Abstract
We report a case of left upper lobe torsion in a patient who had a pneumothorax as a complication of subclavian venous access for an elective neurosurgical operation. Despite appropriate management of the pneumothorax, the patient’s chest radiograph did not improve. Computed tomography of the chest was concerning for left upper lobe torsion. Fiberoptic bronchoscopy revealed near complete obstruction of the left upper lobe bronchus. Review of computed tomography imaging before and after bronchoscopy and subsequent thoracotomy confirmed lobar torsion. Consideration of lobar torsion in the differential diagnosis of patients with persistently abnormal chest imaging despite appropriate management after complications of routine procedures is important for early recognition and intervention of a potentially life-threatening problem.
Keywords: Chronic obstructive pulmonary disease, lung torsion, pneumothorax
Lung torsion (LT) is rare but has a high degree of morbidity and mortality. Clinical suspicion in the appropriate setting with early recognition and intervention is necessary to minimize damage. Unfortunately, due to its limited incidence, LT is difficult to anticipate.
Case description
A 77-year-old man with a previous meningioma resection presented for an elective neurosurgical resection of recurrent tumor. Initially, he elected not to pursue additional therapies. Two years later, due to worsening vision changes and proptosis in his left eye, magnetic resonance imaging was performed, revealing progression of the tumor. Intraoperatively, a left-sided subclavian central line was placed; a chest radiograph (CXR) in the intensive care unit to confirm line placement revealed a new left-sided pneumothorax (Figure 1a) compared to the preoperative CXR. A chest tube was placed with complete reexpansion of the lung on CXR.
Figure 1.
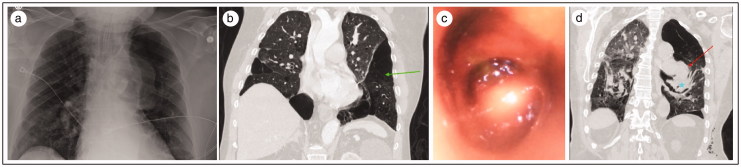
(a) Postoperative chest radiograph with left subclavian line and pneumothorax. (b) Coronal CT view of the thorax reveals bullous emphysematous changes in the left lower lobe (green arrow). The left upper lobe appears normal. (c) Bronchoscopic view of the left upper lobe shows abnormal configuration with distortion and occlusion of the subsegments. (d) Coronal CT view shows abrupt cutoff of the left upper lobe branches (red arrow) with swirling of airways (blue star) in the upward direction.
The patient was discharged but returned the next day when he noticed clear fluid draining from his nose upon bending over, prompting concern for a cerebrospinal fluid leak. The leak was repaired endoscopically. Postoperatively, the patient was kept sedated and intubated to minimize coughing. A CXR performed to confirm endotracheal tube placement again revealed a possible left pneumothorax. Computed tomography (CT) of the chest revealed left upper lobe partial torsion compared to a previous CT (Figure 1b). Bronchoscopy showed a luminal obstruction of the left upper lobe (Figure 1c) with invagination of mucosa that seemed to improve with passage of the bronchoscope.
Later, the patient was extubated, but a repeat CT showed persistent partial torsion (Figure 1d). The patient underwent a thoracotomy and the left upper lobe was detorsed. Postoperatively, he developed severe hypoxemic respiratory failure secondary to pulmonary embolism and complete consolidation of his left lung suspected due to ischemia-reperfusion injury with superimposed pneumonia requiring initiation of veno-venous extracorporeal membrane oxygenation. Subsequently, he developed profound shock with multiorgan failure. The family elected to withdraw care.
Discussion
LT is the parenchymal rotation of a lobe or whole lung around its corresponding bronchovascular pedicle, which results in the obstruction of the airway, arterial and venous blood supply, and lymphatic drainage.1 All-cause incidence ranges from 0.089% to 0.4%. The clinical manifestations of this disease occur as a result of concurrent obstruction of the bronchus, pulmonary artery, bronchial artery, pulmonary vein, and lymphatic drainage. Experimentally isolated pulmonary artery occlusion does not in itself cause infarction because the bronchial artery remains intact and protective.2 Similarly, bronchial arterial circulation does not cause ischemia alone and isolated venous occlusion can lead to pleural effusions and hemoptysis. While isolated occlusion of individual vascular components has not displayed ischemia experimentally, the clinical setting of LT usually involves pedicular rotation and occlusion of the entire lobar blood supply, which in turn leads to ischemia, gangrene, necrosis, systemic inflammatory syndrome, and ultimately acute respiratory distress syndrome.2 Anything increasing lobar/lung mobility is thought to increase risk for LT, including division/absence of the inferior pulmonary ligament, lung pedicle, and well-developed interlobular fissure (usually after right upper lobectomy).
LT is usually described under three circumstances: postoperative (63.4%), posttraumatic (8.3%), and spontaneous (29.4%).3 The most common surgeries associated with LT are lung resection (57%) and lung transplantation (14.7%).3 Predisposing factors for LT include conditions that can easily displace the lung in its cavitary space, including increased mobility from the inferior pulmonary ligament, transection of interlobar fissures causing loss of parenchymal bridging, increased displaceability from air or fluid, and a long left lobar pedicle.4
On CXR, LT can present as a consolidated or collapsed lobe.4 This was the most common finding in the reported cases of LT. Displacement of the pulmonary hilum of the atelectatic lobe and change in the pulmonary vasculature sweep are also key findings.4 An abrupt cutoff of the bronchus of the affected lobe is seen in many cases.5 LT can be diagnosed radiographically if the consolidated lobe’s position has changed, if the hilum of the involved lobe has been displaced, or if the pulmonary vasculature positioning and branching are abnormal.4 Chest CT is the study of choice and can show subtotal or total occlusion of the involved bronchus, including the collapsed lobe, that is key to make the diagnosis. It can also depict the altered relationship between the trachea and pulmonary arteries.5 In some cases, malrotation of the pulmonary vasculature can be seen in the mediastinal window with or without occlusion.6 Diagnosis requires an initial high index of suspicion since LT presents with nonspecific signs. The initial choice of diagnostics is CXR which, as stated above, usually shows progressive lung consolidation or opacification. CT imaging and/or bronchoscopy are then required for definitive diagnosis. Bronchoscopy usually shows bronchial occlusion or a fish mouth orifice, while CT imaging usually shows bronchial or vascular malposition or abrupt truncation.
Once a diagnosis of LT is made, interventional strategies must be pursued early—both to reduce mortality (the average mortality rate for LT is 8.3%) and to reduce complications from ischemia, including gangrene and infarction.5 Treatment strategies for LT involve repositioning or resection. Direct resection is preferred if lung tissue is thought to be nonviable intraoperatively. Signs of nonviable lung tissue include ischemic appearance, airless tissue, and edema. Although repositioning viable lung tissue does not affect mortality, repositioning ischemic lung tissue, either as an independent therapeutic option or before resection, is associated with higher mortality rates.5 This is likely due to reperfusion insults from reintroducing circulation to necrotic tissue and subsequent release of inflammatory substances.
This case highlights an often overlooked and fatal process. Patients with progressive consolidation or symptoms suggestive of an extensive inflammatory response of the lung in the setting of lung trauma, chest surgery, or processes that increase lung displacement need to have LT on the differential. LT is a time-sensitive process that carries significant mortality and complications and requires prompt diagnosis for surgical interventions.
References
- 1.Cable DG, Deschamps C, Allen MS, et al. Lobar torsion after pulmonary resection: presentation and outcome. J Thorac Cardiovasc Surg. 2001;122(6):1091–1093. doi: 10.1067/mtc.2001.117839. [DOI] [PubMed] [Google Scholar]
- 2.Gilkeson RC, Lange P, Kirby TJ. Lung torsion after lung transplantation: evaluation with helical CT. AJR Am J Roentgenol. 2000;174(5):1341–1343. doi: 10.2214/ajr.174.5.1741341. [DOI] [PubMed] [Google Scholar]
- 3.Dai J, Dong X, Wang H, et al. Predictors of survival in lung torsion: a systematic review and pooled analysis. J Thorac Cardiovasc Surg. 2016;152(3):737–745.e3. doi: 10.1016/j.jtcvs.2016.03.077. [DOI] [PubMed] [Google Scholar]
- 4.Felson B. Lung torsion: radiographic findings in nine cases. Radiology. 1987;162(3):631–638. doi: 10.1148/radiology.162.3.3809475. [DOI] [PubMed] [Google Scholar]
- 5.Fogarty JP, Dudek G. An unusual case of lung torsion. Chest. 1995;108(2):575–578. [DOI] [PubMed] [Google Scholar]
- 6.Chung SH, Nam JE, Choe KO, et al. Radiologic findings of lung lobe torsion in reconstructed multidetector computed tomography image lead to early detection. Clin Imaging. 2010;34(5):400–403. doi: 10.1016/j.clinimag.2009.10.035. [DOI] [PubMed] [Google Scholar]