Abstract
Objective:
Previous studies suggest that maternal postpartum mental health issues may impact parenting and child development in preterm infants, but have often not measured symptomatology in the Neonatal Intensive Care Unit (NICU) nor followed families through early childhood. This study examines how maternal depressive symptoms and stress in the NICU are related to parenting behaviors at age 5 years, in mothers of children born very preterm (≤30 weeks gestation).
Method:
This longitudinal study followed a diverse sample of 74 very preterm children and their mothers. Maternal depression and stress were assessed in the NICU. At age 5, mother-child dyads were observed and coded for maternal intrusiveness, negativity, sensitivity, and positivity. Other covariates, including maternal and child intelligence, maternal education, income-to-needs ratio, maternal depression at age 5 years, and child sex were included in multivariate analyses.
Results:
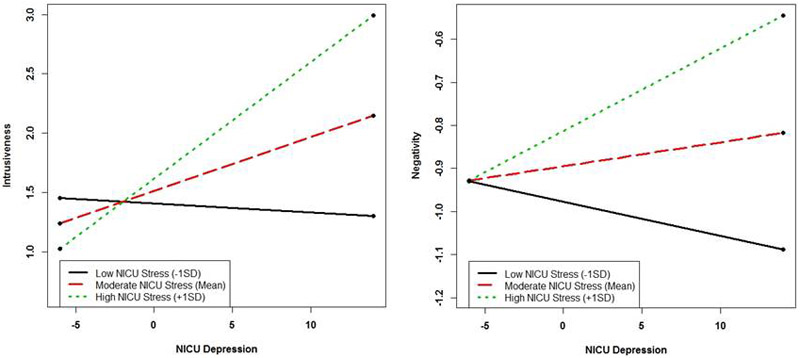
The interaction between maternal NICU stress and NICU depression for intrusiveness and negativity indicates that greater NICU depression was associated with more intrusiveness under medium or high levels of NICU stress, and more negativity under high levels of NICU stress. Furthermore, greater NICU depression was associated with less sensitivity, over and above other covariates.
Conclusion:
Findings suggest that early maternal peripartum depression and stress in the NICU can have lasting impacts on multiple parenting behaviors, highlighting the need for screening and targeted interventions in the NICU.
Keywords: parenting, parent-child interactions, depression, NICU, preterm
INTRODUCTION
The preterm birth rate in the United States remains near 10% of all deliveries, and is increasing.1 Improved survival of premature infants secondary to neonatology advances2 has led to a corresponding increase in relative parental pathology, particularly for mothers.3–5 A compelling body of literature demonstrates that premature birth and subsequent Neonatal Intensive Care Unit (NICU) hospitalization adversely impacts maternal mental health, with mothers of NICU infants diagnosed with higher rates of depression,6–8 posttraumatic stress,4,9 and anxiety.7 The NICU is a uniquely stressful experience for both mothers and infants, with maternal concerns regarding the infant’s survival, inability to nurture (i.e. holding/feeding), helplessness about the future, and finances all potentially impacting outcomes for both mothers and infants.10,11
Investigation into this critical postpartum period indicates that maternal depression may impact parenting behaviors which could impair neurodevelopment of preterm infants.8,12 Maternal behaviors studied include: intrusiveness (i.e. controlling behavior), negativity, sensitivity (i.e. responsiveness to child), and positivity. Longitudinal studies have found a consistent impact of maternal postpartum depression (PPD) on parenting and early childhood development in term infants, including increased likelihood of behavior problems, sleep difficulties, and cognitive and language impairments.13–16 Emerging literature suggests similar findings in the preterm population, with the impact of this perturbation in the maternal-infant parenting system wide-ranging and long-lasting.17–19
While research performed to date has examined the impact of maternal psychopathology in the postpartum period on specific parenting behaviors (e.g., intrusiveness, sensitivity) in preterm infants,8,17,19 the long-term impact of maternal depression and stress processes that specifically occur in the NICU, rather than after the child returns home, remains unknown based upon existing studies. Research has indicated that mothers of children in the NICU show higher levels of depression and anxiety symptoms than those with healthy term children.5–7 However, while mothers of NICU children indicate multiple NICU stressors,20 it is unknown whether NICU stress operates independently (in an additive way) to NICU depression in predicting behaviors, or whether the stress and depression may interact with one another, exacerbating difficulties. Prior research on term children has found other life events can moderate the impact of maternal depression.14
The study is one of the first that examines the impact of NICU maternal depression and NICU stress on multiple parenting behaviors, including intrusiveness, negativity, sensitivity, and positivity, in mothers of preterm-born children now 5-years old. We hypothesized that higher levels of maternal NICU depression and NICU stress would be related to greater intrusiveness and negativity, and less sensitivity and positivity. Additionally, we hypothesized that these parenting behaviors would interact with one another, such that the impact of NICU depression on all four parenting behaviors would be worse when the mother also experienced high NICU stress.
METHOD
Participants
This study was a prospective, longitudinal multi-method study, investigating mothers and very preterm children (VPT; ≤30 weeks gestation). Participants were recruited within the first three days of life from a Level III NICU in the Midwestern United States between 2007-2010, serving a diverse racial/ethnic and socioeconomic population. Exclusion criteria included known congenital anomaly, severe sepsis, or respiratory failure in the first 72 hours of life. Twohundred nineteen people were recruited for this study. Of those recruited but not enrolled, 18 declined participation, and 46 were too sick or the attending physician declined participation. One hundred fifty-five subjects were enrolled in the study, and 95 subjects had a mother complete the NICU questionnaire battery. Reasons for not completing the battery included expiration (n=20), transfer (n=1), withdrawal (n=7), refusal, completion by another family member, and adoption (n=32). Seventy-six participants completed the 5-year follow-up visit (17 participants were lost to follow-up, 2 participants expired after discharge) (Figure S1, available online). There were no differences in NICU depression, NICU stress, child sex, income-to-needs ratio, medical risk, or race between those who dropped out of the study and those who remained. Mothers who remained were more likely to have had some college education, and thus education was controlled for in analyses. In multiple birth families (31%), all children were included, as individual parent-child relationships may vary within multiples.21 Two participants were not living with their mother at follow-up. The final sample included 74 VPT children in 62 families. Median gestational age was 26 weeks (Interquartile Range=25-28, Range=23-30), 57% were on public health insurance, 42% in single parent households, and child’s race/ethnicity was 55% Caucasian, 37% African-American, 4% Asian, 4% Biracial (Table 1). Using the Bayley Scales of Infant Development-III (BSID-III)22 at age 2, children’s median cognitive score on the BSID-III and interquartile range was 85±15, language score was 89±18, and motor development score was 85±15.
Table 1.
Sample Demographics and Neonatal Characteristics (N=74)
| Variable | Frequency(%) | Mean±SD or Median(IQR) |
|---|---|---|
| Neonatal Characteristics | ||
| Gestational Age(wks) | 26(25-28) | |
| Birthweight(g) | 855(708-1075) | |
| Sex(Male) | 34(46%) | |
| Multiple Birth | 27(37%) | |
| Race(African-American) | 27(37%) | |
| Endotracheal Ventilation(hours) | 90(24-756) | |
| Postnatal Steroids | 8(11%) | |
| Confirmed Sepsis | 24(32%) | |
| Necrotizing Enterocolitis | 5(7%) | |
| Requires O2 at 36wks | 43(58%) | |
| PDA requiring Medication | 33(45%) | |
| Days in NICU | 90±25 | |
| Neonatal Risk Composite | 2.1±1.8 | |
| Maternal and Social Characteristics in NICU | ||
| Maternal Age at Birth(years) | 28(23-34) | |
| Parity | 2±1 | |
| Public Insurance | 42(57%) | |
| EPDS Score | 6(1-12) | |
| NICU Stress Scale Score | 2.7(2.1-3.9) | |
| 5 Year Follow-Up | ||
| Age at Testing(years) | 5.5(5.33-5.75) | |
| Public Insurance | 42(57%) | |
| Child Full Scale IQ | 90±14 | |
| Maternal IQ | 96±12 | |
| Maternal Education(At least some college) | 57(77%) | |
| Income-to-Needs Ratio | 1.26(0.83-2.47) | |
| Maternal Depression(BDI-II) | 6±9 | |
| Maternal Intrusiveness | 1.6±0.9 | |
| Maternal Negativity | −.86±.23 | |
| Maternal Sensitivity | 4.0±1.0 | |
| Maternal Positivity | 3.8±1.0 | |
Note: Means and SDs are reported for normally distributed data; Medians and Interquartile Ranges (IQR) are reported for nonnormally distributed data. Maternal negativity was initially skewed, so a reciprocal transformation (1/negativity) was completed to normalize data, and then reverse coded. NICU=Neonatal Intensive Care Unit. BDI-II = Beck Depression Inventory, 2nd Edition; EPDS = Edinburgh Postnatal Depression Scale; PDA = Patent Ductus Arteriosus.
Procedure
At NICU discharge, mothers completed a battery of questionnaires that included measures of stress, depression, and family demographics.7 At 5-years, children returned for a research visit and completed a comprehensive neurodevelopmental assessment (Median=5.5 years, Range=4.7-6.8 years). Mothers and children also completed mother-child interactions that were videotaped. Mothers were told to complete a jigsaw puzzle, match letters, build a tower, and perform a color/shape matching activity with their child, in that order.23 Following the interaction, mothers and children were simultaneously administered standardized measures of intelligence by two different study staff. After completion of the intelligence testing, mothers completed a depression questionnaire. Of note, there were assessments performed at 2 years, however, due to only a small percentage of children completing a parent-child interaction at 2, these measures were not included in the study, with the exception of the BSID-III22 for sample description.
Ethical Considerations.
Informed consent was obtained in the NICU with re-consent at the 2 and 5-year longitudinal visits. The IRB approved all aspects of this study.
Measures
Maternal depressive symptoms.
Mothers completed the Edinburgh Postnatal Depression Scale (EPDS)24 at NICU discharge. This 10-item self-report measure assesses PPD over the prior 7 days with a score of 13 or higher (Range=0-30) indicating clinically significant PPD. The EPDS has been well-validated as a predictor of clinical depression in postpartum women.30 Mothers later completed the Beck Depression Inventory, 2nd Edition (BDI-II)25 at age 5, a 21-item self-report that assesses depressive symptoms with scores >19 indicating moderate to severe depression, and >14 indicating mild depression.
NICU stress.
Mothers completed a modified version of the NICU parental role alteration subscale of the Parental Stressor Scale (PSS)26 at discharge. In this 10-item scale (Range=10-50), higher scores indicate feeling more stress surrounding parental role alteration. There is no clinical cut-off, and prior research indicates that higher PSS scores are associated with lower family income, single parent families, and first NICU experience.20 Items ask about stressful aspects of the NICU experience, including not being able to or being afraid to hold, feed, or otherwise care for the baby. Only this subscale was collected to reduce participant burden and the maximize participants completing the entire survey.
Neonatal risk.
The Infant Clinical Risk Index (Range= 0–10) was modeled on an existing risk index for VPT infants23 comprised of the following dichotomized factors: small for gestational age, oxygen therapy at 36-weeks, maternal antenatal steroids (no=1, yes=0), postnatal steroids, necrotizing enterocolitis, treated patent ductus arteriosus, retinopathy of prematurity, culture-positive sepsis, change in weight-for-height/length standard deviation (SD) score, and upper quartile for days receiving total parenteral nutrition.
Socioeconomic risk.
Two measures of socioeconomic risk were collected at age 5. Maternal education was measured on a 5-category scale, from Junior High to a Post-Graduate Degree. We used a dichotomous split of having at least some college education or having a high school or education or less (n=17, 23%). Income-to-needs ratio was operationalized as the total family income divided by the federal poverty level based on family size in the year of the followup visit, a method previously used in this and other cohorts.27 The ratio was initially skewed because of two mothers (three children) with higher family incomes; these three participants were top-coded to the next highest income-to-needs ratio. These socioeconomic factors at NICU discharge were also examined, but variables did not significantly vary across time (i.e. education correlation: ρ=.73, P<.001) or produce distinct results; thus only age 5 variables were used.
Child and maternal intelligence.
Child intelligence was measured at the 5 year visit using the full scale intelligence quotient (IQ) composite from the Wechsler Preschool and Primary Scale of Intelligence, 3rd Edition.28 Maternal IQ was measured at the 5 year visit using the Weschler Test of Adult Reading (WTAR).29 Child cognitive, motor, and language development at age 2 were assessed using the BSID-III,22 although only used for descriptive purposes. All scales are normed with M=100, SD=15.
Parenting behaviors.
The videotaped mother-child interactions were coded for four different parenting behaviors: maternal intrusiveness, sensitivity, negativity, and positivity. These were coded using the Parent-Child Interaction Rating Scale (PCIRS),30 a validated measure of parenting that has been used extensively in samples of children with and without developmental delays.31–33 It is highly similar to the parenting scales from the NICHD Early Child Care Research Network (ECCRN),34 which has been used with families of preterm children,35 and is consistent with other measures of sensitivity and intrusiveness.36 Maternal intrusiveness measures how interactions are adult-centered, overstimulating, and controlling. Maternal negativity measures expression of negative affect or tone, hostility, or disapproval. Maternal sensitivity measures how interactions are child-centered, well-timed, and appropriate to the needs, mood, capabilities of the child. Maternal positivity measures the expression of positive affect, tone, warmth, and praise for the child. All scales are 1-5; higher scores indicate greater intensity and frequency. Ratings were made by a master coder and team of research assistants blinded to the hypotheses of the study. Research assistants were trained for multiple sessions using previously coded tapes before reliability was assessed with a weighted kappa criterion (κ=.60). Once reliability was established, coders independently coded tapes; 25% of tapes were coded by everyone for continuing reliability purposes. Disagreements were discussed in group and decided upon by the master coder. Interclass Correlation Coefficients (ICCs) collected at the end of the study all indicated excellent reliability: intrusiveness (ICC=.869), negativity (ICC=.909), sensitivity (ICC=.848), and positivity (ICC=.932).
Statistical Analyses
We conducted correlation analyses (Spearman’s rho) to examine the association of potential covariates with parenting behaviors. Covariates examined included child sex (0=female, 1=male), maternal education (0=some college or higher, 1=high school or less), income-to-needs ratio, maternal IQ, child IQ, and 5-year maternal depressive symptoms. Neonatal medical risk, parity, gravidity, child age at 5-year visit, and race were also examined as potential covariates, but were not correlated with any parenting behaviors and not included in the final model. Given the imperfections associated with using correlations in nested data (i.e. multiple births), any variables correlated p<.10 for any model were retained as covariates for final analyses.
One regression was conducted for each parenting behavior using linear mixed modeling in IBM SPSS Statistics, Version 24 to account for nested data. Interactions and simple slopes between NICU stress and NICU depression were analyzed;37 only significant interactions were included in the final models.
Analyses utilized multiple imputation to address 12 participants (16%) who were missing the mother-child interaction data, but completed the battery of questionnaires at discharge and 5-year follow-up. Mother-child interaction data was missing due to malfunctioning equipment or fathers participating in the interaction task. Multiple imputation provides more accurate estimates than listwise deletion.38 Fifty datasets were generated with the missing data randomly produced and aggregate (pooled) data is reported.38
Due to the relatively smaller sample size, final analyses were verified by running the non-imputed dataset with bootstrapping (1000 samples) and 95% confidence intervals to assess stability of our findings and both datasets produced similar results (Table S1, available online).
RESULTS
Overall, 21% of included mothers had clinically significant PPD at NICU discharge. At the 5 year assessment, 4% had moderate to severe depression, and 10% had mild depression. The means for both timepoints were below the clinical range, and they were not significantly correlated with one another (Table 2). Twenty percent of those with significant depressive symptoms at NICU discharge also had clinically significant depression at 5 years. Between potential predictors and 5-year parenting behaviors, greater NICU depression and NICU stress were associated with greater intrusiveness, less sensitivity, and greater negativity. NICU stress was also associated with less positivity, although mothers were more sensitive toward their daughters ρ=−.24, p=.020). Parenting behaviors were moderately to strongly correlated with one another (Table 2).
Table 2.
Correlation Table of Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. NICU Depression | ||||||||||||
| 2. NICU Stress | .08 | |||||||||||
| 3. Child Sex | .02 | .05 | ||||||||||
| 4. Maternal Education | .06 | .34** | .21 | |||||||||
| 5. Income to Needs | .03 | −.24* | −.19 | −.50*** | ||||||||
| 6. Child IQ | −.01 | −.43*** | −.28* | −.27* | .08 | |||||||
| 7. Maternal IQ | .02 | −.23 | −.18 | −.57*** | .55*** | .38** | ||||||
| 8. Depression at 5 | .12 | .18 | −.11 | .08 | .02 | −.16 | .05 | |||||
| 9. Intrusiveness | .43*** | .28* | .17 | .27* | −.10 | −.25* | −.06 | .02 | ||||
| 10. Negativity | .32** | .35** | .06 | .17 | −.20 | −.11 | −.14 | .11 | .62*** | |||
| 11. Sensitivity | −.25* | −.27* | −.24* | −.24* | .17 | .21 | .22 | .02 | −.51*** | −.52*** | ||
| 12. Positivity | .00 | −.26* | −.21 | −.24 | .17 | .17 | .18 | .05 | −.36** | −.46*** | .63*** |
Note: Correlations conducted using Spearman’s rho due to rank-order data, and completed in unadjusted samples. Child Sex was coded such that 0=female, 1=male. Maternal Education was coded such that 0=some college or higher, 1=high school or less. NICU = Neonatal Intensive Care Unit.
p < .05
p < .01
p < .001
Among potential predictor variables, maternal NICU depression was not associated with NICU stress or any other covariates. Greater NICU stress was associated with a smaller income-to-needs ratio, less maternal education, and lower child IQ. As expected, maternal education and income-to-needs were strongly negatively correlated with each other, and greater maternal education was strongly associated with higher maternal IQ. Less maternal education was associated with greater intrusiveness and less sensitivity. Higher child IQ was also associated with less intrusiveness and moderately associated with a higher maternal IQ.
Although maternal positivity and sensitivity were strongly correlated, as were maternal negativity and intrusiveness, we kept them as four separate dependent variables both due to their theoretical differences, and the differences in the strengths of their relationships with other variables. For example, while maternal sensitivity was negatively correlated with NICU depression (r=−.25), there was no relationship between maternal positivity and NICU depression (r=.00). Prior research using these scales have also analyzed them separately.31,32
Regression Analyses
For maternal intrusiveness, there was an interaction between NICU depression and NICU stress (Table 3). The interaction was probed by examining simple slopes.37 Subjects were not split into groups as these were continuous×continuous interactions, but examined at three different points along the regression line. Simple slopes were created at −1SD, Mean, and +1SD of NICU Stress (Figure 1). At low levels of NICU Stress, depression was not related to intrusiveness, B(SE)=−.01(.03), p=.807. At the mean of NICU Stress, greater depression was associated with more intrusiveness, B(SE)=.05(.02), p=.014. At high levels of NICU stress, this relation was even stronger, B(SE) =.10(.02), p<.001. In addition, lower child IQ scores were associated with greater maternal intrusiveness. None of the other variables remained significant predictors in the final model.
Table 3.
Mixed Model Regressions to Age 5 Parenting Behaviors
| B | SE | P | 95% CI | |
|---|---|---|---|---|
| Model: Maternal Intrusiveness | ||||
| Depression × NICU Stress | .04 | .02 | .028 | [.005,.082] |
| Depression at Discharge | .05 | .02 | .012 | [.011,.0891] |
| NICU Stress at Discharge | .14 | .13 | .284 | [−.115,.392] |
| Model: Maternal Negativity | ||||
| Depression × NICU Stress | .01 | .00 | .039 | [.001,.0201] |
| Depression at Discharge | .01 | .01 | .132 | [−.002,.018] |
| NICU Stress at Discharge | .08 | .03 | .010 | [.021,.1521] |
| Model: Maternal Sensitivity | ||||
| Depression at Discharge | −.05 | .02 | .021 | [−.094,−.008] |
| NICU Stress at Discharge | −.13 | .15 | .377 | [−.417,. 158] |
| Model: Maternal Positivity | ||||
| Depression at Discharge | −.00 | .02 | .925 | [−.045,.050] |
| NICU Stress at Discharge | −.20 | .15 | .203 | [−.508,. 111] |
Note: N=74. Numbers represent pooled unstandardized regression coefficients with regressions done in linear mixed modeling. All models adjusted for child sex, maternal education, income to needs ratio, child IQ, maternal IQ, and maternal depression at age 5. Only child IQ remained a significant predictor of Intrusiveness at age 5, B(SE)=−.02(.01), p=.024. Full results available upon request. NICU = Neonatal Intensive Care Unit; SE = standard error.
Figure 1.
Interactions Between Maternal Depression and Neonatal Intensive Care Unit (NICU) Stress on (a) Intrusiveness and (b) Negativity
Note: Figure 1 demonstrates the significant interactions between NICU Depression and NICU Stress on observed intrusiveness (left) and negativity (right). Simple slopes are at −1 SD, the mean, and +1 SD of NICU Stress.
For maternal negativity, there was an interaction between NICU depression and higher NICU stress (Table 3, Figure 1). At low levels of NICU stress, depression was not associated with negativity, B(SE)=−.01(.01), p=.258, nor were they associated at moderate levels of NICU Stress, B(SE)=.01(.00), p=.200. However, at high levels of NICU Stress, greater depression was associated with greater negativity, B(SE)=.02(.01), p<.001. None of the other variables remained significant predictors in the final model.
For maternal sensitivity and positivity, the interaction between NICU depression and NICU stress was not significant so the final model is interpreted without the interaction. For maternal sensitivity, regression analyses using linear mixed modeling indicated that more NICU depressive symptoms were associated with less sensitivity at the 5-year visit (Table 3). For maternal positivity, although NICU stress was correlated with less positivity in the zero-order correlations, none of the predictors were significant in the mixed modeling after adjusting for all variables in the model.
DISCUSSION
This study is one of the first longitudinal studies to identify and examine depression and stress in a racially/ethnically diverse set of mothers of VPT children while still in the NICU and follow parenting through early childhood. Our findings suggest both maternal NICU depression and NICU stress play significant roles in later parenting behaviors, long after discharge, even after accounting for other known risk factors. Greater depressive symptomatology at NICU discharge was related to less sensitive and more intrusive mothering at age 5. That these findings were seen five years later suggests that early maternal depression disrupts early parent-child relational processes39 and can have long-term implications for development.
Maternal depression has long been considered a critical risk factor in the mother-child bond.13,14 When depressed, it can be difficult to be sensitive and child-centered, while negativity and impatience may be more immediate responses to frustration.40 However, the majority of studies examining the link between PPD and parenting behaviors have investigated mothers of typically developing children.
For mothers of children born VPT, depression during the NICU hospitalization may be a different experience than mothers who face PPD with their child at home.4 In our study, mothers had not taken their infants home from the hospital, and may have experienced many other stressors specifically related to being in the NICU. Our findings indicated that mothers with higher levels of NICU Stress were less educated, younger, had a lower income-to-needs ratio, and had children with lower IQs, which may have exacerbated the NICU experience.
Screening for maternal depression is becoming more commonplace in the NICU41,42 and our findings support that early screening and intervention for mothers is critical. Our findings suggested 21% of mothers experienced clinical depression at NICU discharge. Although some studies report higher rates,42 this is in line with other studies examining NICU depressive symptoms, suggesting about 1 in 5 suggests women are at substantial risk.5,43
However, if NICUs are only screening for depression, they may be missing important risk factors. Our study included a screener of NICU stress measuring specific aspects of stress unique to having an infant in the NICU, such as not being able hold your baby,26 and found increased maternal NICU stress was related to more negative and intrusive parenting at age 5. In particular, there was an interaction between NICU stress and NICU depression, such that in cases of high NICU stress, depression was strongly related to greater intrusiveness and negativity. In cases of low NICU stress, depression did not appear to play a role in intrusiveness or negativity. Thus, NICU stress and depression appear to be distinct constructs and predictors. Maternal depression may be more important for sensitivity, but the impact of NICU stress and depression seem to work in tandem for the more negative and intrusive aspects of later parenting. Given these results, it is recommended that both stress and depressive symptoms be measured in the NICU to form a more comprehensive and nuanced picture of maternal functioning.
There was no association between NICU stress or depression and positive parenting, which was surprising given the strong correlation between sensitivity and positivity. However, the timing of depressive symptoms may play a role; depression in the NICU may disrupt how mothers learn to respond to cues at the beginning of the child’s life, which could impact bonding and relational processes.4,16 Depressive symptoms may have an impact on positive parenting later in development, when the child is a more active player in the relationship. Thus, while maternal NICU depression may have long-term implications for noticing child cues and appropriate responsiveness, it could have a reduced role in the amount of praise and positive affect displayed toward the child. Additionally, specific aspects of depression (i.e. worry) may be more prevalent in mothers of VPT infants than other symptoms, differentially impacting positive and negative parenting behaviors.
Furthermore, maternal depression when the child was 5 was included as a covariate to ensure that our findings regarding NICU symptomatology were not due to chronic depression,44 though, notably, NICU depression and 5 year depression were not associated. This may indicate that NICU depression has distinct characteristics, differing from other time points. We used the EPDS to measure depression at NICU discharge, which is a readily available standard measurement of PPD. However, assessing mothers at NICU discharge perhaps meant they were experiencing different emotions as they prepared to go home, including increased worry, or relief. Future studies examining PPD should follow-up with mothers one to two months after discharge to determine the stability of symptomatology, and use clinical interviews in addition to questionnaires. Furthermore, correlations may have been attenuated by using a different depression questionnaire at age 5, as the EPDS only measures PPD.
Depression at age 5 was also not correlated with any parenting behaviors, which was surprising, as this association has been found in other research on depression and parenting.14,18,19 There are a number of potential explanations. Fourteen percent of mothers had clinically significant depression at child age 5, which is consistent with other preterm studies looking at symptomatology during this age period,43,45 although higher rates are also seen.44 However, a more impaired sample may be needed to find associations between depression and parenting later in development, as these associations have primarily been examined earlier in development for preterm families.19 The first year of life is often seen as a “sensitive period” where maternal depression may be differentially important for the child,16 which may explain our findings. The diversity of our VPT infant sample is distinct from prior samples, which include fewer families of lower socioeconomic risk, although diverse samples of preterm infants still generally find depression and parenting are related.46 It also unknown if other parent-child interaction tasks, such as a free play task, would have elicited concurrent links between depression and parenting behaviors.
We also examined a number of well-known risk factors as covariates, including parent and child IQ, child sex, and measures of SES, and found less maternal education was correlated with greater NICU stress, less sensitivity, and more intrusiveness. The link between maternal general stress and education is well-known in the literature,47 but there may be clinical implications for NICU stress in particular. For example, there may be alternative ways to provide information to families with less education that may be more helpful, ways of encouraging additional social support, or providing stress-reducing interventions.3,48
In this study, lower child IQ was also associated with greater intrusiveness, which has been found in other studies of preterm children.17 While intrusiveness generally has negative implications for a child’s behavior, that is not always true in high-risk samples, who may require more direct intervention from parents. Of note, child and maternal IQ were moderately positively associated with one another, which could indicate heritability of IQ,27 although interestingly, maternal IQ was unrelated to intrusive parenting. Future research should examine how intelligence may moderate the impact of intrusiveness on child outcomes.
One important limitation of our study is that there is no comparison group of term infants or low-risk late preterm infants at birth, and this study only applies to mothers of VPT children. At the time of initial data collection, the focus was on understanding the developmental course of our highest-risk preterm infants while still in the NICU. One of our key measures, NICU stress, examines feelings associated with having a child in the NICU, and we could not have measured this in other comparison groups that are not cared for in the NICU. While our goal is to understand how the symptomatology in the NICU environment impacts long term parenting behaviors, we cannot know whether our findings would generalize to maternal stress and depression more broadly, in both late preterm and term populations. The results regarding the NICU experience of VPT infants itself may also not generalize to moderate or late preterm infants who do spend time in the NICU. There are other limitations that must be considered. Our sample size, while substantial for a cohort of VPT children, was modest and may have impacted our power to identify significant covariates or interactions. There were 12 missing mother-child interactions which could have impacted results, however, they were not associated with study or demographic variables and multiple imputation was used to account for the missing data. As a further check, we repeated all our final regressions using bootstrapping, and these yielded the same significant results. We used continuous variables in the interaction, so as not to split the sample into groups and further reduce power. We also had a substantial age range for the 5-year time point, although age at 5-year testing was not correlated with parenting behaviors. While our protocol specified testing children around their fifth birthday, to reach families and increase retention rates, multiple attempts were used, and participants were brought in when available.
Overall, our findings suggest that early maternal symptomatology in the NICU can have a lasting impact on parenting behaviors. These findings highlight that screening for NICU stress along with depression is imperative to better understand the challenges these mothers face. This is a novel finding and important considering the growing evidence indicating that infants’ environments, including aspects of parenting, are important for strengthening neural pathways underlying cognitive, language, and social-emotional development,10 and may be differentially important in children born preterm.18 Providers may find it helpful to thoughtfully consider the role of prematurity on parenting and children’s behavior as they mature, and ask questions about the impact of NICU admission on parental functioning. Further, it is critical to examine and identify those mothers who are experiencing both higher levels of depression and stress in the NICU so that medical professionals can provide targeted interventions for families during and after the NICU course. Future research should examine how parenting behaviors may mediate the process between NICU experience and later child outcomes.
Supplementary Material
Acknowledgments
This work was supported by the National Institute of Health (grants NIH R01 HD057098, U54 HD087011, K23 MH105179, K02 NS089852, UL1 TR000448, and including sub award KL2 TR000450), the McDonnell Center for Systems Neuroscience, the Cerebral Palsy International Research Foundation, the Dana Foundation, the Child Neurology Foundation, and the University of Missouri-St. Louis Office of International Programs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Dr. Rogers has received grant or research support from the National Institute of Mental Health, the McDonnell Center for Systems Neuroscience, St. Louis Children’s Hospital, the Parker Fund for Young Investigators, and the Doris Duke Charitable Foundation. She has served as a consultant to the Nurses for Newborn’s Foundation. She has received travel expenses from the American College of Neuropsychopharmacology. Drs. Gerstein, Njoroge, Smyser, and Ms. Paul report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Dr. Emily D. Gerstein, University of Missouri-St. Louis, MO..
Dr. Wanjiku F.M. Njoroge, Perelman School of Medicine at the University of Pennsylvania..
Ms. Rachel A. Paul, Washington University School of Medicine, St. Louis, MO..
Dr. Christopher D. Smyser, Washington University School of Medicine, St. Louis, MO..
Dr. Cynthia E. Rogers, Washington University School of Medicine, St. Louis, MO..
REFERENCES
- 1.Martin JA, Hamilton BE, Osterman M. Births in the United States, 2016. NCHS Data Brief. 2017;64(287):1–8. [PubMed] [Google Scholar]
- 2.Stefana A, Lavelli M. Parental engagement and early interactions with preterm infants during the stay in the neonatal intensive care unit: protocol of a mixed-method and longitudinal study. BMJ Open. 2017;7(2):e013824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mendelson T, Cluxton-Keller F, Vullo GC, Tandon SD, Noazin S. NICU-based interventions to reduce maternal depressive and anxiety symptoms: a meta-analysis. Pediatrics. 2017:e20161870. [DOI] [PubMed] [Google Scholar]
- 4.Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU). J Clin Psychol Med Settings. 2010;17(3):230–237. [DOI] [PubMed] [Google Scholar]
- 5.Vigod SN, Villegas L, Dennis C, Ross LE. Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG Int J Obstet Gynaecol. 2010;117(5):540–550. [DOI] [PubMed] [Google Scholar]
- 6.Miles MS, Holditch-Davis D, Schwartz TA, Scher M. Depressive symptoms in mothers of prematurely born infants. J Dev Behav Pediatr. 2007;28(1):36–44. [DOI] [PubMed] [Google Scholar]
- 7.Rogers CE, Kidokoro H, Wallendorf M, Inder TE. Identifying mothers of very preterm infants at-risk for postpartum depression and anxiety before discharge. J Perinatol. 2013;33(3):171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korja R, Savonlahti E, Ahlqvist-Björkroth S, et al. Maternal depression is associated with mother–infant interaction in preterm infants. Acta Paediatr. 2008;97(6):724–730. [DOI] [PubMed] [Google Scholar]
- 9.Feeley N, Zelkowitz P, Cormier C, Charbonneau L, Lacroix A, Papageorgiou A. Posttraumatic stress among mothers of very low birthweight infants at 6 months after discharge from the neonatal intensive care unit. Appl Nurs Res. 2011;24(2):114–117. [DOI] [PubMed] [Google Scholar]
- 10.Montirosso R, Tronick E, Borgatti R. Promoting neuroprotective care in Neonatal Intensive Care Units and preterm infant development: Insights from the neonatal adequate care for quality of life study. Child Dev Perspect. 2017;11(1):9–15. [Google Scholar]
- 11.Carter JD. Infants in a neonatal intensive care unit: parental response. Arch Dis Child - Fetal Neonatal Ed. 2005;90(2):F109–F113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldman R, Granat A, Pariente C, Kanety H, Kuint J, Gilboa-Schechtman E. Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. J Am Acad Child Adolesc Psychiatry. 2009;48(9):919–927. [DOI] [PubMed] [Google Scholar]
- 13.Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. 2010;33(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clin Psychol Rev. 2000;20(5):561–592. [DOI] [PubMed] [Google Scholar]
- 15.Grace SL, Evindar A, Stewart D. The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch Womens Ment Health. 2003;6(4):263–274. [DOI] [PubMed] [Google Scholar]
- 16.Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: A sensitive period? J Am Acad Child Adolesc Psychiatry. 2010;49(7):699–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wolke D, Jaekel J, Hall J, Baumann N. Effects of sensitive parenting on the academic resilience of very preterm and very low birthweight adolescents. J Adolesc Health. 2013;53(5):642–647. [DOI] [PubMed] [Google Scholar]
- 18.Poehlmann J, Hane A, Burnson C, Maleck S, Hamburger E, Shah PE. Preterm infants who are prone to distress: differential effects of parenting on 36-month behavioral and cognitive outcomes. J Child Psychol Psychiatry. 2012;53(10):1018–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muller-Nix C, Forcada-Guex M, Pierrehumbert B, Jaunin L, Borghini A, Ansermet F. Prematurity, maternal stress and mother–child interactions. Early Hum Dev. 2004;79(2): 145–158. [DOI] [PubMed] [Google Scholar]
- 20.Carter JD, Mulder RT, Darlow BA. Parental stress in the NICU: The influence of personality, psychological, pregnancy and family factors. Personal Ment Health. 2007;1(1):40–50. [Google Scholar]
- 21.Feldman R, Eidelman AI, Rotenberg N. Parenting stress, infant emotion regulation, maternal sensitivity, and the cognitive development of triplets: A model for parent and child influences in a unique ecology. Child Dev. 2004;75(6):1774–1791. [DOI] [PubMed] [Google Scholar]
- 22.Bayley N Bayley Scales of Infant and Toddler Development® 3rd Edition (Bayley-III®). Psychol Corp San Antonio TX. 2006. [Google Scholar]
- 23.Woodward LJ, Clark CA, Bora S, Inder TE. Neonatal white matter abnormalities an important predictor of neurocognitive outcome for very preterm children. PloS One. 2012;7(12):e51879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–786. [DOI] [PubMed] [Google Scholar]
- 25.Beck AT, Steer RA, Brown GK. BDI-II, Beck Depression Inventory: Manual. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 26.Miles MS, Funk SG, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993;42(3):148–152. [PubMed] [Google Scholar]
- 27.Lean RE, Paul RA, Smyser CD, Rogers CE. Maternal intelligence quotient (iq) predicts Iq and language in very preterm children at age 5 years. J Child Psychol Psychiatry. 2018;59(2):150–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wechsler D Wechsler Preschool and Primary Scale of Intelligence. 3rd ed. San Antonio, TX:The Psychological Corporation;2004. [Google Scholar]
- 29.Wechsler D Wechsler Test of Adult Reading. San Antonio, TX:The Psychological Corporation;2001. [Google Scholar]
- 30.Belsky J, Crnic K, Gable S. The determinants of coparenting in families with toddler boys: Spousal differences and daily hassles. Child Dev. 1995;66:629–642. [PubMed] [Google Scholar]
- 31.Ciciolla L, Crnic KA, West SG. Determinants of change in maternal sensitivity: Contributions of context, temperament, and developmental risk. Parenting. 2013;13(3):178–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fenning RM, Baker JK, Baker BL, Crnic KA. Parenting children with borerline intellectual functioning: A unique risk population. Am J Ment Retard. 2007;112:107–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Norona AN, Baker BL. The effects of early positive parenting and developmental delay status on child emotion dysregulation: Parenting, delay status and emotion regulation. J Intellect Disabil Res. 2017;61(2):130–143. [DOI] [PubMed] [Google Scholar]
- 34.NICHD Early Child Care Research Network. Child care and mother-child interaction in the first three years of life. Dev Psychol. 1999;35(6):1399–1413. [PubMed] [Google Scholar]
- 35.Clark CA, Woodward LJ, Horwood LJ, Moor S. Development of emotional and behavioral regulation in children born extremely preterm and very preterm: Biological and social influences. Child Dev. 2008;79(5):1444–1462. [DOI] [PubMed] [Google Scholar]
- 36.Treyvaud K, Anderson VA, Howard K, et al. Parenting behavior is associated with the early neurobehavioral development of very preterm children. Pediatrics. 2009;123(2):555–561. [DOI] [PubMed] [Google Scholar]
- 37.Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J Educ Behav Stat. 2006;31(4):437–448. [Google Scholar]
- 38.Enders CK. Applied Missing Data Analysis. New York: Guilford Press; 2010. [Google Scholar]
- 39.Martins C, Gaffan EA. Effects of early maternal depression on patterns of infant-mother attachment: A meta-analytic investigation. J Child Psychol Psychiatry. 2000;41(6):737–746. [PubMed] [Google Scholar]
- 40.Campbell SB, Brownell CA, Hungerford A, Spieker SJ, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Dev Psychopathol. 2004;16(02):231–252. [DOI] [PubMed] [Google Scholar]
- 41.Beck CT. Recognizing and screening for postpartum depression in mothers of NICU infants. Adv Neonatal Care. 2003;3(1):37–46. [DOI] [PubMed] [Google Scholar]
- 42.Gillaspy S, Tahirkheli N, Cherry A, McCaffree MA, Tackett A. Postpartum depression on the neonatal intensive care unit: current perspectives. Int J Womens Health. 2014:975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Poehlmann J, Schwichtenberg AJM, Bolt D, Dilworth-Bart J. Predictors of depressive symptom trajectories in mothers of preterm or low birth weight infants. J Fam Psychol. 2009;23(5):690–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.van der Waerden J, Galéra C, Larroque B, Saurel-Cubizolles M-J, Sutter-Dallay A-L, Melchior M. Maternal depression trajectories and children’s behavior at age 5 years. J Pediatr. 2015;166(6):1440–1448.e1. [DOI] [PubMed] [Google Scholar]
- 45.Parent Treyvaud K. and family outcomes following very preterm or very low birth weight birth: a review. Semin Fetal Neonatal Med. 2014;19:131–135. [DOI] [PubMed] [Google Scholar]
- 46.Miles MS, Holditch-Davis D, Thoyre S, Beeber L. Rural African-American mothers parenting prematurely born infants: An ecological systems perspective. Newborn Infant Nurs Rev. 2005;5(3):142–148. [Google Scholar]
- 47.Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a head start population. J Clin Child Adolesc Psychol. 2002;31(3):384–392. [DOI] [PubMed] [Google Scholar]
- 48.Matricardi S, Agostino R, Fedeli C, Montirosso R. Mothers are not fathers: differences between parents in the reduction of stress levels after a parental intervention in a NICU. Acta Paediatr. 2013;102(1):8–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.