Abstract
This study used data from six neuropsychological measures of executive function (EF) and general intellectual functioning (GIF) administered to 303 regular users of heroin and/or cocaine as indicators in a latent profile analysis (LPA). Results indicated the presence of three profiles: impaired GIF and EF profile (30.8%), intact GIF and EF profile (58.8%), and high GIF/intact EF profile (10.4%). Using a multinomial logistic regression, it was determined that individuals who reported being diagnosed with either a learning disability (LD) and/or attention-deficit/hyperactivity disorder (ADHD) were more likely to be in the impaired GIF and EF profile than other profiles. Results from a logistic regression indicated that the impaired GIF and EF profile was associated with a greater prevalence of past hepatitis B and/or C infection. Implication for harm reduction and treatment programs and the need to take into account individuals with LD and ADHD are discussed.
Keywords: adults, neuropsychology, at risk/prevention
Substance use disorders (SUDs) are a significant public health problem due to the societal and economic costs and their association with poor health outcomes. Estimated costs related to the use of illegal drugs in 2002 exceeded $180 billion. This figure included estimates of lost productivity and poor health outcomes (Office of National Drug Control, 2004) such as sexually transmitted infections. Infectious diseases such as viral hepatitis B and C have a particular high association with the use of heroin and cocaine. For example, McCoy and colleagues (McCoy, Lai, Metsch, Messiah, & Zhao, 2004) reported seroprevalance rates for HIV greater than 20% in a community sample of injection and noninjection drug users of heroin and crack cocaine. Another study concluded that young users of heroin and/or cocaine are at increased risk for hepatitis B infection (Kuo, Sherman, Thomas, & Strathdee, 2004). Existing research has also demonstrated that injection drug users in Baltimore that have injected for 6 years or less had prevalence estimates around and above 50% for hepatitis B (HBV) and hepatitis C (HCV) and approximately 15% for HIV (Garfein, Vlahov, Galai, Doherty, & Nelson, 1996). In addition to the increased risk for poor health outcomes, heroin and cocaine use has been reported as a problem drug among approximately 30% of individuals entering treatment in 2005 for SUDs (SAMHSA, 2006).
Cognitive Impairment, Developmental Disorders, and Increased Risk of SUDs
Several studies suggest that childhood cognitive impairment as well as a diagnosis with some developmental disorders represent important risk factors for drug use and abuse later in life. Findings indicate that children with poorer performance on neuropsychological measures assessing domains thought to be associated with some developmental diagnoses are at an increased risk for developing substance use disorders (Giancola & Parker, 2001; Najam, Moss, Kirisci, & Tarter, 1997; Tapert, Baratta, Abrantes, & Brown, 2002). Past research also demonstrates that the presence of a diagnosis with certain developmental disorders is associated with SUDs. For example, the association between attention-deficit/hyperactivity disorder (ADHD) and progression of drug use has been demonstrated in longitudinal studies (Biederman, Wilens, Mick, Faraone, & Spencer, 1998). Levin (2007) reviews findings that estimate the prevalence of ADHD at around 5% to 33% for opiate- and cocaine-dependent individuals. Studies indicate that individuals with other learning disorders may be at greater risk for SUDs as well. For example, Cosden (2001) reviews findings suggesting that individuals with a learning disorder are disproportionately represented in substance use treatment programs. Young adults with learning disorders that persist through adolescence were found to be more likely to have an SUD (Beitchman, Wilson, Douglas, Young, & Adlaf, 2001). Furthermore, researchers suggest that despite lower prevalence of use, individuals with mild mental retardation that also use drugs may experience more substance use problems (Westermeyer, Kemp, & Nugent, 1996; Westermeyer, Phaobtong, & Neider, 1988).
Although there is research suggesting an increased risk for an SUD among individuals with certain developmental disorders, there is little research that examines the prevalence of conditions such as learning disabilities or ADHD among adults with SUDs, particularly heroin and cocaine. Even less research is available on the potential increase in the risk of infectious disease with cognitive impairment due to preexisting developmental conditions.
Identifying Cognitive Deficits Among Substance Using Populations
Effectively determining the prevalence of individuals that meet criteria for a learning disability or other developmental disorder among substance users is difficult due to the fact that while some nationally representative surveys such as the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) and the National Comorbidity Survey–Replication (NCS-R) conducted among adults and within the United States do obtain some information on developmental conditions (primarily attention-deficit disorder, ADD, or ADHD), none include a neuropsychological battery often used to aid in the diagnosis of such disorders. The information that is obtained is usually collected through questionnaires or asking whether a participant had been diagnosed with a learning disability in childhood. A brief neuropsychological evaluation can aid in the validation of self-reported diagnoses and in the identification of cases that may not have been identified earlier in life.
Although the use of a neuropsychological battery is helpful, two limitations in using such measures to identify the presence of developmental disorders among substance users are potential confounders and diagnostic limitations. Determining whether impaired performance is the result of a preexisting condition or drug use can be estimated to some extent through adjustment in regression models or restricting the sample to a homogenous group. However, making effective diagnoses and differentiating between developmental conditions using neuropsychological measures is limited. A review of previous research indicates that individuals with learning disabilities, ADHD, and other developmental disorders may show similar impairments in tasks assessing abilities often referred to as “executive functions.” According to the definition used by Harris (1998), executive functions include the ability to make decisions, sustain attention, avoid distractions, and be flexible in thinking and planning. Performance on working memory tasks, many of which require both the ability to ignore distracting information as well as sustain attention, is shown to be impaired among individuals with learning disabilities, ADHD, and other developmental disorders (Numminen et al., 2000; Roth & Saykin, 2004; Seidman, 2006; Swanson & Sachse-Lee, 2001). Measures where individuals identify patterns and avoid repetitive errors, thought to assess concept formation and/or cognitive flexibility, are theoretically linked to ADD or ADHD (Roth & Saykin, 2004; Seidman, 2006). However, studies suggest that children with learning disorders also show impairments on measures of executive functioning (e.g., Obrzut, Hynd, & Obrzut, 1983). The ability to inhibit responses is a key theoretical construct in the detection of attention problems related to ADHD; but impaired inhibition may also contribute to the difficulties evidenced in learning disabilities (Denckla, 1996; Lazar & Frank, 1998). Furthermore, measures of impulsivity and intellectual functioning are highly correlated, suggesting that individuals with borderline or impaired intellectual abilities may display poor performance through this association (Greenberg, Kindschi, & Corman, 1999). Finally, Numminen and colleagues (2000) found that performance on a measure assessing planning ability was lower among children with learning and intellectual deficits. However, other studies demonstrate that ADHD is associated with poorer performance on a planning measure as well (Culbertson & Zillmer, 2001). In summary, previous findings indicate that a short battery of neuropsychological measures alone may be useful in identifying the presence of a developmental disorder but limited in the ability to differentiate between the diagnoses without the aid of a clinical interview in addition to medical and educational histories.
Cognitive Impairment, Developmental Disorders, and Health Outcomes
Findings in the field of substance use suggest that those with poorer performance on measures of cognitive function have poorer health outcomes. Much of the research in this area has examined how impairment on neuropsychological measures is associated with poorer treatment response. Findings in this area indicate that impairment on neuropsychological measures is associated with shorter stays in treatment and poorer treatment responses across different treatment modalities (Moeller et al., 2001; Paraherakis, Charney, & Gill, 2001).
While there is evidence of a disparity in treatment outcomes among individuals with cognitive impairments and SUDs, there is less research in the area of infectious disease and HIV risk behaviors. A growing field of research examines how poor performance on cognitive measures is associated with risk behaviors and the prevalence of infectious disease among substance users (Mitchell, Severtson, & Latimer, 2007; Severtson & Latimer, 2006; Severtson, Mitchell, Mancha, & Latimer, in press). However, little attention has focused on identifying cognitive impairments that might be associated with developmental disorders among substance users. Even less examines how these impairments relate to the spread of infectious diseases associated with heroin, cocaine, and injection drug use. Recent studies suggest that individuals who perform in the impaired range on a planning measure are more likely to share drug use equipment the more frequently they inject drugs. This association was not observed among those with intact performance on this measure (Severtson et al., in press). Another study indicated an inverse association between estimated premorbid intellectual ability and hepatitis C prevalence among injection drug users (Severtson & Latimer, 2006). Such findings suggest the potential for an association between impaired cognitive functions and infectious disease among substance users.
The Current Study
To address gaps in previous research, we sought to test two principle hypotheses. The first is to identify a pattern of performance on neuropsychological measures that is associated with self-reported diagnosis of ADHD, ADD, or another type of learning disability. Much of the research on cognition among adult substance-using populations has focused on the relationship between use of particular drugs and resulting cognitive decline and/or impairment in particular domains (e.g., Bolla, Funderburk, & Cadet, 2000; Verdejo-Garcia, Lopez-Torrecillas, Gimenez, & Perez-Garcia, 2004; Vik, Cellucci, Jarchow, & Hedt, 2004). After adjusting for this well-researched association, we hypothesize that there will be an assocation between self-reported learning disability and/or ADHD and impaired cogntive performance on neuropsychological measures. The next step is to examine the association between patterns of performance on neuropsychological measures and prevalence of hepatitis B and/or C. We hypothesized that those who exhibit the pattern of performance associated with developmental disorders would be more likely to test positive for HBV and/or HCV after adjusting for potential confounders.
Method
The current study utilized baseline data from the NEURO-HIV Epidemiologic Study, a longitudinal epidemiological investigation funded by the National Institute on Drug Abuse (NIDA) designed to evaluate neuropsychological and social-behavioral risk factors of contracting HIV, hepatitis A, hepatitis B, and hepatitis C among injection and noninjection drug users. Study participants were recruited using a variety of community-based outreach strategies, including street recruitment, referrals, and advertisements in local newspapers. Upon arrival, participants were given detailed information about the study and informed consent was obtained. Participants received a monetary incentive ($45) for completion of the baseline assessment. The project was approved and monitored by the Institutional Review Board at the Johns Hopkins Bloomberg School of Public Health. More detailed descriptions of the data set are available in previous publications (e.g., Mitchell et al., 2007).
The present study sample is based on 303 HIV negative drug users who reported current or lifetime regular use of heroin, cocaine, and/or crack cocaine with regular use defined as daily or nearly daily use for 3 months or more. Participants from the total baseline study sample were excluded from the first two analyses if they are older than the age of 45 and if they tested positive for HIV as both could potentially confound the association between premorbid disorder and neuropsychological test performance. Participants were also excluded if they exceeded 120 omission errors on the Test of Variable of Attention as excessive omission errors are thought to be related to insufficient effort and were determined to be excessive within this sample (Greenberg et al., 1999). In addition, 28 participants with missing information on lab results were excluded from the analysis.
Measures
HIV-Risk Behavior Interview.
The HIV-Risk Behavior Interview included questions about sociodemographics; medical, educational, and neuro-developmental histories; and detailed behavioral information about drug use and sexual practices. The interview obtained data on illicit drug use (injection and noninjection), sexual activity (steady, casual, sex-trade partners), and clinical symptoms related to HIV infection and other STIs. The baseline assessment evaluated each participant’s history of drug use, including drug type, route of administration, frequency of administration, and quantity used per administration for a number of time periods. The drug use section began by detailing all of the drugs used by participants in their lifetime. Next, a record was taken for each drug used in the participants’ lifetime in terms of their use of each drug by route of administration, frequency, and quantity during the 24 hours, week, month, and 6 months preceding the assessment. Similarly detailed information was gathered about participants’ sexual risk behavior, including information on the frequency of condom use, engaging in sexual exchange, and number of casual partners. This information was collected for the previous day, week, month, and 6 months. In addition to risk behavior and drug use information, the interview obtained information on treatment readiness, recent treatment participation, and knowledge and perceived risk of HIV and other infectious diseases. The primary variables to be utilized from the interview include the following.
Developmental disorders.
Participants were asked in two separate questions if they had ever been told that they had a learning disability or ADD/ADHD. Given the high comorbidity between the disorders, and the difficulty in detecting nuanced differences with this sample, we chose to use one variable in the analyses, self-reported diagnosis of ADHD/ADD and/or learning disability.
Potential confounders.
As previously reviewed, literature suggests that substance use has been to shown to lead to cognitive impairments. For this reason, we included years of regular use as a covariate in predicting profile membership. We also included recent cocaine use as a covariate to determine whether there was a difference in the effects of acute use and cognitive impairment by substance.
In examining infectious disease prevalence, we included two high-risk behaviors, history of participation in sexual exchange (buying or selling sex with either money or drugs) and history of injection drug use.
Neuropsychological measures.
The neuropsychological battery of the study included validated and well-known measures of cognitive function. For this analysis, we used raw scores from select measures and obtained values adjusted for gender, education, ethnicity, and age using standardized residuals from linear regressions. The following neuropsychological measures from the study battery were included as part of this study.
The Wisconsin Card Sorting Test (WCST; Heaton, Chelune, Talley, Kay, & Curtiss, 1993) was included as a measure of abstraction and problem solving. Performance may also be affected by memory and attention abilities as well. The WCST is a computerized task where participants are asked to match cards in a deck to one of four primary cards. There are three variables in which the participant can match cards and each participant must go through each variable twice. Therefore, the test is finished after the participant completes six categories or after the participant goes through all 128 cards. The Wisconsin Card Sort provides several measures but categories completed and perseverative errors (PE) are most commonly used in identifying impairment (Lezak, 2004). For this analysis, we used perseverative errors. This is calculated by summing the number of errors the participant made by matching on an incorrect category after having been informed once that the category is incorrect.
The Test of Variable of Attention (TOVA; Greenberg et al., 1999) was included as a measure of attention. For the TOVA, participants are asked to press a clicker when a hole appears at the bottom of a square. Participants are asked not to press the button when incorrect stimuli appear. Several measures are provided by the test, including commission errors, omission errors, and response time (RT). For the current analysis, response time was used as it represents an estimation of reaction speed.
The Shipley Institute of Living Scale (SILS; Zachary, 1991) is comprised of two components and is thought to estimate intellectual functioning. The first section is a vocabulary test with a list of 40 target words. Next to each of the target words are 4 other words. Participants are asked to circle the one word among the 4 words that is the synonym of the target word. The score is computed by summing up the number of correct items. For each skipped item, participants receive a fourth of a point. The second component of the SILS is the Abstraction section. Here participants are asked to complete 20 word problems. Each correct answer receives two points and the score is summed up. The original focus of the SILS was to investigate cognitive impairment based on the discrepancy between the Abstraction and Vocabulary sections, though as pointed out by Lezak (2004), the utility of this approach has not received consistent support. An age-adjusted total score has been used as a rough estimate of premorbid IQ in drug-using samples (Bolla et al., 2000); therefore, the current study utilized the sum of both components.
The Tower of London (TOL; Culbertson & Zillmer, 2001) has two sets of boards with three pegs and each board has three colored balls (red, blue, and green) and is thought to assess planning abilities. The examiner arranges the balls on the pegs in a specific pattern and participants are asked to move the balls to match the pattern presented by the examiner. Participants are asked to complete each trial in the minimum number of moves. In the version used in this analysis, each participant completed the same 10 trials. Of the 10 trials, there are 2 trials that could be completed in four moves, 3 trials that could be completed in five moves, 3 trials that could be completed in six moves, and 2 that could be completed in seven moves. Each trial solved in the minimal number of moves would be considered a correct item. In addition to counting moves, times were recorded from the moment the participant was presented with the pattern to the moment the participant initiated the first move and from the time of the first move to the time the problem was completed up to 2 minutes, at which point the trial was discontinued. For the current analysis, performance was based on the total move score, which is computed by summing the number of moves in excess of the minimum number of moves the item could be completed.
The Digit Span subtest of the Wechsler Adult Intelligence Scale, Third Edition (WAIS-III; Wechsler, 1997) is a measure of simple attention and working memory. In the “Forward” portion of the task, participants are read a series of single-digit numbers with an approximately 1-second gap between each digit. After the examiner reads the series of digits, participants are asked to repeat them. The test gets increasingly more difficult by adding one additional digit to individual items. Each trial contains two items. The test ends when the participant fails to correctly repeat two items within one trial. The participant is next administered the “Backward” portion of the test. This portion of the test is similar except that the participants are to repeat the numbers in backward order. The age-corrected total score of the task loads onto the Working Memory component of the WAIS-III. The current study used the sum of the raw scores from both sections.
The Stroop Color-Word Task (Golden & Freshwater, 2002) is given in three sections and is thought to assess divided attention. The first section includes the word portion where participants are asked to read as many words in 45 seconds as they can. The words are Red, Green, and Blue. In the next section of the test, participants are presented with four Xs in three different colors and are asked to name as many colors as they can in 45 seconds. In the final section of the test, participants are presented with the three color words in different color font and are asked to name the color of the word, ignoring the word itself. The Stroop is thought to assess inhibition and cognitive flexibility. Performance is traditionally based on the interference score, which is computed by subtracting the total colors correctly named on the color-word portion by an expected value computed using the first two portions of the test. This study utilized the number of words read in the color-word section as it provides an unstandardized raw score similar to the items from other measures used in this analysis.
Laboratory data.
Participants provided blood samples as part of their participation. Each participant was tested for the presence of HIV and hepatitis A, B, and C. Hepatitis B results included the antibody to the hepatitis B core antigen (HBcAb), antibody to the hepatitis B surface antigen (HBsAb), and the hepatitis B surface antigen (HBsAg). We used positive or negative results on the HBcAb test, which has been used in previous studies as an indication of past infection or current infection (Kuo et al., 2004) of hepatitis B. In addition, we used results from the blood test for hepatitis C.
Statistical Analysis
The first step of the analysis explored the distributions of the neuropsychological measures. Previous research using data obtained from the NEURO-HIV Epidemiologic Study indicates that many measures do not follow a Gaussian distribution, as is common with certain neuropsychological measures. Therefore, appropriate transformations were made to approximate normal distributions. Following these transformations, linear regression analyses were run with each test variable as an outcome. The measures were regressed on age, gender, ethnicity, and education. The standardized residuals were then computed for each participant. This strategy was employed because, as Lezak (2004) discusses, demographic variables are associated with performance on neuropsychological tasks and failure to consider such variations can lead to inaccurate assessments of impairment. Therefore, test results represent scores standardized to a mean of 0 and a standard deviation of 1 that are adjusted for the age, gender, ethnicity, and education of the participants.
In the second stage of the analysis, a latent profile analysis was fit using each neuropsychological measure as an indicator variable. Latent profile analysis is similar to latent class analysis in that it assumes the existence of an underlying categorical latent variable but uses continuous rather than categorical indicators (Gibson, 1959). The primary assumption of a latent profile model is that of conditional independence; meaning that the correlation between measures is only a product of the latent variable and no within-profile correlation exists between indicator variables. These assumptions were checked. We chose to examine both information criteria and likelihood ratio tests in determining the best fitting model. Emphasis would be placed on the Bayesian Information Criteria (BIC) and the bootstrap likelihood ratio test (BLRT) as recommended by previous research by Nylund, Asparouhov, and Muthen (2007) in determining the appropriate number of classes. We also used Akaike’s Information Criteria (AIC) and the Lo-Mendall-Rubin test (LMR) in determining the best model, two methods also reviewed in detail by Nylund and colleagues. The latent profile approach was selected because it allows for the identification of a categorical latent variable representing patterns of performance. This allows a “typing” of a participant as opposed to factor analysis approaches, which identifies dimensional traits within an individual.
Once the number of profiles (or classes) was identified, a multinomial regression model was run with the profiles as the outcome to determine whether self-reported learning disability or ADHD predicts profile membership independent of years of use, acute use of cocaine, age, and other demographic variables. The primary assumption of this model is one of nondifferential measurement, meaning that covariates should not be associated with indicators within profiles. From this analysis, it was anticipated that self-reported learning disability, ADD, or ADHD would be associated with profiles indicative of poorer performance on neuropsychological measures independent of acute and chronic drug use. Because we did not have the power to detect nuanced differences in neuropsychological performance between disorders, we chose to assess self-reported diagnosis with either disorder versus no self-reported diagnosis.
After the regression of profile membership on self-reported diagnosis and covariates, the final stage of the analysis involved examining the association between profile membership and infection with either hepatitis B or hepatitis C after adjusting for relevant covariates. From this analysis, we anticipated that the pattern of performance on neuropsychological measures most associated with self-reported history of a learning disability and/or ADD/ADHD would be associated with greater prevalence of past HBV and/or HCV infection.
Both the multinomial and logistic regression analyses required accounting for the classification error. Latent profile analysis, like latent class analysis, provides an estimate of the probability of class membership for each participant. However, there is error in the classification of individuals, the amount to which is reflected in the overall entropy score. For example, based on a pattern of performance an individual may be most likely to belong to Profile (or class) 1 in a three-class model, yet there is some probability that he or she belongs to Profile 2 and possibly Profile 3. Using the most probable membership without taking into account this error can lead to erroneous inferences through underestimating assignment error. To correct for the problem, we used a method modeled after the work of Wang and fellow researchers (Wang, Hendricks Brown, & Bandeen-Roche, 2005), which involved generating several data sets based on profile (or class) probabilities. We simulated 20 data sets based on the probability of membership in each profile. Profiles were assigned based on a random value drawn from a multinomial distribution. We set the seed using a random integer generator. We then combined the estimates using the “micombine” command as part of the ICE addition to Stata 10, which combines results using Rubin’s rules (Rubin, 1987). This approach accounted for the error in class assignment and allowed for a more accurate assessment of the association between latent profiles and the hypothesized predictors and outcomes in both models.
Results
Demographic characteristics are presented in Table 1. Approximately 64% of the participants were male, 55% were White, 48% completed less than 12 years of education, and the mean age was just over 30 years old. Results also suggest that 78% of participants had a history of injection drug use and nearly a third of participants had either bought or sold sex for money or drugs.
Table 1.
Sample Characteristics (n = 303)
| Variable | N or M | % or SD |
|---|---|---|
| Gender | ||
| Male | 195 | 64.4 |
| Female | 108 | 35.6 |
| Ethnicity | ||
| White | 168 | 55.5 |
| African American or other | 135 | 44.6 |
| Years of education | ||
| 12 or more | 157 | 51.8 |
| Less than 12 or GED | 146 | 48.2 |
| History of injection drug use | ||
| Yes | 237 | 78.2 |
| No | 66 | 21.8 |
| Learning disability | ||
| Yes | 41 | 13.5 |
| No | 262 | 86.5 |
| ADD/ADHD | ||
| Yes | 44 | 14.5 |
| No | 259 | 85.5 |
| Participation in sex exchange | ||
| Yes | 95 | 31.4 |
| No | 208 | 68.6 |
| Recent cocaine use | ||
| Yes | 188 | 62.1 |
| No | 115 | 37.9 |
| Hepatitis C | ||
| Yes | 165 | 54.5 |
| No | 138 | 45.5 |
| Hepatitis Ba | ||
| Yes | 134 | 45.3 |
| No | 162 | 54.7 |
| Age | 31.54 | 6.47 |
| Years of regular use | 9.55 | 5.94 |
| Digit Span total | 15.47 | 3.68 |
| Tower of London move score | 39.80 | 17.70 |
| TOVA response time | 407.43 | 79.72 |
| SILS, total | 44.74 | 13.40 |
| WCST perseverative errors | 17.53 | 14.13 |
| Stroop Color-Word | 38.71 | 10.06 |
Note: ADD/ADHD = attention-deficit disorder/attention-deficit/hyperactivity disorder; TOVA = Test of Variable of Attention; SILS = Shipley Institute of Living Scale; WCST = Wisconsin Card Sorting Test.
Hepatitis B represents core antigen test results.
Latent Profile Analysis
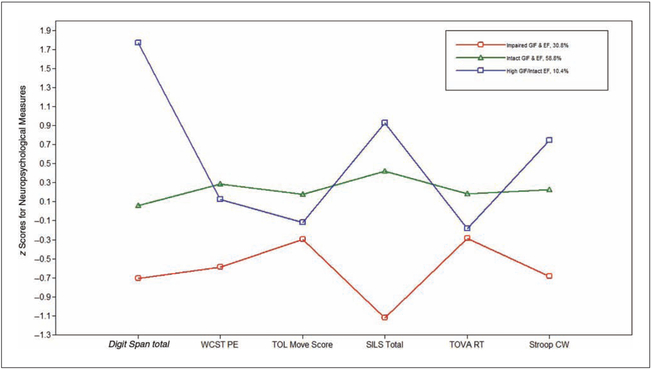
Using standardized residuals as described previously, each measure was set to a mean of zero and a standard deviation of one (z scores). Fit indices form the separate latent profile analyses are presented in Table 2. Based on the fit indices the three-profile model appeared to be a better fit for the data. In addition, this model appeared theoretically correct and useful given the relatively small sample size. The remaining analysis used the three-profile model. The standardized means of the neuropsychological measures within profiles for the final model are presented in Figure 1. Based on the pattern of performance we labeled Profile 1 the impaired general intellectual functioning (GIF) and executive function (EF) profile because performance on most measures was about half a standard deviation below demographically adjusted means for this sample. Profile 2 was labeled intact GIF and EF as most test scores were near the adjusted mean of the sample. Profile 3 was labeled high GIF/intact EF as most of the performances were only slightly below the adjusted mean of the sample with the exception of Digit Span and the SILS. The label also seemed appropriate because both of these neuropsychological measures are used to assess intellectual functioning. From the performance patterns, it appears that three tests, particularly the SILS, Stroop Color Word Test, and Digit Span, are useful in distinguishing between all profiles. The Tower of London Move Score, WCST, and TOVA RT appear to be most effective in distinguishing between two profiles, but less effective in distinguishing between all groups.
Table 2.
Fit Statistics and Entropy Values from Latent Profile Models
| Two Profiles | Three Profiles | Four Profiles | |
|---|---|---|---|
| AIC | 5,008.72 | 4,982.17 | 4,982.98 |
| BIC | 5,079.28 | 5,078.72 | 5,105.53 |
| LMR LRT | 183.95 | 39.56 | 12.87 |
| p < .001 | p = .032 | p = .358 | |
| BLRT | 188.55 | 40.55 | 13.19 |
| p < .001 | p < .001 | p = .667 | |
| Entropy | 0.76 | 0.76 | 0.78 |
Note: AIC = Akaike’s Information Criteria; BIC = Bayesian Information Criteria; LMR LRT = Lo-Mendall-Rubin test; results represent the difference in likelihoods and the corresponding p values; BLRT = bootstrap likelihood ratio test.
Figure 1.
Latent profile analysis results.
Note: GIF = general intellectual functioning; EF = executive function; WCST PE = Wisconsin Card Sorting Test perseverative errors; TOL = Tower of London; SILS = Shipley Institute of Living Scale; TOVA RT = Test of Variable of Attention response time; Stroop CW = Stroop Color-Word Test.
Regression of Latent Profile Membership on Developmental Disorder
The next step involved regressing profile membership on self-reported preexisting learning disability and/or ADHD after adjusting for demographic variables and drug use covariates. For this analysis, a multinomial logistic regression was run with the impaired EF and GIF profile as the comparison group. Results are presented in Table 3 and represent the combined estimates across the 20 imputed data sets. Findings indicate that individuals that reported having a learning disability and/or ADHD had about five times the odds of belong to the impaired GIF and EF, adjusted odds ratio (AOR) = 5.23, 95% confidence interval (CI): 2.52, 10.84, than the intact GIF and EF profile. In a comparison of the impaired GIF and EF profile to the high GIF/intact EF profile, individuals with either a learning disability and/or ADHD had five times the odds of being in the impaired profile (AOR = 5.20, 95% CI: 1.54, 17.51) versus the high intellectual functioning profile. No other covariates, most notably recent cocaine use and years of regular heroin and/or cocaine drug use, were statistically significantly associated with neuropsychological performance profile.
Table 3.
Results of Latent Profiles Regressed on Self-Reported Developmental Disorders and Covariates
| Impaired GIF and EF (Comparison Group) |
Intact GIF and EF |
High GIF/ Intact EF |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Impaired GIF and EF Versus Intact GIF and EF |
Impaired GIF and EF Versus High GIF/Intact EF |
|||||||||
| Variable | N | % | N | % | Adjusted Odds Ration |
95% Confidence Interval |
N | % | Adjusted Odds Ration |
95% Confidence Interval |
| Self-reported disorder | ||||||||||
| No SR LD or ADHD | 56 | 59 | 154 | 89 | 1.00 | — | 27 | 85 | 1.00 | — |
| SR LD and/or ADHD | 39 | 41 | 23 | 11 | 5.23** | 2.70, 12.03 | 5 | 15 | 5.20** | 1.54, 17.51 |
| Ethnicity | ||||||||||
| African American or Other | 44 | 47 | 76 | 43 | 1.00 | — | 14 | 45 | 1.00 | — |
| White Ethnicity | 50 | 53 | 101 | 57 | 0.97 | 0.47, 1.99 | 17 | 55 | 1.41 | 0.40, 4.89 |
| Years of regular drug use | ||||||||||
| 4 years or less | 23 | 24 | 37 | 21 | 1.00 | — | 9 | 28 | 1.00 | — |
| More than 4 years | 72 | 76 | 140 | 79 | 0.78 | 0.35, 1.71 | 23 | 72 | 1.39 | 0.43, 4.47 |
| Gender | ||||||||||
| Male | 62 | 65 | 111 | 63 | 1.00 | — | 22 | 71 | 1.00 | — |
| Female | 33 | 35 | 66 | 37 | 0.93 | 0.47, 1.83 | 9 | 29 | 1.52 | 0.54, 4.23 |
| Age | — | — | 1.05 | 0.99, 1.11 | — | 1.06 | 0.96, 1.17 | |||
| Education | ||||||||||
| High school education or more | 46 | 48 | 96 | 54 | 1.00 | — | 16 | 50 | 1.00 | — |
| <High school education | 49 | 52 | 81 | 46 | 1.08 | 0.54, 2.16 | 16 | 50 | 0.82 | 0.28, 2.40 |
| Acute cocaine use | ||||||||||
| No recent cocaine | 41 | 43 | 64 | 36 | 1.00 | — | 11 | 34 | 1.00 | — |
| Recent cocaine | 54 | 57 | 114 | 64 | 0.67 | 0.36, 1.28 | 21 | 66 | 0.61 | 0.23, 1.58 |
Note: N represents mean values across 20 imputations. GIF = general intellectual functioning; EF = executive function; SR LD = self-reported learning disability; ADHD = attention-deficit/hyperactivity disorder.
p < .01.
Regression of Profile Membership on Infectious Disease
The final stage of the analysis involved estimating the association between profile membership and the association with infectious disease. Findings for the logistic regression analyses are presented in Table 4. With regard to the specific hypothesis and using the impaired GIF and EF profile as the referent group, both the high GIF/intact EF profile (AOR = 0.22, 95% CI: 0.07, 0.68) and the intact GIF and EF profile (AOR = 0.48, 95% CI: 0.22, 0.98) were less likely to test positive for hepatitis C and/or hepatitis B after adjusting for demographic characteristics and risk behaviors such as injecting drugs and participating in sexual exchange. By inverting the odds ratios, individuals whose performance was in the impaired range and most associated with self-reported developmental disorders were more likely to have been infected with HCV and/or HBV than individuals in the high GIF and intact EF (AOR = 4.55, 95% CI: 1.47, 14.29) and the intact GIF and EF (AOR = 2.08, 95% CI: 1.02, 4.55). Results from other covariates were in the anticipated direction, with injection drug use (AOR = 4.80, 95% CI: 2.31, 9.98) and less education (AOR = 2.39, 95% CI: 1.35, 4.21) being associated with a statistically significantly greater odds of infection with HBV and/or HCV.
Table 4.
Logistic Regression Results Hepatitis B/C Infection
| Hepatitis Infection |
||||
|---|---|---|---|---|
| Variable | N | % | Adjusted Odds Ration | 95% Confidence Interval |
| Profile | ||||
| Impaired GIF and EF | 95 | 76 | 1.00 | — |
| Intact GIF and EF | 177 | 62 | 0.22** | 0.07, 0.68 |
| High GIF/impaired EF | 31 | 44 | 0.48* | 0.22, 0.98 |
| Age | — | 1.04 | 0.99, 1.09 | |
| Gender | ||||
| Male | 195 | 66 | 1.00 | — |
| Female | 108 | 62 | 0.92 | 0.52, 1.64 |
| Ethnicity | ||||
| African American or Other | 135 | 54 | 1.00 | — |
| White race | 168 | 73 | 1.71 | 0.83, 3.50 |
| Education | ||||
| High school education or more | 157 | 54 | 1.00 | — |
| <High school education | 146 | 76 | 2.39** | 1.35, 4.21 |
| Years of regular drug use | ||||
| 4 or less | 68 | 62 | 1.00 | |
| More than 4 | 235 | 65 | 1.12 | 0.54, 2.29 |
| Acute cocaine use | ||||
| No use | 115 | 59 | 1.00 | — |
| Recent use | 188 | 68 | 1.36 | 0.77, 2.39 |
| Injection drug use (IDU) | ||||
| No IDU | 66 | 30 | 1.00 | — |
| IDU | 237 | 74 | 4.80** | 2.31, 9.98 |
| Participation in sexual exchange (SE) | ||||
| No SE | 204 | 62 | 1.00 | — |
| SE | 95 | 68 | 1.32 | 0.71, 2.46 |
Note: For “Hepatitis Infection,” results represent infection with hepatitis B or C versus no infection. N for profiles represent mean Ns across 20 imputed data sets. GIF = general intellectual functioning; EF = executive function.
p < .05.
p < .01.
Discussion
Overall findings generally supported the hypotheses. After adjusting for demographic variables and acute and chronic effects of heroin and cocaine use, a self-reported diagnosis with a learning disability or ADD/ADHD was associated with a lower pattern of performance on neuropsychological measures of intellectual and executive functions compared to individuals who did not report such conditions. Interestingly, neither chronic nor acute use was associated with impairment pattern. The lack of an association between cognition and drug use differs from previous findings (e.g., Vedejo-Garcia et al., 2004), but this result could be explained by study design utilized in previous research. Studies on cognition and substance use often exclude participants suspected of having a preexisting condition to reduce confounding, or researchers employ case-control designs. In contrast, this study sought to explore the variation in cognition by developmental condition among regular users of cocaine and heroin. Second, this study utilized scores standardized for age, which may be collinear with years of regular use and attenuated this association.
Another important finding was that those most likely to belong to the impaired profile were more likely to test positive for hepatitis B and C infection than those without impairment. This was after adjusting for known risk factors such as years of use, age, education, and participation in sexual exchange. In summary, individuals who regularly use heroin and/or cocaine and exhibit an impaired performance profile are more likely to have reported a preexisting developmental disorder such as ADHD or a learning disability. Furthermore, individuals exhibiting this pattern of performance are more likely to have contracted an infectious disease.
These findings have important implications for interventions directed at regular users of cocaine and heroin. Approximately 30% of the sample was estimated to belong to the impaired GIF and EF profile. Such a finding would suggest that about a third of chronic users of cocaine and heroin may present with some degree cognitive impairment. The fact that impairment was also observed on measures thought to be most resistant to the effects of drug use may indicate that deficits are due to conditions present prior to the onset of substance use. This would represent a large subpopulation with a greater prevalence and possibly risk of infectious diseases and, as reviewed previously, have less success in treatment programs. Therefore, targeted interventions may be needed to identify cognitively impaired individuals who regularly use drugs to aid in the reduction of infectious diseases among regular drug users. Furthermore, treatment and harm reduction programs may need to address unique needs of this population and to prevent infectious disease and treat substance use disorders within this subpopulation.
This study does have notable limitations. For example, the cross-sectional nature of the data precludes establishing whether the impairment is indeed related to preexisting conditions or is the result of chronic drug use, a combination of both, or unmeasured confounders such as other psychiatric illnesses. However, while not eliminating potential confounders, we do feel that controlling for these variables and selecting measures thought to be more resistant to cognitive decline related to drug use strengthens the case for a temporal association. Another limitation relates to the self-reported measures of learning disabilities and ADHD. Using self-reported histories are limited due to the potential biases in recall and they cannot be easily validated given that no diagnostic criteria were obtained as part of this study. In addition, no medical or educational records were obtained to verify self-reports. While this is a limitation, this analysis is innovative and novel in that it utilized neuropsychological test data to identify the possible presence of these conditions. In addition, given the generally low socioeconomic background of many participants in this sample, there may have been limited access to specialized programs and general medical care. Therefore, records may have still led to an underdiagnosis and underawareness of developmental conditions. This limitation may serve as a catalyst for greater research into the prevalence and possible increased risks of adverse health outcomes among those with learning disabilities and other developmental disorders and an SUD. Finally, the lack of a complete diagnostic interview and a larger sample size prevented the examination of the nuanced differences between different and distinct disorders as well as the potential confounding effect of comorbid psychiatric illnesses. Again, such limitations highlight the need for future research into this area focusing on whether individuals with specific developmental conditions may be at increased risk of SUDs and related health conditions.
Overall, this study highlights a substantial subgroup of heroin and cocaine users with cognitive impairment that may have been the result of preexisting conditions. These individuals could have a greater vulnerability of contracting an infectious disease. When these findings are taken into consideration with other research suggesting poorer treatment response among those with cognitive impairments (e.g. Moeller et al., 2001), a greater emphasis may need to be placed on understanding and identifying developmental disorders among drug-using populations and how to modify and address the unique concerns of these individuals.
Acknowledgments
Funding
This research was funded by a grant awarded to William Latimer from the National Institute on Drug Abuse (NIDA-R01 DA14498), the Drug Dependence Epidemiology Training Grant (NIDA T32 DA007292) at the Johns Hopkins Bloomberg School of Public Health, William Latimer, Director, and the Inderdisciplinary Alcohol Research Training Program at the University of Pittsburgh (T32 AA007453), Marie Cornelius, Director. The authors wish to acknowledge the contributions to this research staff that are and have worked at the Neurocognitive and Behavioral Research Center as well as students and fellows from the Drug Dependence Epidemiology Training Grant at the Johns Hopkins Bloomberg School of Public Health.
Biography
Stevan Geoffrey Severtson, Ph.D., is a post-doctoral fellow with the Alcohol Research Training Program at the University of Pittsburgh. His research interests focus on substance use disorders and associated health outcomes among adults with learning and cognitive impairments.
Sarra L. Hedden, Ph.D., is a postdoctoral fellow at the Johns Hopkins Bloomberg School of Public Health in the Department of Mental Health. Her research interests include drug dependence epidemiology and comparisons of statistical methods in drug dependence clinical trials.
Silvia S. Martins, M.D, Ph.D., is faculty at the Department of Mental Health, Johns Hopkins Bloomberg School of Public Health. She conducts epidemiological research on drug abuse and problem gambling epidemiology with a special emphasis on adolescence and young adulthood.
William W. Latimer, Ph.D., is Associate Professor of the Johns Hopkins Bloomberg School of Public Health. His research focuses on the epidemiology and prevention of drug dependence and infectious disease. He is director of the NIDA Drug Dependence Epidemiology Training Program (T-32 DA007292) and the Humphrey Fellowship Program for international fellows.
Footnotes
Declaration of Conflicting Interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- Beitchman JH, Wilson B, Douglas L, Young A, & Adlaf E (2001). Substance use disorders in young adults with and without LD: Predictive and concurrent relationships. Journal of Learning Disabilities, 34, 317–332. [DOI] [PubMed] [Google Scholar]
- Biederman J, Wilens TE, Mick E, Faraone SV, & Spencer T (1998). Does attention-deficit hyperactivity disorder impact the developmental course of drug and alcohol abuse and dependence? Biological Psychiatry, 44, 269–273. [DOI] [PubMed] [Google Scholar]
- Bolla KI, Funderburk FR, & Cadet JL (2000). Differential effects of cocaine and cocaine alcohol on neurocognitive performance. Neurology, 54, 2285–2292. [DOI] [PubMed] [Google Scholar]
- Cosden M (2001). Risk and resilience for substance abuse among adolescents and adults with LD. Journal of Learning Disabilities, 34, 352–358. [DOI] [PubMed] [Google Scholar]
- Culbertson WC, & Zillmer EA (2001). Tower of London-Drexel (TOL-DX) technical manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Denckla MB (1996). Biological correlates of learning and attention: What is relevant to learning disability and attention-deficit hyperactivity disorder? Journal of Developmental and Behavioral Pediatrics, 17, 114–119. [PubMed] [Google Scholar]
- Fals-Stewart W (1993). Neurocognitive defects and their impact on substance abuse treatment. Journal of Addictions & Offender Counseling, 13, 46. [Google Scholar]
- Fals-Stewart W, & Lucente S (1994). Effect of neurocognitive status and personality functioning on length of stay in residential substance abuse treatment: An integrative study. Psychology of Addictive Behaviors, 8, 179. [Google Scholar]
- Garfein RS, Vlahov D, Galai N, Doherty MC, & Nelson KE (1996). Viral infections in short-term injection drug users: The prevalence of the hepatitis C, hepatitis B, human immunodeficiency, and human T-lymphotropic viruses. American Journal of Public Health, 86, 655–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giancola PR, & Parker AM (2001). A six-year prospective study of pathways toward drug use in adolescent boys with and without a family history of a substance use disorder. Journal of Studies on Alcohol, 62, 166–178. [DOI] [PubMed] [Google Scholar]
- Gibson WA (1959). Three multivariate models: Factor analysis, latent structure analysis and latent profile analysis. Psychometrika, 24, 229–252. [Google Scholar]
- Golden CJ, & Freshwater SM (2002). The Stroop Color and Word Test: A manual for clinical and experimental uses. Chicago: Stoelting. [Google Scholar]
- Greenberg LM, Kindschi CL, & Corman CL (1999). TOVA Test of Variables of Attention: Clinical guide. Los Alimitos, CA: Universal Attention Disorders. [Google Scholar]
- Harris JC (1998). Developmental neuropsychiatry, Vol. 2: Assessment, diagnosis, and treatment of developmental disorders. 1995, New York, NY, US: Oxford University Press. [Google Scholar]
- Heaton RK, Chelune GJ, Talley JL, Kay GG, & Curtiss G (1993). Wisconsin Card Sort Test manual: Revised and expanded. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Kuo I, Sherman SG, Thomas DL, & Strathdee SA (2004). Hepatitis B virus infection and vaccination among young injection and non-injection drug users: Missed opportunities to prevent infection. Drug and Alcohol Dependence, 73, 69–78. [DOI] [PubMed] [Google Scholar]
- Lazar JW, & Frank Y (1998). Frontal systems dysfunction in children with attention-deficit/hyperactivity disorder and learning disabilities. Journal of Neuropsychiatry and Clinical Neuroscience, 10, 160–167. [DOI] [PubMed] [Google Scholar]
- Levin FR (2007). Diagnosing attention-deficit/hyperactivity disorder in patients with substance use disorders. Journal of Clinical Psychiatry, 68(Suppl. 11), 9–14. [PubMed] [Google Scholar]
- Lezak MD (2004). Neuropsychological assessment (4th ed.). Oxford, UK: Oxford University Press. [Google Scholar]
- McCoy CB, Lai S, Metsch LR, Messiah SE, & Zhao W (2004). Injection drug use and crack cocaine smoking: Independent and dual risk behaviors for HIV infection. Annals of Epidemiology, 14, 535–542. [DOI] [PubMed] [Google Scholar]
- Mitchell MM, Severtson SG, & Latimer WW (2007). Interaction of cognitive performance and knowing someone who has died from AIDS on HIV risk behaviors. AIDS Education and Prevention, 19, 289–297. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Dougherty DM, Barratt ES, Schmitz JM, Swann AC, & Grabowski J (2001). The impact of impulsivity on cocaine use and retention in treatment. Journal of Substance Abuse Treatment, 21, 193–198. [DOI] [PubMed] [Google Scholar]
- Najam N, Moss HB, Kirisci L, & Tarter RE (1997). Executive cognitive functioning predicts drug use in youth. Journal of the Indian Academy of Applied Psychology, 23, 3–12. [Google Scholar]
- Numminen H, Service E, Ahonen T, Korhonen T, Tolvanen A, Patja K, et al. (2000). Working memory structure and intellectual disability. Journal of Intellectual Disability Research, 44, 579–590. [DOI] [PubMed] [Google Scholar]
- Nylund K, Asparouhov T, & Muthen B (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: An Interdisciplinary Journal, 14, 535–569. [Google Scholar]
- Obrzut JE, Hynd GW, & Obrzut A (1983). Neuropsychological assessment of learning disabilities: A discriminant analysis. Journal of Experimental and Child Psychology, 35, 46–55. [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control. (2004). The economic costs of drug abuse in the United States, 1992–2002 (Publication No. 207303). Washington, DC: Executive Office of the President. [Google Scholar]
- Paraherakis A, Charney DA, & Gill K (2001). Neuropsychological functioning in substance-dependent patients. Substance Use and Misuse, 36, 257–271. [DOI] [PubMed] [Google Scholar]
- Roth RM, & Saykin AJ (2004). Executive dysfunction in attention-deficit/hyperactivity disorder: Cognitive and neuroimaging findings. Psychiatric Clinics in North America, 27, 83–96. [DOI] [PubMed] [Google Scholar]
- Rubin DB (1987). Multiple imputation for nonresponse in surveys. New York: John Wiley. [Google Scholar]
- SAMHSA. (2006). Results from the 2005 National Survey on Drug Use and Health: National findings. Washington, DC: Author. [Google Scholar]
- Seidman LJ (2006). Neuropsychological functioning in people with ADHD across the lifespan. Clinical Psychology Review, 26, 466–485. [DOI] [PubMed] [Google Scholar]
- Severtson SG, & Latimer WW (2006, June). Hepatitis C status among heroin and cocaine injection drug users: The role of intellectual function deficits. Poster presented at the CPDD Conference, Scottsdale, AZ. [Google Scholar]
- Severtson SG, Mitchell MM, Mancha BE, & Latimer WW (in press). The association between planning abilities and sharing injection drug use equipment among injection drug users in Baltimore, MD. Journal of Substance Use. [Google Scholar]
- Swanson HL, & Sachse-Lee C (2001). Mathematical problem solving and working memory in children with learning disabilities: Both executive and phonological processes are important. Journal of Experimental Child Psychology, 79, 294–321. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Baratta MV, Abrantes AM, & Brown SA (2002). Attention dysfunction predicts substance involvement in community youths. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 680–686. [DOI] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Lopez-Torrecillas F, Gimenez CO, & Perez-Garcia M (2004). Clinical implications and methodological challenges in the study of the neuropsychological correlates of cannabis, stimulant, and opioid abuse. Neuropsychology Review, 14, 1–41. [DOI] [PubMed] [Google Scholar]
- Vik PW, Cellucci T, Jarchow A, & Hedt J (2004). Cognitive impairment in substance abuse. Psychiatry Clinics of North America, 27, 97–109. [DOI] [PubMed] [Google Scholar]
- Wang C-P, Hendricks Brown C, & Bandeen-Roche K (2005). Residual diagnostics for growth mixture models: Examining the impact of a preventive intervention on multiple trajectories of aggressive behavior. Journal of the American Statistical Association, 100, 1054–1076. [Google Scholar]
- Wechsler D (1997). WAIS-III administration and scoring manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Westermeyer J, Kemp K, & Nugent S (1996). Substance disorder among persons with mild mental retardation: A comparative study. American Journal on Addictions, 5, 23–31. [Google Scholar]
- Westermeyer J, Phaobtong T, & Neider J (1988). Substance use and abuse among mentally retarded persons: A comparison of patients and a survey population. American Journal of Drug and Alcohol Abuse, 14, 109–123. [DOI] [PubMed] [Google Scholar]
- Zachary RA (1991). The manual of the Shipley Institute of Living Scale. Los Angeles: Western Psychological Services. [Google Scholar]