Abstract
The authors conducted a household survey and observation to assess carbon monoxide (CO) knowledge and risks as well as prevalence of CO alarms in an urban community prior to the enactment of a mandatory ordinance requiring CO alarms in one U.S. city. From July to December 2009, household surveys and observations were completed in 603 residences. Participants were mostly African-American (61%), women (70%), 25–54 years in age (66%), and with a high school education or less (51%). Most homes visited contained CO-producing appliances, including gas stoves (86%), gas furnaces (82%), and gas water heaters (79%). Participants’ overall mean percentage correct knowledge score was 57%. CO alarms were reported by 33% of participants and observed among 28% of households. Low rates of CO knowledge and CO alarm ownership, combined with high rates of CO-producing sources in homes, suggests the need for widespread campaigns to promote CO alarms. Recommendations are also made to integrate the lessons learned from the public health community’s experience promoting smoke alarms.
Introduction
Carbon monoxide (CO) poisoning is a significant yet preventable public health problem that is only recently gaining the necessary attention of public health and safety officials and policy makers. CO is a colorless, odorless gas that is produced through the incomplete combustion of hydrocarbons (Kao & Nanagas, 2005). CO sources are ubiquitous in homes, especially in heating equipment such as gas furnaces, gas and propane heaters, clothes dryers, stoves, woodstoves, and fireplaces. Other sources of CO include motor vehicle exhaust and tobacco smoke.
CO exposure is a leading cause of poisoning death in the U.S., killing approximately 450 people annually (Centers for Disease Control and Prevention [CDC], 2011). Technically, CO is identified as a toxicant, a poison that is made by humans or introduced into the environment as a function of human activity (Graber, Macdonald, Kass, Smith, & Anderson, 2007). The effects of CO exposure are often difficult to recognize because of their nonspecific nature. Early symptoms of CO exposure include headache, dizziness, weakness, nausea, confusion, and vision problems; disorientation, unconsciousness, and death may result at higher levels of CO exposure (Raub et al., 2000).
The Centers for Disease Control and Prevention (CDC) estimated that during the years 2004–2006, 20,636 nonfatal, unintentional, non-fire-related CO exposures were seen in emergency departments each year (CDC, 2008). Compared to older children, those four years of age and younger had the highest estimated rate of CO-related emergency departments visits (11.6/100,000). For adults, the rate of CO exposure was highest (10.4/100,000) among those aged 25–34 and lowest (3.6/100,000) among those 65 years and older (CDC, 2008). According to CDC, 73% of the estimated annual CO events seen in emergency departments occur in the home (CDC, 2008).
CO alarms are one of the most important protective devices for preventing CO exposure and poisoning in homes. Given the indiscernible nature of CO itself and the nonspecific nature of symptoms from exposure to it, CO alarms serve as a warning tool to prevent prolonged exposure to high levels of CO. These devices, which retail for $20 to $60, emit an audible alarm when CO is detected at either or both an amount present or a length of exposure that would produce morbidity or mortality. The Consumer Product Safety Commission and other groups have long recommended CO alarms as a defense against CO poisoning (Consumer Product Safety Commission, 2012). Yoon and co-authors (1998) estimated that CO alarms could prevent at least half of nonfire unintentional CO poisoning.
As of this writing, statutes from 27 states address issues of CO alarms in certain types of residential dwellings. Many of the statutes limit CO alarms by the type of residence (e.g., rental property), when it was built (e.g., new construction only) or upon a change of ownership. Only Illinois and Massachusetts statutes mandate alarms in “every dwelling” (National Conference of State Legislatures, 2012). In Maryland, where our study was undertaken, a law was enacted in 2009 requiring CO alarms for new residential construction.
Estimates of CO alarm use in the literature are sparse and equivocal. Runyan and coauthors (2005) conducted a random-digit-dial survey among a nationally representative sample that revealed that 29% of homes reported a CO alarm. More recently, Hampson and Weaver (2011) completed a computer-based survey of two sets of medical center employees in Washington and Utah and found CO alarm use reported in 51% of homes. Unfortunately both studies rely on self-reported information, which is a documented limitation (Chen, Gielen, & McDonald, 2003).
The Johns Hopkins Home Safety Project sought to describe among an urban population the knowledge and behaviors relevant to preventing carbon monoxide poisoning as well as household risks. Specifically, our article aims to describe the prevalence of observed CO alarms prior to the enactment of a city ordinance requiring CO alarms in all city residences. We also aim to identify correlates of CO alarm use.
Methods
Study Design and Sampling
A baseline survey of East Baltimore households was conducted between July and December 2009 as part of a community intervention trial, assessing the impact of an enhanced Baltimore City Fire Department (BCFD) home visit program through which smoke alarms are installed.
Neighborhood Selection and Address Randomization
In preparation for a community intervention trial that would be evaluated using a two-group, quasi-experimental design, we created a sampling frame that would be comparable across important confounders of key outcomes, such as prevalence of smoke alarms and the prior success of BCFD personnel in gaining access to the premises through their program. Based on a desired final sample size of 350–400 completed baseline surveys in each community, we determined that we would need a total of 12 census tracts. We formed a sample of 10,000 paired combinations (which we called “blends”) of six randomly chosen census tracts out of the 49 census tracts in East Baltimore. We then computed a summary statistic for each blend composed as the blend’s unweighted average of 1) vacancy rate; 2) number of previous BCFD home visits attempted; 3) percentage of BCFD home visits that were successful (i.e., BCFD gained entry); 4) residential fire rate; 5) percentage of dwellings built after 1984; and 6) percentage of owner-occupied properties.
The quality of matching in each pair of blends was assessed as the difference between the two blends of the raw sum of the above six indicators. The 10,000 matched scores were sorted and the study team selected candidate matches out of the top one percentile of match scores for further consideration. Members of the team, which included community representatives, drove through several of the top candidate matches to observe the neighborhoods to ensure that they had residential properties as expected and would be suitable for the intervention trial (e.g., neighborhoods had been gentrified for a large development project or new industry had come in since the time of the census).
The final selection of 12 census tracks (six paired tracts in each community) included a total of 10,333 residences. Residences that were not eligible for the BCFD installation program (i.e., public housing and city managed apartment complexes, n = 375) were excluded. From the remaining 9,958 eligible addresses, three separate samples of 1,200 addresses were randomly selected. A new random selection was done when all previously selected addresses had been resolved (i.e., enrolled, refused, deemed ineligible, or did not respond after five attempts to contact).
Data Collection
All selected addresses received a project letter detailing the survey and contact information in case a resident wished to schedule an appointment or opt out of the survey. Data collectors, in teams of two, knocked on the doors of selected addresses, leaving a copy of the project letter at any door where there was no answer. Each house was visited on five nonconsecutive days or until an eligible resident completed the survey, refused at the door or via telephone, or was deemed ineligible by the data collectors. If unsuccessful after five attempts, the address was coded as “no answer” and not visited again unless the resident called the project office to make an appointment to complete the survey.
Eligibility criteria included both housing structure and resident characteristics. Premises deemed unsafe, vacant, or nonexistent by data collectors were coded as ineligible residences. To be eligible, respondents had to be English speaking and at least 18 years old. After determining eligibility and obtaining written informed consent, data collectors, with permission, conducted the survey inside the participant’s home. Surveys were conducted on small netbook computers and lasted about 30–45 minutes. Data collectors read questions aloud and recorded the respondent’s answers.
Measures
Sociodemographic Characteristics
Sociodemographic measures as part of the survey included self-reported race and ethnicity, education, household role, gender, age of respondent and all household members, and homeowner status. Household income was determined in two parts. First, the respondent viewed a card listing seven income ranges and selected the one that contained their household income. Per capita income was then calculated by dividing the midpoint of that income range by the total number of residents.
CO Knowledge
Eleven questions examined participant’s knowledge about CO sources and poisoning risks, CO signs and symptoms, CO alarm functionality and recommendations, legal requirements for alarms, and proper evacuation steps in response to an activated CO alarm. All items were created for the purpose of our study and pretesting used cognitive interviewing to improve wording and comprehension. Percentage correct scores were calculated for knowledge items.
CO Sources in Home
Participants were asked whether they had common household gas appliances (e.g., furnace, water heater, stove, clothes dryer). The total number of CO-producing appliances found in the home was tallied for each household.
CO Alarm Status
After completing the survey, which included a self-report question on whether there was a CO alarm in the home, data collectors asked all respondents to show them any CO alarms in their home. Data collectors confirmed its existence, tested whether it was working by pressing the “test” button, and recorded the result.
Data Analysis
In addition to providing frequency distributions for the variables under study, we used Chi-square tests to examine bivariate relationships between having a working CO alarm and sociodemographic factors and CO knowledge. Inverse probability weights were used to examine the potential biases due to the study area having a higher frequency of African-American and low-income respondents than all of Baltimore. Weights were calculated based on race and income distributions obtained from the 2000 census data.
Weighted and unweighted multiple logistic regression models were then constructed to examine the relationships between the outcome, having a working CO alarm, and sociodemographic factors and CO knowledge and their results compared. Results of the unweighted versus weighted models varied by no more than 10%; therefore, results for the unweighted models are presented. The analysis was conducted using Intercooled STATA 9.2.
Results
Recruitment
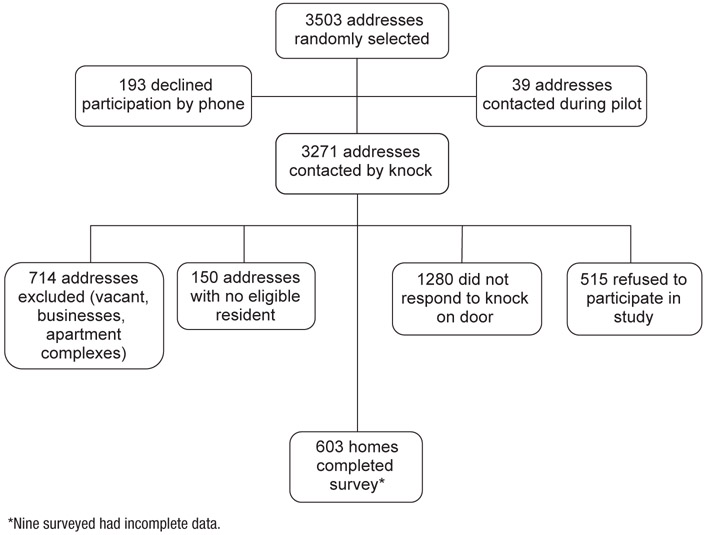
From a total of 3,503 eligible addresses, we excluded 193 who refused via telephone in response to the project letter and another 39 who participated in a pilot test of the computer survey application. Data collectors attempted to visit the remaining 3,271 addresses in person and excluded another 2,659 addresses for various reasons (Figure 1). Household surveys were conducted with 612 participants, but nine had incomplete data and were removed, resulting in a final sample size of 603 completed surveys.
FIGURE 1.
Study Design
Demographic Characteristics
A majority of respondents were African-American (61%), female (70%), between the ages of 25 and 54 (66%), and had a high school education or less (51%). Most self-identified as the “head of the household” (81%) (Table 1). Almost three-quarters of the respondents (74%) reported a per capita income of $25,000 or less and a little more than half (52%) rented their home. Forty percent of respondents lived with children under the age of 18.
TABLE 1.
Sample Sociodemographic Characteristics, Carbon Monoxide (CO)-Producing Appliances, and CO Alarm Ownership
| Characteristics | Pearson χ2 (p-Value) | Observed CO Alarm | Total Sample N = 603 (%) | ||
|---|---|---|---|---|---|
| Yes n = 166 (28%) |
No n = 437 (72%) |
||||
| Gender | Male | 0.10 (76) | 48 (29) | 132 (30) | 180 (30) |
| Female | 118 (71) | 305 (70) | 423 (70) | ||
| Age | 18 to 24 | 2.35 (.80) | 26 (16) | 63 (14) | 89 (15) |
| 25 to 34 | 44 (27) | 123 (28) | 167 (28) | ||
| 35 to 44 | 32 (19) | 86 (20) | 118 (20) | ||
| 45 to 54 | 26 (16) | 82 (19) | 108 (18) | ||
| 55 to 64 | 25 (15) | 49 (11) | 74 (12) | ||
| 65 and above | 13 (8) | 34 (8) | 47 (8) | ||
| Household role | Head of household | 0.23 (.63) | 132 (80) | 355 (81) | 487 (81) |
| Other | 34 (21) | 82 (19) | 116 (19) | ||
| Education | Less than high school diploma/GED | 5.01 (.17) | 21 (13) | 58 (13) | 79 (13) |
| High school diploma/GED | 57 (34) | 173 (40) | 230 (38) | ||
| Some college | 40 (24) | 71 (16) | 111 (19) | ||
| Completed college | 48 (29) | 133 (31) | 181 (30) | ||
| Per capita income | $5000 or less | 4.40 (.22) | 29 (21) | 100 (29) | 129 (27) |
| $5001 to $10000 | 31 (22) | 72 (21) | 103 (21) | ||
| $10001 to $25000 | 42 (30) | 82 (24) | 124 (26) | ||
| $25000 or more | 39 (28) | 86 (25) | 125 (26) | ||
| Race | Black or African-American | 0.92 (.34) | 96 (58) | 263 (63) | 359 (61) |
| Other | 69 (42) | 158 (38) | 227 (39) | ||
| Homeowner status | Rent | 15.95 (.00) | 59 (38) | 238 (57) | 297 (52) |
| Own or pay mortgage | 97 (62) | 183 (44) | 280 (49) | ||
| Children (<18) in home | Yes | 0.04 (.84) | 65 (39) | 175 (40) | 240 (40) |
| No | 101 (61) | 262 (60) | 363 (60) | ||
| CO sources in home | Gas furnace | 0.73 (.39) | 120 (85) | 286 (81) | 406 (82) |
| No gas furnace | 22 (16) | 66 (19) | 88 (18) | ||
| Gas water heater | 2.28 (.13) | 118 (84) | 281 (78) | 399 (79) | |
| No gas water heater | 23 (16) | 81 (22) | 104 (21) | ||
| Gas stove | 0.16 (.69) | 144 (87) | 375 (86) | 519 (86) | |
| No gas stove | 21 (13) | 61 (14) | 82 (14) | ||
| Gas clothes dryer | 0.26 (.61) | 52 (33) | 124 (30) | 176 (31) | |
| No gas clothes dryer | 108 (68) | 285 (70) | 393 (69) | ||
| Total number of CO sources in home | No CO equipment | 2.27 (.69) | 15 (9) | 53 (12) | 68 (11) |
| 1 CO equipment | 19 (11) | 60 (14) | 79 (13) | ||
| 2 CO equipment | 31 (19) | 84 (19) | 115 (19) | ||
| 3 CO equipment | 67 (40) | 159 (36) | 226 (38) | ||
| 4 CO equipment | 34 (21) | 81 (19) | 115 (19) | ||
CO Sources in the Home
As shown in Table 1, most homes visited contained CO-producing appliances. In fact, 76% of the sample reported two or more items that produce CO (data not shown). The most commonly reported items were gas stoves (86%), gas furnaces (82%), and gas water heaters (79%). Less than 1% reported the use of a kerosene heater (data not shown).
CO Alarm Status
A majority of respondents (54%) reported not having a working CO alarm; another 13% were unsure. One-third (33%) of respondents reporting having a CO alarm (data not shown). We were able to confirm through observation that 166 (28%) participants had at least one working CO alarm. The only sociodemographic characteristic related to having a working CO alarm was homeowner status (Table 1). Compared to those who rented, those who owned their home or paid a mortgage were statistically significantly more likely to have a working CO alarm (62% vs. 44%, p = .00). We found no relationship between having a working CO alarm and either the presence or total number of COproducing appliances in the home (Table 1).
CO Knowledge
As shown in Table 2, CO knowledge varied across different topics. Most respondents knew that children and teens are not the only ones at risk of CO poisoning (92%); and that CO is a gas that cannot be seen (84%). Conversely, few respondents were able to correctly identify symptoms of CO poisoning (17%) and the proper location for a CO alarm (18%). More than one-third (38%) of city residents knew that (at the time of the survey) CO alarms were not required by law. The overall mean percentage correct knowledge score was 57%.
TABLE 2.
Carbon Monoxide (CO) Knowledge and CO Alarm Ownership
| Knowledge ItemsL: True/False or Multiple Choice Options. Correct Answer Indicated in Italics. |
Pearson χ2 (p-Value) |
Observed CO Alarm | Total Sample N = 603 # (%) Correct |
|
|---|---|---|---|---|
| Yes n = 166 #(%) Correct |
No n = 437 #(%) Correct |
|||
| CO is a gas that cannot be seen. | 3.19 (.074) | 146 (88) | 358 (82) | 504 (84) |
| You can smell CO, false. | 14.77 (.00) | 135 (81) | 285 (65) | 420 (70) |
| Electric heaters do not cause CO poisoning. | 1.24 (.27) | 74 (45) | 173 (40) | 247 (41) |
| Only children and teens are at risk for CO poisoning, false. | 1.58 (.21) | 157 (95) | 400 (92) | 557 (92) |
| Symptoms of CO poisoning are similar to the flu. | 4.71 (.03) | 37 (22) | 65 (15) | 102 (17) |
| Near all sleeping areas is the best place to install a CO alarm in the home. | 1.40 (.24) | 35 (21) | 74 (17) | 109 (18) |
| The first thing to do if your CO alarm goes off is to get everyone out of the house and call 911. | 7.15 (.01) | 143 (86) | 333 (76) | 476 (79) |
| How often should you change the battery in your CO alarm, every six months. | 0.19 (.66) | 78 (47) | 214 (49) | 292 (48) |
| Using a gas oven to heat your home could cause CO poisoning, true. | 2.49 (.11) | 134 (81) | 326 (75) | 460 (76) |
| Your smoke alarm will alert you when CO levels are too high, false. | 2.46 (.12) | 107 (65) | 251 (57) | 358 (59) |
| In Baltimore city, all homes are required by law to have a CO alarm, false. | 5.34 (.02) | 51 (31) | 179 (41) | 230 (38) |
| Overall mean percentage correct knowledge score | t = 3.16 (.002) | 60% | 55% | 57% |
We found a significant relationship between having a CO alarm and overall mean percentage correct knowledge score (Table 2); respondents with higher mean percentage correct knowledge scores were more likely to have an observed CO alarm in their home compared to those with a lower knowledge score (60% vs. 55%, t = 3.16, p = .002). Individual knowledge items varied with CO alarm ownership. For instance, knowing that one cannot smell CO was significantly associated with having a CO alarm (81% vs. 65%, χ2 = 14.8, p = .00) as was knowledge of CO poisoning symptoms (22% vs. 15%, χ2 = 4.71, p = .03). CO alarm owners, however, were less likely than those without alarms to correctly answer the question about legal requirements for CO alarms in Baltimore city (31% vs. 41%, χ2 = 5.34, p = .02).
Predictors of CO Alarm Ownership
Results from the multiple logistic regression analysis, including odds ratio (ORs) and corresponding confidence intervals (CIs) are summarized in Table 3. The results indicate that having at least one working CO alarm is associated with owning a home or paying a mortgage (OR = 3.43; 95% CI: 1.69, 6.98; p = .0007). Two knowledge items were associated with observed CO alarms, knowing that CO cannot be smelled (OR = 2.90; 95% CI: 1.45, 5.98; p = .039) and knowing what to do when an alarm activates (OR = 2.20; 95% CI: 1.00, 4.82; p = .0495). Mistakenly thinking that CO alarms are legally required was associated with CO alarm ownership (OR = 0.25; 95% CI: 0.14, 0.45; p = .0001).
TABLE 3.
Logistic Regression Model of Sociodemographic Characteristics and Carbon Monoxide (CO) Knowledge Correlates of CO Alarm Ownership
| Sociodemographic Characteristics | Adjusted ORa | 95% CIa | |
|---|---|---|---|
| Gender | Male | 1 | |
| Female | 1.41 | 0.71, 2.59 | |
| Age | 18 to 24 | 1 | |
| 25 to 34 | 0.34 | 0.11, 1.08 | |
| 35 to 44 | 0.25 | 0.08, 0.84 | |
| 45 to 54 | 0.22 | 0.07, 0.71 | |
| 55 and above | 0.31 | 0.09, 1.05 | |
| Household role | Other | 1 | |
| Head of household | 1.41 | 0.60, 3.34 | |
| Education | High school/GED | 1 | |
| <High school/GED | 1.22 | 0.48, 3.09 | |
| Some college | 1.46 | 0.65, 3.27 | |
| Completed college | 0.91 | 0.40, 2.07 | |
| Per capita income | $5000 or less | 1 | |
| $5001 to $10000 | 1.40 | 0.60, 3.24 | |
| $10001 to $25000 | 1.24 | 0.47, 3.28 | |
| $25000 or more | 1.29 | 0.43, 3.89 | |
| Race/ethnicity | Other | 1 | |
| Black or African- American | 0.92 | 0.47, 1.77 | |
| Homeowner status | Rent | 1 | |
| Own or pay mortgage | 3.43 | 1.69, 6.98* | |
| Children (<18) in home | No | 1 | |
| Yes | 1.01 | 0.53, 1.94 | |
| Homes with CO-producing equipment | |||
| Gas furnace | No | 1 | |
| Yes | 1.22 | 0.53, 2.78 | |
| Gas water heater | No | 1 | |
| Yes | 1.42 | 0.63, 3.21 | |
| Gas stove | No | 1 | |
| Yes | 0.80 | 0.33, 1.94 | |
| Gas clothes dryer | No | 1 | |
| Yes | 0.71 | 0.41, 1.25 | |
| Knowledge question | |||
| CO is a gas that cannot be seen. | Incorrect | 1 | |
| Correct | 1.27 | 0.59, 2.70 | |
| You can smell CO, false. | Incorrect | 1 | |
| Correct | 2.90 | 1.41, 5.98** | |
| Electric heaters do not cause CO poisoning. | Incorrect | 1 | |
| Correct | 0.73 | 0.40, 1.33 | |
| Only children and teens are at risk for CO poisoning, false. | Incorrect | 1 | |
| Correct | 1.17 | 0.29, 4.73 | |
| Symptoms of CO poisoning are similar to the flu. | Incorrect | 1 | |
| Correct | 1.75 | 0.88, 3.46 | |
| Near all sleeping areas is the best place to install a CO alarm in the home. | Incorrect | 1 | |
| Correct | 1.75 | 0.90, 3.40 | |
| The first thing to do if your CO alarm goes off is to get everyone out of the house and call 911. | Incorrect | 1 | |
| Correct | 2.20 | 1.00, 4.82*** | |
| How often should you change the battery in your CO alarm, every six months. | Incorrect | 1 | |
| Correct | 0.94 | 0.54, 1.62 | |
| Using a gas oven to heat your home could cause CO poisoning, true. | Incorrect | 1 | |
| Correct | 0.89 | 0.44, 1.80 | |
| Your smoke alarm will alert you when CO levels are too high, false. | Incorrect | 1 | |
| Correct | 1.30 | 0.70, 2.40 | |
| In Baltimore city, all homes are required by law to have a CO alarm, false. | Incorrect | 1 | |
| Correct | 0.25 | 0.14, 0.45**** | |
0R = odds ratio; CI = confidence interval.
p = .0007;
p = .0039;
p = .0495;
P < .0001.
Discussion
Our results provide some of the first evidence on the extent to which residents in urban neighborhoods are aware of CO poisoning risk, are exposed to it, and are taking action to protect themselves. The findings suggest that considerable education is needed to better inform residents of the causes and symptoms of CO poisoning; the proper location, maintenance, and response to CO alarms; and the differences between smoke alarms and CO alarms. The overall mean percentage correct knowledge score was 57%, a failing grade by any test measure. The importance of these findings is underscored by the fact that almost 90% of homes had at least one source of CO and more than 50% had three or more sources. Thus, potential exposures to CO are a real threat in these urban neighborhoods and most residents are ill informed about CO.
We found shockingly low levels of self-reported CO alarm ownership, with just 33% self-reporting at least one working alarm in their home. This self-reported CO alarm possession prevalence is only slightly higher than that reported by Runyan and co-authors (2005). In their random-digit-dial telephone survey of 1,000 households designed to be representative of the entire U.S. population, 29% reported having a CO alarm. Our data differ significantly from Hampson and Weaver (2011); their computer-based survey of 1,351 individuals reported CO alarm use by 51% of their respondents.
An important strength of our study is the ability to confirm self-reported CO alarm ownership with observed data, a technique recognized to be the gold standard for reporting injury prevention behaviors. The observed prevalence of at least one working CO alarm in the home fell to 28% from 33% who self-reported alarm use. The differences between observed and reported rates in this case are not as high as those found for smoke alarm ownership by us (Chen, Gielen, & McDonald, 2003) and others (Douglas, Mallonee, & Istre, 1999). Nevertheless, the discrepancy between self-report and observed practices reminds us that we cannot rely on self-report alone to determine household safety behaviors.
The low rates of CO alarm ownership and knowledge, combined with the high rates of CO-producing sources in homes, also suggest the need for widespread campaigns to promote the use of CO alarms. Our data did not identify specific subgroups of the population least likely to have working CO alarms, which further supports the conclusion that campaigns should be targeted broadly, to homeowners, landlords, and tenants. Moreover, promotional campaigns should consider the needs of low-income communities to address the costs of and easy access to such safety devices.
Public health and safety officials should consider the lessons we have learned in our effort to promote and distribute smoke alarms and integrate these into CO alarm promotion and distribution programs. Criteria have been established to define gold standard smoke alarm campaigns including 1) working in local communities and recruiting community partners, 2) canvassing homes in high-risk areas, 3) using smoke alarms with special features (like long-lasting lithium batteries and a hush feature), and 4) conducting follow up activities to ensure alarm functionality (Ballesteros, Jackson, & Martin, 2005). CO promotion campaigns while in their nascent stages should be encouraged to incorporate these important lessons learned from the smoke alarm experience. Although not yet deemed a gold standard criterion, another potentially important finding from the smoke alarm experience is the concern about whether audible alarms awaken sleeping children and the call to consider voicerecording options (Smith, Splaingard, Hayes, & Xiang, 2006).
The results presented here should be interpreted in the context of several limitations. Our ability to generalize results is limited to other urban populations with similar demographic characteristics to the participants in this study. The majority of our sample was African-American adults living in a predominantly low-income, urban area, and we did not include Spanish-speaking residents. We were able to weight our sample to account for the higher frequencies of African-American and low-income residents in our study area compared to all of Baltimore and found only minor differences. Although our sampling methodology included random selection of households within census tracts specifically chosen to result in a representative sample of East Baltimore homes, our completed sample size was smaller than originally anticipated due to high rates of refusal and residents not being home. We do not have data to compare those who completed the survey to those who did not.
Conclusion
Our work recognizes and documents the need for enhanced education and promotion efforts targeted to CO poison prevention. As of March 2011 (after the completion of our data collection), all Baltimore city residences are required to have at least one working CO alarm. Legislation is a necessary but insufficient mechanism alone to ensure that all residents are safe in their homes. Implementation of the law needs to be supported with public health campaigns that address the knowledge gaps that we identified and to enhance access to and affordability of CO alarms for low-income and other special need communities.
Acknowledgements:
We are grateful to the residents of Baltimore who allowed us into their homes and who completed our survey and observation. We would also like to thank Dharssi Safiyya who assisted us with a review of the literature on carbon monoxide while she was pursuing a master of public health degree at the Johns Hopkins Bloomberg School of Public Health.
References
- Ballesteros MF, Jackson ML, & Martin MW (2005). Working toward the elimination of residential fire deaths: the Centers for Disease Control and Prevention’s Smoke Alarm Installation and Fire Safety Education (SAIFE) program. Journal of Burn Care Rehabilitation, 26(5), 434–439. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2008). Nonfatal, unintentional, non-fire-related carbon monoxide exposures—United States, 2004–2006. Morbidity and Mortality Weekly Reports, 57(33), 896–899. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2011). Carbon monoxide poisoning prevention clinical education webcast. Retrieved from http://www.cdc.gov/co/
- Chen LH, Gielen AC, & McDonald EM (2003). Validity of self reported home safety practices. Injury Prevention, 9(1), 73–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consumer Product Safety Commission. (2008). Carbon monoxide (CO) questions and answers. Retrieved from http://www.cpsc.gov/cpscpub/pubs/466.html
- Douglas MR, Mallonee S, & Istre GR (1999). Estimating the proportion of homes with functioning smoke alarms: A comparison of telephone survey and household survey results. American Journal of Public Health, 89(7), 1112–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graber JM, Macdonald SC, Kass DE, Smith AE, & Anderson HA (2007). Carbon monoxide: The case for environmental public health surveillance. Public Health Reports, 122(2), 138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson NB, & Weaver NK (2011). Residential carbonmonoxide alarm use: Opportunities for poisoning prevention. Journal of Environmental Health, 73(6), 30–33. [PubMed] [Google Scholar]
- Kao LW, & Nanagas KA (2005). Carbon monoxide poisoning. Medical Clinics of North America, 89(6), 1161–1194. [DOI] [PubMed] [Google Scholar]
- National Conference of State Legislatures. (2011). Carbon monoxide detector laws by state. Retrieved from http://www.ncsl.org/default.aspx?tabid=13238
- Raub JA, Mathieu-Nolf M, Hampson NB, & Thom SR (2000). Carbon monoxide poisoning—a public health perspective. Toxicology, 145(1), 1–14. [DOI] [PubMed] [Google Scholar]
- Runyan CW, Johnson RM, Yang J, Waller AE, Perkis D, Marshall SW, Coyne-Beasley T, & McGee KS (2005). Risk and protective factors for fires, burns, and carbon monoxide poisoning in U.S. households. American Journal of Preventive Medicine, 28(1), 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GA, Splaingard M, Hayes JR, & Xiang H (2006). Comparison of a personalized parent voice smoke alarm with a conventional residential tone smoke alarm for awakening children. Pediatrics, 118(4), 1623–1632. [DOI] [PubMed] [Google Scholar]
- Yoon SS, Macdonald SC, & Parrish RG (1998). Deaths from unintentional carbon monoxide poisoning and potential for prevention with carbon monoxide detectors. Journal of the American Medical Association, 279(9), 685–687. [DOI] [PubMed] [Google Scholar]