Abstract
Diet has an important role in the treatment and prevention of chronic illnesses. Physicians are regarded as having proficient knowledge about nutrition, but most believe that they lack an understanding of clinical nutrition. In fall 2016, a group of medical students developed a culinary medicine elective for 20 students at Texas Tech University Health Sciences Center School of Medicine in Lubbock that included four didactic sessions and four interactive cooking labs that culminated in a final contest. The elective was meant to educate medical students about nutrition and dietary habits for their own benefit and that of their future patients. Surveys were administered to participants before and after the elective. Results showed a significant increase in confidence in overall culinary skill level, knowledge of ingredients, knowledge of cooking techniques, and ability to use kitchen supplies (P = 0.002, 0.002, 0.0004, and 0.003, respectively). The culinary medicine elective appears to be a valuable addition to the medical school curriculum.
KEYWORDS: Culinary medicine, medical education, nutrition, preventive medicine
The evidence-based field of culinary medicine is a fusion of the science of medicine with the art of cooking put in a practical context to help improve the health of patients.1 Confidence in delivery of cost-effective lifestyle changes can improve dialogue with patients regarding the health risks of chronic diseases and can help address the challenges of patient compliance.2 Chronic diseases are responsible for 86% of annual health care spending and make up 7 of the top 10 causes of death in the USA.3 A recent JAMA publication revealed that diet is now the number one risk factor for morbidity and mortality in the USA.4 With chronic disease epidemics (e.g., diabetes) on the rise, it is vital that US medical schools improve the proficiency of physicians’ integration of preventive medicine into patient care.5 Patients can be empowered to take an active role in their care, leading to better well-being and lower medical costs through primary prevention.1 At the Texas Tech University Health Sciences Center School of Medicine, we became aware of the paucity of nutritional instruction in our curriculum. The objective of this project was to develop and implement a culinary medicine elective into our medical training. We hypothesized that students would be better equipped with and confident in their knowledge and skills in culinary medicine concepts after completing the elective.
Methods
This observational hypothesis-driven study consisted of 20 first- and second-year medical students at the Texas Tech University Health Sciences Center School of Medicine. This size was chosen due to a limited number of cooking stations in the lab, and student selection was based on availability for teaching sessions. Detailed educational objectives were created to guide the elective (Table 1). Before the start of the elective, a baseline survey was conducted to establish student self-assessment on a scale from 1 to 5 with categories of overall culinary skill, knowledge of ingredients, knowledge of cooking techniques, and ability to use kitchen supplies. The reported change of these variables after the elective was analyzed using the Mann-Whitney U test, which was appropriate based upon relative ranks. Another pre-elective survey was given with a mix of multiple-choice questions on a Likert scale and open-ended questions to assess nutritional knowledge and confidence, cooking habits, and factors that contribute to the success of a physician in promoting lifestyle changes. The same initial surveys were administered a month after conclusion of the elective to assess changes in perspectives and long-term retention. All surveys were submitted anonymously to avoid potential bias.
Table 1.
Educational objectives and future directions for the culinary medicine elective
| Educational objectives | Future directions |
|---|---|
|
|
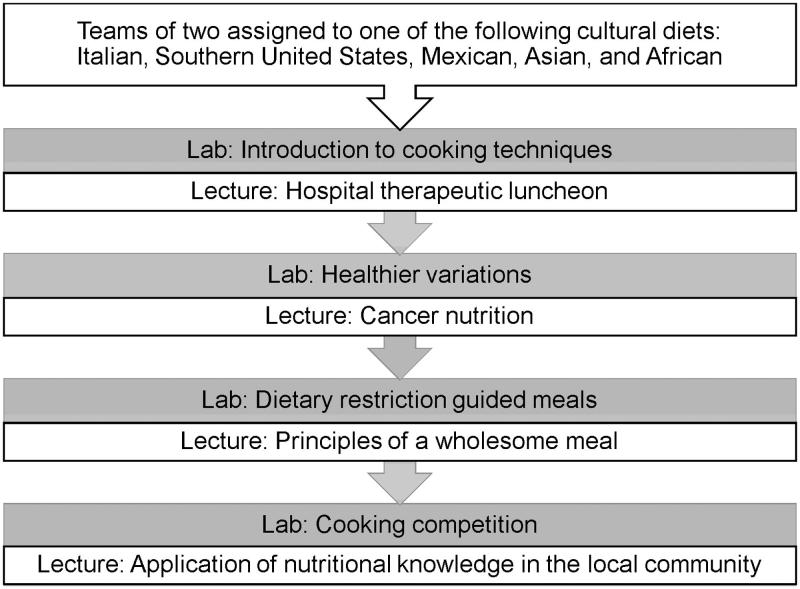
The elective consisted of four didactic sessions and four interactive labs and took place during the fall 2016 semester. Topics covered for each lab and lecture are outlined in Figure 1. Local chefs assisted with the hands-on cooking segments and gave demonstrations of select cooking skills. The labs were conducted at the Texas Tech University College of Human Sciences cooking lab in Lubbock.
Figure 1.
Overall structure of the elective, showing topics covered for each lab and lecture. In the first lecture, the hospital dietitians explained individualized diets prescribed in an inpatient setting, identifying modifications for various health conditions such as kidney disease, diabetes, and hyperlipidemia.
Students were divided into teams of two and assigned to one of five cultural diets—Chinese, Mediterranean, Nigerian, Central American, and US Southern cuisine—as related to a patient. Student teams were assigned a new culture for each lab to expand the breadth of cultural experience. Patient profiles were as follows:
A 42-year-old Southern man with a history of elevated cholesterol levels presenting for a routine primary care visit.
An 80-year-old Italian woman concerned about poor appetite and dealing with chronic kidney disease.
A young Hispanic couple dealing with diabetes. The husband has been losing weight quickly and is concerned with what he can and cannot eat.
A 65-year-old Asian woman with questions about osteoporosis after a few family members had been recently diagnosed with it.
A 38-year-old Nigerian man interested in the DASH (Dietary Approaches to Stop Hypertension) diet he heard about from a friend.
Each lab session began with a presentation by a local chef that featured a demonstration of specific cooking skills or a discussion of basic cooking concepts such as grain‐water ratios, proper use of cutting utensils, and indications for various cooking oils. After the presentation, the chef joined the members of the elective planning team who volunteered to act as teaching assistants in helping students as needed. Sampling of each other’s creations was highly encouraged in students, not only to compare differences between cuisines and dietary restrictions but to demonstrate how the foods changed from week to week.
For the first lab, an experienced local chef selected recipes that established a typical example for each cuisine that did not adhere to current public health guidelines. These recipes utilized essential cooking skills such as filleting a chicken breast or chopping an onion. Students created recipes for the second lab that were meant to be more health conscious (e.g., with lower sodium, incorporation of essential micronutrients, etc.) than those used in the first lab by making changes in ingredients and cooking techniques. Elective team members created recipes for the third lab that addressed specific health concerns (e.g., kidney disease, osteoporosis, or diabetes). This week also featured a food preparation skills challenge in which each student chopped an onion and the guest chef evaluated his or her performance. The team with the highest score was able to choose their own criteria for the final cooking competition-themed lab. The final lab challenged students to apply what they had learned in previous lab sessions by randomly assigning them financial, dietary, and cultural criteria to use in their task of creating a meal for a family of four. Possibilities included a $15 or $20 budget for financial criteria; chronic kidney disease, hypertension, diabetes, osteoporosis, or hyperlipidemia for dietary criteria; and Southern, Hispanic, Caribbean, Asian, or Italian cuisines for cultural criteria. Health Science Center faculty judges were present to taste students’ creations and utilized a judging rubric that evaluated taste, health (adherence to diet assigned), nutritional information (understanding and ability to convey nutritional value of the meal to the judges), cost-effectiveness, presentation, and overall integration of components. Each area was evaluated on a scale of 1 to 5, with the taste score being multiplied by two. Scores were compiled, which then revealed the team that was most successful in their application of nutritional concepts learned throughout the lab.
Results
Twenty-two first- and second-year medical students who applied were examined for eligibility. Twenty of those students were selected to be included in the elective; two were found to be unavailable on elective dates. Eighteen students (90%) completed the pre-elective survey, and 17 (85%) completed the postelective survey. Self-assessment of various nutrition-related categories on a scale of 1 to 5 showed significant improvement between pre-elective and postelective surveys. Overall culinary skill level, knowledge of ingredients, knowledge of cooking technique, and ability to use kitchen supplies all increased significantly (Table 2). This increase indicated that participants were more confident and comfortable with their knowledge and skill levels. Questions pertaining to diets showed that in the pre-elective survey, 11 of 18 participants had never heard of the DASH diet, whereas in the postelective survey, 14 indicated that they would recommend that a patient continue this diet.
Table 2.
Survey results before and after culinary medicine elective
| Survey question | Median response (scale 1–5) |
P value | |
|---|---|---|---|
| Pre-elective | Postelective | ||
| Overall culinary skill level | 3 | 4 | 0.0022 |
| Knowledge of ingredients | 3 | 4 | 0.0022 |
| Knowledge of cooking technique | 2 | 4 | 0.0004 |
| Ability to use kitchen supplies | 3 | 4 | 0.0034 |
Factors affecting personal dietary habits were evaluated on a 1 to 5 Likert scale, with 1 being not at all and 5 being very strongly. We asked, “How strongly do the following impact your daily ability to eat a healthy diet?” with the options of unsure what is healthy, lack of time, low interest in cooking, low interest in cleaning up after, money/cost, and family/roommates. The top three responses in order of impact on personal dietary habits were lack of time, low interest in cleaning up after, and money/cost.
Factors that contribute to the success of a physician in promoting positive lifestyle changes were evaluated on a 1 to 5 Likert scale, with 1 being most significant and 5 being least significant. The choices included physician training/knowledge, patient compliance, physician‐patient relationship, appointment length, and patient misinformation. The three factors with the highest significance (as perceived by our participants) were patient compliance, physician knowledge/training, and patient misinformation.
From the set of three open-ended questions that assessed students’ opinions of the elective, we found that all of the students enjoyed the elective and found the elective to be a good learning experience. The first question asked, “If your skills improved, tell us more about how they improved.” Nine students commented on improvement in knife skills. For the question “If your knowledge of food did improve, tell us more about how it improved,” four students mentioned knowledge of culturally diverse dishes and eight highlighted their knowledge of dietary restrictions. One student wrote, “My knowledge concerning the nutritional value of certain foods improved, and I felt [it] helped me answer more questions on what comprises a nutritional meal.” Finally, the third question asked, “Do you have any recommendations on ways we can make the lab experience better?” Recommendations included “providing additional recipes in each cultural type of food” and gaining access to more cooking tools/supplies.
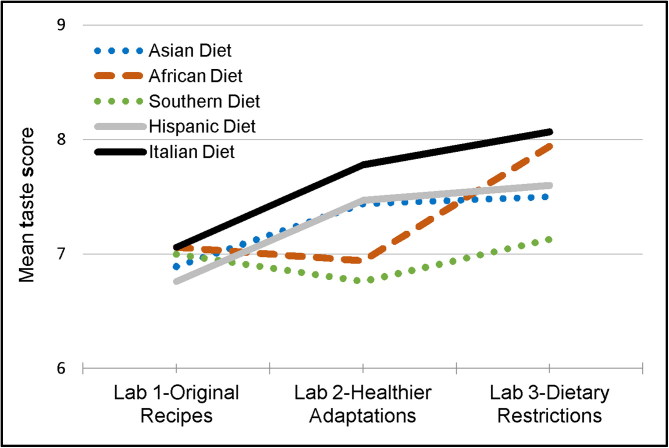
Average taste ratings for the dishes of each of the five cuisines increased across lab sessions as more health-oriented and medically indicated dietary restrictions were imposed (Figure 2). Although this change may be attributed to the increased culinary skill level of the students, this finding may serve to dispel myths that dishes modified to be healthier are lacking in taste.
Figure 2.
Mean taste score for different diets over the course of the three labs.
Discussion
Inadequate knowledge and low confidence in making patient-specific recommendations on dietary and lifestyle changes discourage physicians from engaging in regular nutritional counseling.6 These issues can be addressed by implementing nutrition training in the preclinical years of medical school and integrating additional information throughout student and physician careers. Evidence-based research has shown that medical students endorsed greater competency in educating their patients using nutritional interventions after being exposed to nutritional modules compared to those who did not.5 With this increase in self-competency, dietary interventions that have been proven to have a significant impact on cardiovascular disease will be easier to implement by students.7 A continuing education conference uniting medical and culinary professionals found that participants reported a significant increase in frequency of cooking their own meals and felt more confident counseling patients regarding weight loss.8 As future physicians become increasingly familiar with principles of nutrition, prevention of noninfectious disease can start to shift from secondary and tertiary toward primary.
Nutrition instruction can occur as part of an existing related course, presented in the form of modules, or via problem-based learning.9 Because clear-cut objectives for educating medical students about nutrition do not yet exist, medical schools interested in adopting a culinary program must familiarize themselves with schools that have an established nutrition program.10 The optimal guide would be nutrition education paired with the goals of the Accreditation Council for Graduate Medical Education.7 The Nutrition in Medicine study surveyed medical schools across the nation and found that less than one-third met the minimum of 25 hours of nutritional education and only 2.5% provided nutrition counseling skills in their curriculum. Although the requirement for nutritional education hours across medical schools has remained stagnant according to the Nutrition in Medicine surveys, electives similar to the culinary medicine elective at Texas Tech can help inspire others to create similar programs.2
This hypothesis-driven study had some limitations. First, the intervention was done at a single institution, limiting variability. Second, the study sample was small due to space limitations of the cooking lab and therefore did not include the entire medical school class. Third, fewer students responded to the nutrition knowledge and confidence postsurvey, which may have impacted our results. Fourth, the surveys were done anonymously on a voluntary basis, and it was difficult to assess who had not completed the survey. Fifth, without a control group, no causal relationships can be drawn between the culinary medicine curriculum and improvement in nutritional knowledge and culinary skills. Sixth, due to limitations regarding the availability of pairing information of pre and post values, the reported P values were based upon the two-sample t test, which may be inappropriate given the likely dependence between our pre and post groups. Finally, the short length of the course gave students limited exposure to the elective material, and we were not able to assess long-term retention of the learned knowledge.
Based on these findings, we conclude that the culinary medicine elective is a meaningful and worthwhile intervention for future physicians because it succeeded in improving student culinary medical knowledge and skill. We can infer from our research that this cohort is more comfortable with nutrition after the intervention and may more readily incorporate diet into their patients’ treatment plans. This elective can be expanded in future years to encompass the application of that knowledge, tested by an objective structured clinical examination focused on lifestyle medicine.
Funding Statement
The Office of Curriculum at TTUHSC provided funding for this first-time elective.
Acknowledgments
The authors thank Jaden Fackrell and Jimbo Ruiz for help in the creation of this elective; Dr. Webster, associate professor of medical education and cell biology and biochemistry at Texas Tech University Health Sciences Center (TTUHSC), for reviewing the article; and Phillip Watkins and Dr. Eneko Larumbe of the TTUHSC Clinical Research Institute for advice regarding statistical analysis. Additionally, the authors thank the Texas Tech University College of Human Sciences for lending cooking lab space; Crafthouse Gastropub and Top Tier Catering for original recipe development and leading classes; and Ruiz Wholesale for donating kitchen supplies for the cooking labs. Finally, the authors thank Margaret Vugrin from the Preston Smith Library at TTUHSC and all of the teaching assistants who volunteered their time.
References
- 1.La Puma J. What is culinary medicine and what does it do? Popul Health Manag. 2016;19:1–3. doi: 10.1089/pop.2015.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams KM, Butsch WS, Kohlmeier M. The state of nutrition education at US medical schools. J Biomed Educ. 2015;2015:1–7. doi: 10.1155/2015/357627. [DOI] [Google Scholar]
- 3.Centers for Disease Control and Prevention Chronic disease prevention and health promotion. https://www.cdc.gov/chronicdisease/overview/index.htm. Published 2017. Accessed November 5, 2017.
- 4.Mokdad AH, Ballestros K, Echko M, et al. The state of US health, 1990–2016. JAMA. 2018;319:1444–1472. doi: 10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birkhead AG, Foote S, Monlezun DJ, et al. Medical student-led community cooking classes: a novel preventive medicine model that’s easy to swallow. Am J Prev Med. 2014;46:e41–e42. doi: 10.1016/j.amepre.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010;304:202–203. doi: 10.1001/jama.2010.903. [DOI] [PubMed] [Google Scholar]
- 7.Crawford AL, Aspry KE. Teaching doctors-in-training about nutrition: where are we going in 2016? R I Med J (2013). 2016;99:23–25. [PubMed] [Google Scholar]
- 8.Eisenberg DM, Myrdal Miller A, McManus K, Burgess J, Bernstein AM. Enhancing medical education to address obesity: “See one. Taste one. Cook one. Teach one.” JAMA Intern Med. 2013;173:470–472. doi: 10.1001/jamainternmed.2013.2517. [DOI] [PubMed] [Google Scholar]
- 9.Adams KM, Kohlmeier M, Powell M, Zeisel SH. Nutrition in medicine. Nutr Clin Pract. 2010;25:471–480. doi: 10.1177/0884533610379606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Polak R, Phillips EM, Nordgren J, et al. Health-related culinary education: a summary of representative emerging programs for health professionals and patients. Glob Adv Health Med. 2016;5:61–68. doi: 10.7453/gahmj.2015.128. [DOI] [PMC free article] [PubMed] [Google Scholar]