Abstract
Background:
The keystone perforator island flap provides a versatile form of reconstruction. Perceived benefits include better donor-recipient color match, less contour defect, and fewer complications. To date, there has been no high-quality evidence comparing keystone flaps to split-thickness skin grafts (SSG) from both a qualitative and quantitative point of view.
Methods:
The Objective and Patient Reported Assessments of Skin grafts versus Keystone flap cohort study compares keystone flaps with SSGs for the reconstruction of skin cancer defects. Patient-reported outcome measures were collected using the EuroQol 5 dimension scale and Patient and Observer Scar Assessment Scale (POSAS) questionnaires. Objective assessments of skin quality were assessed with the Courage and Khazaka system. Cost analysis was also performed.
Results:
Thirty-eight patients were studied: 20 keystone flaps and 18 SSGs. The keystone group had higher EuroQol 5 dimension scale scores (keystone median = 1.0; SSG median = 0.832; P = 0.641) indicating better general quality of life and lower POSAS scores indicating better disease/condition specific quality of life (keystone mean = 27.7; SSG mean = 35.7; P = 0.323). Observer POSAS scores were significantly lower in the keystone group compared with the SSG group (keystone mean = 10.889; SSG mean = 17.313; P < 0.001). Preservation of sensation was significantly better in keystone flaps (P = 0.006). There was an average £158/$207 (15%) saving when performing a keystone flap.
Conclusion:
This pilot study demonstrates a number of possible benefits of keystone flaps over SSGs. The results demonstrate the need for further research comparing these reconstructive options. We propose a prospective, controlled study using the methods developed in this pilot study.
INTRODUCTION
The keystone perforator island flap, adapted from the Bezier flap,1 was described2 and popularized by Behan et al.3 It is a local, type A fasciocutaneous advancement flap, consisting of 2 V to Y advancements, with a blood supply based on random perforating vessels (Fig. 1).4 Since the introduction of the keystone flap, 4 subtypes have been described, mainly based on the size of the defect and the extent of flap dissection (Table 1).5 The keystone flap has been demonstrated to be a versatile form of head and neck,6–9 nasal,10 lower limb,11,12 periarticular,5 and postburn excision reconstruction.13
Fig. 1.
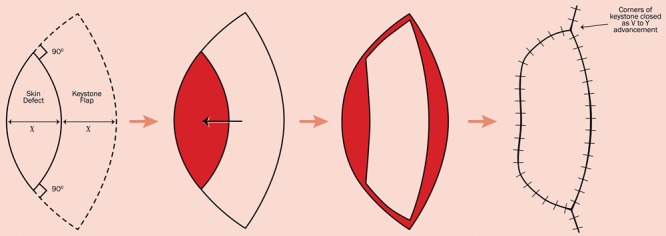
Design of a keystone fasciocutaneous advancement flap.
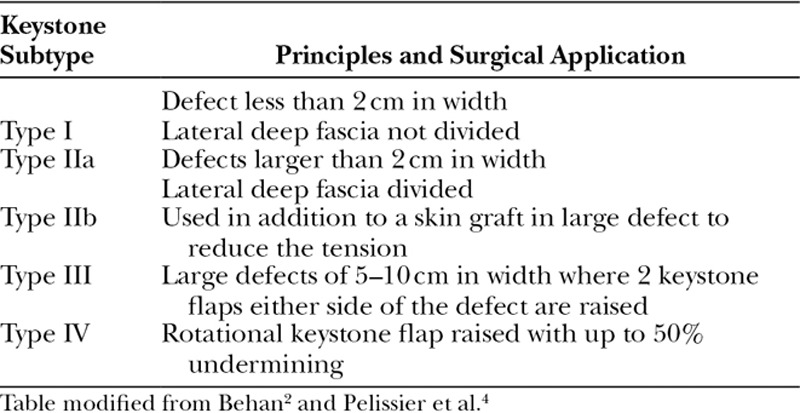
Table 1.
Four Subtypes of the Keystone Flap Are Described Although Type I and IIa Are the Most Commonly Used
In our opinion, the advantages of the keystone flap over split-thickness skin grafts (SSG) are clear: a better donor-recipient color match, less contour defect (Fig. 2), more supple and robust soft tissue coverage, no donor-site morbidity, lower complication rate, and simplified recovery. Qualitative and quantitative assessments of these advantages are undocumented in the literature, aside from complication rates, with the largest study to date of 176 patients indicating only 4.6% of all keystone flaps sustained a complication requiring therapeutic intervention,14 compared with a reported failure rate of SSGs in the lower limb as high as 66%.15
Fig. 2.
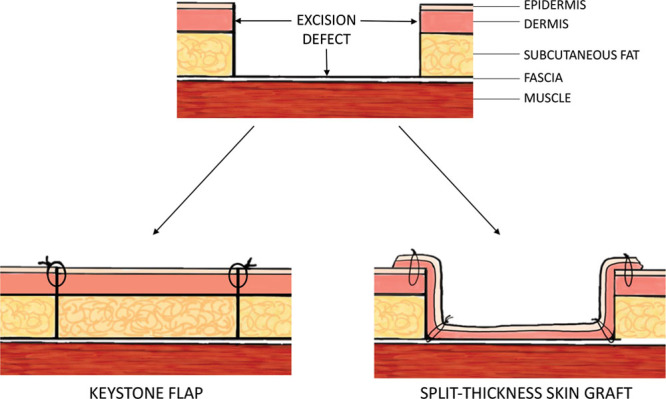
Schematic demonstrating the difference in contour and tissue quality between a keystone flap and a split thickness skin graft.
To our knowledge, there have been no studies comparing the results of keystone flap reconstruction to SSGs. In the era of joint patient-clinician decision-making, it is of benefit to the plastic surgery community to have objective and patient-reported outcome data available to support decision-making processes. We present the Objective and Patient Reported Assessments of Skin grafts versus Keystone flaps (OPRASK) study, providing evidence to support clinical decision-making and a study protocol for further, large-scale assessment of these 2 reconstructive options.
STUDY OBJECTIVES
Primary Objective
To determine if there is a difference in POSAS and EuroQol 5 dimension scale (EQ-5D-5L) scores between keystone flaps and SSGs for the closure of postskin cancer excision defects.
Secondary Objectives
To determine if there is objective evidence to suggest that there is a difference in the outcome between keystone flaps and SSGs for postskin cancer excision defects.
To examine the health economic costs associated with keystone flaps and SSGs.
Methods
The OPRASK study is a retrospective cohort study comparing a group of patients who have undergone keystone flap reconstruction with a group who have received an SSG for closure of a postskin cancer resection defect. The study protocol was reviewed by the Joint Study Review Committee at Swansea University and received ethical approval from the East of England – Cambridgeshire and Hertfordshire Research Ethics Committee (REC number 230581). Patient data were pseudo-anonymized using a unique identifier and managed in accordance with the Data Protection Act 1998 and the 2018 General Data Protection Regulations. The principles of the Declaration of Helsinki were followed at all times.
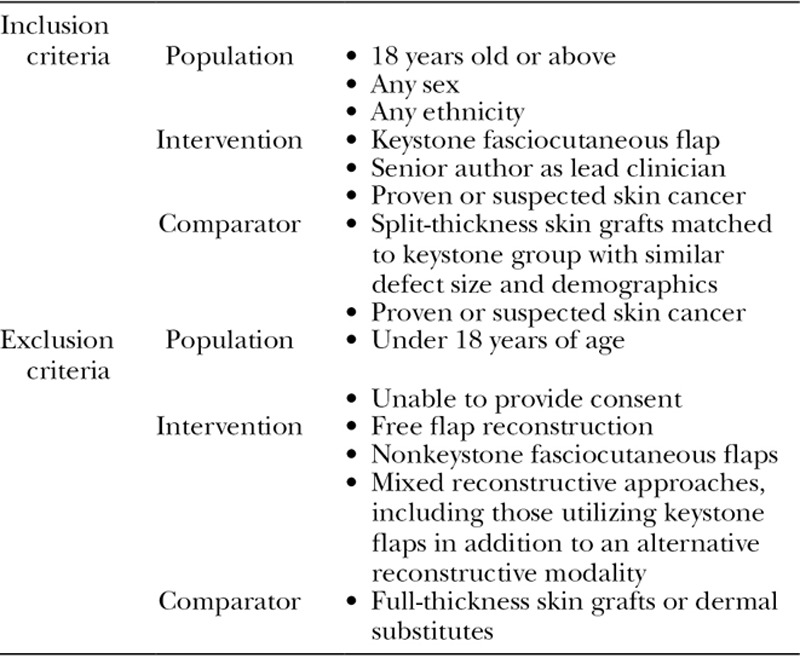
Patient Identification and Inclusion
Electronic patient records, operation logs and electronic photographs of patients under the care of the senior author (I.S.W.) were used to identify patients who had undergone keystone flap reconstruction. A case-matched cohort of SSGs was identified taking into account age, sex, body site, and defect size. Inclusion and exclusion criteria are documented in Table 2.
Table 2.
Predefined Inclusion and Exclusion Criteria for the OPRASK Study
Patient-reported Outcome Measures
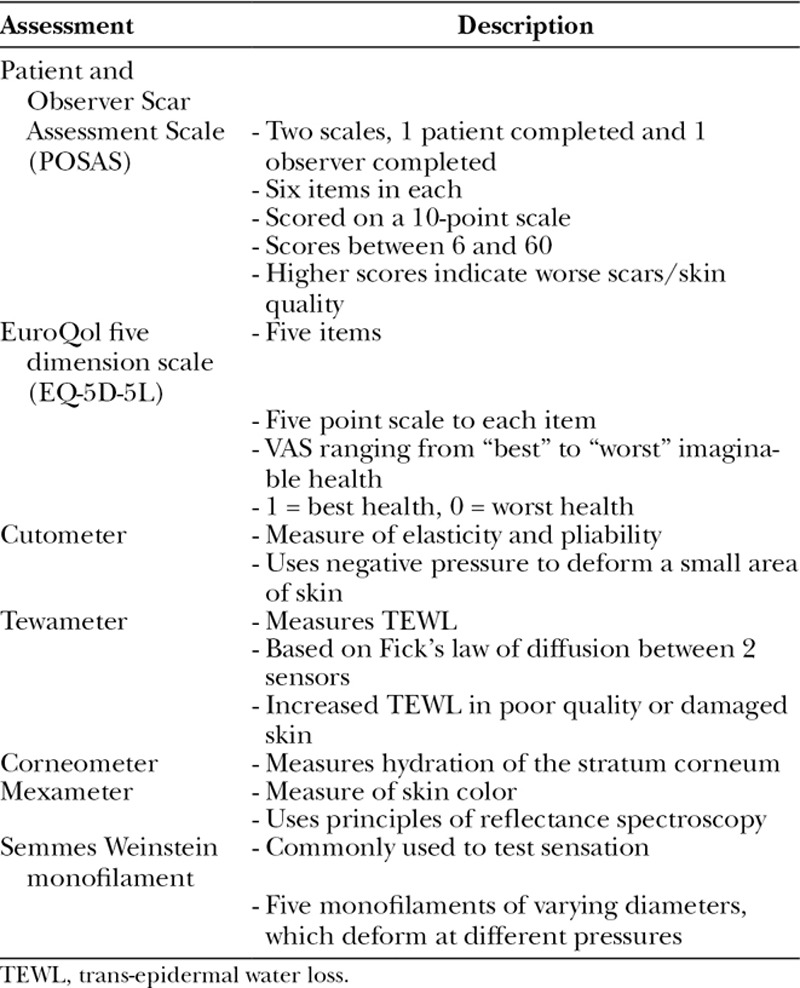
Patient-reported outcome measures (PROMs) are completed by patients to capture one or more aspects of their health and wellbeing, typically taking the form of standardized and validated questionnaires.16 They are broadly divided into generic PROMs (those that assess general aspects of health and wellbeing) and site, disease, or condition-specific PROMs (which cover aspects that are specific to that condition or anatomical domain).17 To be meaningfully used, they must be psychometrically robust, as described elsewhere.17,18 As the main aim of this study was to assess the patient perspective of the difference between keystone flaps and SSGs, both generic and condition-specific PROMs were used. To assess scar burden and quality, the scar-specific Patient and Observer Scar Assessment Scale (POSAS)19,20 was used. First presented in 2005 by Draaijers et al.,21 it is the most commonly used scar-specific PROM. It consists of 2 scales, one completed by the patient and the other by an observer, each consisting of 6 items scored on a 10-point scale.22 The patient scale assesses the scar for color, pliability, thickness, itching, pain, and irregularity compared with their normal skin. The observer rating scale consists of 6 items: vascularity, pigmentation, pliability, thickness, relief, and surface area. Total scores range between 6 and 60, with 6 being perfectly normal skin and 60 being the worst imaginable scar. The POSAS has been well validated in burns scars21,23 and linear scars22 making it well suited for application in this study.
The EQ-5D-5L, a simple generic measure of health status, is the most widely used generic PROM internationally,24 is recommend by The National Institute for Health and Care Excellence25 and used extensively in the National Health Service PROM program in the United Kingdom.16 It consists of 5 descriptive dimensions, covering mobility, self-care, usual activity, pain/discomfort, and anxiety/depression along with a 100 mm visual analog scale (VAS) ranging from “best imaginable health” to “worst imaginable health.” The EQ-5D-5L has a 5-level response category for each item, resulting in a 5-digit code. This is converted to an index value using an anchor-based scale in which 1 represents full health and 0 a state equivalent to being dead.26
Objective Assessment
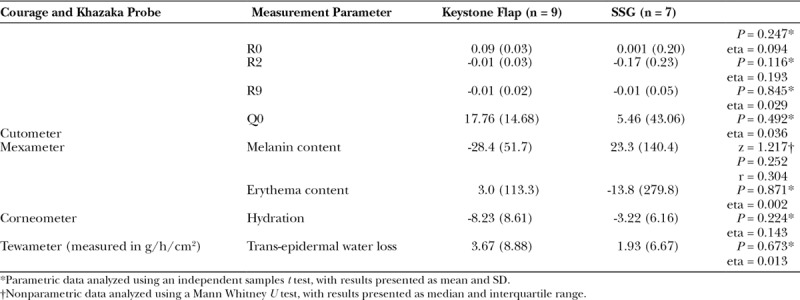
In addition to collecting PROM data, objective measures of skin quality were also recorded. The Courage and Khazaka system (Courage and Khazaka GmbH, Cologne, Germany)27 was used to investigate the elasticity, pliability, color, moisture level, and trans-epidermal water loss of the skin of the reconstructions.
Elasticity and pliability were measured using the reliable and sensitive Cutometer MPA 580 probe,28,29 which contained a 6 mm aperture into which the skin was drawn using 450 mbar of negative pressure.30 The software shipped with the Cutometer calculates a number of parameters based on the deformation curves generated as a result of the negative pressure. The R0 and Q0 parameters, both of which demonstrate firmness, the R2 parameter, which demonstrates elasticity and the R9 parameter indicating the tiring effect of the skin over multiple measurements, were all reported.
Trans-epidermal water loss was measured using the Tewameter TM30031 probe, a commonly used device in the literature for both normal and scarred skin.32,33 Hydration of the stratum corneum was measured using the Corneometer CM 825 probe.34,35 Skin color was measured with the Mexameter MX 18 using principles of reflectance spectroscopy.28,36 To complete a comprehensive quantitative assessment, skin sensation was assessed using the Semmes Weinstein monofilament test37 (Table 3).
Table 3.
Summary of Patient-reported and Objective Measurements Used in the OPRASK Study
Study Procedure
All patients meeting the inclusion criteria were invited to participate in the study via a comprehensive letter and information pack, followed-up with a second letter and phone call as required. Patients were invited to attend one of 3 study days; however, if they were unable to attend they could complete a questionnaire pack (containing the POSAS and EQ-5D-5L) and return this by post. All patients gave written consent and travel expenses were reimbursed for those attending a study clinic.
At study clinics, each patient rotated through 3 stations, completing the POSAS and EQ-5D-5L and undergoing testing with the Semmes Weinstein monofilament and the Courage and Khazaka equipment. Room temperature, humidity, and ambient light conditions were consistent throughout the study. Objective investigations were conducted at least 10 minutes after the patient arrived, allowing skin blood flow to return to normal following exertion. Each objective assessment was repeated 5 times, from both the keystone flap/SSG and a corresponding area of normal skin on the contralateral side. Average results from the abnormal side were subtracted from the normal side in the final analysis such that each patient acted as their own internal control. The observer section of the POSAS was completed by 2 independent clinicians (T.D. and A.K.), and the average score used to reduce the risk of bias. Clinical notes were interrogated for basic demographic data, details regarding lesion size and type, type of reconstruction, and the postoperative course including recurrence and complications. To calculate follow-up duration, the point at which they attended a study clinic or completed the questionnaire pack was used as the most recent data and the difference between this and their operation date used.
Statistical Analysis
Total scores were calculated for POSAS and EQ-5D-5L according to the developer’s guidelines. Missing data were handled by 2 approaches. Any questionnaires with more than 50% missing data were excluded from the analysis. For data where repeat measures were taken (objective skin measurements), if greater than 60% of the repeats were recorded, the mean of these were calculated and used to replace the missing data. This method is used throughout the statistical literature, although others exist.38 If less than 60% of the data were available, all data for this measurement property were excluded.
Patient numbers were limited by the cohort size. A post hoc power calculation using the number recruited, POSAS score effect size and, α = 0.05, demonstrated power of 0.32 (G*Power V3.1).
All data were collated in Excel (Microsoft, Redmond, Wash.) and analyzed in SPSS V.22 (IBM Analytics, N.Y.). Tests for normality were performed, with normally distributed data compared using parametric analysis [data presented as mean (M) ± SD] and skewed data analyzed with nonparametric tests [data presented as median (Md) ± interquartile range (IQR)]. Significance was taken as P < 0.05.
RESULTS
Thirty-eight patients responded to the invitation and agreed to be enrolled, with 17 attending a study clinic and 21 returning the questionnaire pack only (Fig. 3). Baseline characteristics can be seen in Table 4. The average patient age and length of follow-up were significantly lower in the keystone compared with the SSG group (t test; P = 0.001), but sex was evenly distributed in both groups (chi-square; P = 1.000). Defect size did not significantly differ between groups (Mann Whitney U test; P = 0.264). Figures 4 and 5 demonstrate an example of a keystone flap from the cohort studied.
Fig. 3.
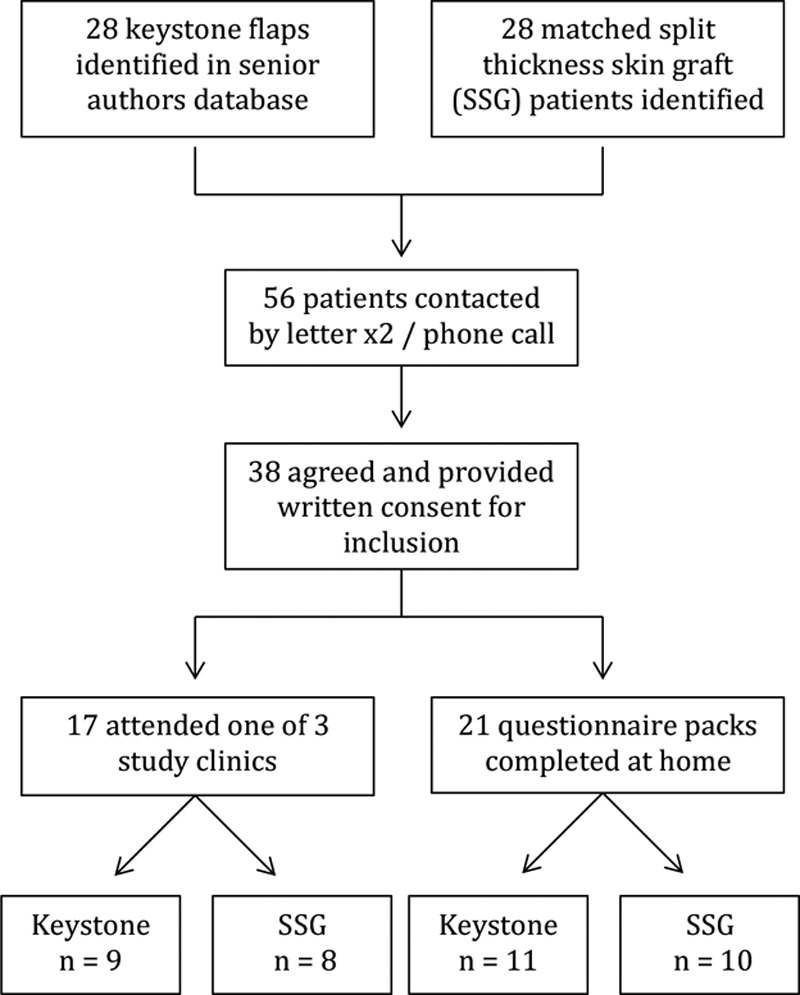
Study flow diagram demonstrating recruitment to the OPRASK study.
Table 4.
Baseline Characteristics of Patients Included in the Study
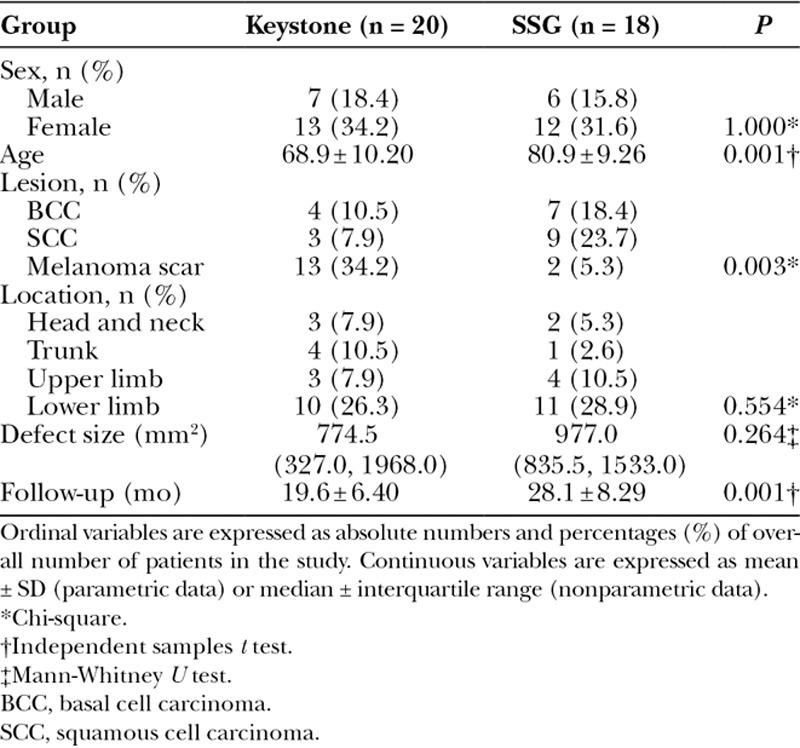
Fig. 4.
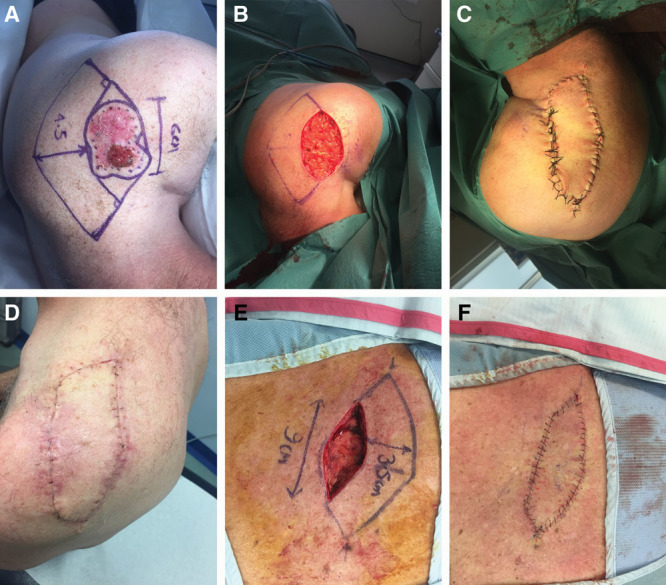
Examples of 2 keystone perforator flaps used to reconstruct large defects that would not closure primarily and would otherwise require an SSG. A, B, C, D – Left shoulder. A, Preoperative lesion and keystone flap markings. B, Defect following lesion excision. C, Inset of keystone flap at end of procedure. D, Postoperative follow-up at 2 weeks. E, F, Right upper back. E, Intraoperative image showing excision of lesion and resulting defect. F, Inset of keystone flap at end of procedure.
Fig. 5.

Postoperative follow-up at 4 weeks.
Patient-reported Data
Anchored index scores for EQ-5D-5L were calculated for each patient. The median score in the keystone flap group was 1.0 (IQR = 0.4) versus 0.8 (IQR = 0.3) in the SSG group. A lower score represents a worse level of health and thus there is a trend toward the SSG group having a lower overall quality of life. This difference was, however, not significant (Mann Whitney U test, z = -0.51; P = 0.641; r = 0.08).
To investigate if age plays a role in EQ-5D-5L scores, a one-way analysis of covariance was performed. After adjusting for age, no significant difference was demonstrated between the EQ-5D-5L scores in either procedural group (F = 0.47; P = 0.498). Partial eta squared for the covariant was 0.077, suggesting a small effect size and that only 7.7% of the variance in the EQ-5D-5L score is explained by age.
No significant difference in VAS was demonstrated between those who underwent a keystone flap (M = 81.8; SD = 15.3) and those who underwent an SSG (M = 77.7; SD = 17.4; P = 0.455, two-tailed). There is, however, a trend toward a higher VAS in the keystone group, suggesting a greater quality of life as seen in the index values.
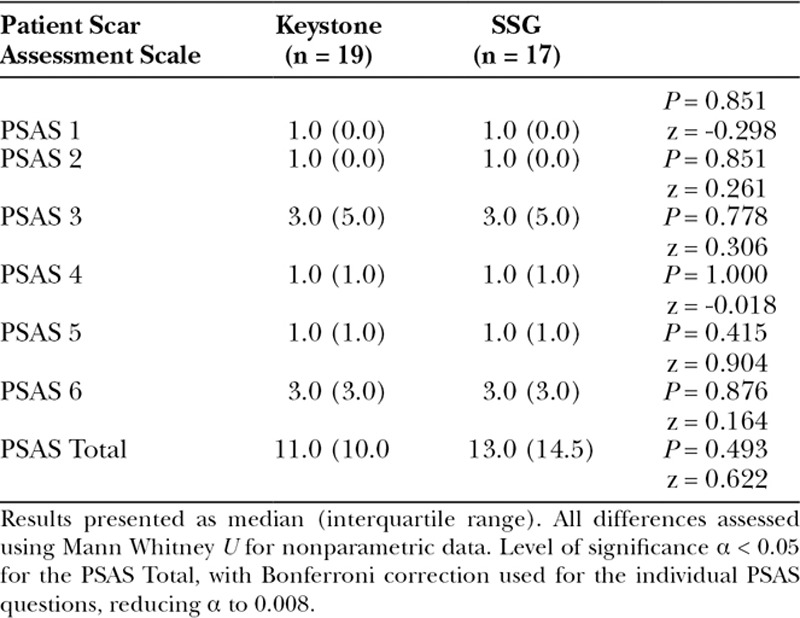
Table 5 shows Patient Scar Assessment Scale (PSAS) results. A Bonferroni correction was applied to the alpha value for between-group analysis of the individual PSAS scores to reduce the risk of a type 1 error, giving an alpha of 0.008 for significance. The median total PSAS score for the keystone flap group was 11 (IQR, 10) and 13 (IQR, 14.5) for the SSG group. This was nonsignificant (Mann Whitney U test, z = 0.493; P = 0.622; r = 0.08). Questions relating to scar color (PSAS 3) and scar irregularity (PSAS 6) showed the highest median values, indicating worse results.
Table 5.
Scores for the Patient-reported Component of the POSAS for the Keystone Flap and SSG Groups
A significant difference between the observer POSAS scores for the keystone flap group (M = 10.9; SD = 2.4) and the SSG group (M= 17.3; SD = 3.1; P < 0.001, independent samples t test) was observed (Fig. 6).
Fig. 6.
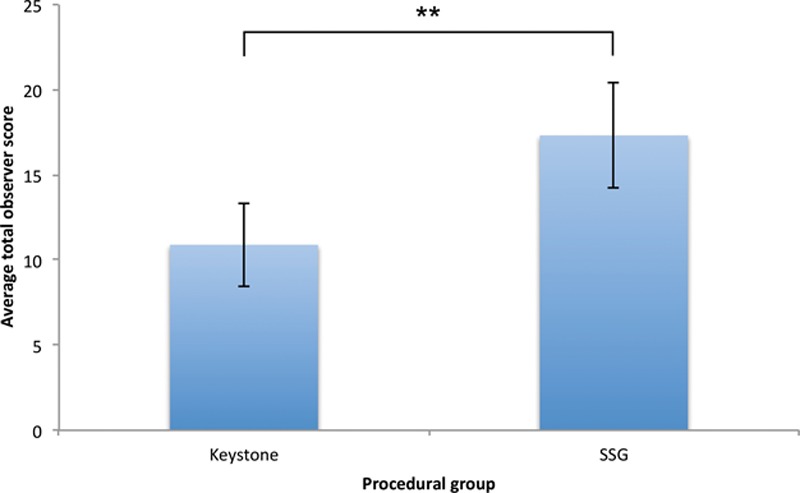
Mean score for the observer component of the POSAS questionnaire in the keystone flap and SSG groups. The mean score is the average score for each group taken from the average of 2 independent researchers scoring each patient. SD is demonstrated. Independent samples t test was used to compare means with P < 0.001.
Total POSAS scores were calculated (sum total of PSAS and OSAS scores). These were lower in the keystone group (M = 27.7; SD = 16.8) than the SSG group (M = 35.7; SD = 14.3), suggesting that keystones are more comparable to normal skin to both patients and clinical observers. This was, however, nonsignificantly different (P = 0.323; eta square = 0.08; independent samples t test).
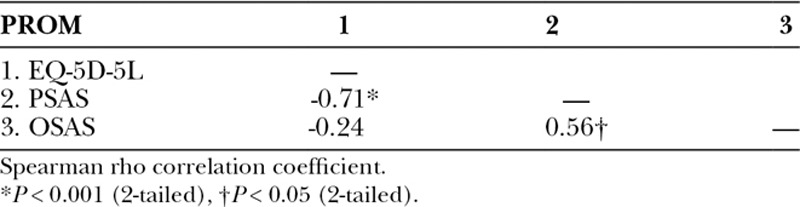
Table 6 demonstrates the results of correlation testing between the total PSAS score, the average total OSAS score, and the EQ-5D-5L. It was hypothesized that both patients and clinicians would have similar views with regard to the outcome of surgery and that the EQ-5D-5L would have a negative correlation with POSAS scores (lower POSAS scores and higher EQ-5D-5L scores both indicate ‘better’ scar or general quality of life, respectively). A between-group analysis was also performed, investigating the relationship between PSAS and OSAS in the keystone flap and SSG groups. Both groups showed a large positive correlation between PSAS and OSAS, although this did not reach the level of significance (keystone; rho = 0.52; confidence interval = 0.08–0.79; P = 0.192 and SSG; rho = 0.52; confidence interval = 0.05–0.80; P = 0.188).
Table 6.
Correlation between the Total PSAS, Average Total OSAS, and EQ-5D-5L Scores
Objective Data
In assessing sensation between the nonoperated side and the operated side, the data were split into those people in each procedural group (keystone flap or SSG) that did or did not have a change in the categorical score on the Semmes Weinstein monofilament test between their normal and abnormal sides. This generated 4 categories (keystone – Yes, keystone – No, SSG – Yes, SSG – No), which were compared in a two-by-two table using the Pearson chi-square test (Table 7). Significantly fewer people in the keystone group experienced a reduction in sensation compared with their normal side, indicating a strong association between the type of procedure and the reduction in sensation compared with the normal side (chi-square = 7.61; P = 0.006; phi = -0.79).
Table 7.
Comparison of Changes in Sensation on the Semmes Weinstein Monofilament Test between the Normal and Abnormal Sides in Those Undergoing Keystone Flap or Split-thickness Skin Graft Reconstruction
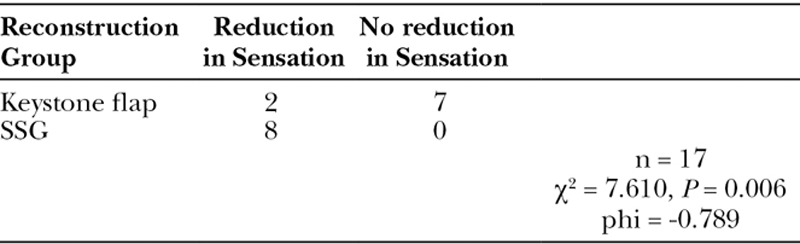
Table 8 shows the results of the Courage and Khazaka data. No significant difference between keystone flaps and SSGs were demonstrated in any of the objective parameters measured. There was, however, a trend toward SSGs being firmer that keystone flaps (keystone Q0 = 17.8 versus SSG Q0 = 5.5). Furthermore, both demonstrated a reduction in their trans-epidermal water loss, but an increase in hydration in the stratum corneum.
Table 8.
Data from the Cutometer, Mexameter, Corneometer, and Tewameter Compared between the Keystone Flap Group and SSG
Complications
There were 2 complications in the keystone group (10%) and 7 in the SSG group (39%). There was 1 infection in the keystone group, successfully treated with oral antibiotics and 1 hypertrophic scar. In the SSG group, 2 people developed infections, with 1 graft overgranulated and 4 grafts partially or completely failed.
Excision Rate and Detection of Recurrence
One lesion was incompletely excised in the SSG group, with no incompletely excised lesions in the keystone group. There was 1 recurrence in the SSG group and none in the keystone group. A Fisher’s exact test was used to examine this relationship between these results and the type of reconstruction, with no evidence of a relationship (P = 0.474, respectively).
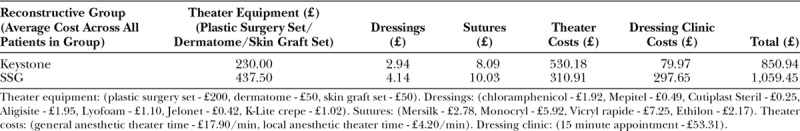
Cost Analysis of Keystone Flaps and Split-thickness Skin Grafts
Costs were calculated to include time in theater, type and amount of anesthetic, equipment used, sutures, dressings, and follow-up appointments in the dressing clinic until the wound was healed (defined as the point where the wound could be managed without dressings at home by the patient which equated to a mean of 1.5 weeks for a keystone flap and 5.6 weeks for an SSG; Table 9). There was an average cost saving of £208/$268 (19.7%) in the keystone flap group versus the split-thickness skin graft (keystone flap = £850.94; SSG = £1059.45; P = 0.389, independent samples t test).
Table 9.
Costs Used to Calculate the Average Cost of Providing a Keystone Flap or Split-thickness Skin Graft from the Point of Procedure to a Healed Wound
DISCUSSION
The benefits of the keystone flap have been well documented for the reconstruction of defects in range of topographical areas,5–7,9,11–13 although there is little objective or patient-reported outcome data comparing them to SSGs. This study aimed to generate pilot data to address this. Key outcomes are documented in Table 10.
Table 10.
Key Study Outcomes
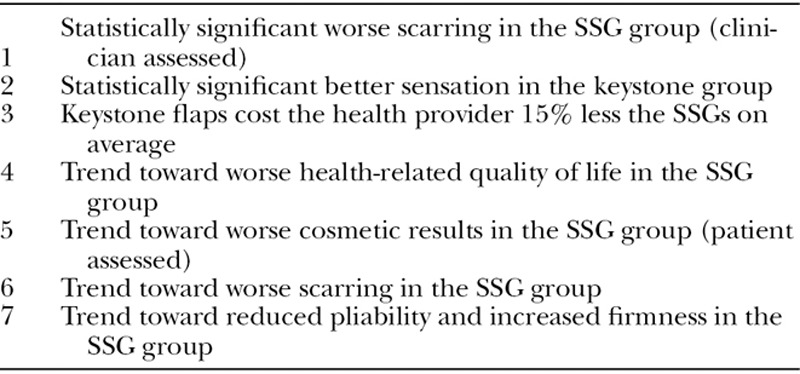
There was a trend toward an inferior quality of life in the SSG group versus the keystone flap group, with lower median scores in both the EQ-5D-5L and EQ-5D-5L VAS in the SSG group. It is of note that only 7.7% of the variance in EQ-5D-5L score was ascribed to age.
It was hypothesized that the POSAS would provide a greater ability to differentiate between reconstruction type, given its focus on scarring. Again there was a trend toward “worse” scarring in the SSG group, reflected by a higher median total patient component of the POSAS. Scar color and irregularity showed the greatest difference between the operated side and the normal skin from a patient perspective. Although the EQ-5D-5L and POSAS scores all showed a trend toward worse results for the SSGs versus the keystone flaps, statistical significance was not achieved.
For the clinical observer, our results show that statistically, the keystone flap is aesthetically and functionally preferable, with the observer component of the POSAS demonstrating a significantly lower score in the keystone group.
Significantly, fewer people in the keystone group experienced a reduction in sensation compared with the normal side and there was a trend toward keystone flaps being firmer than SSGs. These findings are important as a lack of protective sensation and thinner, less robust soft-tissue coverage, may result in acute injury or wound breakdown from frictional forces or direct trauma.
Cost analysis demonstrated that the average keystone flap costs £158 ($207) less than an SSG (a 15% saving). In an era of prudent healthcare, a reliance on rationing of healthcare resources and the growing incidence of skin cancer, there is a large health economic benefit to consider.
Although subjective and quantitative data suggest a trend toward better overall outcomes with a keystone flap versus SSGs, the lack of statistical significance is likely due to a number of factors. The low power, due to a modest cohort size and the need for nonparametric statistical analysis, makes it difficult for the results to reach significance. It is also likely that our patient population, generally elderly, with a significant number living in a semirural setting, suffering from cancer, is not overly concerned by the aesthetic or functional outcome of their reconstruction. This is suggested by the majority of patients scoring the lowest category possible (1 out of 10) for a large number of the PSAS questions. It is likely that this age group is less concerned with the factors asked in the POSAS questionnaire than younger patients might be. It is our belief that in a younger population, living in major cities, with higher expectations, that these results would be different. We also note a significant difference in the average age between both groups. This is likely to represent unconscious bias on the part of the clinical team when recommending different treatment options and is something to address in a future, prospective study.
Despite being a small cohort it is important to note that no keystone flaps failed, whereas 4 SSGs experienced either partial or complete loss. This lower complication rate is an important finding and one that should be discussed with patients.
Trends identified suggest that a fully powered, prospectively collected data set is warranted. Both EQ-5D-5L and POSAS questionnaires functioned well and were easy to administer. Similarly, sensation was easy to measure and provided useful information. We, however, feel that the collection of objective data using the Courage and Khazaka adds considerably to the cost and complexity of the study without significant benefits and as such would suggest this is not included in future protocols.
CONCLUSIONS
The limited cohort size available in this retrospective study limited its statistically power and the conclusions that can be drawn. However, a trend toward greater patient satisfaction, better appearance, and cost savings to the health provider of keystone flaps over SSGs was seen. The development of a larger, prospectively designed trial is now required to fully evaluate the difference and provide evidence-based treatment that is preferential to our patient population.
ACKNOWLEDGMENTS
The authors would like to acknowledge the support of Enviroderm, (the UK supplier of Courage and Khazaka equipment) and Steve Atherton for Figure 1.
Footnotes
Published online 16 November 2018.
Supported by The Royal College of Surgeons England Pump Priming Grant (I.S.W.). Royal College of Surgeons of England Research Fellowship (T.J.), Welsh Clinical Academic Training Fellowship (T.D., T.J., Z.J.), MRC Clinical Research Training Fellowship (Z.J.), AMBU Pathway to Portfolio Grant (I.S.W., T.D., T.J.).
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by an AMBU Pathway to Portfolio Grant.
REFERENCES
- 1.Behan FC, Terrill PJ, Breidahl A, et al. Island flaps including the Bezier type in the treatment of malignant melanoma. Aust N Z J Surg. 1995;65:870. [DOI] [PubMed] [Google Scholar]
- 2.Behan FC. The keystone design perforator island flap in reconstructive surgery. ANZ J Surg. 2003;73:112. [DOI] [PubMed] [Google Scholar]
- 3.Behan F, Findlay M, Cheng L. The Keystone Perforator Island Flap Concept. 2012Elsevier Australia. [Google Scholar]
- 4.Pelissier P, Santoul M, Pinsolle V, et al. The keystone design perforator island flap. Part I: anatomic study. J Plast Reconstr Aesthet Surg. 2007;60:883. [DOI] [PubMed] [Google Scholar]
- 5.Jovic TH, Jessop ZM, Slade R, et al. The use of keystone flaps in periarticular wound closure: a case series. Front Surg. 2017;4:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun Y. Keystone flap for large posterior neck defect. Indian J Surg. 2016;78:321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Behan FC, Lo CH, Sizeland A, et al. Keystone island flap reconstruction of parotid defects. Plast Reconstr Surg. 2012;130:36e. [DOI] [PubMed] [Google Scholar]
- 8.Behan FC, Rozen WM, Wilson J, et al. The cervico-submental keystone island flap for locoregional head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2013;66:23. [DOI] [PubMed] [Google Scholar]
- 9.Loh IW, Rozen WM, Behan FC, et al. Eyelid reconstruction: expanding the applications of the keystone perforator island flap concept. ANZ J Surg. 2012;82:763. [DOI] [PubMed] [Google Scholar]
- 10.Kostopoulos E, Casoli V, Agiannidis C, et al. The keystone perforator island flap in nasal reconstruction: an alternative reconstructive option for soft tissue defects up to 2 cm. J Craniofac Surg. 2015;26:1374. [DOI] [PubMed] [Google Scholar]
- 11.Martinez JC, Cook JL, Otley C. The keystone fasciocutaneous flap in the reconstruction of lower extremity wounds. Dermatol Surg. 2012;38:484. [DOI] [PubMed] [Google Scholar]
- 12.Huang J, Yu N, Long X, et al. A systematic review of the keystone design perforator island flap in lower extremity defects. Medicine (Baltimore). 2017;96:e6842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Busaidi AA, Semalesan N, Al-Busaidi SS. Keystone design sliding skin flap for the management of small full thickness burns. Sultan Qaboos Univ Med J. 2011;11:412. [PMC free article] [PubMed] [Google Scholar]
- 14.Moncrieff MD, Bowen F, Thompson JF, et al. Keystone flap reconstruction of primary melanoma excision defects of the leg-the end of the skin graft? Ann Surg Oncol. 2008;15:2867. [DOI] [PubMed] [Google Scholar]
- 15.Stankiewicz M, Coyer F, Webster J, et al. Incidence and predictors of lower limb split-skin graft failure and primary closure dehiscence in day-case surgical patients. Dermatol Surg. 2015;41:775. [DOI] [PubMed] [Google Scholar]
- 16.Devlin NJ, Appleby J. Getting the most out of PROMS. Putting Health Outcomes at the Heart of NHS Decision-making. The King’s Fund. London: 2010. [Google Scholar]
- 17.Wormald JCR, Rodrigues JN. Outcome measurement in plastic surgery. J Plast Reconstr Aesthet Surg. 2018;71:283. [DOI] [PubMed] [Google Scholar]
- 18.Dobbs TD, Hughes S, Mowbray N, et al. How to decide which patient-reported outcome measure to use? A practical guide for plastic surgeons. J Plast Reconstr Aesthet Surg. 2018;71:957. [DOI] [PubMed] [Google Scholar]
- 19.Vercelli S, Ferriero G, Sartorio F, et al. How to assess postsurgical scars: a review of outcome measures. Disabil Rehabil. 2009;31:2055. [DOI] [PubMed] [Google Scholar]
- 20.Seong Hwan Bae YCB. Analysis of frequency of use of different scar assessment scales based on the scar condition and treatment method. Arch Plast Surg. 2014;41:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Draaijers LJ, Tempelman FR, Botman YA, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113:1960. [DOI] [PubMed] [Google Scholar]
- 22.van de Kar AL, Corion LUM, Smeulders MJC, et al. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116:514. [DOI] [PubMed] [Google Scholar]
- 23.van der Wal MB, Tuinebreijer WE, Bloemen MC, et al. Rasch analysis of the Patient and Observer Scar Assessment Scale (POSAS) in burn scars. Qual Life Res. 2012;21:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Devlin NJ, Brooks R. EQ-5D and the EuroQol group: past, present and future. Appl Health Econ Health Policy. 2017;15:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institute for Health and Care Excellence. Guide to the Methods of Technology Appraisal 2013. 2013London, United Kingdom: National Institute for Health and Care Excellence (NICE). [PubMed] [Google Scholar]
- 26.Devlin NJ, Shah KK, Feng Y, et al. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ. 2018;27:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hua W, Xie H, Chen T, et al. Comparison of two series of non-invasive instruments used for the skin physiological properties measurements: the ‘Soft Plus’ from Callegari S.p.A vs. the series of detectors from Courage & Khazaka. Skin Res Technol. 2014;20:74. [DOI] [PubMed] [Google Scholar]
- 28.Nedelec B, Correa JA, Rachelska G, et al. Quantitative measurement of hypertrophic scar: intrarater reliability, sensitivity, and specificity. J Burn Care Res. 2008;29:489. [DOI] [PubMed] [Google Scholar]
- 29.Draaijers LJ, Botman YA, Tempelman FR, et al. Skin elasticity meter or subjective evaluation in scars: a reliability assessment. Burns. 2004;30:109. [DOI] [PubMed] [Google Scholar]
- 30.Courage and Khazaka electronic GmbH, Cologne, Germany. Information and operating instructions for the CutometeR MPA 580 and the Software CutometeR Mpa Q. 2010. Available at http://www.courage-khazaka.de/index.php/en/. Accessed July 5, 2018.
- 31.Rosado C, Pinto P, Rodrigues LM. Comparative assessment of the performance of two generations of Tewameter: TM210 and TM300. Int J Cosmet Sci. 2005;27:237. [DOI] [PubMed] [Google Scholar]
- 32.Mercurio DG, Segura JH, Demets MB, et al. Clinical scoring and instrumental analysis to evaluate skin types. Clin Exp Dermatol. 2013;38:302. [DOI] [PubMed] [Google Scholar]
- 33.Lee KC, Dretzke J, Grover L, et al. A systematic review of objective burn scar measurements. Burns Trauma. 2016;4:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clarys P, Clijsen R, Taeymans J, et al. Hydration measurements of the stratum corneum: comparison between the capacitance method (digital version of the Corneometer CM 825®) and the impedance method (Skicon-200EX®). Skin Res Technol. 2012;18:316. [DOI] [PubMed] [Google Scholar]
- 35.Anthonissen M, Daly D, Peeters R, et al. Reliability of repeated measurements on post-burn scars with Corneometer CM 825(®). Skin Res Technol. 2015;21:302. [DOI] [PubMed] [Google Scholar]
- 36.van der Wal M, Bloemen M, Verhaegen P, et al. Objective color measurements: clinimetric performance of three devices on normal skin and scar tissue. J Burn Care Res. 2013;34:e187. [DOI] [PubMed] [Google Scholar]
- 37.McGill M, Molyneaux L, Yue DK. Use of the Semmes-Weinstein 5.07/10 gram monofilament: the long and the short of it. Diabet Med. 1998;15:615. [DOI] [PubMed] [Google Scholar]
- 38.Sterne JA, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]


