Percutaneous coronary intervention (PCI) improves survival and reduces the risk of recurrent myocardial ischemia in patients with acute coronary syndrome.1 Conversely, the role of PCI in patients with stable coronary artery disease (CAD) remains controversial.2 In the ORBITA trial, PCI was not associated with significant improvement in exercise time or angina frequency compared with a sham procedure,2 whereas long-term outcomes of the FAME 2 trial showed that a fractional flow reserve (FFR)-guided PCI strategy was superior to medical therapy (MT) in terms of cardiovascular outcomes.3 To address this controversy, we have performed an updated meta-analysis comparing the efficacy of PCI versus MT at a mean follow-up duration of 5 years.
A comprehensive search strategy was devised using MEDLINE, EMBASE and CENTRAL (inception to 30 May 2018) to identify randomized controlled trials (RCTs) with a sample size greater than 400 patients (to avoid small study effects)4 and over 4 years follow-up duration. We included trials reporting PCI with stent implantation in 70% or more of the patients and statin therapy in 50% or more patients in the study population. The outcomes of interest were all-cause mortality, myocardial infarction (MI), stroke, cardiovascular mortality, revascularization and angina relief. Quality assessment of each trial was performed using the Cochrane risk of bias tool. The literature search, data extraction and bias risk assessment was done by authors ANL, MSK and UF independently. Estimates were pooled using the DerSimonian and Laird random effects model and reported as risk ratio (RR) with 95% confidence interval (CI). Heterogeneity was quantified by I2 with values greater than 75% consistent with high grade heterogeneity. Publication bias was assessed using Egger’s regression test. Analyses were conducted at 5% significance. Comprehensive Meta-Analysis (version 3) was used for meta-analysis.
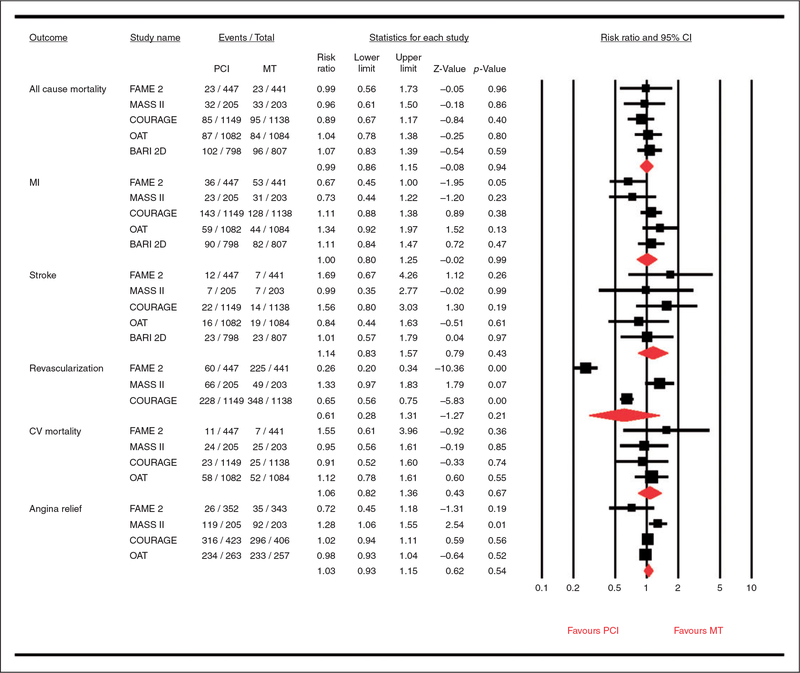
Five RCTs (8117 patients)3,5–8 were finalized in this meta-analysis (Table 1). At a mean follow-up duration of 5 years, there were no significant differences between PCI and MT in terms of all-cause mortality (RR 0.99, 95% CI 0.86–1.15, P = 95%, I2 = 0%), MI (RR 1.00, 0.95% CI 0.80–1.25, P = 0.99, I2 = 54%), stroke (RR 1.14, 95% CI 0.83–1.57, P = 0.43, I2 = 0%), revascularization 0.61, 95% CI 0.28–1.31, P = 0.21, I2= 97%), cardiovascular mortality (RR 1.06, 95% CI 0.82–1.36, P = 0.67, I2 = 0%) or angina relief (RR 1.03, 95% CI 0.93–1.15, P = 0.54, I2 = 66%) (Figure 1). Egger’s regression test did not detect publication bias (P (two-tailed) = 0.19).
Table 1.
Baseline characteristics of the studies.
| Studies (year) |
Groups | n | Age (years) |
Men (%) | DM (%) | Prior Ml (%) | LVEF (%) | Aspirin (%) | β-blockers (%) | Statins (%) | CCB (%) | ACEI/ARB (%) | Stenotic vessels >50% (mean) |
Stent (%) | DES (%) | Follow-up (months) |
CRoBa |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BARI-2D (2005)7 | PCI | 1176 | 62.3 | 70.4 | 100.0 | 31.7 | 57.0 | 93.5 | 83.9 | 94.6 | - | 91.2 | - | 90.0 | 35.0 | 5 | ***** |
| MT | 1192 | 62.4 | 70.3 | 100.0 | 32.4 | 57.3 | 94.2 | 87.9 | 95.4 | - | 92.0 | - | |||||
| OAT (2006)7 | PCI | 1082 | 58.6 | 78.0 | 18.0 | 12.0 | 47.4 | 94.0 | 86.0 | 80.0 | 65.0 | 80.0 | - | 87.0 | 8.0 | 4 | ***** |
| MT | 1084 | 58.7 | 78.0 | 23.0 | 11.0 | 48.0 | 97.0 | 89.0 | 82.0 | 61.0 | 80.0 | - | |||||
| MASS II (2006)8 | PCI | 205 | 60.0 | 67.0 | 23.0 | 52.0 | 67.0 | 100.0 | 85.0 | 74.0 | - | 28.0 | 2.35 | 72.0 | 0.0 | 5 | ***** |
| MT | 203 | 60.0 | 69.0 | 36.0 | 39.0 | 68.0 | 97.0 | 85.0 | 59.0 | - | 28.0 | 3.37 | |||||
| COURAGE (2007)5‘9 | PCI | 1149 | 61.5 | 85.0 | 32.0 | 38.0 | 60.8 | 95.0 | 85.0 | 93.0 | 42.0 | 62.0 | 1.9 | 94.0 | 3.0 | 4.6 | ***** |
| MT | 1138 | 61.8 | 85.0 | 35.0 | 39.0 | 60.9 | 94.0 | 86.0 | 93.0 | 52.0 | 65.0 | 2.0 | |||||
| FAME-2 (2018)3 | PCI | 447 | 63.5 | 79.6 | 27.5 | 37.1 | - | 90.2 | 68.3 | 90.2 | 29.3 | 78.0 | 93.9 | 97.0 | 95.0 | 5 | ****** |
| MT | 441 | 63.8 | 76.6 | 26.5 | 37.8 | - | 91.9 | 83.8 | 100.0 | 29.7 | 86.5 | 93.7 |
ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; BARI-2D: Bypass Angioplasty Revascularization 2 Diabetes; COURAGE: Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation; CCB: calcium channel blockers; CRoB: Cochrane risk of bias; DES: drug-eluting stent; DM: diabetes mellitus; FAME: Fractional Flow Reserve versus Angiography for Multivessel Evaluation; LVEF: left ventricular ejection fraction; MASS: Medicine, Angioplasty or Surgery Study; MI: myocardial infarction; OAT: Occluded Artery Trial.
Scale constitutes of seven domains: random sequence generation (selection bias); allocation concealment (selection bias); blinding of participants and personnel (performance bias); blinding of outcome assessment (detection bias); incomplete data reporting (attrition bias); selective reporting (reporting bias) and other bias. Each domain carries one star and five or more stars represents good quality.
Figure I.
Forest plot comparing percutaneous coronary intervention (PCI) versus medical therapy (MT) in stable coronary artery disease patients.
MI: myocardial infarction; CV: cardiovascular; CI: confidence interval.
This meta-analysis suggests that in patients with stable CAD, PCI was not associated with a reduction in cardiovascular outcomes, angina relief or survival benefit compared with MT at 5 years mean follow-up duration. The former meta-analyses included studies with shorter follow-ups with the lesser use of stents, which is contrary to the current standard of care.9,10 The current study is unique because of the inclusion of more contemporary trials with longer follow-up durations and studies in which the use of stents ranged from 72% to 97% in the PCI arm. Therefore, these results should be considered more robust and reliable in view of current practice.
This study revalidates the beneficial role of optimal MT in patients with stable CAD. A recent meta-analysis of 10 studies (106,002 patients) confirmed that evidence-based medication regimens (beta-blockers, angiotensin-converting enzyme inhibitors, antiplatelet therapy and statins) were associated with a reduced risk of cardiovascular events and mortality.11 However, it is important to mention that intensive MT should be coupled with aggressive risk modification to generate favorable cardiovascular outcomes. For instance, in a post hoc analysis of the BARI-2D trial, current or former smoking was associated with greater than twice the risk of all-cause mortality in patient with diabetes and stable CAD receiving MT or PCI.12 Therefore, it is critical that physicians should enforce the importance of risk modification while prescribing guideline-directed MT.
This meta-analysis has limitations which are mainly related to the limitations inherent in the included RCTs. As drug-eluting stents were approved only after 2004, PCI was performed using bare-metal stents in the majority of the RCTs with the exception of the FAME 2 trial,3 in which second generation drug-eluting stents were used as part of the study protocol. In some trials, balloon angioplasty alone without stenting was performed in more than 25% of the patients.7 Also, there were a significant number of patients who crossed over from the MT to the PCI arm in these trials, which is not factored in in this meta-analysis. Another limitation is the heterogeneity in inclusion criteria and eligibility for PCI in these RCTs. In the OAT trial, patients with stable CAD were included who had persistent total occlusion of the infarct-related coronary artery 3–28 days after MI.7 Only the FAME 2 trial included an objective criterion, FFR for inclusion in the study.3 In other trials, FFR was not mandatory to assess the significance of the coronary lesion. The majority of the patients probably represented a low-risk cohort, as evident from an average left ventricular ejection fraction of over 45% in all these trials. Furthermore, only a small proportion of patients with multivessel disease were included in these trials. Only one third of patients in the COURAGE and BARI-2D trials had three-vessel disease,5,6 while the FAME 2 trial included only 9% of patients with three-vessel disease.3
In conclusion, in patients with stable CAD, PCI was not associated with a reduction in cardiovascular outcomes, angina relief or improved survival compared with MT at a mean follow-up duration of 5 years.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Windecker S, Kolh P, Alfonso F, et al. 2014. ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35: 2541–2619. [DOI] [PubMed] [Google Scholar]
- 2.Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet (London, England) 2018; 391: 31–40. [DOI] [PubMed] [Google Scholar]
- 3.Xaplanteris P, Fournier S, Pijls NHJ, et al. Five-year outcomes with PCI guided by fractional flow reserve. N Engl J Med 2018; 379: 250–259. [DOI] [PubMed] [Google Scholar]
- 4.Schwarzer G, Carpenter JR and G. Small-study effects in meta-analysis In: Meta-Analysis with R. Cham: Springer International Publishing, 2015, pp. 107–141. [Google Scholar]
- 5.Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356: 1503–1516. [DOI] [PubMed] [Google Scholar]
- 6.Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009; 360: 2503–2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hochman JS, Lamas GA, Buller CE, et al. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 2006; 355: 2395–23407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hueb W, Lopes NH, Gersh BJ, et al. Five-year follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation 2007; 115: 1082–1089. [DOI] [PubMed] [Google Scholar]
- 9.Stergiopoulos K, Boden WE, Hartigan P, et al. Percutaneous coronary intervention outcomes in patients with stable obstructive coronary artery disease and myocardial ischemia: a collaborative meta-analysis of contemporary randomized clinical trials. JAMA Intern Med 2014; 174: 232–240. [DOI] [PubMed] [Google Scholar]
- 10.Thomas S, Gokhale R, Boden WE, et al. A meta-analysis of randomized controlled trials comparing percutaneous coronary intervention with medical therapy in stable angina pectoris. Can J Cardiol 2013; 29: 472–482. [DOI] [PubMed] [Google Scholar]
- 11.Du L, Cheng Z, Zhang Y, et al. The impact of medication adherence on clinical outcomes of coronary artery disease: a meta-analysis. EurJ Prev Cardiol 2017; 24: 962–970. [DOI] [PubMed] [Google Scholar]
- 12.Khan AA, Chung MJ, Novak E, et al. The long-term risk of smoking in diabetic patients with stable ischemic heart disease treated with intensive medical therapy and lifestyle modification. EurJ Prev Cardiol 2017; 24: 1506–1514. [DOI] [PubMed] [Google Scholar]