Abstract
Idiopathic pulmonary fibrosis (IPF) is a lethal fibrotic lung disease with an increasing global burden. It is hypothesized that fibroblasts have a number of functions that may affect the development and progression of IPF. However, the present understanding of cellular and molecular mechanisms associated with fibroblasts in IPF remains limited. The present study aimed to identify the dysregulated genes in IPF fibroblasts, elucidate their functions and explore potential microRNA (miRNA)-mRNA interactions. mRNA and miRNA expression profiles were obtained from IPF fibroblasts and normal lung fibroblasts using a next-generation sequencing platform, and bioinformatic analyses were performed in a step-wise manner. A total of 42 dysregulated genes (>2 fold-change of expression) were identified, of which 5 were verified in the Gene Expression Omnibus (GEO) database analysis, including the upregulation of neurotrimin (NTM), paired box 8 (PAX8) and mesoderm development LRP chaperone, and the downregulation of ITPR interacting domain containing 2 and Inka box actin regulator 2 (INKA2). Previous data indicated that PAX8 and INKA2 serve roles in cell growth, proliferation and survival. Gene Ontology analysis indicated that the most significant function of these 42 dysregulated genes was associated with the composition and function of the extracellular matrix (ECM). A total of 60 dysregulated miRNAs were also identified, and 1,908 targets were predicted by the miRmap database. The integrated analysis of mRNA and miRNA expression data, combined with GEO verification, finally identified Homo sapiens (hsa)-miR-1254-INKA2 and hsa-miR-766-3p-INKA2 as the potential miRNA-mRNA interactions in IPF fibroblasts. In summary, the results of the present study suggest that dysregulation of PAX8, hsa-miR-1254-INKA2 and hsa-miR-766-3p-INKA2 may promote the proliferation and survival of IPF fibroblasts. In the functional analysis of the dysregulated genes, a marked association between fibroblasts and the ECM was identified. These data improve the current understanding of fibroblasts as key cells in the pathogenesis of IPF. As a screening study using bioinformatics approaches, the results of the present study require additional validation.
Keywords: bioinformatics, fibroblasts, idiopathic pulmonary fibrosis, Inka box actin regulator 2, next-generation sequencing, paired box 8
Introduction
Idiopathic pulmonary fibrosis (IPF) is a chronic, progressive, fibrotic lung disease. IPF predominantly affects elderly men. Patients with IPF usually present with exertional dyspnea, dry cough and inspiratory bibasilar Velcro-like crackles on lung auscultation. At present, high-resolution computed tomography is the most important diagnostic tool for IPF, which typically presents with usual interstitial pneumonia pattern (1,2). IPF is a lethal lung disease. The prognosis of IPF is poorer compared with a number of types of cancer (3), with an estimated median survival of 3-5 years if untreated (2). The incidence of IPF, hospitalization rates and mortality due to IPF have increased during previous years, suggesting an increasing global burden of this disease (4-6).
The pathogenesis of IPF remains largely unknown. Data from observational studies suggest that cigarette smoking, air pollution (7), environmental exposure (8), chronic viral infection (9) and esophageal reflux (10) predispose individuals to IPF (4). There is also increasing evidence for genetic predisposition to IPF: Recent genome-wide association studies identified that several genetic variants, primarily involved in epithelial cell-cell adhesion and integrity, the innate immune response, host defense and DNA repair, are associated with increased risk of IPF (11-13). These together indicate that gene-environmental interactions serve important roles in the pathogenesis of IPF. In genetically predisposed individuals, repetitive environmental exposures lead to an aberrant injury-remodeling process (14). Activated lung epithelial cells produce pro-fibrotic growth factors, chemokines and other mediators, resulting in abnormal wound healing characterized by mesenchymal transition of epithelial cells, activation and differentiation of fibroblasts and myofibroblasts. These fibroblasts and myofibroblasts secrete excessive amounts of extracellular matrix proteins including fibrillary collagens, vimentin and fibronectin (15), contributing to the destruction of lung architecture by progressive scarring.
It is hypothesized that fibroblasts have a number of functions that may affect the development and progression of IPF (16). Although previous studies have described the differences between IPF and normal lung fibroblasts (17-21), the knowledge concerning the cellular and molecular mechanisms associated with fibroblasts in IPF remains limited, and their specific roles requires additional investigation (16,22).
For an improved understanding of the roles fibroblasts serve in the pathogenesis of IPF, the present study used a next generation sequencing (NGS) platform and a step-wise bioinformatic approach to analyze the expression levels of mRNAs and microRNAs (miRNAs) and their interactions in IPF fibroblasts compared with normal lung fibroblasts. The aims of the present study were to identify the top differentially expressed genes and subsequently elucidate the function of these dysregulated genes, and to explore potential miRNA-mRNA interactions in IPF fibroblasts.
Materials and methods
Study design
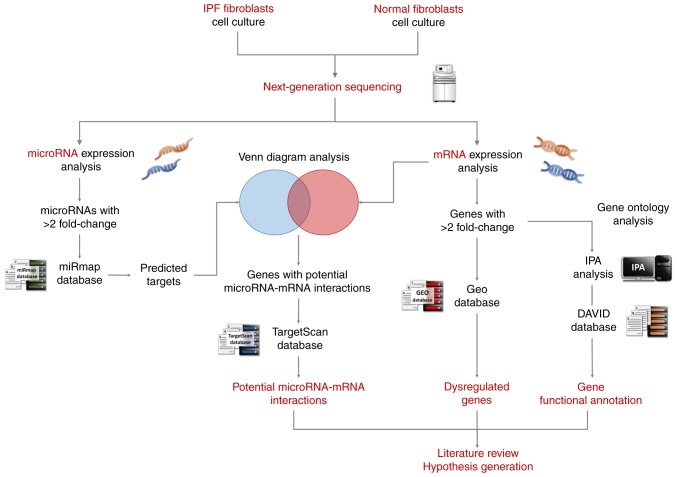
The study design is summarized in Fig. 1. Firstly, cell cultures of the IPF fibroblasts and healthy lung fibroblasts were generated. Then, total RNA of the fibroblasts were extracted and sent for RNA and small RNA sequencing using the NGS platform. The differentially expressed genes (>2 fold-change) were analyzed with Ingenuity® Pathway Analysis (IPA) and the Database for Annotation, Visualization and Integrated Discovery (DAVID) for pathway analysis and functional interpretation. These dysregulated genes were additionally verified in representative Gene Expression Omnibus (GEO) datasets. The differentially expressed miRNAs (>2 fold-change) were analyzed with miRmap (mirmap.ezlab. org) (23) for target prediction. Then, Venn diagrams were used to determine genes with potential miRNA-mRNA interactions. These potential miRNA-mRNA interactions were confirmed using a second miRNA prediction database, TargetScan (www.targetscan.org) (24). Finally, a literature search for the functions of these dysregulated genes was performed, and a hypothesis was generated.
Figure 1.
Schematic illustration of the study design. Following culture of the IPF fibroblasts and healthy lung fibroblasts, the total RNA were extracted and deep sequenced using a next-generation sequencing platform. The differentially expressed genes (>2 fold-change) were identified, and analyzed with IPA and DAVID for pathway analysis and functional interpretation. The GEO IPF databases were analyzed to confirm dysregulated genes identified in the present study. Conversely, the differentially expressed miRNAs (>2 fold-change) were analyzed with miRmap for target prediction. Then, genes with potential miRNA-mRNA interactions were determined by Venn diagram analysis. These miRNA-mRNA interactions were verified by a second miRNA prediction database, TargetScan. Finally, a literature search was performed and a hypothesis was generated. IPF, idiopathic pulmonary fibrosis; IPA, Ingenuity® Pathway Analysis; DAVID, Database for Annotation, Visualization, and Integrated Discovery; GEO, Gene Expression Omnibus.
Culture of primary cells
Diseased human lung fibroblasts (DHLF)-IPF (cat. no. CC-7231) and normal human lung fibroblasts (NHLF; cat. no. CC-2512) were purchased from Lonza Walkersville Inc. (Walkersville, MD, USA). The cells were grown in FGW™-2 Fibroblast Growth Medium-2 Bulletkit™ (Lonza Walkersville Inc.; cat. no. CC-3132), containing 0.5 ml human fibroblast growth factor-basic, 0.5 ml insulin, 10 ml fetal bovine serum and 0.5 ml GA-1000. To avoid losing any original characteristics over multiple generations, the DHLF-IPF and NHLF cells used for the NGS analysis were harvested from the 1st generation of cells following cultivation from the primary cells.
NGS
The expression profiles of miRNAs and mRNAs were examined using NGS. Protocol was described in our previous studies (25-27). In brief, total RNA from the DHLF-IPF and NHLF cells were extracted with TRIzol® reagent (Thermo Fisher Scientific, Inc., Waltham, MA, USA) at Welgene Biotech Co., Ltd. (Taipei, Taiwan). Purified RNA was quantified at an optical density of 260 nm using an ND-1000 spectrophotometer (NanoDrop Technologies; Thermo Fisher Scientific, Inc.) and the RNA quality was examined using a Bioanalyzer 2100 (Agilent Technologies, Inc., Santa Clara, CA, USA) with RNA 6000 LabChip® kit (Agilent Technologies, Inc.). Next, the samples were prepared for library construction and sequencing using an Illumina preparation kit (Illumina, Inc., San Diego, CA, USA). For small RNA sequencing, the harvested cDNA constructs containing 18-40-nucleotide RNA fragments (140-155 nucleotides in length with all adapters) were selected. The libraries were then sequenced on an Illumina instrument (75 single-end cycles). Following trimming and removal of reads with low quality scores using Trimmomatics (28), the qualified reads were analyzed with miRDeep2 (29) and the UCSC Genome Browser (genome.ucsc.edu/) (30). The miRNAs with low levels (<1 normalized read per million) in either DHLF-IPF or NHLF cells were excluded.
For transcriptome sequencing, the library was constructed with a SureSelect Strand Specific RNA Library Preparation kit (Agilent Technologies, Inc.), and sequenced on a Solexa platform (150 paired-end cycles), using the TruSeq SBS kit (Illumina, Inc.). Similar with small RNA sequencing data, Trimmomatics (version 0.36) was implemented to trim or remove the reads with low quality score. Qualified reads were analyzed using HISAT2 (version 2.1.0) (31). The genes with low expression levels [<0.3 fragment per kilobase of transcript per million mapped reads (FPKM)] in either DHLF-IPF or NHLF cells were excluded. The 2-tailed P-values were calculated [2(Cufflinks version 2.2.1)] with non-grouped samples used ‘blind mode’, in which all samples were treated as replicates of a single global ‘condition’ and used to build one model for statistical analysis (32,33). Genes with P<0.05 [(-log10) P-value >1.3] and >2 fold-changes were considered to be significantly dysregulated genes.
miRmap and TargetScan database analysis
miRmap is an open-source software library, which provides comprehensive miRNA-target prediction (23). By calculating the complementary ability of miRNA-mRNA interactions, the putative target genes of each miRNA may be identified. By combining thermodynamic, evolutionary, probabilistic and sequence-based features, the predictor also estimates mRNA-repression strength for ranking potential candidate targets. The prediction produces a list of putative target genes with an miRmap score, a predictive reference value. In the present study, an miRmap score ≥99 was used as the criterion for selecting putative miRNA targets.
TargetScan is an online database for predicting biological targets of miRNAs (24). It searches for the presence of conserved 8, 7 and 6 mer sites, which match the seed region of each miRNA. Predictions are ranked based on the predicted targeting efficacy or the probability of conserved targeting.
IPA
IPA (Qiagen Inc., Valencia, CA, USA) (34) is a web-based software application for the analysis, integration and interpretation of data derived from ‘omics experiments, including RNA sequencing, small RNA sequencing, microarrays, metabolomics and proteomics. IPA enables the rapid understanding and visualization of data, and provides a range of data in addition to pathway analysis, including the identification of key regulators and activity to explain expression patterns, prediction of downstream effects on biological and disease processes, and provision of targeted data on genes, proteins, chemicals and drugs. The dysregulated genes from the IPF fibroblasts were uploaded to IPA (version 2.3) to identify the top canonical pathways, upstream regulators, and molecular and cellular functions.
DAVID database analysis
DAVID is a powerful gene functional classification tool that integrates multiple functional annotation databases, including Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes databases (https://david.ncifcrf.gov/) (35,36). By calculating the similarity of global annotation profiles with an agglomeration algorithm method, a list of notable genes may be classified into clusters of associated ‘Biological Process, ‘Cellular Components’, and ‘Molecular Functions’. It also provides an Expression Analysis Systematic Explorer (EASE) score, a modified one-tailed Fisher’s Exact P-value, for analysis. The reference score represents how specifically the user genes are involved in the category. An EASE score=0.1 was selected as the default, and =1 to extend clustering range in the analysis in the present study.
GEO database analysis
The GEO is a web database that collects submitted high-throughput gene-expression data of microarrays, chips or NGS (www.ncbi.nlm.nih.gov/geo) (37). Microarrays of accession numbers GSE24206, which included whole lung tissue samples from patients with early and advanced IPF (38) and GSE44723, which included samples of cultured lung fibroblasts from patients with IPF (39), were used in the present study. GSE44723 assessed gene expression in fibroblasts obtained from 4 normal controls, 4 patients with rapidly progressing IPF and 6 patients with slowly progressing IPF. GSE24206 assessed gene expression in whole lung biopsy or explant samples from 6 healthy controls, 8 patients with early IPF and 9 patients with advanced IPF. The databases used the platform of Affymetrix Human Genome U133 Plus 2.0 Array. Raw data extracted from the GEO were replotted using GraphPad Prism 7 software (GraphPad Software, Inc., La Jolla, CA, USA).
Statistical analysis
Statistical analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA). To identify the differentially expressed genes, the Wilcoxon rank-sum test was used to compare gene expressions between two groups (patients with IPF vs. controls), and the Kruskal-Wallis test followed by Benjamini-Hochberg multiple-testing corrections was used to compare gene expressions across three groups. P<0.05 was considered to indicate a statistically significant difference. Dysregulated genes identified from the IPF and normal fibroblasts NGS analysis were considered verified if they met the following criteria: Exhibiting concordant up-/downregulation in the GSE24206 and GSE44723 datasets, and demonstrating significantly different expression between patients with IPF and controls or across three groups in at least one dataset.
Results
Gene expression profiles and miRNA changes in IPF fibroblasts
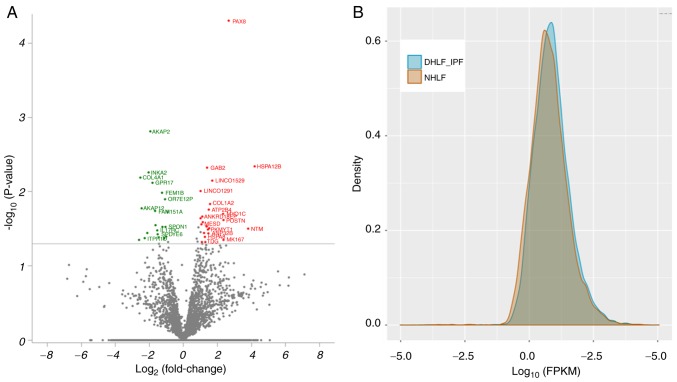
Samples from DHLF-IPF and NHLF cells were sequenced for mRNA and small RNA using an NGS platform. The volcano plot of dysregulated genes in fibroblasts of patients with IPF (DHLF-IPF cells) compared with normal controls (NHLF cells) is presented in Fig. 2A. The red nodes represent the significantly upregulated genes, and the green nodes represent significantly downregulated genes. The density plot of the deep sequencing results between the DHLF-IPF and NHLF cells is presented in Fig. 2B. The gene expression of DHLF-IPF cells demonstrated increased FPKM values and increased density compared with NHLF cells. Gene expression analysis revealed 42 differentially expressed genes with fold-change >2, including 23 upregulated and 19 down-regulated genes (Table I). miRNA expression analysis revealed 60 miRNAs with fold-change >2, including 43 upregulated and 17 downregulated miRNAs (Table II). According to miRmap analysis, 1,908 targets were predicted from these dysregulated miRNAs.
Figure 2.
Differential gene expression patterns between IPF and normal fibroblasts. (A) The volcano plot of -log10 (P-value) vs. log2 (fold-change) demonstrated differentially expressed genes in DHLF-IPF vs. NHLF. Genes with -log10 (P-value) >1.3 and >2 fold-changes are plotted in red (upregulated genes) or green (downregulated genes). (B) The frequency distribution of FPKM between DHLF-IPF cells and NHLF cells was compared and presented in the density plot. IPF, idiopathic pulmonary fibrosis; FPKM, fragments per kilobase of transcript per million mapped reads; DHLF, diseased human lung fibroblasts; NHLF, normal human lung fibroblasts.
Table I.
Dysregulated gene in IPF fibroblasts compared with normal lung fibroblasts.
| A, Upregulated | |||||
|---|---|---|---|---|---|
| Gene | Full gene name | DHLF-IPF FPKM | NHLF FPKM | Fold-change | P-value |
| HSPA12B | Heat shock protein family A (Hsp70) member 12B | 59.62 | 3.28 | 18.18 | 0.005 |
| NTM | Neurotrimin | 117.08 | 8.40 | 13.94 | 0.032 |
| PAX8 | Paired box 8 | 86.90 | 13.69 | 6.35 | 0.000 |
| MKI67 | Marker of proliferation Ki-67 | 16.75 | 3.25 | 5.15 | 0.045 |
| POSTN | Periostin | 42.91 | 8.35 | 5.14 | 0.024 |
| MYO1C | Myosin IC | 21.87 | 4.34 | 5.04 | 0.020 |
| LINC01529 | Long intergenic non-protein coding RNA 1529 | 41.54 | 12.83 | 3.24 | 0.007 |
| COL1A2 | Collagen type I alpha 2 chain | 69.47 | 23.42 | 2.97 | 0.015 |
| CCNL1 | Cyclin L1 | 38.61 | 13.41 | 2.88 | 0.031 |
| ATP2B4 | ATPase plasma membrane Ca2+ transporting 4 | 29.61 | 10.64 | 2.78 | 0.017 |
| ANP32B | Acidic nuclear phosphoprotein 32 family member B | 52.75 | 19.24 | 2.74 | 0.037 |
| PKMYT1 | Protein kinase, membrane associated tyrosine/threonine 1 | 571.51 | 212.09 | 2.69 | 0.032 |
| GAB2 | GRB2-associated binding protein 2 | 23.34 | 8.87 | 2.63 | 0.005 |
| GPM6B | Glycoprotein M6B | 39.57 | 15.38 | 2.57 | 0.029 |
| TDG | Thymine DNA glycosylase | 32.79 | 13.38 | 2.45 | 0.048 |
| HSPA8 | Heat shock protein family A (Hsp70) member 8 | 94.93 | 39.54 | 2.40 | 0.041 |
| CD248 | CD248 molecule | 25.01 | 10.79 | 2.32 | 0.036 |
| LINC00847 | Long intergenic non-protein coding RNA 847 | 91.64 | 41.90 | 2.19 | 0.026 |
| ANKRD18EP | Ankyrin repeat domain 18E, pseudogene | 98.99 | 45.65 | 2.17 | 0.022 |
| CNN3 | Calponin 3 | 70.11 | 33.29 | 2.11 | 0.047 |
| MESD | Mesoderm development LRP chaperone | 93.66 | 44.85 | 2.09 | 0.028 |
| IQGAP1 | IQ motif containing GTPase activating protein 1 | 45.40 | 22.51 | 2.02 | 0.023 |
| LINC01291 | Long intergenic non-protein coding RNA 1291 | 161.02 | 80.15 | 2.01 | 0.010 |
|
| |||||
| B, Downregulated | |||||
|
| |||||
| TYW1 | tRNA-YW synthesizing protein 1 homolog | 24.22 | 146.89 | -6.06 | 0.044 |
| COL4A1 | Collagen type IV alpha 1 chain | 4.11 | 23.87 | -5.81 | 0.006 |
| AKAP12 | A-kinase anchoring protein 12 | 4.24 | 23.09 | -5.45 | 0.017 |
| ITPRID2 | ITPR interacting domain containing 2 | 4.96 | 23.91 | -4.82 | 0.042 |
| PRKAR1B | Protein kinase cAMP-dependent type I regulatory subunit beta | 30.41 | 131.62 | -4.33 | 0.036 |
| INKA2 | Inka box actin regulator 2 | 11.38 | 47.14 | -4.14 | 0.006 |
| AKAP2 | A-kinase anchoring protein 2 | 12.30 | 47.75 | -3.88 | 0.002 |
| GPR17 | G protein-coupled receptor 17 | 14.88 | 52.29 | -3.51 | 0.008 |
| FAM151A | Family with sequence similarity 151 member A | 11.47 | 36.15 | -3.15 | 0.018 |
| UXT-AS1 | UXT antisense RNA 1 | 48.81 | 151.15 | -3.10 | 0.028 |
| IL17RC | Interleukin 17 receptor C | 8.18 | 23.55 | -2.88 | 0.033 |
| SPDYE6 | Speedy/RINGO cell cycle regulator family member E6 | 10.45 | 30.07 | -2.88 | 0.037 |
| MED31 | Mediator complex subunit 31 | 25.55 | 69.73 | -2.73 | 0.041 |
| FEM1B | Fem-1 homolog B | 14.77 | 35.13 | -2.38 | 0.010 |
| NCL | Nucleolin | 19.51 | 45.91 | -2.35 | 0.030 |
| PTX3 | Pentraxin 3 | 20.35 | 44.55 | -2.19 | 0.042 |
| OR7E12P | Olfactory receptor family 7 subfamily E member 12 pseudogene | 126.50 | 268.42 | -2.12 | 0.013 |
| SPON1 | Spondin 1 | 16.93 | 34.91 | -2.06 | 0.030 |
| COL4A2 | Collagen type IV alpha 2 chain | 12.65 | 25.46 | -2.01 | 0.040 |
IPF, idiopathic pulmonary fibrosis; FPKM, fragments per kilobase of transcript per million mapped reads; DHLF, diseased human lung fibroblast; NHLF, normal human lung fibroblast.
Table II.
Dysregulated miRNAs in IPF fibroblasts vs. normal lung fibroblasts.
| miRNA | DHLF-IPF Seq (norm) | NHLF Seq (norm) | Fold-change | Up/Down |
|---|---|---|---|---|
| hsa-miR-10b-5p | 3,357.09 | 317.7 | 10.57 | Up |
| hsa-miR-412-5p | 50.6 | 5.86 | 8.63 | Up |
| hsa-miR-329-3p | 6.77 | 1.69 | 4.01 | Up |
| hsa-miR-4661-5p | 4.51 | 1.17 | 3.85 | Up |
| hsa-miR-4521 | 17.7 | 4.82 | 3.67 | Up |
| hsa-miR-3130-3p | 3.8 | 1.17 | 3.25 | Up |
| hsa-miR-369-3p | 26.73 | 8.34 | 3.21 | Up |
| hsa-miR-615-3p | 11.17 | 3.52 | 3.17 | Up |
| hsa-miR-766-3p | 5.58 | 1.82 | 3.07 | Up |
| hsa-miR-548am-5p | 5.11 | 1.69 | 3.02 | Up |
| hsa-miR-5000-3p | 5.46 | 1.82 | 3.00 | Up |
| hsa-miR-619-5p | 3.44 | 1.17 | 2.94 | Up |
| hsa-miR-486-5p | 424.28 | 145.3 | 2.92 | Up |
| hsa-miR-493-5p | 369.05 | 132.01 | 2.80 | Up |
| hsa-miR-3613-5p | 10.45 | 3.78 | 2.76 | Up |
| hsa-miR-625-3p | 5.7 | 2.08 | 2.74 | Up |
| hsa-miR-33b-5p | 4.75 | 1.82 | 2.61 | Up |
| hsa-miR-382-3p | 14.49 | 5.6 | 2.59 | Up |
| hsa-miR-379-3p | 33.38 | 13.55 | 2.46 | Up |
| hsa-miR-199b-5p | 471.8 | 192.86 | 2.45 | Up |
| hsa-miR-127-3p | 292.67 | 120.67 | 2.43 | Up |
| hsa-miR-1254 | 2.79 | 1.17 | 2.38 | Up |
| hsa-miR-543 | 31.95 | 13.42 | 2.38 | Up |
| hsa-miR-549a | 15.92 | 6.91 | 2.30 | Up |
| hsa-miR-193a-3p | 5.7 | 2.48 | 2.30 | Up |
| hsa-miR-665 | 24.11 | 10.56 | 2.28 | Up |
| hsa-miR-376c-3p | 20.55 | 9.12 | 2.25 | Up |
| hsa-miR-487a-3p | 32.9 | 14.99 | 2.19 | Up |
| hsa-miR-582-3p | 4.87 | 2.22 | 2.19 | Up |
| hsa-miR-134-5p | 174.73 | 80.14 | 2.18 | Up |
| hsa-miR-1185-5p | 3.68 | 1.69 | 2.18 | Up |
| hsa-miR-493-3p | 159.05 | 73.89 | 2.15 | Up |
| hsa-miR-136-3p | 424.16 | 198.72 | 2.13 | Up |
| hsa-miR-136-5p | 12.35 | 5.86 | 2.11 | Up |
| hsa-miR-1185-1-3p | 49.06 | 23.33 | 2.10 | Up |
| hsa-miR-654-3p | 1,401.49 | 669.93 | 2.09 | Up |
| hsa-miR-185-3p | 6.18 | 3 | 2.06 | Up |
| hsa-miR-548ao-3p | 2.14 | 1.04 | 2.06 | Up |
| hsa-miR-668-3p | 3.21 | 1.56 | 2.06 | Up |
| hsa-miR-410-3p | 865.2 | 424.42 | 2.04 | Up |
| hsa-miR-409-3p | 3,074.39 | 1,512.26 | 2.03 | Up |
| hsa-miR-494-3p | 6.3 | 3.13 | 2.01 | Up |
| hsa-miR-1197 | 7.84 | 3.91 | 2.01 | Up |
| hsa-miR-182-5p | 47.63 | 95.52 | −2.01 | Down |
| hsa-miR-422a | 1.66 | 3.39 | −2.04 | Down |
| hsa-miR-3200-3p | 3.8 | 7.95 | −2.09 | Down |
| hsa-miR-335-5p | 49.53 | 103.99 | −2.10 | Down |
| hsa-miR-138-1-3p | 87.18 | 189.86 | −2.18 | Down |
| hsa-miR-365a-5p | 1.43 | 3.13 | −2.19 | Down |
| hsa-miR-5699-5p | 1.07 | 2.35 | −2.20 | Down |
| hsa-miR-664a-3p | 2.38 | 5.86 | −2.46 | Down |
| hsa-miR-1538 | 2.26 | 5.6 | −2.48 | Down |
| hsa-miR-4662a-5p | 2.97 | 7.56 | −2.55 | Down |
| hsa-miR-335-3p | 341.14 | 920.39 | −2.70 | Down |
| hsa-miR-29c-5p | 1.19 | 3.39 | −2.85 | Down |
| hsa-miR-9-5p | 1.54 | 4.69 | −3.05 | Down |
| hsa-miR-4461 | 2.61 | 7.95 | −3.05 | Down |
| hsa-miR-3662 | 1.43 | 4.82 | −3.37 | Down |
| hsa-miR-4767 | 1.31 | 4.82 | −3.68 | Down |
| hsa-miR-204-5p | 45.37 | 170.97 | −3.77 | Down |
IPF, idiopathic pulmonary fibrosis; DHLF, diseased human lung fibroblast; NHLF, normal human lung fibroblast; Up, upregulation; Down, downregulation; hsa, Homo sapiens; miR, microRNA.
IPA and DAVID analysis of dysregulated genes in IPF fibroblasts
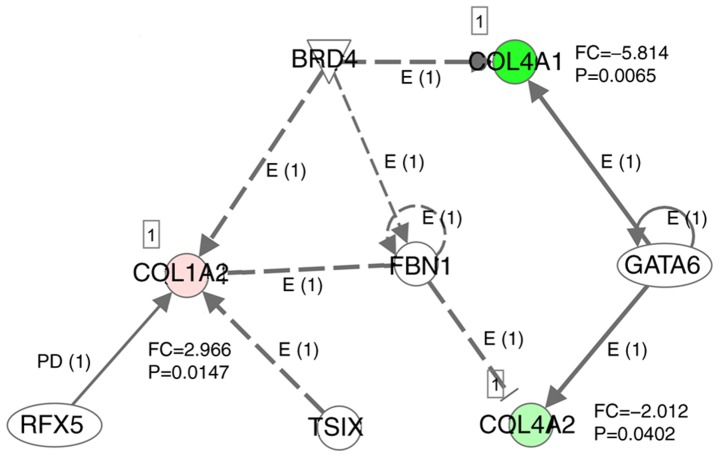
The pathways and functional annotation of the 42 dysregulated genes in IPF fibroblasts were first analyzed using IPA. The results are summarized in Table III. The top canonical pathways were cAMP-mediated signaling, GP6 signaling pathway, cardiac-adrenergic signaling, hepatic fibrosis/hepatic stellate cell activation and calcium transport I. The top upstream regulators were fibrillin-1, bromodo-main-containing protein 4, transcription factor GATA-6, TSIX and DNA-binding protein RFX5. Fig. 4 demonstrates the network of these top 5 upstream regulators and dysregulated genes. The top molecular and cellular functions included cell cycle, cell morphology, cellular development, lipid metabolism and molecular transport.
Table III.
Summary of Ingenuity® Pathway Analysis of 42 dysregulated genes in idiopathic pulmonary fibrosis fibroblasts.
| Categories | P-value | Overlap (%) | No. of molecules |
|---|---|---|---|
| Top canonical pathways | |||
| cAMP-mediated signaling | 0.0007 | 4/225 (1.8) | - |
| GP6 signaling pathway | 0.0018 | 3/131 (2.3) | - |
| Cardiac-adrenergic signaling | 0.0021 | 3/140 (2.1) | - |
| Hepatic fibrosis/hepatic stellate cell activation | 0.0045 | 3/183 (1.6) | - |
| Calcium transport I | 0.0181 | 1/10 (10.0) | - |
| Top upstream regulators | |||
| FBN1 | 0.0002 | - | - |
| BRD4 | 0.0021 | - | - |
| GATA6 | 0.0030 | - | - |
| TSIX | 0.0037 | - | - |
| RFX5 | 0.0037 | - | - |
| Top molecular and cellular function | |||
| Cell cycle | 0.0013-0.0181 | - | 6 |
| Cell morphology | 0.0018-0.0395 | - | 4 |
| Cellular development | 0.0018-0.0106 | - | 4 |
| Lipid metabolism | 0.0018-0.0199 | - | 2 |
| Molecular transport | 0.0018-0.0055 | - | 2 |
IPA, Ingenuity® Pathway Analysis; IPF, idiopathic pulmonary fibrosis; FBN1, fibrillin-1; BRD4, bromodomain-containing protein 4; GATA6, transcription factor GATA-6; RFX5, DNA-binding protein RFX5.
Figure 4.
Network of top 5 upstream regulators and dysregulated genes in idiopathic pulmonary fibrosis fibroblasts. The top 5 upstream regulators, including FBN1, BRD4, GATA6, TSIX and RFX5, were generated using Ingenuity® Pathway Analysis based on the significance of overlap between the dysregulated genes and the genes that were regulated by the upstream regulators. The dysregulated genes targeted by these top upstream regulators were COL1A2, COL4A1 and COL4A2, all belonging to the fibrillar collagen family. Numbers in parentheses are the number of reports supporting interactions. E, expression; FC, expression fold-change; PD, protein-DNA binding; CLO1A2, collagen alpha-2(I) chain; COL4A1, collagen alpha-1(IV) chain; COL4A2, collagen alpha-2(IV) chain; FBN1, fibrillin-1; BRD4, bromodomain-containing protein 4; GATA6, transcription factor GATA-6; RFX5, DNA-binding protein RFX5.
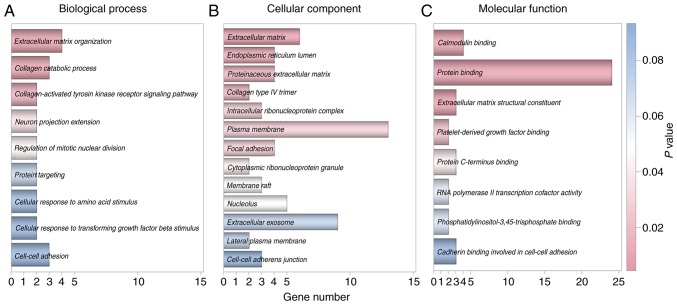
The functional annotation of the 42 dysregulated genes was subsequently analyzed using DAVID. Notably, results within the ‘Biological Process’, ‘Cellular Component’ and ‘Molecular Function’ categories all indicated that the most significant function of these dysregulated genes was associated with the composition and function of the extracellular matrix (ECM) (Fig. 3).
Figure 3.
Gene Ontology analysis of dysregulated genes identified in idiopathic pulmonary fibrosis fibroblasts. Functional annotation of the 42 dysregulated genes was determined using Database for Annotation, Visualization, and Integrated Discovery. Results within the (A) Biological Process, (B) Cellular Component and (C) Molecular Function categories all indicated that the most significant function of these genes was associated with the composition and function of extracellular matrix.
GEO database analysis of dysregulated genes in IPF fibro- blasts
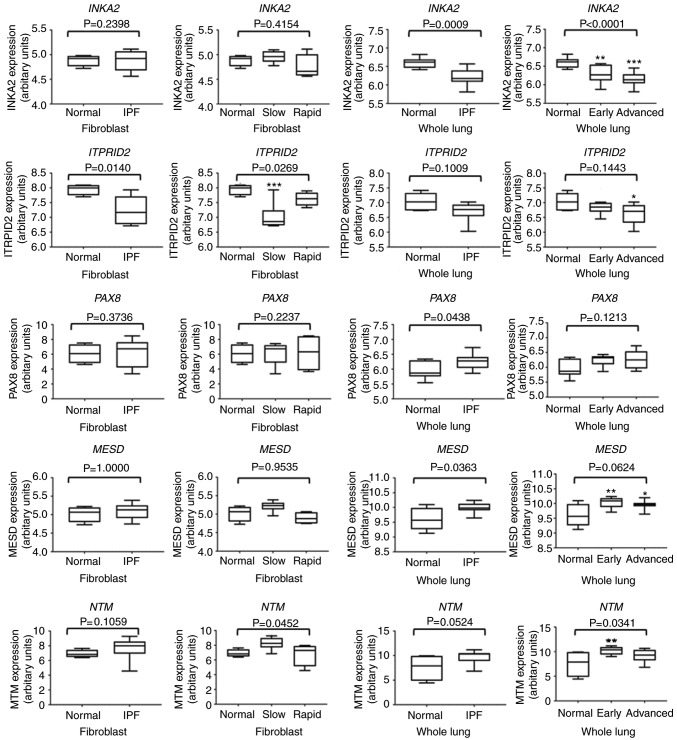
To additionally verify the 42 dysregulated genes in clinical samples from patients with IPF, the GEO database was searched and two representative microarray datasets were selected: GSE44723 (IPF cultured lung fibroblasts) and GSE24206 (early and advanced IPF whole lung tissues). Dysregulated genes were considered verified if they exhibited concordant up-/downregulation in the two GSE44723 and GSE24206 datasets, with significantly different expression between patients with IPF and controls in at least one dataset. The results are summarized in Table IV. Based on the GEO analysis, neurotrimin (NTM), paired box 8 (PAX8) and mesoderm development LRP chaperone (MESD) were verified as the upregulated genes, and ITPR interacting domain containing 2 (ITPRID2) and Inka box actin regulator 2 (INKA2) as the downregulated genes in IPF. The detailed expression levels of these 5 genes in each group were plotted and compared in Fig. 5.
Table IV.
Gene Expression Omnibus verification of 42 dysregulated genes in IPF fibroblasts.
| A, Upregulated genes
| |||||
|---|---|---|---|---|---|
| Genes | Fold-change |
GSE44723
|
GSE24206
|
||
| Up-/Downregulation | P-value | Up-/Downregulation | P-value | ||
| HSPA12B | 18.15 | N/A | - | Up | 0.835 |
| NTM | 13.94 | Up | 0.257 | Up | 0.010 |
| PAX8 | 6.35 | Up | 0.341 | Up | 0.032 |
| MKI67 | 5.15 | Down | 0.582 | Up | 0.017 |
| POSTN | 5.14 | Down | 0.688 | Up | 0.008 |
| MYO1C | 5.04 | Down | 0.810 | Up | 0.259 |
| LINC01529 | 3.24 | N/A | - | N/A | - |
| COL1A2 | 2.97 | Down | 0.397 | Up | <0.001 |
| CCNL1 | 2.88 | Up | 0.737 | Down | <0.001 |
| ATP2B4 | 2.78 | Up | 0.147 | Up | 0.159 |
| ANP32B | 2.74 | Up | 0.443 | Down | 0.159 |
| PKMYT1 | 2.69 | Down | 0.929 | Up | 0.832 |
| GAB2 | 2.63 | Down | 0.873 | Down | <0.001 |
| GPM6B | 2.57 | Up | 0.890 | Down | 0.013 |
| TDG | 2.45 | N/A | - | Down | 0.113 |
| HSPA8 | 2.40 | N/A | - | Up | 0.081 |
| CD248 | 2.32 | Down | 0.255 | Up | 0.115 |
| LINC00847 | 2.19 | Down | 0.053 | Up | 0.091 |
| ANKRD18EP | 2.17 | N/A | - | N/A | - |
| CNN3 | 2.11 | N/A | - | Down | 0.095 |
| MESD | 2.09 | Up | 0.958 | Up | 0.002 |
| IQGAP1 | 2.02 | Up | 0.437 | Down | 0.717 |
| LINC01291 | 2.01 | N/A | - | N/A | - |
|
| |||||
| B, Downregulated genes | |||||
|
| |||||
| TYW1 | -6.06 | Up | 0.201 | Down | 0.716 |
| COL4A1 | -5.81 | Down | 0.224 | Up | 0.354 |
| AKAP12 | -5.45 | Up | 0.410 | Down | 0.004 |
| ITPRID2 | -4.82 | Down | 0.019 | Down | 0.031 |
| PRKAR1B | -4.33 | Down | 0.194 | Up | 0.767 |
| INKA2 | -4.14 | Down | 0.213 | Down | 0.001 |
| AKAP2 | -3.88 | N/A | - | Down | 0.007 |
| GPR17 | -3.51 | N/A | - | Down | 0.460 |
| FAM151A | -3.15 | N/A | - | Down | 0.081 |
| UXT-AS1 | -3.10 | N/A | - | N/A | - |
| IL17RC | -2.88 | Down | 0.841 | Down | 0.630 |
| SPDYE6 | -2.88 | N/A | - | Down | 0.220 |
| MED31 | -2.73 | Up | 0.478 | Up | 0.831 |
| FEM1B | -2.38 | Up | 0.873 | Down | 0.024 |
| NCL | -2.35 | N/A | - | Down | 0.166 |
| PTX3 | -2.19 | Up | 0.918 | Down | <.001 |
| OR7E12P | -2.12 | N/A | - | Down | 0.937 |
| SPON1 | -2.06 | Up | 0.986 | Down | 0.036 |
| COL4A2 | -2.01 | Down | 0.214 | Up | 0.584 |
Fold-change indicates the results of RNA-seq analysis from the next-generation sequencing data. GEO, Gene Expression Omnibus; IPF, idiopathic pulmonary fibrosis; N/A, not available.
Figure 5.
Gene Expression Omnibus analysis of 5 dysregulated genes in IPF fibroblasts. Representative microarray datasets GSE44723 (slowly and rapidly progressing IPF: cultured lung fibroblasts) and GSE24206 (early and advanced IPF: whole lung tissue) were used for verification of differential gene expressions identified from Next Generation Sequencing analysis. The results indicated that the expression of INKA2 and ITRPID2 were downregulated and PAX8, MESD and NTM were upregulated in IPF. Cultured lung fibroblasts and whole lung from healthy subjects were used as the normal controls. P-values were calculated using the Wilcoxon rank-sum test for comparisons of two groups, and the Kruskal-Wallis test for comparisons of three groups. Adjusted P-values were calculated using the Kruskal-Wallis test followed by Benjamini-Hochberg multiple-testing corrections. *Adjusted P<0.05, **adjusted P<0.01 and ***adjusted P<0.001. IPF, idiopathic pulmonary fibrosis; INKA2, Inka box actin regulator 2; ITPRID2, ITPR interacting domain containing 2; PAX8, paired box 8; MESD, mesoderm development LRP chaperone; NTM, neurotrimin.
Identification of dysregulated genes with potential miRNA-mRNA interactions in IPF fibroblasts
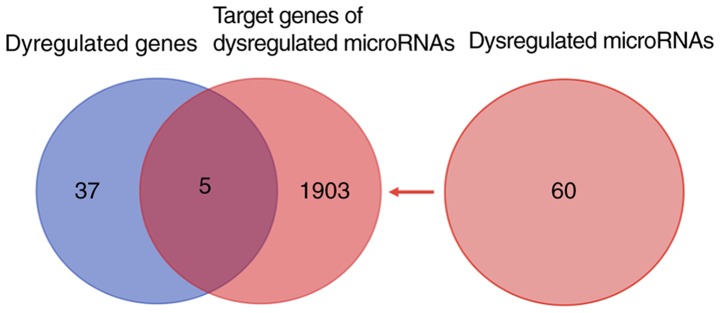
Venn diagram analysis of the 1,908 target genes of 60 dysregulated miRNAs, predicted from miRmap, and the 42 dysregulated genes revealed 5 dysregulated genes with potential miRNA-mRNA interactions in IPF fibroblasts (Fig. 6). A total of 2 miRNA-mRNA interactions, Homo sapiens (hsa)-miR-185-3p-heat shock protein family A member 12B (HSPA12B) and hsa-miR185-3p-GRB associated binding protein 2 (GAB2), were excluded due to a lack of biological plausibility (the miRNA and mRNA were upregulated). The remaining 3 genes with miRNA-mRNA interactions were subsequently verified in a second miRNA predicting database, TargetScan. The results identified hsa-miR-185-3p-TRNA-YW synthesizing protein 1 homolog (TYW1), hsa-miR-3662- glycoprotein M6B (GPM6B), hsa-miR-1254-INKA2 and hsa-miR-766-3p-INKA2 as the potential miRNA-mRNA interactions in IPF fibroblasts (Table V).
Figure 6.
Venn diagram analysis of miRNA-mRNA interactions in idiopathic pulmonary fibrosis fibroblasts. RNA sequencing revealed 42 dysregulated genes (left). Small RNA sequencing revealed 60 dysregulated miRNAs, which predicted 1,908 target genes (right) based on miRmap database. Venn diagram analysis identified 5 dysregulated genes with potential miRNA-mRNA interaction. miRNA, microRNA.
Table V.
Dysregulated genes with potential miRNA-mRNA interaction in IPF fibroblasts.
| Gene | Gene full name | mRNA fold-change | miRNA | miRNA fold-change | miRmap score | TargetScan Total context++ score |
|---|---|---|---|---|---|---|
| TYW1 | tRNA-YW synthesizing protein 1 homolog | -6.06 | hsa-miR-185-3p | 2.06 | 99.12 | -0.37 |
| GPM6B | glycoprotein M6B | 2.44 | hsa-miR-3662 | -3.37 | 99.81 | -0.09 |
| INKA2 | Inka box actin regulator 2 | -4.14 | hsa-miR-1254 hsa-miR-766-3p |
2.38 3.07 |
99.28 99.09 |
-0.32 -0.67 |
IPF, idiopathic pulmonary fibrosis; miRNA, microRNA; hsa, Homo sapiens; TYW1, TRNA-YW synthesizing protein 1 homolog; GPM6B, glycoprotein M6B; INKA2, Inka box actin regulator 2.
Discussion
The pathogenic mechanisms of IPF have not yet been fully elucidated. The hallmarks of IPF are aberrant activation of lung epithelial cells, accumulation of fibroblasts and myofibroblasts, and excessive production of ECM (4,14-16). Previous data indicate that fibroblasts, as one of the key cells, serve a crucial role in the development and progression of IPF (16). An improved understanding of the gene regulation in IPF fibroblasts may assist in the development of novel therapeutics targeting this key cell. In the present study, the whole mRNA and miRNA profiles of IPF fibroblasts were obtained using an NGS platform, and bioinformatics analyses were performed in a step-wise manner. A total of 42 dysregulated genes were identified, and then bioinformatics tools IPA and DAVID were used for pathway and functional analyses. A total of 5 of the differentially expressed genes were verified in the representative GEO datasets, including NTM, PAX8 and MESD (upregulated), and ITPRID2 and INKA2 (downregulated). Integrated analysis of mRNA and miRNA expression data was also performed, and hsa-miR-185-3p-TY W1, hsa-miR-3662-GPM6B, hsa-miR-1254-INKA2 and hsa-miR-766-3p-INKA2 were identified as the potential miRNA-mRNA interactions in IPF fibroblasts. According to the GEO verification, hsa-miR-1254-INKA2 and hsa-miR-766-3p-INKA2 were considered as the most likely dysregulated miRNA-mRNA interactions in IPF fibroblasts. However, these interactions were identified based on bioinformatic analysis. Therefore, they require additional experiments to confirm the results. Hsa-miR185-3p-HSPA12B and hsa-miR185-3p-GAB2 were excluded from subsequent analysis, as the miRNAs and mRNAs were dysregulated in the same manner. There is a possibility of indirect modulation, in that the upregulated hsa-miR185-3p may control one or more other targets. Which may in turn upregulate the expression levels of HSPA12B or GAB2. Nevertheless, the upregulated levels of HSPA12B or GAB2 were not validated in the GEO database analysis. Whether these 2 miRNA-mRNA interactions were excluded or not did not affect the final results.
In the GO analysis, it was identified that the most important function of the identified dysregulated genes was associated with the composition and function of the ECM. Replacement of the normal lung structure with an excessive deposition of disorganized collagen and ECM is the hallmark of IPF (40). Although previous evidence suggests that fibroblasts and myofibroblasts in the fibrotic foci are the key cells leading to excessive ECM production (41), the crosstalk between epithelial cells, fibroblasts, myofibroblasts and ECM remains largely uncharacterized. The results from the present study improve the understanding of the fibroblast-ECM interaction in the pathogenesis of IPF. The development of novel therapeutic strategies targeting the fibrotic ECM may provide an opportunity to halt fibrosis and restore organ function (42). A recent study confirmed the importance of the ECM in IPF pathogenesis and treatment: Kwapiszewska et al (43) compared transcriptomic profiles in lung homogenates and fibroblasts obtained from patients with IPF treated with or without pirfenidone. They identified that cell migration-inducing and hyaluronan-binding protein (CEMIP) was markedly downregulated by pirfenidone treatment. They also identified that circulating CEMIP levels were significantly increased in patients with IPF compared with the healthy controls, and that pirfenidone treatment was associated with a significant decrease in CEMIP levels. CEMIP has been previously associated with ECM production, inflammation and cell proliferation (44,45). They concluded that pirfenidone exhibited effects on multiple pathways in fibroblasts and other pulmonary cells, through the regulation of the ECM structure and inflammatory reactions.
The INKA2 gene, also known as family with sequence similarity 212 member B or chromosome 1 open reading frame 183, encodes the protein serine/threonine-protein kinase PAK4 (PAK4)-inhibitor INKA2. The PAK4-inhibitor INKA proteins, with 2 isoforms in humans, are endogenous inhibitors of PAK4 (46). The PAK proteins are a family of serine/threonine cyclin-dependent kinase inhibitor 1-activating protein kinases and have been implicated in a range of biological activities (46). PAK4 is an effector molecule for the Rho GTPase cell division control protein 42 homolog. Previous experiments have indicated that active PAK4 protects cells from apoptosis (47,48). PAK4 is associated with tumorigenesis and progression in different types of cancer through promoting cell growth, proliferation, migration and metastasis (49-55). The downregulation of INKA2 identified in the present study may potentially upregulate the expression of PAK4, which in turn promotes cell proliferation and inhibits cell apoptosis in IPF fibroblasts. The NGS data suggested that the FPKM of PAK4 was 0.2922 in IPF fibroblasts, but undetectable in normal lung fibroblasts. Based on the quality control criterion to exclude genes with FPKM <0.3 in either IPF or normal fibroblasts, PAK4 was not able to be analyzed in the present study. The upregulation of PAK4 in IPF fibroblasts required additional confirmation. It was also identified that the miRNAs hsa-miR-1254 and hsa-miR-766-3p, 2 putative regulators of INKA2, were upregulated in IPF fibroblasts. Therefore, the results suggested that the miRNA-mRNA interaction in the INKA2 gene may serve a role in cell growth, proliferation or apoptosis inhibition in IPF fibroblasts.
The PAX8 gene encodes protein PAX8, which is a member of the paired box family of transcription factors. PAX8 is involved in the development and differentiation of thyroid follicular cells (56,57), and is associated with the growth of cancer cells (58,59). Overexpression of PAX8 has been observed in a number of types of cancer. It also has a critical role in the survival and proliferation of epithelial cells (60). In the present study, upregulation of PAX8 was identified in IPF fibroblasts. These data suggested that PAX8 may serve a role in promoting the growth, survival or proliferation of fibroblasts in IPF. The upregulation of NTM and MESD (also known as mesoderm development candidate 2), and downregulation of ITPRID2 (also known as Ki-Ras-induced actin-interacting protein or sperm specific antigen 2) were also identified in IPF fibroblasts. Neurotrimin, a neural cell adhesion molecule, may promote neurite outgrowth and adhesion via a homophilic mechanism (61,62). In addition to brain tissue, human tissue-specific expression analysis indicated a high expression of NTM in human lung tissue (63). MESD, a specialized chaperone for low-density lipoprotein receptor-related protein (LRP)5 and LRP6, is a universal inhibitor of Wnt/LRP signaling on the cell surface (64,65). ITPRID2 encodes a protein that is involved in the regulation of filamentous actin and extracellular signals (66), and may be associated with structural integrity and/or signal transductions in human cancer (67). The functions of NTM, MESD and ITPRID2 remain largely unknown. Their associations with human lung diseases, particularly IPF, require additional investigation.
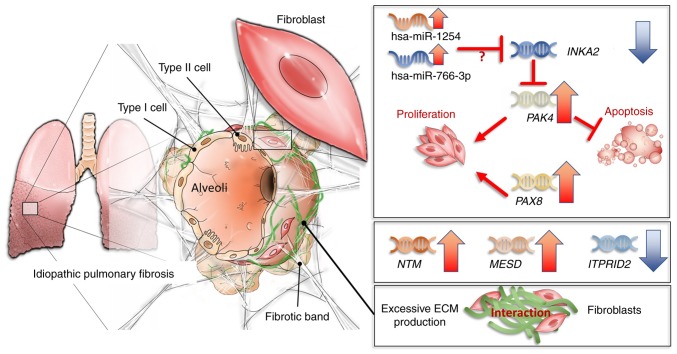
The identified gene dysregulation in fibroblasts and their proposed mechanisms in IPF are summarized in Fig. 7. In summary, the present study demonstrated that NTM, PAX8 and MESD were upregulated and ITPRID2 and INKA2 were downregulated in IPF fibroblasts. Dysregulation of PAX8 and INKA2 may participate in the regulation of proliferation and survival in IPF fibroblasts. Functional analysis of the dysregu-lated genes suggested a marked association between fibroblasts and ECM. The integrated analysis of miRNA and mRNA expression profiles suggested that the upregulated miRNAs hsa-miR-1254 and hsa-miR-766-3p may downregulate INKA2 and serve important roles in IPF. These data improve the current understanding of fibroblasts as key cells in the pathogenesis of IPF. As a screening study using bioinformatics approaches, without biological or cross-platform replicates, the results of the present study require additional validation.
Figure 7.
Proposed mechanisms demonstrating gene regulations of fibroblasts and their potential roles in IPF. Upregulation of hsa-miR-1254 and hsa-miR-766-3p may inhibit INKA2 expression, leading to overexpression of PAK4, which may promote fibroblast proliferation and migration, and protect fibroblasts from apoptosis. Overexpression of PAX8 may also have a role in fibroblast proliferation. The functions of NTM, MESD and ITPRID2 remain unknown. Whether they contribute to the pro-proliferative and pro-fibrotic microenvironment requires additional study. Based on the results of the Gene Ontology analysis, the gene dysregulations in IPF fibroblasts may also have a role in the excessive production and deposition of disorganized ECM. The hsa-miR-1254-INKA2 and hsa-miR-766-3p-INKA2 interactions were identified based on bioinformatic analysis, and therefore requires additional experiments to confirm. IPF, idiopathic pulmonary fibrosis; hsa, Homo sapiens; INKA2, Inka box actin regulator 2; PAK4, serine/threonine-protein kinase PAK4; PAX8, paired box 8; MESD, mesoderm development LRP chaperone; NTM, neurotrimin; ITPRID2, ITPR interacting domain containing 2; ECM, extracellular matrix.
Acknowledgments
The authors gratefully acknowledge the assistance from the Center for Research and Development of Kaohsiung Medical University (Kaohsiung, Taiwan), and the assistance with statistical analysis from Mr. Tse-Kuang Kai at Kaohsiung Medical University Hospital.
Funding
The present study was supported in part by research grants from the Ministry of Science and Technology (grant nos. MOST 107-2320-B-037-011-MY3 and MOST 106-2314-B-037-016-MY2), the Kaohsiung Medical University Hospital Research Foundation (grant nos. KMUHS10701, KMUHS10712, KMUH106-6R15 and KMUH107-7M06), and the Kaohsiung Medical University (grant no. KMU-DK108003).
Availability of data and materials
The data used and analyzed in this study are available from the corresponding author on reasonable request.
Authors’ contributions
CCS, IWC and PLK conceived the study. CCS, WAC and MJT analyzed and interpreted the data. CCS, WAC, MJT, IWC and PLK prepared the manuscript. SHL performed cell culture and laboratory experiments. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, Behr J, Cottin V, Danoff SK, Morell F, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44-e68. doi: 10.1164/rccm.201807-1255ST. [DOI] [PubMed] [Google Scholar]
- 2.Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, et al. An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vancheri C, Failla M, Crimi N, Raghu G. Idiopathic pulmonary fibrosis: A disease with similarities and links to cancer biology. Eur Respir J. 2010;35:496–504. doi: 10.1183/09031936.00077309. [DOI] [PubMed] [Google Scholar]
- 4.Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med. 2018;378:1811–1823. doi: 10.1056/NEJMra1705751. [DOI] [PubMed] [Google Scholar]
- 5.Hutchinson J, Fogarty A, Hubbard R, McKeever T. Global incidence and mortality of idiopathic pulmonary fibrosis: A systematic review. Eur Respir J. 2015;46:795–806. doi: 10.1183/09031936.00185114. [DOI] [PubMed] [Google Scholar]
- 6.Navaratnam V, Fogarty AW, Glendening R, McKeever T, Hubbard RB. The increasing secondary care burden of idiopathic pulmonary fibrosis: Hospital admission trends in England from 1998 to 2010. Chest. 2013;143:1078–1084. doi: 10.1378/chest.12-0803. [DOI] [PubMed] [Google Scholar]
- 7.Sack C, Vedal S, Sheppard L, Raghu G, Barr RG, Podolanczuk A, Doney B, Hoffman EA, Gassett A, Hinckley-Stukovsky K, et al. Air pollution and subclinical interstitial lung disease: The Multi-Ethnic Study of Atherosclerosis (MESA) air-lung study. Eur Respir J. 2017;50:1700559. doi: 10.1183/13993003.00559-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baumgartner KB, Samet JM, Coultas DB, Stidley CA, Hunt WC, Colby TV, Waldron JA. Occupational and environmental risk factors for idiopathic pulmonary fibrosis: A multicenter case-control study. Collaborating centers. Am J Epidemiol. 2000;152:307–315. doi: 10.1093/aje/152.4.307. [DOI] [PubMed] [Google Scholar]
- 9.Tang YW, Johnson JE, Browning PJ, Cruz-Gervis RA, Davis A, Graham BS, Brigham KL, Oates JA, Jr, Loyd JE, Stecenko AA. Herpesvirus DNA is consistently detected in lungs of patients with idiopathic pulmonary fibrosis. J Clin Microbiol. 2003;41:2633–2640. doi: 10.1128/JCM.41.6.2633-2640.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tobin RW, Pope CE, II, Pellegrini CA, Emond MJ, Sillery J, Raghu G. Increased prevalence of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;158:1804–1808. doi: 10.1164/ajrccm.158.6.9804105. [DOI] [PubMed] [Google Scholar]
- 11.Fingerlin TE, Murphy E, Zhang W, Peljto AL, Brown KK, Steele MP, Loyd JE, Cosgrove GP, Lynch D, Groshong S, et al. Genome-wide association study identifies multiple susceptibility loci for pulmonary fibrosis. Nat Genet. 2013;45:613–620. doi: 10.1038/ng.2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noth I, Zhang Y, Ma SF, Flores C, Barber M, Huang Y, Broderick SM, Wade MS, Hysi P, Scuirba J, et al. Genetic variants associated with idiopathic pulmonary fibrosis susceptibility and mortality: A genome-wide association study. Lancet Respir Med. 2013;1:309–317. doi: 10.1016/S2213-2600(13)70045-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peljto AL, Zhang Y, Fingerlin TE, Ma SF, Garcia JG, Richards TJ, Silveira LJ, Lindell KO, Steele MP, Loyd JE, et al. Association between the MUC5B promoter polymorphism and survival in patients with idiopathic pulmonary fibrosis. JAMA. 2013;309:2232–2239. doi: 10.1001/jama.2013.5827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mora AL, Rojas M, Pardo A, Selman M. Emerging therapies for idiopathic pulmonary fibrosis, a progressive age-related disease. Nat Rev Drug Discov. 2017;16:755–772. doi: 10.1038/nrd.2017.170. [DOI] [PubMed] [Google Scholar]
- 15.Gomperts BN, Strieter RM. Fibrocytes in lung disease. J Leukoc Biol. 2007;82:449–456. doi: 10.1189/jlb.0906587. [DOI] [PubMed] [Google Scholar]
- 16.Pardo A, Selman M. Lung fibroblasts, aging, and idiopathic pulmonary fibrosis. Ann Am Thorac Soc. 2016;13(Suppl 5):S417–S421. doi: 10.1513/AnnalsATS.201605-341AW. [DOI] [PubMed] [Google Scholar]
- 17.Ramos C, Montaño M, García-Alvarez J, Ruiz V, Uhal BD, Selman M, Pardo A. Fibroblasts from idiopathic pulmonary fibrosis and normal lungs differ in growth rate, apoptosis, and tissue inhibitor of metalloproteinases expression. Am J Respir Cell Mol Biol. 2001;24:591–598. doi: 10.1165/ajrcmb.24.5.4333. [DOI] [PubMed] [Google Scholar]
- 18.Pierce EM, Carpenter K, Jakubzick C, Kunkel SL, Evanoff H, Flaherty KR, Martinez FJ, Toews GB, Hogaboam CM. Idiopathic pulmonary fibrosis fibroblasts migrate and proliferate to CC chemokine ligand 21. Eur Respir J. 2007;29:1082–1093. doi: 10.1183/09031936.00122806. [DOI] [PubMed] [Google Scholar]
- 19.Kurundkar AR, Kurundkar D, Rangarajan S, Locy ML, Zhou Y, Liu RM, Zmijewski J, Thannickal VJ. The matricellular protein CCN1 enhances TGF-β1/SMAD3-dependent profibrotic signaling in fibroblasts and contributes to fibrogenic responses to lung injury. FASEB J. 2016;30:2135–2150. doi: 10.1096/fj.201500173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conte E, Gili E, Fruciano M, Korfei M, Fagone E, Iemmolo M, Lo Furno D, Giuffrida R, Crimi N, Guenther A, Vancheri C. PI3K p110γ overexpression in idiopathic pulmonary fibrosis lung tissue and fibroblast cells: In vitro effects of its inhibition. Lab Invest. 2013;93:566–576. doi: 10.1038/labinvest.2013.6. [DOI] [PubMed] [Google Scholar]
- 21.Vuga LJ, Ben-Yehudah A, Kovkarova-Naumovski E, Oriss T, Gibson KF, Feghali-Bostwick C, Kaminski N. WNT5A is a regulator of fibroblast proliferation and resistance to apoptosis. Am J Respir Cell Mol Biol. 2009;41:583–589. doi: 10.1165/rcmb.2008-0201OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desai O, Winkler J, Minasyan M, Herzog EL. The role of immune and inflammatory cells in idiopathic pulmonary fibrosis. Front Med. 2018;5:43. doi: 10.3389/fmed.2018.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vejnar CE, Zdobnov EM. MiRmap: Comprehensive prediction of microRNA target repression strength. Nucleic Acids Res. 2012;40:11673–11683. doi: 10.1093/nar/gks901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agarwal V, Bell GW, Nam JW, Bartel DP. Predicting effective microRNA target sites in mammalian mRNAs. Elife. 2015;4 doi: 10.7554/eLife.05005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheu CC, Tsai MJ, Chen FW, Chang KF, Chang WA, Chong IW, Kuo PL, Hsu YL. Identification of novel genetic regulations associated with airway epithelial homeostasis using next-generation sequencing data and bioinformatics approaches. Oncotarget. 2017;8:82674–82688. doi: 10.18632/oncotarget.19752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang WA, Tsai MJ, Jian SF, Sheu CC, Kuo PL. Systematic analysis of transcriptomic profiles of COPD airway epithelium using next-generation sequencing and bioinformatics. Int J Chron Obstruct Pulmon Dis. 2018;13:2387–2398. doi: 10.2147/COPD.S173206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsai MJ, Chang WA, Jian SF, Chang KF, Sheu CC, Kuo PL. Possible mechanisms mediating apoptosis of bronchial epithelial cells in chronic obstructive pulmonary disease - A next-generation sequencing approach. Pathol Res Pract. 2018;214:1489–1496. doi: 10.1016/j.prp.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 28.Bolger AM, Lohse M, Usadel B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedländer MR, Mackowiak SD, Li N, Chen W, Rajewsky N. miRDeep2 accurately identifies known and hundreds of novel microRNA genes in seven animal clades. Nucleic Acids Res. 2012;40:37–52. doi: 10.1093/nar/gkr688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kent WJ, Sugnet CW, Furey TS, Roskin KM, Pringle TH, Zahler AM, Haussler D. The human genome browser at UCSC. Genome Res. 2002;12:996–1006. doi: 10.1101/gr.229102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim D, Langmead B, Salzberg SL. HISAT: A fast spliced aligner with low memory requirements. Nat Methods. 2015;12:357–360. doi: 10.1038/nmeth.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galipon J, Ishii R, Suzuki Y, Tomita M, Ui-Tei K. Differential binding of three major human ADAR isoforms to coding and long non-coding transcripts. Genes. 2017;8:E68. doi: 10.3390/genes8020068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trapnell C, Roberts A, Goff L, Pertea G, Kim D, Kelley DR, Pimentel H, Salzberg SL, Rinn JL, Pachter L. Differential gene and transcript expression analysis of RNA-seq experiments with TopHat and Cufflinks. Nat Protoc. 2012;7:562–578. doi: 10.1038/nprot.2012.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krämer A, Green J, Pollard J, Jr, Tugendreich S. Causal analysis approaches in ingenuity pathway analysis. Bioinformatics. 2014;30:523–530. doi: 10.1093/bioinformatics/btt703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang da W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 36.Huang da W, Sherman BT, Lempicki RA. Bioinformatics enrichment tools: Paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 2009;37:1–13. doi: 10.1093/nar/gkn923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Edgar R, Domrachev M, Lash AE. Gene Expression Omnibus: NCBI gene expression and hybridization array data repository. Nucleic Acids Res. 2002;30:207–210. doi: 10.1093/nar/30.1.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meltzer EB, Barry WT, D’Amico TA, Davis RD, Lin SS, Onaitis MW, Morrison LD, Sporn TA, Steele MP, Noble PW. Bayesian probit regression model for the diagnosis of pulmonary fibrosis: Proof-of-principle. BMC Med Genomics. 2011;4:70. doi: 10.1186/1755-8794-4-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peng R, Sridhar S, Tyagi G, Phillips JE, Garrido R, Harris P, Burns L, Renteria L, Woods J, Chen L, et al. Bleomycin induces molecular changes directly relevant to idiopathic pulmonary fibrosis: A model for ‘active’ disease. PLoS One. 2013;8:e59348. doi: 10.1371/journal.pone.0059348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barratt SL, Creamer A, Hayton C, Chaudhuri N. Idiopathic pulmonary fibrosis (IPF): An overview. J Clin Med. 2018;7:E201. doi: 10.3390/jcm7080201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sgalla G, Iovene B, Calvello M, Ori M, Varone F, Richeldi L. Idiopathic pulmonary fibrosis: Pathogenesis and management. Respir Res. 2018;19:32. doi: 10.1186/s12931-018-0730-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Walraven M, Hinz B. Therapeutic approaches to control tissue repair and fibrosis: Extracellular matrix as a game changer. Matrix Biol. 2018:71–72. 205–224. doi: 10.1016/j.matbio.2018.02.020. [DOI] [PubMed] [Google Scholar]
- 43.Kwapiszewska G, Gungl A, Wilhelm J, Marsh LM, Thekkekara Puthenparampil H, Sinn K, Didiasova M, Klepetko W, Kosanovic D, Schermuly RT, et al. Transcriptome profiling reveals the complexity of pirfenidone effects in idiopathic pulmonary fibrosis. Eur Respir J. 2018;52:1800564. doi: 10.1183/13993003.00564-2018. [DOI] [PubMed] [Google Scholar]
- 44.Soroosh A, Albeiroti S, West GA, Willard B, Fiocchi C, de la Motte CA. Crohn’s disease fibroblasts overproduce the novel protein KIAA1199 to create proinflammatory hyaluronan fragments. Cell Mol Gastroenterol Hepatol. 2016;2:358–368. e4. doi: 10.1016/j.jcmgh.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li L, Yan LH, Manoj S, Li Y, Lu L. Central role of CEMIP in tumorigenesis and its potential as therapeutic target. J Cancer. 2017;8:2238–2246. doi: 10.7150/jca.19295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baskaran Y, Ang KC, Anekal PV, Chan WL, Grimes JM, Manser E, Robinson RC. An in cellulo-derived structure of PAK4 in complex with its inhibitor Inka1. Nat Commun. 2015;6:8681. doi: 10.1038/ncomms9681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gnesutta N, Qu J, Minden A. The serine/threonine kinase PAK4 prevents caspase activation and protects cells from apoptosis. J Biol Chem. 2001;276:14414–14419. doi: 10.1074/jbc.M011046200. [DOI] [PubMed] [Google Scholar]
- 48.Gnesutta N, Minden A. Death receptor-induced activation of initiator caspase 8 is antagonized by serine/threonine kinase PAK4. Mol Cell Biol. 2003;23:7838–7848. doi: 10.1128/MCB.23.21.7838-7848.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Callow MG, Clairvoyant F, Zhu S, Schryver B, Whyte DB, Bischoff JR, Jallal B, Smeal T. Requirement for PAK4 in the anchorage-independent growth of human cancer cell lines. J Biol Chem. 2002;277:550–558. doi: 10.1074/jbc.M105732200. [DOI] [PubMed] [Google Scholar]
- 50.Siu MK, Chan HY, Kong DS, Wong ES, Wong OG, Ngan HY, Tam KF, Zhang H, Li Z, Chan QK, et al. p21-activated kinase 4 regulates ovarian cancer cell proliferation, migration, and invasion and contributes to poor prognosis in patients. Proc Natl Acad Sci USA. 2010;107:18622–18627. doi: 10.1073/pnas.0907481107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wong LE, Chen N, Karantza V, Minden A. The Pak4 protein kinase is required for oncogenic transformation of MDA-MB-231 breast cancer cells. Oncogenesis. 2013;2:e50. doi: 10.1038/oncsis.2013.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guo Q, Su N, Zhang J, Li X, Miao Z, Wang G, Cheng M, Xu H, Cao L, Li F. PAK4 kinase-mediated SCG10 phosphorylation involved in gastric cancer metastasis. Oncogene. 2014;33:3277–3287. doi: 10.1038/onc.2013.296. [DOI] [PubMed] [Google Scholar]
- 53.Wang C, Li Y, Zhang H, Liu F, Cheng Z, Wang D, Wang G, Xu H, Zhao Y, Cao L, et al. Oncogenic PAK4 regulates Smad2/3 axis involving gastric tumorigenesis. Oncogene. 2014;33:3473–3484. doi: 10.1038/onc.2013.300. [DOI] [PubMed] [Google Scholar]
- 54.Xia M, Wei J, Tong K. MiR-224 promotes proliferation and migration of gastric cancer cells through targeting PAK4. Pharmazie. 2016;71:460–464. doi: 10.1691/ph.2016.6580. [DOI] [PubMed] [Google Scholar]
- 55.Zhang X, Zhang X, Li Y, Shao Y, Xiao J, Zhu G, Li F. PAK4 regulates G6PD activity by p53 degradation involving colon cancer cell growth. Cell Death Dis. 2017;8:e2820. doi: 10.1038/cddis.2017.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pasca di Magliano M, Di Lauro R, Zannini M. Pax8 has a key role in thyroid cell differentiation. Proc Natl Acad Sci USA. 2000;97:13144–13149. doi: 10.1073/pnas.240336397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mansouri A, Chowdhury K, Gruss P. Follicular cells of the thyroid gland require Pax8 gene function. Nat Genet. 1998;19:87–90. doi: 10.1038/ng0598-87. [DOI] [PubMed] [Google Scholar]
- 58.Muratovska A, Zhou C, He S, Goodyer P, Eccles MR. Paired-Box genes are frequently expressed in cancer and often required for cancer cell survival. Oncogene. 2003;22:7989–7997. doi: 10.1038/sj.onc.1206766. [DOI] [PubMed] [Google Scholar]
- 59.Ghannam-Shahbari D, Jacob E, Kakun RR, Wasserman T, Korsensky L, Sternfeld O, Kagan J, Bublik DR, Aviel-Ronen S, Levanon K, et al. PAX8 activates a p53-p21-dependent pro-proliferative effect in high grade serous ovarian carcinoma. Oncogene. 2018;37:2213–2224. doi: 10.1038/s41388-017-0040-z. [DOI] [PubMed] [Google Scholar]
- 60.Di Palma T, Filippone MG, Pierantoni GM, Fusco A, Soddu S, Zannini M. Pax8 has a critical role in epithelial cell survival and proliferation. Cell Death Dis. 2013;4:e729. doi: 10.1038/cddis.2013.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Struyk AF, Canoll PD, Wolfgang MJ, Rosen CL, D’Eustachio P, Salzer JL. Cloning of neurotrimin defines a new subfamily of differentially expressed neural cell adhesion molecules. J Neurosci. 1995;15:2141–2156. doi: 10.1523/JNEUROSCI.15-03-02141.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gil OD, Zanazzi G, Struyk AF, Salzer JL. Neurotrimin mediates bifunctional effects on neurite outgrowth via homophilic and heterophilic interactions. J Neurosci. 1998;18:9312–9325. doi: 10.1523/JNEUROSCI.18-22-09312.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fagerberg L, Hallström BM, Oksvold P, Kampf C, Djureinovic D, Odeberg J, Habuka M, Tahmasebpoor S, Danielsson A, Edlund K, et al. Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics. Mol Cell Proteomics. 2014;13:397–406. doi: 10.1074/mcp.M113.035600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lin C, Lu W, Zhai L, Bethea T, Berry K, Qu Z, Waud WR, Li Y. Mesd is a general inhibitor of different Wnt ligands in Wnt/LRP signaling and inhibits PC-3 tumor growth in vivo. FEBS Lett. 2011;585:3120–3125. doi: 10.1016/j.febslet.2011.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lu W, Liu CC, Thottassery JV, Bu G, Li Y. Mesd is a universal inhibitor of Wnt coreceptors LRP5 and LRP6 and blocks Wnt/beta-catenin signaling in cancer cells. Biochemistry. 2010;49:4635–4643. doi: 10.1021/bi1001486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Inokuchi J, Komiya M, Baba I, Naito S, Sasazuki T, Shirasawa S. Deregulated expression of KRAP, a novel gene encoding actin-interacting protein, in human colon cancer cells. J Hum Genet. 2004;49:46–52. doi: 10.1007/s10038-003-0106-3. [DOI] [PubMed] [Google Scholar]
- 67.Fujimoto T, Koyanagi M, Baba I, Nakabayashi K, Kato N, Sasazuki T, Shirasawa S. Analysis of KRAP expression and localization, and genes regulated by KRAP in a human colon cancer cell line. J Hum Genet. 2007;52:978–984. doi: 10.1007/s10038-007-0204-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used and analyzed in this study are available from the corresponding author on reasonable request.