Abstract
Background:
The existence of racial and ethnic disparities in leg amputations rates is well documented. Despite this, approaches to addressing these alarming disparities have been hampered by the inability to identify at-risk individuals in a region and design targeted interventions. We undertook this study to identify small geographic areas in which efforts focused on high-risk individuals with peripheral artery disease (PAD) could address disparities in leg amputation rates.
Methods:
We used de-identified Texas state admission data to identify PAD-related admissions associated with an initial revascularization (leg angioplasty or leg bypass) or an primary leg (above-ankle) amputation between from 2004 through 2009.
Results:
21,273 major initial procedures were performed in Texas from 2004 through 2009 for PAD-related diagnoses, including 16,898 revascularizations and 4,375 leg amputations. A multivariate logistic regression demonstrated that an initial leg amputations done without revascularization was significantly associated with, among other variables: people categorized as black (odds ratio [OR] 1.79) or Hispanic (OR 1.42); those with Medicaid coverage (OR 1.89); and those treated at low volume hospitals (OR 1.78; p<0.001 for all). Four geographic regions were identified with significantly higher risk-adjusted leg amputation rates. Of the 349 Texas hospitals performing major procedures, 72 (21%) reported no revascularization procedures during the six year period studied.
Conclusions:
Prevention efforts directed at specific geographic areas may be more likely to reach at-risk people with PAD and thereby reduce leg amputations disparities in Texas. Such efforts might also find strategies to direct patients toward higher volume centers with higher revascularization rates.
Keywords: leg amputation, bypass, disparities, race, ethnicity
Introduction
Many previous have previously reported lower rates of revascularization and higher rates of leg amputations among people with peripheral artery disease (PAD) who are categorized as black or Hispanic, are uninsured, have Medicare or Medicaid as a payer, or live in high poverty areas1–11. Other work has also demonstrated significantly higher risk-adjusted rates of leg amputations in the Gulf Coast region of the United States, including much of southern and southeastern Texas12. Leg amputation greatly impacts quality of life and function, and associated costs are high13.
Disparities in leg amputation are attributable to complex interaction of policy factor, such as access to healthcare and modes of healthcare finance; institutional and provider factors, such as experience, use of guidelines, stereotyping and biases; and patient factors, such as compliance and medical service seeking behavior.14 Accordingly, the unevenly-high rates of leg amputation will likely persistent till we apply a comprehensive strategy that incorporate multi-level interventions to address these these complex groups of factors. Despite extensive reporting of these disparities, governmental organizations, advocates, and others seeking to eliminate these disparities through prevention efforts are often left without a starting point. We undertook this study to identify specific geographic areas in Texas with high rates of leg amputations that might provide foci for prevention efforts targeted at high-risk individuals.
Methodology
Study Subjects
The population of interest was adults who underwent either lower extremity revascularization or primary leg amputation (as outcome variables) within the state of Texas for PAD and foot pathologies including infection, gangrene or non-healing ulcers. Lower extremity revascularization procedures include endovascular interventions (angioplasty and stenting) as well as lower extremity bypass (incl. femoropopliteal and femorotibial). A leg amputation was defined as an amputation done at or above the level of the ankle. For the purposes of this study, a primary leg amputation was a leg amputation performed without any vascular imaging (such as angiogram or arterial ultrasound) or revascularization during the same hospital stay.
De-identified hospital admission data from Texas Inpatient Public Use Data File between 2004 and 2009 was used to identify the study population. ICD-9 and procedural codes were used to identify patients who had either revascularization or leg amputation (see Supplemental Tables A and B). We included patients only if at least one of the admission diagnosis codes documented both PAD and some foot pathology such as gangrene, ulcer, or infection (incl. osteomyelitis). We excluded patients who were under 18 years of age at the time of admission. We excluded patients who underwent amputation and had any diagnosis code suggesting an indication related to major trauma, congenital or developmental orthopedic problems, or complications of a previous leg amputation. Unless otherwise specified, persons categorized as “black” include persons categorized in the dataset as either “non-Hispanic black” or “Hispanic black”, and persons categorized as “Hispanic” include “Hispanic white” and “Hispanic other race” but not “Hispanic black”.
Regional and Hospital Characteristics
Public health service regions, as defined by the Texas Department of State Health Services (https://www.dshs.texas.gov/regions/), were used to categorize patients into geographic areas. The prevalence of poverty within the zip code of residence was obtained from U.S. Census Bureau data.
We considered a hospital’s experience with lower extremity revascularization or leg amputations as a study sample unit. The sample therefore is the total number of lower extremity revascularization and leg amputation procedures for the population of interest during the 2004 to 2009 study period. Hospitals were then categorized into quartiles based on the proportion of total procedures done in the state during that time. For example, a hospital was in the first quartile if it was among the highest volume hospitals that accounted for 25% of state’s volume during that time and in the fourth quartile if it was among the lowest volume hospitals that accounted for 25% of the state’s volume during that time.
Statistical analysis
Descriptive statistics are reported using medians and 25–75% interquartile ranges unless denoted otherwise. Nonparametric analyses, including Chi-squared tests for binary variables and the Mann-Whitney test for continuous variables, were used for all comparisons. Multivariate logistic models were created with primary leg amputation (i.e. amputation done without an attempted revascularizaton during the index hospitalization) as the dependent variable. These multivariate models were built using a combination of forward and backwards stepwise regression. Variables remained in the final model only if associated with a p-value of less than 0.05. Variables with more than 10% missing data were omitted from the multivariate analysis. Intercooled Stata version 8.2 (StataCorp, College Station, TX) was used for all statistical analyses. A p-value of <0.05 was considered statistically significant.
Results
Characteristics of Texans with PAD who Underwent Primary Leg Amputation
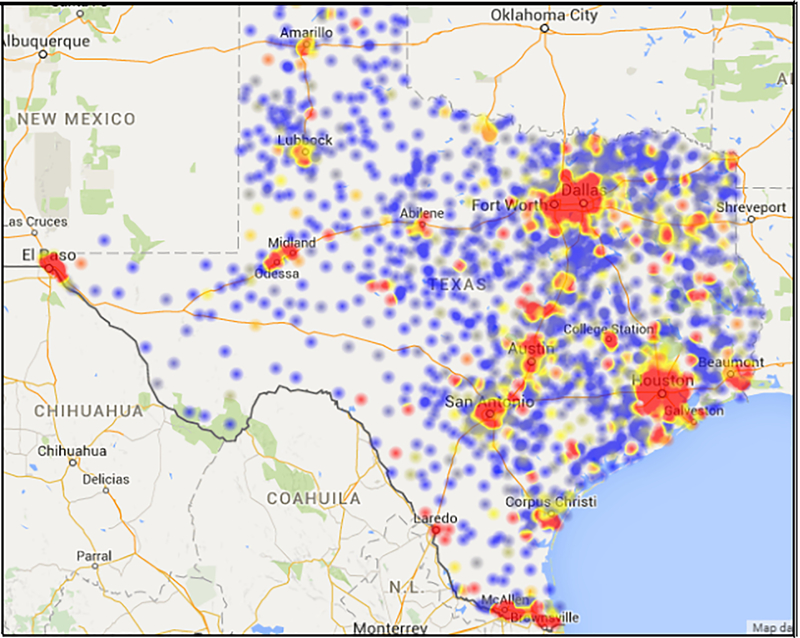
In total, 21,273 patients with PAD and foot complications underwent revascularization or leg amputations in Texas from 2004 through 2009. Of these, 16,898 (79%) were revascularizations and 4,375 (21%) were primary leg amputations. Compared to those that underwent revascularization, persons who underwent primary leg amputation had a higher prevalence of diabetes, heel ulcers, foot infections, and foot osteomyelitis (p<0.01 for all; Table 1). Primary leg amputation was more frequently performed among persons who were 75 years or older, black, or Hispanic, and was less performed often among Native Americans. Significantly higher proportions of patients who lived in the South Plains, Texarkana, Central Texas, West Central and Rio Grande Valley regions underwent primary leg amputation compared to revascularization, while a significantly higher proportion of patients who lived in the Panhandle, the Houston-Galveston and the Dallas-Fort Worth-Arlington metropolitan areas underwent revascularization. People that underwent primary leg amputation were also more frequently covered by Medicaid and Medicare or uninsured and less often by commercial insurance, health-maintenance organization or preferred provider organizations, or other payers. Finally, people that underwent primary leg amputation were more often admitted to the hospital through the emergency department or other routes categorized as urgent (see Table 1). Most leg amputations for people with PAD and foot complications occurred within the major metropolitan areas of the state (Figure 2).
Table 1:
Demographic, geographic and clinical characteristics of Texans who underwent revascularization or leg amputation for a diagnosis of PAD and foot pathology, 2004–2009. Numbers in parenthesis represent the proportion of the column total.
| Variable | All patients (n=21,273) | Revascularization (n=16,898) | Primary leg amputation (n=4,375) | p-value |
|---|---|---|---|---|
| Diabetes | 9,396 (44.2) | 7,012 (41.5) | 2,384 (54.5) | <0.001 |
| Heel ulcer | 254 (7.2) | 164 (5.7) | 90 (13.7) | <0.001 |
| Foot infection | 4,426 (20.8) | 2,467 (14.6) | 1,959 (44.8) | <0.001 |
| Foot osteomyelitis | 1,453 (6.8) | 930 (5.5) | 523 (12.0) | <0.001 |
| Gender | 0.137 | |||
| Male | 12,286 (57.8) | 9,733 (57.6) | 2,553 (58.4) | |
| Female | 8,339 (39.2) | 6,666 (39.5) | 1,673 (38.2) | |
| Missing/Deidentified | 648 (3.1) | 499 (3.0) | 149 (3.4) | |
| Age | ||||
| 18–44 years | 408 (1.9) | 320 (1.9) | 88 (2.0) | 0.61 |
| 45–64 years | 6,781 (31.9) | 5,672 (33.6) | 1,109 (25.4) | <0.001 |
| 65–74 years | 6,406 (30.1) | 5,310 (31.4) | 1,096 (25.1) | <0.001 |
| 75+ years | 7,678 (36.1) | 5,596 (33.1) | 2,082 (47.6) | <0.001 |
| Race & ethnicity | ||||
| non-Hispanic white | 11,340 (53.3) | 9,456 (56.2) | 1,844 (42.2) | <0.001 |
| non-Hispanic black | 3,423 (16.1) | 2,457 (14.5) | 966 (22.1) | <0.001 |
| Hispanic white | 1,423 (6.7) | 986 (5.8) | 437 (10.0) | <0.001 |
| Hispanic black | 16 (0.1) | 13 (0.1) | 3 (0.1) | 0.86 |
| Hispanic other race | 3,926 (18.5) | 3,037 (18.0) | 889 (20.3) | <0.001 |
| Asian | 143 (0.7) | 109 (0.7) | 34 (0.8) | 0.34 |
| Native American | 216 (1.0) | 197 (1.2) | 19 (0.4) | <0.001 |
| All other races, non-Hispanic | 786 (3.7) | 603 (3.6) | 183 (4.2) | 0.06 |
| Region | ||||
| Panhandle | 745 (3.5) | 616 (3.7) | 129 (3.0) | 0.03 |
| South Plains | 610 (2.9) | 448 (2.7) | 162 (3.7) | <0.001 |
| Dallas/Fort Worth/Arlington | 4,412 (20.8) | 3,688 (21.9) | 724 (16.6) | <0.001 |
| Texarkana | 1,409 (6.7) | 1,042 (6.2) | 367 (8.4) | <0.001 |
| East Texas | 1,137 (5.4) | 900 (5.4) | 237 (5.4) | 0.81 |
| Houston-Galveston | 4,629 (21.9) | 3,789 (22.5) | 840 (19.2) | <0.001 |
| Central Texas | 1,896 (9.0) | 1,365 (8.1) | 531 (12.2) | <0.001 |
| Southwest | 2,427 (11.5) | 1,937 (11.5) | 490 (11.2) | 0.63 |
| West Central | 623 (2.9) | 469 (2.8) | 154 (3.5) | 0.009 |
| West Texas | 501 (2.4) | 397 (2.4) | 104 (2.4) | 0.92 |
| Rio Grande Valley | 2,805 (13.2) | 2,179 (13.0) | 626 (14.3) | 0.01 |
| Payer, primary or secondary | ||||
| Medicare | 14,403 (67.7) | 11,145 (66.0) | 3,258 (74.5) | <0.001 |
| Medicaid | 4,636 (21.8) | 3,164 (18.7) | 1,472 (33.7) | <0.001 |
| Commercial (private) insurance | 4,581 (21.5) | 3,853 (22.8) | 728 (16.6) | <0.001 |
| HMO/PPO | 3,182 (15.0) | 2,750 (16.3) | 432 (9.9) | <0.001 |
| Liability or indemnity | 1,243 (5.8) | 1,083 (6.4) | 160 (3.7) | <0.001 |
| Other insurance | 1,188 (5.6) | 1,018 (6.0) | 170 (3.9) | <0.001 |
| Charity or uninsured | 1,406 (6.6) | 1,047 (6.2) | 359 (8.2) | <0.001 |
| Admission source | ||||
| E.R. or other urgent admission | 8,591 (40.4) | 6,240 (36.9) | 2,351 (53.7) | <0.001 |
| Skilled nursing facility | 273 (1.3) | 202 (1.2) | 71 (1.6) | 0.03 |
| Other non-urgent admission | 12,497 (58.8) | 10,513 (62.2) | 1,984 (45.4) | <0.001 |
| Teaching hospital designation | 2,688 (12.6) | 2,127 (12.6) | 561 (12.8) | 0.68 |
Figure 2:
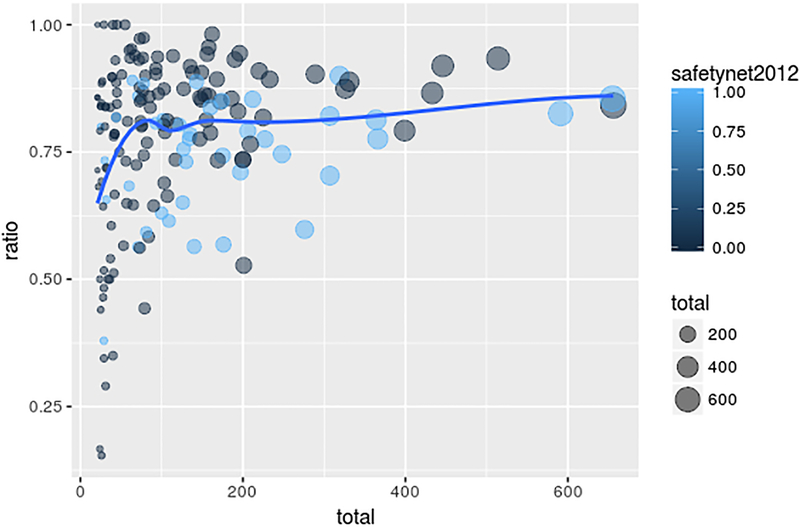
The relationship between hospital volume and revascularizations as a proportion of total procedures (revascularizations + leg amputations) in Texas hospitals, 2004–2009 (p<0.001, R2=0.18).
Distribution of Procedures Across Hospitals in Texas
A total of 349 hospitals in Texas performed either revascularization or leg amputation procedures for Texans with PAD and foot complications from 2004 through 2009. Approximately one quarter of these procedures were performed at just 11 hospitals (3.2% of all hospitals in Texas performing these procedures; hereafter referred to as “very high volume hospitals”), and another quarter of these procedures were performed in another 25 hospitals (7.1% of all hospitals in Texas performing these procedures; hereafter referred to as “high volume hospitals”). The total number of procedures ranged from 326 to 656 (average of 54–109 per year) for hospitals in the very high volume group and 172 to 319 (average of 29–53 per year) for hospitals in the high volume group. Most hospitals (271, or 77.7% of hospitals performing revascularization or leg amputation procedures) performed no more than 90 total procedures (average of no more than 15 per year) during the study period (hereafter referred to as “low volume hospitals”; see Table 2). Of these, 72 (21%) of Texas hospitals performing major procedures for patients with PAD and performed no revascularizations for patients with PAD and foot pathology during the six year study period. Whereas none of the very high volume hospitals had a revascularization proportion of less than 65%, 10–12% of high and medium volume hospitals and more than half (54%) of low volume hospitals had revascularization proportions of less than 65% (Table 2). A significant relationship was seen between procedure volume and ratio of revascularization procedures to primary leg amputations (p<0.001, R2=0.18; see Figure 1). Significantly more people categorized as black underwent major procedures in low volume hospitals than people in other racial or ethnic categories (31.6 vs. 25.4%, p<0.001).
Table 2:
Categorization of Texas hospitals by total volume of revascularization and leg amputation procedures, 2004 through 2009.
| hospital group | number of hospitals (% of total) | total number of procedures | range of total volume per hospital, 2004–2009 | number (%) of hospitals with revascularization proportion <0.65 |
|---|---|---|---|---|
| very high volume | 11 (3.2) | 5,081 | 326–656 | 0 (0) |
| high volume | 25 (7.2) | 5,539 | 172–319 | 3 (12.0) |
| moderate volume | 42 (12.0) | 5,494 | 93–169 | 4 (9.5) |
| low volume | 271 (77.7) | 5,448 | ≤90 | 146 (53.9) |
Figure 1:
Heat map showing the location and density of leg amputations performed in Texas for PAD and foot complications, 2004 through 2009.
Factors Associated with Primary Leg Amputations among Texans with PAD
A multivariate logistic model identified 22 factors that were significantly associated with primary leg amputations for people with PAD and foot complications (Table 3). The overall model c-statistic was 0.79. Primary leg amputations were more frequent among foot osteomyelitis or other foot infection, among people with high medical risk, among men, and among those greater than 75 years of age. Admission through the emergency department (or other source categorized as urgent) was more frequently associated with leg amputation (p<0.001 for all; Table 3).
Table 3:
Dependent variables significantly associated with primary leg amputations (i.e. no preceding revascularization) among people with PAD and foot complications treated at Texas hospitals 2004–2009.
| Variable | Odds Ratio | 95% Confidence Interval | z | P-value |
|---|---|---|---|---|
| Clinical Characteristics of Foot Pathology | ||||
| foot osteomyelitis | 2.06 | (1.80, 2.35) | 10.47 | <0.001 |
| foot infection | 4.63 | (4.24, 5.06) | 33.69 | <0.001 |
| Age, Sex, Poverty, Race and Ethnicity | ||||
| >75 years of age | 1.55 | (1.43, 1.69) | 10.44 | <0.001 |
| male | 1.30 | (1.20, 1.40) | 6.38 | <0.001 |
| categorized as black | 1.79 | (1.61, 1.99) | 10.73 | <0.001 |
| categorized as Hispanic | 1.42 | (1.28, 1.57) | 6.83 | <0.001 |
| categorized as Native American | 0.43 | (0.26, 0.73) | −3.12 | 0.002 |
| Poverty | ||||
| at least 12% of population in zip code of residence living below the federal poverty level | 1.14 | (1.05, 1.24) | 3.14 | 0.002 |
| Primary or Secondary Payer | ||||
| Medicaid | 1.89 | (1.72, 2.07) | 13.81 | <0.001 |
| Medicare | 1.14 | (1.04, 1.26) | 2.74 | 0.006 |
| uninsured or charity | 1.70 | (1.45, 1.98) | 6.69 | <0.001 |
| Hospital Admission Source | ||||
| admission through emergency department or other urgent admission | 1.39 | (1.29, 1.51) | 8.10 | <0.001 |
| Geography and Other Hospital Characteristics | ||||
| low volume hospital | 1.78 | (1.63, 1.93) | 13.6 | <0.001 |
| teaching hospital designation | 1.15 | (1.01, 1.32) | 2.04 | 0.04 |
| Texas Public Health Region | ||||
| Central Texas | 1.79 | (1.58, 2.04) | 8.86 | <0.001 |
| West Central | 1.78 | (1.43, 2.22) | 5.16 | <0.001 |
| Texarkana | 2.19 | (1.89, 2.54) | 10.3 | <0.001 |
| South Plains | 2.48 | (2.01, 3.07) | 8.35 | <0.001 |
Factors not shown: medical comorbidity index; medical risk index; calendar year.
Even after extensive risk adjustment (including accounting for medical risk, gender and age, region, insurance carrier, and hospital volume), persons categorized as black or Hispanic underwent leg amputation much more frequently than people in other categories (odds ratios 1.79 and 1.42, respectively; p<0.001). Those categorized as Native American less frequently underwent leg amputation (odds ratio 0.43, p=0.002). Persons living in areas with higher rates of poverty (specifically, zip codes with 12% or more of residents living at or below the federal poverty limit) more frequently underwent leg amputation (p=0.002). People with Medicaid or Medicare as their primary or secondary payer and persons who were uninsured also had higher risk-adjusted rates of leg amputations.
Certain geographic and hospital characteristics were also associated with leg amputations. People treated at low volume hospitals – i.e., those performing an average of 15 or fewer total revascularization and leg amputation procedures per year – had significantly higher risk-adjusted amputation rates (odds ratio 1.78, p<0.001). Teaching designation was associated with a slightly-elevated leg amputation rate. Significantly-elevated leg amputation rates were noted in four Texas Public Health Regions: West Central Texas (including Odessa and San Angelo), Central Texas (including Temple), Texarkana (including Tyler), and the South Plains (including Abilene and Wichita Falls). A zip code-level analysis produced a ranking of zip codes of residence by leg amputation incidence. The 100 zip codes with the highest incidence rates are shown in Figure 3 and are listed in Supplemental Table C.
The risk-adjusted probability of leg amputation decreased significantly over time. Compared to 2004–2005, the odds ratio for people treated in calendar years 2006, 2007, 2008 and 2009 were 0.79, 0.72, 0.65, and 0.63, respectively (p<0.001 for all).
Discussion
Disparities in the rates of leg amputations have been documented for at least two decades1–11, yet no efforts to address these disparities have been reported in the United States. There are many reasons why previous publications have not led to efforts to address these disparities, and among them may be the possibility that more specific regional or local data is needed to inform efforts. With this in mind we undertook an analysis of Texas inpatient data with the intent of identifying geographic areas that could benefit from prevention efforts designed to reduce leg amputations among at-risk people with PAD.
Our study has several very actionable findings. First, the analysis has identified some very specific geographic areas where people at risk for leg amputation live. Specifically, the individual-level, risk-adjusted analysis demonstrated that persons in four geographic regions (Central Texas, West Central Texas, Texarkana, and the South Plains) have significantly-higher rates of amputation that people residing in other areas of Texas. A zip code-level analysis provided a rank list of even smaller areas based on leg amputation incidence. Directing prevention efforts to individuals in these specific areas should be the priority of anyone hoping to reduce leg amputation rates in Texas.
Second, even after accounting for other patient-level characteristics, leg amputations occurred much more frequently in low volume hospitals (i.e. those that performed an average of less than 15 major procedures [leg bypass operations, endovascular interventions for the leg, or leg amputations). Indeed, more than one in five hospitals performing major procedures for this patient population did not report having performed any revascularization procedures during this six year span. The choice of hospital is heavily influenced by geography, with people most often choosing a hospital close to home. These findings suggest, however, that patients at risk for leg amputation may benefit from being treated at a moderate, high or very high volume hospitals.
Third, disparately-high rates of leg amputations are still seen among Texans categorized as black or Hispanic. Though the exact reasons for these mechanisms is not clear, it should be acknowledged that differential access to health care providers (primary care providers, specialist, and allied health care providers alike) and differential rates of diagnostic testing and treatments (as has been documented in the case of stroke15 and due to either unrecognized or explicit bias on the part of providers) are very likely to contribute. One strategy to eliminate disparities might be to address these underlying cause, and another would be to employ actions to offset these disadvantages. Examples of the latter might include providing access to educational materials, opportunities for free screening, or biannual foot exams to at-risk individuals.
Our analysis has many limitations. We do not have data more recent than calendar year 2009, although there have been no policy or regulatory changes to suggest improvement. We relied on diagnosis codes and, therefore, were unable to quantify the severity or anatomic location of foot infection or PAD. We do not have information on baseline functional status, and we therefore could not adjust for the small but potentially-significant number of amputations that are performed in non-ambulatory patients, a situation generally recognized as a valid indication for leg amputation.16 Finally, although it is possible that some patients who underwent leg amputation had previously undergone revascularization, the higher rate of amputation among those categorized as black – even if revascularization had been performed – would be disturbing..
Supplementary Material
Abbreviations
- PAD
peripheral artery disease
Footnotes
Potential conflicts of interest: none.
References
- 1.Guadagnoli E, Ayanian JZ, Gibbons G, McNeil BJ, LoGerfo FW. The influence of race on the use of surgical procedures for treatment of peripheral vascular disease of the lower extremities. Arch Surg Chic Ill 1960. 1995. April;130(4):381–6. [DOI] [PubMed] [Google Scholar]
- 2.Lavery LA, van Houtum WH, Ashry HR, Armstrong DG, Pugh JA. Diabetes-related lower-extremity amputations disproportionately affect Blacks and Mexican Americans. South Med J. 1999. June;92(6):593–9. [DOI] [PubMed] [Google Scholar]
- 3.Mueller KJ, Patil K, Boilesen E. The role of uninsurance and race in healthcare utilization by rural minorities. Health Serv Res. 1998. August;33(3 Pt 1):597–610. [PMC free article] [PubMed] [Google Scholar]
- 4.Eslami MH, Zayaruzny M, Fitzgerald GA. The adverse effects of race, insurance status, and low income on the rate of amputation in patients presenting with lower extremity ischemia. J Vasc Surg. 2007. January;45(1):55–9. [DOI] [PubMed] [Google Scholar]
- 5.Regenbogen SE, Gawande AA, Lipsitz SR, Greenberg CC, Jha AK. Do differences in hospital and surgeon quality explain racial disparities in lower-extremity vascular amputations? Ann Surg. 2009. September;250(3):424–31. [DOI] [PubMed] [Google Scholar]
- 6.Lefebvre KM, Lavery LA. Disparities in amputations in minorities. Clin Orthop. 2011. July;469(7):1941–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holman KH, Henke PK, Dimick JB, Birkmeyer JD. Racial disparities in the use of revascularization before leg amputation in Medicare patients. J Vasc Surg. 2011. August;54(2):420–426, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henry AJ, Hevelone ND, Belkin M, Nguyen LL. Socioeconomic and hospital-related predictors of amputation for critical limb ischemia. J Vasc Surg Off Publ Soc Vasc Surg Int Soc Cardiovasc Surg North Am Chapter. 2011. February;53(2):330–339.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durazzo TS, Frencher S, Gusberg R. Influence of race on the management of lower extremity ischemia: revascularization vs amputation. JAMA Surg. 2013. July;148(7):617–23. [DOI] [PubMed] [Google Scholar]
- 10.Hughes K, Boyd C, Oyetunji T, Tran D, Chang D, Rose D, et al. Racial/ethnic disparities in revascularization for limb salvage: an analysis of the National Surgical Quality Improvement Program database. Vasc Endovascular Surg. 2014. August;48(5–6):402–5. [DOI] [PubMed] [Google Scholar]
- 11.Lefebvre KM, Chevan J. The persistence of gender and racial disparities in vascular lower extremity amputation: an examination of HCUP-NIS data (2002–2011). Vasc Med Lond Engl. 2015. February;20(1):51–9. [DOI] [PubMed] [Google Scholar]
- 12.Margolis DJ, Hoffstad O, Nafash J, Leonard CE, Freeman CP, Hennessy S, et al. Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care. 2011. November;34(11):2363–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barshes NR, Sigireddi M, Wrobel JS, Mahankali A, Robbins JM, Kougias P, et al. The system of care for the diabetic foot: objectives, outcomes, and opportunities. Diabet Foot Ankle. 2013;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50(6):813–828. [DOI] [PubMed] [Google Scholar]
- 15.Hsia DC, Moscoe LM, Krushat WM. Epidemiology of carotid endarterectomy among Medicare beneficiaries: 1985–1996 update. Stroke. 1998. February;29(2):346–50. [DOI] [PubMed] [Google Scholar]
- 16.Barshes NR, Belkin M. Deciding Between Major Amputation and Attempts at Limb Salvage In: Contemporary Vascular Surgery. Shelton, Connecticut: People’s Medial Publishing House USA, Ltd; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.