ciarkowski SL, et al. The relationship between diabetes mellitus and 30-day readmission rates. Clin Diabetes Endocrinol. 2017;3:3. [DOI] [PMC free article] [PubMed] [Google Scholar]