Abstract
This study compared patient outcomes following irrigation applied using an automated pressure system (AP) to hand irrigation utilizing a syringe (HI) during ureteroscopy. Retrospective chart review was performed to evaluate ureteroscopy procedures without a ureteral access sheath. Procedures in which irrigation was applied by AP were compared to those with HI. Statistical analyses included chi-squared tests and Student's t tests. The AP group contained 206 procedures and the HI group, 25. The AP and HI groups were 54.9% and 36% male, respectively. Mean ages were 53.7 ± 18.9 years in the AP group and 44.0 ± 18.5 years in the HI group. Complication rates were 11.2% in the AP and 8.3% in the HI group (P > 0.99). One stone retrieval failure and one stone recurrence occurred in the HI group; one patient had residual stone in the AP group. No urinary tract infections occurred in the HI group; in the AP group, urinary tract infections occurred in 1.9% of cases. The postoperative pain incidence was equivalent (P = 0.498). The AP group had one subcapsular hematoma; no calyceal ruptures occurred in either group. In conclusion, irrigation applied by an automated setup appears safe, with similar outcomes to irrigation applied with a handheld syringe.
Keywords: Irrigation, ureteroscopy, urinary tract stones
Ureteroscopy is commonly performed for a variety of urological problems. During ureteroscopy, it is imperative that the physician is able to visualize the urinary tract to identify and remove stones or tumors and prevent damage to the urinary tract. A ureteral access sheath (UAS) is often used to facilitate passage of the ureteroscope in the ureter, improve visualization, and drain fluid as it accumulates in the urinary system, which decreases pressure in the urinary system.1–5 However, UAS may increase risk of injury to the mucosa of the urinary system, is not associated with improved outcomes, and cannot be used with semirigid ureteroscopy.1,6,7 Thus, alternative strategies for permitting entry and visualization during ureteroscopy are necessary. In one such strategy, saline irrigation is applied, either utilizing an automated pressure device or handheld syringe. Automated pressure system use during ureteroscopy/ureteroscope ureteroscopy is well established but does increase pressure in the urinary system compared to UAS, which can be damaging and lead to rupture or systemic inflammatory response syndrome.2,4,8–10 Advantages of the automated system are that constant pressure is applied, that the pressure values can be set such that they do not exceed certain values, and that surgeons are not forced to perform irrigation themselves during the procedure.8,11 However, peak pressures are higher with the handheld syringe.2,12 Thus, it is unclear which irrigation technique is better for patient outcomes. This study sought to evaluate whether the use of automated pressure during ureteroscopy in the absence of a UAS is safe and effective and to compare it to hand irrigation with a syringe.
Methods
After receiving institutional review board approval, a retrospective chart review was performed evaluating patients who had a ureteroscopy procedure without a UAS, either utilizing pressurized irrigation (AP) or using hand irrigation (HI), between February 2014 and January 2017. The inclusion criteria were any patient receiving a ureteroscopy regardless of indication. Patients in whom a UAS was utilized were excluded. The primary outcome reviewed was frequency of complications in each group. Secondary outcomes included frequency of return visits to the emergency department, urinary tract infections (UTIs), postoperative pain requiring treatment, procedure length, whether the procedure was successful, and occurrence of damage to the urinary tract such as ureteral ruptures and subcapsular hematomas.
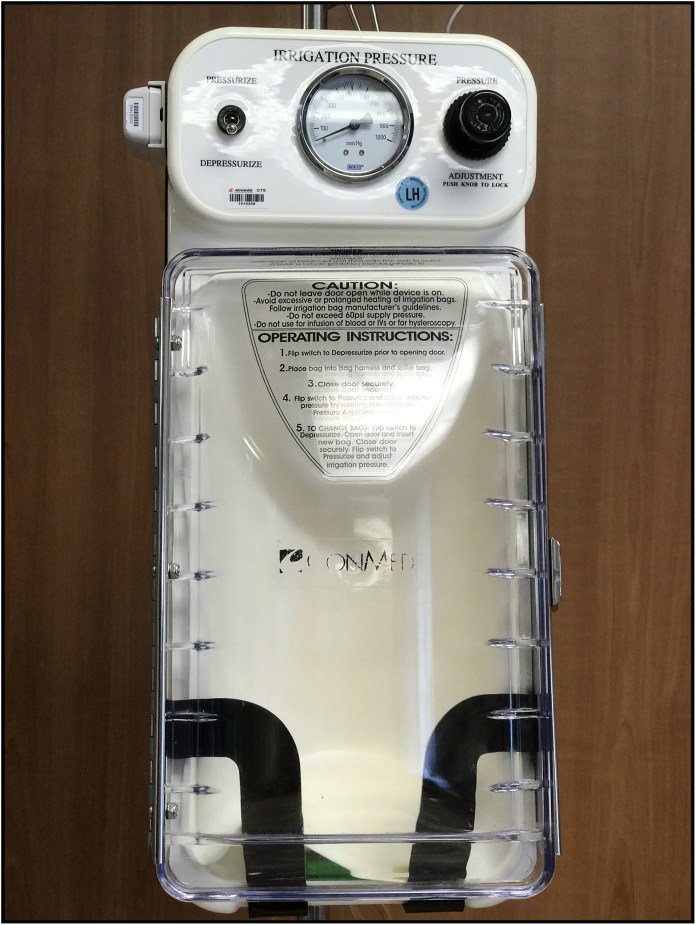
Following the introduction of the ureteroscope, pressure was applied to aid in visualization during the procedure. In the AP group, automated external compression was applied to the irrigation bag, as shown in Figure 1, with a maximum pressure set at 150 mm Hg. In the HI group, hand irrigation was performed using a 60 mL syringe and intravenous extension tubing, and the least required irrigation to aid visualization was injected.
Figure 1.
Automated pressure system.
Statistics were performed using Prism (GraphPad). Means and standard deviations were calculated, and chi-squared and Student’s t tests were performed where applicable. Significance was indicated by a P value <0.05.
Results
A total of 453 charts were reviewed between February 2014 and January 2017, representing 499 ureteroscopy procedures. Of these, 268 procedures were excluded because a UAS was used. In the 231 cases in which a UAS was not used, 206 patients received AP and 25 patients had HI due to surgeon’s preference. Patient characteristics by group are shown in Table 1. The AP group was 54.9% male and the HI group was 37.5% male (P = 0.13). Patients in the HI group tended to be younger, with a mean age of 44.0 ± 18.5 compared with the mean age of 53.7 ± 18.9 years in the AP group (P < 0.05). Most patients received ureteroscopy for the management of ureteral and kidney stones. All patients in the HI group had ureteroscopies for the management of stone disease. Of the 206 procedures in the AP group, 182 procedures were performed for stones, 23 were performed to evaluate or manage tumors, five were performed to manage strictures, one was performed for a calyceal diverticulum infundibular dilation, and one was performed for a retained stent (some procedures had more than one indication). The difference in stone location by group approached statistical significance (P = 0.052). Of the patients with stones, in the AP group 75.7% had ureteral stones while 19.9% had kidney stones. In the HI group, 75% had ureteral stones and 41.7% had kidney stones. In both groups, some procedures were performed for stones at multiple locations. Procedures were performed with a semirigid or flexible ureteroscope, with some patients receiving both. In the AP group, 65.5% received a semirigid ureteroscope and 37.4% received a flexible ureteroscope, while in the HI group 54.2% received a semirigid ureteroscope and 62.5% received a flexible ureteroscope (P = 0.04). Procedures for stone management also included various forms of stone procedures, including laser lithotripsy, basket extraction, and both. There was no difference in the rate at which the AP and HI groups received each of these procedures (P = 0.31). Thus, while there were some differences between the AP and HI groups, the groups were relatively similar.
Table 1.
Patient characteristics of those receiving two types of irrigation during ureteroscopy
| Characteristic | Automated pressure (n = 206) | Hand irrigation (n = 25) | P value |
|---|---|---|---|
| Age (years, mean ± SD) | 53.7 ± 18.9 | 44 ± 18.5 | 0.02* |
| Men | 54.9% | 37.5% | 0.13 |
| Body mass index (kg/m2) | 29.5 ± 6.7 | 31.9 ± 9.4 | 0.12 |
| Stone location | 0.05 | ||
| Ureter | 131 | 13 | |
| Kidney | 16 | 5 | |
| Both | 25 | 5 | |
| No stone | 34 | 1 | |
| Scope type | 0.04* | ||
| Rigid | 123 | 9 | |
| Flexible | 65 | 11 | |
| Both | 12 | 4 | |
| Stone manipulation | 0.31 | ||
| Laser lithotripsy | 14 | 0 | |
| Basket extraction | 65 | 12 | |
| Both | 73 | 7 | |
| Other | 7 | 0 | |
| Neither | 43 | 5 |
*p < 0.05.
It did not appear that the use of HI versus AP altered operative time; the mean operative time in the AP group was 59.2 ± 44.1 compared with 67.8 ± 35.0 minutes in the HI group (P = 0.36). As shown in Table 2, the complication rate was 11.2% in the AP group and 8.3% in the HI group (P > 0.99). Rate of return to the emergency department was 14.1% in the AP group and 25.0% in the HI group (P = 0.22). Most of the procedures were successful, with one failure to retrieve a stone due to the tightness of the ureter in the HI group and one retained stone in the AP group. In the AP group, only 1.9% (4/206) of cases were complicated by UTIs and there was only one case of pyelonephritis, while there were no instances of UTI in the HI group (P > 0.99). The incidence of postoperative pain, including bladder spasms, dysuria, ureteral spasms, and flank pain, was equivalent in the AP and HI groups, affecting 11.2% and 16.7%, respectively (P = 0.498). There was one instance of subcapsular hematoma in the AP group but none in the HI group. There were no occurrences of calyceal rupture or other urinary tract injury in either group (Table 3).
Table 2.
Patient outcomes of those receiving two types of irrigation during ureteroscopy
| Outcome | Automated pressure (n = 206) | Hand irrigation (n = 25) | P value |
|---|---|---|---|
| Complication | 11.2% | 8.3% | > 0.99 |
| Return to emergency department | 14.1% | 25.0% | 0.22 |
| Postprocedure pain | 11.2% | 16.7% | 0.498 |
| Urinary tract infection | 1.9% | 0.0% | > 0.99 |
Table 3.
Complications among those receiving two types of irrigation during ureteroscopy
| Complication | Automated pressure (n = 206) |
Hand irrigation (n = 25) |
||
|---|---|---|---|---|
| N | Highest Clavien-Dindo score | N | Highest Clavien-Dindo score | |
| Subcapsular hematoma | 1 | II | 0 | N/A |
| Urinary tract infection | 4 | II | 0 | N/A |
| Pyelonephritis | 1 | II | 0 | N/A |
| Abdominal pain | 0 | N/A | 2 | I |
| Acute abdomen | 1 | II | 0 | N/A |
| Clostridium difficile infection | 1 | II | 0 | N/A |
| Fever | 6 | II | 0 | N/A |
| Severe hematuria or bleeding requiring intervention | 6 | IIIa | 0 | N/A |
| Acute myocardial infarction | 1 | II | 0 | N/A |
| Chest pain | 1 | II | 0 | N/A |
| Atrial fibrillation | 1 | II | 0 | N/A |
| DVT/pulmonary embolism | 1 | II | 0 | N/A |
| Shortness of breath | 1 | I | 0 | N/A |
| Syncope | 1 | I | 0 | N/A |
| Seizure | 1 | II | 0 | N/A |
| AKI/acute renal failure | 0 | N/A | 1 | II |
AKI indicates acute kidney injury; DVT, deep vein thrombosis.
Discussion
The use of pressure during ureteroscopy makes it possible to instrument and visualize the urinary tract in the absence of a UAS. However, pressure has the potential to damage the urinary tract and thus must be employed judiciously. This study sought to compare the use of AP and HI. In this study, there was no difference in complication rates between the groups. Thus, it seems likely that both approaches are safe and effective.
There has been concern that irrigation may be a risk factor for UTIs and sepsis.10,13 However, a multivariate analysis performed by Zhong et al demonstrated that neither use of irrigation in the absence of a UAS nor irrigation by hand versus a pump was a risk factor for sepsis.10 This study did demonstrate that high irrigation flow rate or volume did increase the risk of sepsis following ureteroscopy. Our findings indicate that the risk of UTI is comparable following ureteroscopy with AP or HI.
Pain and urinary tract injury are also a concern, especially if high pressures are used.13 Pain occurred at similar rates in each group in this study (P = 0.498). There were no intraoperative complications in either group. In the AP group, one patient had a subcapsular hematoma but there were no other urinary tract injuries. Irrigation, and especially irrigation with high pressure, has been demonstrated to be a risk factor for postureteroscopy hematoma formation.14 Despite these concerns, it has not been demonstrated that the use of UAS decreases the likelihood of a renal hematoma. Thus, regardless of approach, it is essential to utilize the minimum irrigation pressure necessary to visualize the urinary tract to prevent urinary tract injuries.
Strengths of this study include the large sample size of the AP group and the heterogeneity of the procedures in both groups. Weaknesses include the small sample size of the HI group and the lack of urinary tract pressure measurements. In addition, there were some significant differences in the two samples, including the fact that the AP group was younger on average and the HI group had a higher prevalence of kidney stones and was more likely to receive a basket extraction alone than the AP group. Further study is needed to determine whether there are advantages to using either AP or HI. In addition, studies should be performed to analyze pressures found in the urinary tract when different methods of applying external pressure during ureteroscopy are employed and to correlate these pressures with outcomes to further refine pressure application techniques.
In conclusion, when a UAS is not used during ureteroscopy, the application of pressure with an automated system appears to have some advantages over irrigation applied by hand using a syringe. More study is necessary to confirm and refine this finding.
References
- 1.Breda A, Territo A, Lopez-Martinez JM. Benefits and risks of ureteral access sheaths for retrograde renal access. Curr Opin Urol. 2016;26(1):70–75. doi: 10.1097/MOU.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 2.Auge BK, Pietrow PK, Lallas CD, Raj GV, Santa-Cruz RW, Preminger GM. Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation. J Endourol. 2004;18(1):33–36. doi: 10.1089/089277904322836631. [DOI] [PubMed] [Google Scholar]
- 3.Stern JM, Yiee J, Park S. Safety and efficacy of ureteral access sheaths. J Endourol. 2007;21(2):119–123. doi: 10.1089/end.2007.9997. [DOI] [PubMed] [Google Scholar]
- 4.Rehman J, Monga M, Landman J, et al. Characterization of intrapelvic pressure during ureteropyeloscopy with ureteral access sheaths. Urology. 2003;61(4):713–718. [DOI] [PubMed] [Google Scholar]
- 5.Holden T, Pedro RN, Hendlin K, Durfee W, Monga M. Evidence-based instrumentation for flexible ureteroscopy: a review. J Endourol. 2008;22(7):1423–1426. doi: 10.1089/end.2007.0327. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan AG, Lipkin ME, Scales CD, Preminger GM. Use of ureteral access sheaths in ureteroscopy. Nat Rev Urol. 2016;13(3):135–140. doi: 10.1038/nrurol.2015.271. [DOI] [PubMed] [Google Scholar]
- 7.Geraghty RM, Ishii H, Somani BK. Outcomes of flexible ureteroscopy and laser fragmentation for treatment of large renal stones with and without the use of ureteral access sheaths: Results from a university hospital with a review of literature. Scand J Urol. 2016;50(3):216–219. doi: 10.3109/21681805.2015.1121407. [DOI] [PubMed] [Google Scholar]
- 8.Eshghi M. Pressure-controlled hydraulic dilation of the ureter: one-step ureteroscopy. J Urol. 1988;140(5):950–953. [DOI] [PubMed] [Google Scholar]
- 9.Jung H, Osther PJ. Intraluminal pressure profiles during flexible ureterorenoscopy. Springerplus. 2015;4(1):373. doi: 10.1186/s40064-015-1114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhong W, Leto G, Wang L, Zeng G. Systemic inflammatory response syndrome after flexible ureteroscopic lithotripsy: a study of risk factors. J Endourol. 2015;29(1):25–28. doi: 10.1089/end.2014.0409. [DOI] [PubMed] [Google Scholar]
- 11.Sakhadeo NB, Venkatesh R, Trafford P, et al. A new system of irrigation for ureteroscopy. Br J Urol. 1996;78(4):639–640. [DOI] [PubMed] [Google Scholar]
- 12.Wilson WT, Preminger GM. Intrarenal pressures generated during flexible deflectable ureterorenoscopy. J Endourol. 1990;4(2):135–141. doi: 10.1089/end.1990.4.135. [DOI] [Google Scholar]
- 13.Osther PJ, Pedersen KV, Lildal SK, et al. Pathophysiological aspects of ureterorenoscopic management of upper urinary tract calculi. Curr Opin Urol. 2016;26(1):63–69. doi: 10.1097/MOU.0000000000000235. [DOI] [PubMed] [Google Scholar]
- 14.Whitehurst LA, Somani BK. Perirenal hematoma after ureteroscopy: A systematic review. J Endourol. 2017; 31(5):438–445. doi: 10.1089/end.2016.0832. [DOI] [PubMed] [Google Scholar]