Abstract
Sweet’s syndrome, or acute febrile neutrophilic dermatosis, has previously been associated with underlying inflammatory bowel disease; however, there are fewer than 50 case reports of such an association. Herein, we describe a young woman with Crohn’s disease who presented with abrupt onset of a painful, tender erythematous rash on the dorsal hands and face.
Keywords: Acute febrile neutrophilic dermatosis, Crohn’s disease, inflammatory bowel disease, Sweet’s syndrome
Sweet’s syndrome is an acute febrile neutrophilic dermatosis characterized by abrupt onset of tender erythematous plaques, nodules, or papules affecting the face, neck, or upper limbs, along with symptoms that frequently include fever, recent history of upper respiratory infection (URI), malaise, and leukocytosis with neutrophilia.1 Sweet’s syndrome is classified into five different categories: idiopathic, para-inflammatory, paraneoplastic, drug induced, and pregnancy associated.2 Autoimmune and inflammatory conditions including inflammatory bowel disease have been linked as underlying etiologies. There are less than 50 reports of Crohn’s-associated Sweet’s syndrome since its description in 1964.3–5 Here we report a case of Sweet’s syndrome that presented in a patient with well-controlled Crohn’s disease.
Case Description
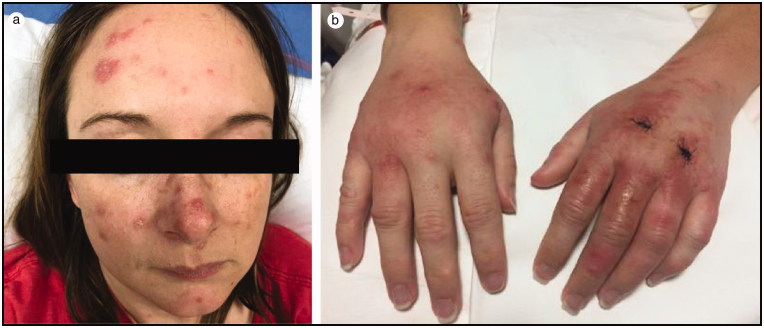
A 31-year-old woman with well-controlled Crohn’s disease (on infliximab) presented with a 1-week history of painful, erythematous nodules and plaques on her face and dorsal left hand. Three days prior to her presentation, she had been prescribed systemic and topical antibiotics for a presumed bacterial skin infection. Her condition did not improve but instead continued to worsen with increasing pain and redness. On admission, she denied any symptoms of a Crohn’s flare. She endorsed subjective fever and recent URI. On physical exam the patient’s vital signs were within normal limits. She had painful, erythematous nodules and plaques asymmetrically distributed on edematous dorsal hands with some lesions appearing pseudovesicular. Similar erythematous papules and larger plaques were present on the forehead, cheeks, chin, nose, ears, and upper cutaneous lip. Some of these plaques had overlying yellowish scale (Figure 1). The patient’s erythrocyte sedimentation rate (ESR) was elevated at 61 mm/h and C-reactive protein (CRP) at 8.8 mg/L. In the context of the clinical and pathological appearance, pain, subjective fevers, recent URI, history of inflammatory bowel disease, and elevated ESR/CRP, the patient met two major and three minor criteria for the diagnosis of Sweet’s syndrome.6
Figure 1.
(a) Erythematous facial papules and plaques and (b) painful, erythematous nodules and plaques on the dorsal hands and wrists. Biopsy sites of the dorsal left hand are seen.
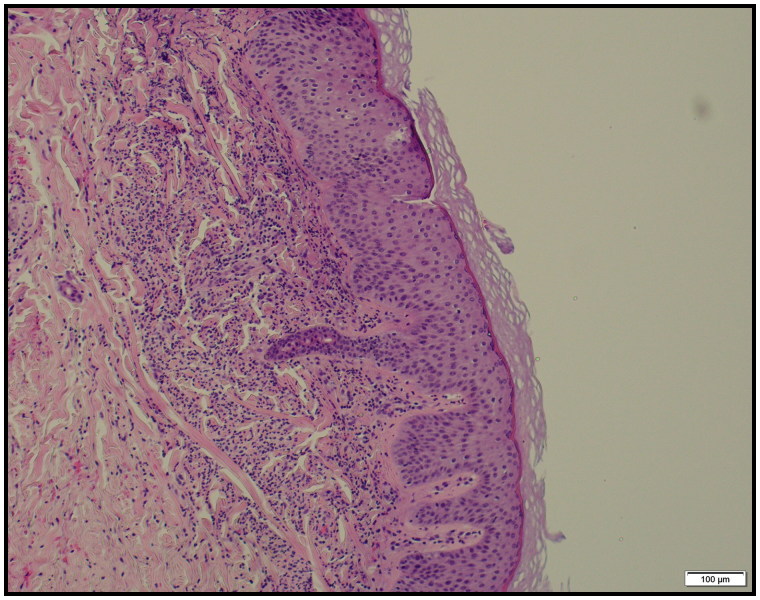
Punch biopsy of the left dorsal hand revealed a diffuse neutrophilic infiltrate predominantly in the upper dermis with associated extravasated red blood cells and rare eosinophils. The epidermis was not involved, and there was no definitive evidence of vasculitis. Dermal edema was not present and no organisms were identified with Grocott-Gomori’s methenamine silver stain and acid-fast bacilli stain. The overall features were consistent with a neutrophilic dermatosis and were compatible with Sweet’s syndrome (Figure 2).
Figure 2.
Skin biopsy of the hand with neutrophilic dermatosis. Hematoxylin and eosin, ×10.
The patient was started on 1 mg/kg prednisone after which rapid, dramatic improvement of her skin eruption was seen. The patient continued on 4 weeks of an oral prednisone taper. After discharge, she reported significant improvement in appearance and pain. After completing 2 weeks of 45-mg oral prednisone therapy, the patient was seen in the outpatient clinic and her rash had completely cleared.
Discussion
Although uncommonly associated with inflammatory bowel disease, when associated with Crohn’s or ulcerative colitis, Sweet’s has a strong predilection in women 30 to 50 years old.7 Less than 50 case reports have been described in association with Crohn’s disease, mainly with Crohn’s colitis.2 Pathological examination of classical Sweet’s syndrome demonstrates diffuse infiltration of neutrophils in the dermis accompanied by papillary dermal edema with no evidence of vasculitis.8
To diagnose classical Sweet’s syndrome, the patient must meet two of two major criteria—consisting of the sudden onset of tender, painful, erythematous nodules or plaques and histopathologic evidence of diffuse neutrophilic infiltrate in the dermis, without vasculitis. The patient must also meet at least two of four minor criteria: preceding fever; coexisting malignancy, inflammatory disease, pregnancy, or preceding upper respiratory or gastrointestinal infection; three of four abnormal laboratory values (elevated ESR, positive CRP, >8000 leukocytes, and >70% neutrophilic predominance); and dramatic improvement with systemic corticosteroids.6 Starting prednisone 1 mg/kg/day with a tapering dose over 4 to 6 weeks has shown to be effective, with lesions disappearing after a few weeks without scarring.1 Recurrence occurs in one-third of patients.7 In one-third of cases, Sweet’s presents concurrently at the time of diagnosis with Crohn’s, so it is important to consider Sweet’s syndrome in patients with established or suspected inflammatory bowel disease, because it could be considered an extraintestinal manifestation of Crohn’s.9 Early diagnosis is important, because response to treatment occurs rapidly.
References
- 1.Vaz A, Kramer K, Kalish RA. Sweet's syndrome in association with Crohn's disease. Postgrad Med J. 2000;76(901):713–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Catalán-Serra I, Martín-Moraleda L, Navarro-López L, et al. Crohn’s disease and Sweet’s syndrome: an uncommon association. Rev Esp Enferm Dig. 2010;102(5):331–337. doi: 10.4321/S1130-01082010000500009. [DOI] [PubMed] [Google Scholar]
- 3.Sweet RD. An acute febrile neutrophilic dermatosis. Br J Dermatol. 1964;76:349–356. [DOI] [PubMed] [Google Scholar]
- 4.Ytting H, Vind I, Bang D, Munkholm P. Sweet's syndrome—an extraintestinal manifestation in inflammatory bowel disease. Digestion 2005;72(2–3):195–200. doi: 10.1159/000088466. [DOI] [PubMed] [Google Scholar]
- 5.Foster EN, Nguyen KK, Sheikh RA, Prindiville TP. Crohn's disease associated with Sweet's syndrome and Sjögren's syndrome treated with infliximab. Clin Dev Immunol. 2005;12(2):145–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Su WP, Liu HN. Diagnostic criteria for Sweet's syndrome. Cutis 1986;37(3):167–174. [PubMed] [Google Scholar]
- 7.Cohen PR. Sweet’s syndrome—a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2(1):34. doi: 10.1186/1750-1172-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen PR, Kurzrock R. Sweet's syndrome revisited: a review of disease concepts. Int J Dermatol. 2003;42(10):761–778. [DOI] [PubMed] [Google Scholar]
- 9.Rappaport A, Shaked M, Landau M, Dolev E. Sweet's syndrome in association with Crohn's disease: report of a case and review of the literature. Dis Colon Rectum. 2001;44(10):1526–1529. [DOI] [PubMed] [Google Scholar]