Abstract
Family factors are associated with suicidal behavior in youth, but little is known about how the joint influence of multiple family factors prospectively predicts onsets of suicidal ideation (SI) in adolescence, a developmental period characterized by increases in SI and risk for suicide. This study investigated whether parent history of SI interacted with either positive or negative parent-child relationship quality to longitudinally predict time to SI onsets during the transition into and across adolescence. Specifically, we used a longitudinal, multi-wave design and survival analyses to examine whether the interaction between these family factors prospectively predicted time to emergence of SI onsets (assessed at 6 month intervals over 3 years) in a community sample of youth ages 8 to 15 (N=238; 57% girls). Results supported an interaction effect, such that more negative relationship quality with parents predicted earlier emergence of SI among those youth whose parents had no history of SI. However, negative parent relationship quality did not amplify risk among youth with parent history of SI; all youth with a parent history of SI were more likely to experience earlier emergence of SI regardless of level of negative relationship quality. Findings did not support an interaction between low levels of parent-child positive relationship quality and parent history of ideation. Implications for the role of family factors in the etiology and prevention of SI are discussed.
Keywords: suicidal ideation, family factors, adolescence
Suicide rates have consistently increased since 1999, and suicide is the second leading cause of death among adolescents in the United States (ages 10–24; CDC, 2014; Curtin & Hedegaard, 2016). Suicidal ideation (SI) is a frequent precursor to suicide attempts and death by suicide is highly recurrent, and associated with significant health care costs (Klonsky, May, Saffer, 2016; Nock, 2016). Lifetime prevalence rates of SI begin to rise in early adolescence, and rapidly increase through late adolescence (Nock et al., 2013). Thus, it is important to better understand and predict the development of SI across adolescence.
Cross-sectional research over the last several decades has revealed a link between family factors and suicide risk, including family psychiatric history and family-environmental factors (e.g., family constellation, family relationships, Amitai & Apter, 2012; Brent & Melhem, 2008; Bridge, Goldstein, & Brent, 2007). However, still relatively little is known about the extent to which family influences may longitudinally predict the development of SI in youth. Moreover, the majority of studies to date have not combined independent sets of risk factors together into a single, coherent etiological risk model. In the current study, we investigated the joint influence of multiple family factors on the development of SI. Consistent with vulnerability-stress models of psychopathology, we examined whether parent history of SI interacted with parent-child relationship quality (RQ) to longitudinally predict time to SI onsets during the transition into and across adolescence.
Parent History of Suicidal Behavior and Youth Suicide Risk
Theory and research suggest that parent history of suicidal behavior may confer an affective, behavioral, or a neurocognitive vulnerability for suicide to offspring, and that this vulnerability may be at least partially heritable (Brent & Melhem, 2008). A number of cross-sectional adoption, twin, and family studies consistently show that suicidal behavior aggregates in families, and that risk for suicide is transmitted independently of other psychiatric disorders (for review see: Brent & Melhem; Geulayov, Gunnel, Holmen, & Metcalf, 2012). A few longitudinal studies further show that parent suicide attempts prospectively predict youth suicide attempts and/or ideation in high risk samples (e.g., offspring of parents with psychiatric illness; Brent, Melhem, & Oquendo, 2015; Connor et al, 2014; Melhem et al., 2007), and in community-based samples (Fergusson, Beautrais, & Horwood, 2003; Geulayov, Metcalf, Heron, Kidger, Gunnel, 2014; Lieb, Bronisch, Hofler, Schreier, & Wittchen, 2005). Taken together, research suggests that parent history of suicidal behavior is a precursor to youth suicidal behavior. However, little is known about the extent to which exposure to family-environmental factors, such as poor relationships with parents, may potentiate risk for the future development of SI among youth with a parent SI history.
Parent-Child Relationship Quality and Youth Suicide Risk
Relationships with parents undergo normative, developmental shifts as youth strive for autonomy (Larson, Richards, Moneta, Holmbeck, & Duckett, 1996). Many youth experience declines in quality of parent-child relationships around adolescence, including an increase in negative RQ and a decrease in positive RQ (Hazel et al., 2014; McGue, Elkins, Walden, & Iacono, 2005). Therefore, it is important to investigate the role of parent-child relationships in predicting SI during the adolescent period, when some youth encounter significant alterations in these relationships.
Cross-sectional studies have repeatedly shown that high levels of negative parent-child RQ, and low levels of positive RQ, are correlates of youth suicidal behavior across a wide range of cultures and countries (e.g., Fleming, Merry, Robinson, Denny, & Watson, 2007; Kim & Kim, 2008; McKinnon, Gariepy, Sentenac, & Elgar, 2016; Samm et al., 2010). Moreover, parent-child relationships characterized by high levels of positive qualities, such as warmth and connectedness, have been shown to be protective against suicidal thoughts and behaviors among youth at higher risk for suicide (e.g., victimized or indigenous youth; Borowsky, Taliaferro, & McMorris, 2013; Harder et al., 2012). There is also evidence that aspects of parent-child RQ (e.g., high levels of parent-child conflict, or low levels of parent-child connectedness or support) prospectively predicts youth SI and suicide attempts in a small handful of longitudinal studies in clinical (Czyz, Liu, & King, 2012; Miller, Esposito-Smythers, & Leichtweis, 2015), and community samples (Adrian, Miller, McCauley, & Vander Stoep, 2016; see King & Merchant, 2008 for a review), including four studies on the same nationally representative sample (Borowsky, Ireland, & Resnick, 2001; Kuramoto-Crawford, Ali, & Wilcox, 2017; Law & Shek, 2016; Nkansah-Amankra et al., 2012; Winfree & Jiang, 2010). Overall, research to date suggests that poor RQ (high negative or low positive relationship quality) is an especially important family-environmental factor that may contribute to the development of SI in adolescence, whereas high positive relationship quality may buffer against SI among those at risk.
Family Factors and Suicide Risk: An Integrative Vulnerability-Stress Model
Researchers investigating the role of familial transmission of suicide have speculated that suicidal behavior is transmitted from parents to offspring, and that this vulnerability may interact with environmental factors to increase the risk for suicide among youth (Brent & Melhem, 2008), consistent with vulnerability-stress models (Ingrid & Luxton, 2005). Thus, adolescents with a parent history of SI may be predisposed to experience ideation themselves, especially when these youth also encounter poor relationships with parents (Brent & Melhem, 2008). Yet, no study to our knowledge has examined whether parent history of SI interacts with family-environmental factors to predict youth SI.
Methodological Limitations of Past Research on Family Factors and Suicide Risk
Research investigating associations between family factors and suicide risk among adolescent youth have been limited in several ways. The large majority of studies have employed cross-sectional designs (e.g., Geulayov et al., 2012; McKinnon et al., 2016; see Bridge et al., 2006), which cannot investigate the temporal direction of the relationship between family factors and youth suicidal behavior. In addition, many studies have focused on clinical or high risk samples of youth (e.g., Czyz et al., 2012; Melhem et al., 2007; Miller et al., 2015). Given that these groups exhibit high levels of psychopathology and comorbidity, reliance on these samples is likely to introduce biases and limit generalizability compared to unselected, general community samples. Consequently, longitudinal, multi-wave studies using community samples to investigate family influences on youth suicidal behavior are needed. However, the few existing longitudinal, population based studies typically use two-time point designs and/or widely spaced assessment intervals (e.g., Kuramoto-Crawford et al., 2017; Lieb et al., 2005; O’Donnel, Stueve, Wardlaw, & O’Donnel, 2003). Further, a recent meta-analyses has shown that almost all longitudinal studies on suicide risk have focused on single risk factors over follow-up intervals that extend over a 5–10 year period; only 5% of studies have assessment intervals that are 6 months or less (Franklin et al., 2017). Consequently, we still have limited knowledge of more proximal, prospective predictors of suicidal behavior, and how multiple risk factors may work together to predict the emergence of SI over relatively short periods of time in adolescence.
Current Study
The primary goal of the current study was to advance understanding of the role of family factors in predicting onsets of SI across the adolescent developmental period. We examined whether the interaction between two family factors emphasized in the suicide risk literature would prospectively predict SI: parent history of suicidal behavior and parent-child RQ. We focused on parent SI history because SI is an understudied, but commonly occurring suicidal behavior. We used a longitudinal, multi-wave design and survival analyses to examine whether the interaction between parent SI history and parent-child RQ prospectively predicted time to youth onsets of SI (assessed at 6 month intervals over 3 years) in a community sample of youth during the transition into and across adolescence. Given that depression strongly predicts SI, we controlled for both parent and child clinical depression.
We hypothesized that youth with a parent history of SI would be more likely to develop SI earlier if they also experienced high levels of negative RQ with parents, or if they had low levels of positive parent-child RQ.
Methods
Participants
Children and adolescents were recruited by brief information letters sent home directly by the participating public school districts to families with a child in 3rd, 6th, or 9th grade. The letter stated that we were conducting a study on social and emotional development in children and adolescents and requested that interested participants call the laboratory to receive more information. We focused on 3rd, 6th, and 9th graders so that we could study the developmental transition from childhood through late adolescence over the course of the 3-year study. Approximately 2000 families were eligible to receive letters, and about 20% of these families contacted the lab. 362 participants were eligible and completed baseline measures for this study. 103 were excluded for incomplete parent data at baseline, or child data across follow-up assessments. Given evidence that parent history of suicidal behavior is most relevant for the suicidal behavior among biological offspring, we removed 18 participants because the participating parent was not a biological parent. Finally, 3 youth who reported current SI at baseline were excluded from analyses in order to longitudinally predict time to SI. Thus, the current analyses focused on 238 adolescents (136 or 57% girls; ages 8.4—15.9, M = 12.24) and participating parents (85% mothers). Most adolescents were Caucasian (81%), 6% were African American, 1% were Asian or Pacific Islander, and 12% classified themselves as Multi-racial or ‘other’. In addition, 6% reported Hispanic or Latino heritage. The majority of adolescents had parents who were married (81%), had completed college education or higher (54%), and came from homes with a family income above $40,000 (83%), whereas only 7% reported receiving food stamps. The sample demographics were representative of the broader population of the school districts from which the sample was drawn (Hankin et al., 2015).
Procedure
All procedures were approved by the university institutional review board. The parent and youth visited the laboratory for their baseline assessment. Parents provided informed written consent for their participation and for their child; youth provided written assent. During the baseline assessment, parents and youth completed a battery of questionnaires, and parents provided information about basic demographics. Additionally, youth and their parents were administered diagnostic interviews to assess for suicidal behavior and depression. Regular follow-up assessments were conducted every 6 months over the phone for 3 years (7 waves of data) to assess youth suicidal behavior.
Measures
Suicidal Ideation (SI).
SI was assessed by the Self -Injurious Thoughts and Behaviors Interview (SITBI; Nock, Holmberg, Photos, & Michel, 2007). This is a clinician-administered interview that assesses presence and frequency of a range of self-injurious thoughts and behaviors. The current study focused on the item inquiring about the presence of SI (“Have you ever had thoughts of killing yourself?”). This question resulted in a dichotomous variable indicating the presence or absence of SI. At baseline, parents were interviewed about their own and their child’s history of suicidal behavior, and youth were interviewed about themselves only. Parents and youth then reported on youth suicidal behavior within the past 6 months at each follow-up. Interviewers determined the presence of youth SI using best estimate diagnostic procedures (Klein et al., 2004). Discrepancies were reconciled using consensus meetings and clinical judgment, with the interviewer integrating child and parent-reports to arrive at a judgment that best represents the child’s suicidal behavior. The SITBI has excellent inter-rater reliability and test-retest reliability (Nock et al., 2007), and has been shown to be a valid measure for youth ages 7–16 (Barrocas, Hankin, Young, & Abela, 2012).
Depression diagnoses.
The Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (KSADS-PL; Kaufman et al., 1997) was used to assess for the presence of a DSM-IV (American Psychiatric Association, 1994) diagnosis of depression among youth. The KSADS is the most frequently used, most studied diagnostic interview with youth and has demonstrated strong evidence of reliability and validity (Klaufman et al., Klein, Dougherty, & Olino, 2005). At baseline, the youth and their parent were interviewed for a lifetime history of depression and for a current depressive disorder. Parents reported on their child’s depression, and youth reported on their own depression. Interviewers determined youths’ diagnostic status using best estimate procedures (Klein et al., 2004), as described earlier. Participants were deemed to have a depressive episode if they met DSM-IV criteria for Major Depressive Disorder Definite (MDD). Inter-rater reliability for the K-SADS, based on 15% of the sample interviews was good (kappa = .91).
The Structured Clinical Interview for DSM-IV Axis I disorders (SCID-I) was used to assess for a diagnosis of depression among parents. The SCID-I yields reliable diagnoses of depressive disorders (Zanarini et al., 2000) and is frequently used in clinical studies of depression in adults. Inter-rater reliability was good (Kappa = .87).
Parent-child Relationship Quality (RQ).
The Network of Relationships Inventory (NRI, Furman & Buhrmester, 1985) was used to assess parent RQ using a 13-item short form (Furman and Buhrmester, 2009). Participants responded to all 13 items for both their mother and father. The NRI is made up of two factors for each relationship: positive and negative RQ (Furman, 1996). 7 items assess positive qualities of relationships (e.g., “how much does this person help you figure out or fix things?”), and 6 items assessing negative qualities (e.g., “how much do you and this person get upset with or mad at each other?”). Positive and negative parent-child RQ composite scores were calculated by averaging mother- and father-child positive and negative RQ factors respectively. Prior studies have shown the NRI, including the short form, to be a valid measure of RQ among youth from ages 7 to 19 (Buhrmester & Furman, 1987; Furman & Buhrmester, 1992; Hazel et al., 2014).
Data Analytic Plan
SPSS statistical package (Version 24.0; IBM Corp., 2013) was used to conduct two separate multivariable Cox proportional hazard regressions to examine whether parent history of SI interacted with each parent-child RQ factor (negative and positive) to predict youth time to SI (scored as weeks) after baseline, with the occurrence of SI onset coded dichotomously (1= event). For each separate regression, parent history of SI, parent-child RQ, and covariates were entered on the first step, with the interaction term (parent SI × mother RQ) entered on the second step. We covaried for parent and youth history of MDD in all analyses.
Results
Descriptive Statistics
Of the 238 youth, 48 (20%) reported SI over the 3-year follow-up during the course of this study. These rates are higher than reported in cross-sectional studies in the general population (Nock et al., 2013), consistent with evidence that prevalence rates are higher when prospective, repeated measures are used compared to retrospective measures given at a single time-point (Hankin et al., 2015; Moffitt et al., 2010). Demographic group characteristics are presented in Table 1. Youth gender, age at baseline, and race were not associated with time to SI onset (lowest p = .13). Parents with a history of SI compared to parents without SI history had more negative parent-child RQ (M = 13.32 vs. M = 11.65), t(236)= −2.61, p < .05, and a trend towards lower positive RQ (M = 25.44 vs. M = 26.54), t(236)= −1.69, p = .093.
Table 1.
Sample characteristics and bivariate associations according to youth report of suicidal ideation after baseline assessment.
| Youth with Suicidal Ideation (n = 48) | Youth without Suicidal Ideation (n = 190) | χ2/t | |||
|---|---|---|---|---|---|
| Youth Demographics | |||||
| Age: mean, SD | 11.9 | 2.2 | 12.3 | 2.3 | 1.11 |
| Female: n, % | 31 | 65% | 105 | 55% | 1.36 |
| Caucasian: n, % | 40 | 83% | 139 | 73% | 2.13 |
| Black: n, % | 1 | 2% | 13 | 7% | |
| Asian/Pacific Islander: n, % | 0 | 0% | 2 | 1% | |
| Multi-racial/Other: n, % | 4 | 8% | 25 | 13% | |
| Hispanic: n, % | 3 | 7% | 11 | 6% | |
| Youth characteristics: n, % | |||||
| History of MDD | 8 | 17% | 4 | 2% | 16.97*** |
| History of Suicidal Ideation | 15 | 31% | 10 | 5% | 27.53*** |
| Family Demographics: n, % | |||||
| PP Biological Mother | 44 | 92% | 161 | 85% | 1.54 |
| PP Married | 41 | 85% | 151 | 80% | 0.87 |
| PP Education: ≥ BA | 28 | 58% | 126 | 67% | −.62 |
| Family Income, mean, SD | $89,750 | $43,995 | $95,073 | $65,007 | .53 |
| Family receives food stamps | 1 | 2% | 15 | 8% | 2.08 |
| Family characteristics: n, % | |||||
| PP History of Suicidal Ideation | 25 | 52% | 70 | 37% | 3.71 † |
| PP History of MDD | 17 | 35% | 50 | 26% | 1.57 |
| Neg. RQ: mean, SD | 13.8 | 5.7 | 12.0 | 4.3 | −2.05* |
| Pos. RQ: mean, SD | 25.7 | 5.2 | 26.2 | 4.9 | .59 |
Note: History of MDD= lifetime history of major depressive disorder; History of suicidal ideation = lifetime history of suicidal ideation; PP = participating parent; ≥ BA = completed Bachelor’s Degree from 4-year college or higher. Neg/Pos RQ = negative and positive parent-child relationship quality based on NRI subscales. All dichotomous variables were coded: 1 = present, 0= absent.
p = .05,
p < 0.05,
p < 0.001.
Vulnerability-Stress Model
Negative parent-child RQ × parent history of SI predicting time to youth SI onsets.
The negative parent-child RQ x parent history of SI interaction was significant, Wald = 4.95, p <.05, OR = 0.88 (see Table 2). To probe the nature of the effect, parent-child negative RQ was examined separately among youth with vs. without parental SI history (with covariates still present). Among youth with parent SI history, the effect of negative parent-child RQ on time to SI onset was not significant, Wald = 0.17, p = .678, OR = 0.98; there was no significant difference in time to onsets between youth with high negative RQ (M = 46 weeks) versus low negative RQ (M = 57 weeks; determined by a median split of RQ scores). In contrast, among youth without parent SI history, negative RQ was a significant predictor of time to SI onset, Wald = 5.98, p = < .05, OR = 1.12 (95% CI: 1.02 – 1.22), such that youth with high negative RQ had significantly shorter time to SI onset (M = 88 weeks) compared to youth with low levels of negative RQ (M = 109 weeks). This effect is depicted in Figure 1. Subsequent sensitivity analyses excluding youth with a history of SI showed that negative parent-child RQ continued to predict time to new SI onsets among youth without parent SI history, Wald = 4.61, p <.05. OR = 1.12.
Table 2.
Parent history of suicidal ideation × parent-child negative relationship quality predicting time to youth suicidal ideation onset.
| Predictor | B | SE | Wald | |
|---|---|---|---|---|
| PP History of SI | 2.25 | .86 | 6.82** | |
| Neg. RQ | .12 | .04 | 6.95** | |
| Neg. RQ × PP Hx of SI | −.13 | .06 | 4.95* | |
| PP Hx of MDD | .41 | .33 | 1.54 | |
| C Hx of MDD | 1.67 | .41 | 16.18*** |
Note. History of MDD= lifetime history of major depressive disorder; History of SI = lifetime history of suicidal ideation; PP = participating parent; Neg RQ = negative parent-child relationship quality. All dichotomous variables were coded: 1 = present, 0= absent.
p < 0.05,
p < 0.01,
p < 0.001
Figure 1.
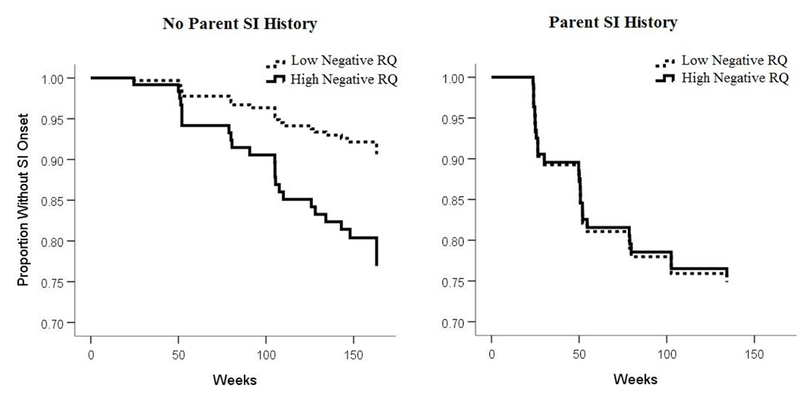
Parent history of suicidal ideation × negative parent-child relationship quality predicting youth suicidal ideation, onset.
Note Low/High Negative RQ = negative parent-child relationship quality based on NRI subscale.
Positive parent-child RQ × parent history of SI predicting time to youth SI onsets.
Positive parent-child RQ did not interact with parent SI history to predict timing to SI onsets, Wald = 0.02, p = .882, OR = 0.991. There was also no main effect of positive parent-child RQ on time to SI onset, Wald < 0.01, p = .972, OR = 1.00.
Discussion
We found that parent history of SI interacted with negative parent-child RQ to predict time to onsets of SI during the transition into and across adolescence. Specifically, higher negative parent-child RQ predicted earlier emergence of SI among those youth with no parent history of SI. However, negative parent-child RQ did not significantly amplify risk among youth with a parent SI history; youth with a parent SI history were at high risk for earlier emergence of SI regardless of levels of negative parent-child RQ. The interaction between negative parent-child RQ and parent SI history held even after controlling for both parent and child diagnoses of depression. Findings did not support an interaction between positive parent-child RQ and parent SI history.
The current study extends previous research in multiple ways. Prior studies have investigated parent history of suicidal behavior (Geulayov et al., 2012), and quality of parent-child relationships (Mckinnon et al., 2010) as separate risk factors for suicidal behavior. Further, most of these studies have been limited by cross-sectional designs (McKinnon et al., Geulayov et al.), or using two-time point designs or widely spaced assessment intervals (i.e., several years, Kuramoto-Crawford et al., 2017; Lieb et al., 2005; O’Donnel, Stueve, Wardlaw, & O’Donnel, 2003). The current study advances knowledge of the prediction of suicide risk within shorter time frames by integrating these two important family factors into a single model and using a rigorous multi-wave design that included repeated assessments of SI every 6 months in a community sample of youth. Our results suggest that the combination of parent SI history and negative parent-child RQ may enhance the prediction of youth SI onsets within the immediate weeks to months.
Findings also inform understanding of the role of family factors in the etiology of SI and interventions for youth. Our results suggest that for youth with no parent history of SI, the family environment may play an especially prominent role in the development of SI onsets. Thus, prevention efforts aimed at reducing negative qualities within parent-child relationships may be especially effective at preventing the development of future SI for youth with no parent SI history. Findings suggest that efficacious family therapies targeting parent-child relationships and parenting behaviors for youth with self-injurious behaviors, such as Resourceful Adolescent Parent Program (RAP-P) or attachment-based family therapy (ABFT; Glenn, Franklin, & Nock, 2015) might be especially promising for preventing the development of SI among youth with no parent SI history during the adolescent period.
On the other hand, SI onsets occurred earlier, and were more prevalent, among all offspring of parents with SI history, regardless of parent-child RQ. A somber implication of this finding is that targeting parent-child RQ among these families may be insufficient to reduce risk for future SI onsets. We posit that the mechanisms through which vulnerability for SI is transmitted from parents to offspring are likely complex, and thus call for a multi-faceted approach to intervention. Specifically, interventions may require targeting youth risk behaviors that may have possibly been inherited from parents (e.g., neurocognitive, emotion regulation, or other neurobiological deficits), in addition to potential family-environmental factors (e.g., parent modeling of maladaptive coping responses, parent suicidal thoughts or behaviors (Brent & Melhem, 2008).
Although we hypothesized that negative RQ would amplify risk for SI onsets among youth with a parent SI history, consistent with a more traditional, “synergistic” type of vulnerability-stress model, results are more in line with a “titration” vulnerability-stress interaction in which high levels of one factor may compensate for low levels of another factor (Abramson et al., 2002). Specifically, youth with no parent SI history are still at risk for SI if they have negative family-environments, particularly high levels of negative RQ with parents. Likewise, youth with low levels of negative RQ with parents are still at high risk for SI if they have a parent history of SI. Therefore, findings are in line with a vulnerability-stress interaction model, although in a different way than hypothesized.
In contrast to negative parent-child RQ, positive RQ did not interact with parent SI history to predict time to youth SI onsets. Therefore, low levels of positive RQ did not exacerbate, or high levels of positive RQ buffer against, the effects of parent history of SI. Follow-up analyses further showed that there was also no main effect of positive RQ on time to ideation onset. Although previous cross-sectional research has found that low levels of positive relationship characteristics (e.g., support, connectedness) within parent-child relationships are frequent correlates of youth suicidal behavior (Borowsky, Resnick, Ireland, & Blum 1999; Mckinnon et al., 2016; Miller, Esposito-Smythers, & Leicthweis, 2015), our findings did not support that positive parent-child RQ is an antecedent to youth SI. One possibility is that decreases in positive quality may be a consequence, rather than predictor, of youth SI. Youth who are contemplating suicide may be less communicative and spend less time with parents, which may lead to decreases in positive parent-child RQ.
The limitations of the current study need to be considered when interpreting findings. Education and income levels in this community sample were higher than national averages (United States Census Bureau, 2010), which may limit generalizability of findings. In addition, we focused on SI because it is the most common form of suicidal behavior among youth, and an antecedent to more lethal suicidal behavior (Nock et al., 2013; 2016). Yet, many youth who experience SI do not go on to attempt suicide (Nock et al., 2013). Given the low base rate of suicide attempts, we were limited by the low power to predict attempts among ideators. Future research is needed to better investigate the role of family factors in processes that contribute to the transition from SI to attempts. Another limitation of this study, and many other studies examining associations between parent factors and youth suicide risk, is that parent history information was obtained about one parent only. More comprehensive assessments that include both parent informants may further enhance our understanding of how the interaction between parent history of suicidal behavior and family-environmental factors may relate to youth suicide risk. This study also focused on a single family-environmental factor (i.e. parent-child relationship quality). However, other aspects of the family environment, such as household income, single versus multiple parent household, etc. may also interact with parent SI history. In addition, this study focused on parent history of SI only. Future multi-wave, longitudinal investigations should examine potential temporal associations between parent and youth suicidal ideation over time. Future research should also investigate mechanisms through which family factors may contribute to youth suicide risk. Both environmental (e.g., parent modeling), and heritable, intermediate phenotypes, may account for the intergenerational transmission of SI and suicidal behavior (Brent et al., 2015; Brent & Melhem, 2008; McGirr, Séguin, Cabot, Lesage, & Turecki, 2009). We further speculate that negative relationships with parents could invoke intense, negative affective responses, in line with models of suicide that highlight the role of intense distress that occurs within the context of social relationships (King & Merchant, 2008; Van Orden et al., 2010). In sum, findings from this study are another step towards understanding suicide risk in adolescence, and highlights the need for additional research on how family factors may contribute to suicidal behaviors.
Acknowledgments
This research was supported by funding from the National Institute of Mental Health (R01MH077195, K01MH109850).
Footnotes
The authors declare that they have no conflict of interest.
References
- Abramson LY, Alloy LB, Hankin BL, Haeffel GJ, MacCoon DG, & Gibb BE (2002). Cognitive vulnerability–stress models of depression in a self–regulatory and psychobiological context In Gotlib IH, & Hammen CL (Eds.), Handbook of depression (pp. 268–294). New York: Guilford. [Google Scholar]
- Adrian M, Miller AB, McCauley E, Stoep AV (2016). Suicidal ideation in early to middle adolescence: sex-specific trajectories and predictors. Journal of Child Psychiatry and Psychology, 57, 645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Association. [Google Scholar]
- Amitai M, & Apter A (2012). Social aspects of suicidal behavior and prevention in early life: A review. International Journal of Environmental Research and Public Health, 9, 985–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, & Carlson G (1988). Suicide attempts in preadolescent child psychiatry inpatients. Suicide and Life-Threatening Behavior, 18, 129–136. doi: 10.1111/j.1943-278X.1988.tb00147.x [DOI] [PubMed] [Google Scholar]
- Barrocas AL, Hankin BL, Young JF, & Abela JRZ (2012). Rates of non-suicidal injury in youth: Age, sex, ad behavioral methods in a community sample. Pediatrics, 130, 39–45. doi: 10.1542/peds.2011-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borowsky IW, Resnick MD, Ireland M, & Blum RW (1999). Suicide attempts among American indian and Alaska native youth. Archives of Adolescent and Pediatric Medicine, 153, 573–580. [DOI] [PubMed] [Google Scholar]
- Brent D, & Melhem N (2008). Familial transmission of suicidal behavior. Psychiatric Clinics of North America, 31, 157–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, & Melhem N, & Oquendo M (2015). Familial pathways to early-onset suicide attempt: A 5.6 year prospective study. JAMA Psychiatry, 72, 160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, & Brent DA (2006). Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry, 47, 372–394. [DOI] [PubMed] [Google Scholar]
- Buhrmester D, & Furman W (1987). The development of companionship and intimacy. Child Development, 58, 1101–1113. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2014). NCfIPaC. Web-based Injury Statistics Query and Reporting System. Available from: http://webappa.cdc.gov.
- Connor KR, Bossarte RM, Lu N, Kaukeinen K, Chan G, Wyman P…Hesselbrock VM (2014). Parent and child psychopathology and suicide attempts among children of parents with alcohol use disorder. Archives of Suicide Research, 18, 117–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtin SC, Warner M, & Hedegaard H (2016). Increase in suicide in the United States, 1999–2014 NCHS Data Brief, 241 Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Czyz EK, Liu Z, & King CA (2012). Social connectedness and on-year trajectories among suicidal adolescents following psychiatric hospitalization. Journal of Clinical Child and Adolescent Psychiatry, 41, 214–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Beautrais AL, & Horwood J (2003). Vulnerability and resiliency to suicidal behaviors in young people. Psychological Medicine, 33, 61–73. [DOI] [PubMed] [Google Scholar]
- Fleming TM, Merry SN, Robinson EM, Denny SJ, & Watson PD (2007). Self-reported suicide attempts and associated risk and protective factors among secondary school students in New Zealand. Australian and New Zealand Journal of Psychiatry, 41, 213–221. doi: 10.1080/00048670601050481. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X…Nock MK (in press). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin. [DOI] [PubMed] [Google Scholar]
- Furman W, & Buhrmester D (1985). Children’s perceptions of the personal relationships in their social networks. Developmental Psychology, 21, 1016–1024. [Google Scholar]
- Furman W, & Buhrmester D (1992). Age and sex differences in perceptions of networks of personal relationships. Child Development, 63, 103–115. [DOI] [PubMed] [Google Scholar]
- Furman W & Buhrmester D (2009). Methods and measures: The network of relationships inventory: The behavioral systems inventory. International Journal of Behavioral Development, 33, 470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geulayov G, Gunnel D, Holmen TL, & Metcalfe C (2012). The association of parental fatal and non-fatal suicidal behavior with offspring suicidal behavior and depression: A systematic review and meta-analyses. Psychological Medicine, 42, 1567–1580. [DOI] [PubMed] [Google Scholar]
- Geulayov G, Metcalf C, Heron J, Kidger J, & Gunnel D (2014). Parental suicide attempt and offspring self-harm and suicidal thoughts: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort. Journal of the American Academy of Child and Adolescent Psychiatry, 53, 509–517. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Franklin JC, & Nock MK (2015). Evidence-based psychosocial treatments for self-injurious thoughts and behaviors in youth. Journal of Clinical Child and Adolescent Psychology, 44, 1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, Gulley L…Oppenheimer CW (2015). Depression from childhood into late adolescence: Journal of Abnormal Psychology, 124, 803–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazel N, Oppenheimer CW, Technow J, Young J, & Hankin BL (2014). Parent relationship quality buffers against the effect of peer stressors on depressive symptoms from middle childhood to adolescence. Developmental Psychology, 50, 2115–2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P…Ryan N (1997). Schedule for affective disorders and schizophrenia for school-aged children – present and lifetime version (KSADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Kim HS, & Kim HS (2008). Risk factors for suicide attempts among Korean adolescents. Child Psychiatry and Human Development, 39, 221–235. [DOI] [PubMed] [Google Scholar]
- King CA, & Merchant CR (2008). Social and interpersonal factors relating to adolescent suicidality: A review of the literature. Archives of Suicide Research, 12, 181–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Segal HG, Naylor M, & Evans T (1993). Family functioning and suicidal behavior in adolescent inpatients with mood disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 1198–1206. [DOI] [PubMed] [Google Scholar]
- Klein DN, Dougherty LR, & Olino TM (2005). Toward guidelines for evidence-based assessment of depression for children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34, 412–432. [DOI] [PubMed] [Google Scholar]
- Klein DN, Shankman SA, Lewinsohn PM, Rohde P, & Seeley JR (2004). Family study of chronic depression in a community sample of young adults. American Journal of Psychiatry, 161, 646–653. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, May AM, & Saffer BY (2016). Suicide, suicide attempts, and suicidal ideation. Annual Review of Clinical Psychology, 12, 307–330. [DOI] [PubMed] [Google Scholar]
- Kuramoto-Crawford SJ, Ali M, & Wilcox HC (2017). Parent-child connectedness and long term risk for suicidal ideation in a nationally representative sample of US adolescents. Crisis, 38, 309–318. doi: 10.1027/0227-5910/a000439. [DOI] [PubMed] [Google Scholar]
- Ingram RE, & Luxton DD (2005). Vulnerability-stress models In Hankin BL & Abela JRZ (Eds.), Development of psychopathology: A vulnerability-stress perspective(pp. 245–288). Thousand Oaks, California: Sage Publications. [Google Scholar]
- Larson RW, Richards MH, Moneta G, Holmbeck G, & Duckett E (1996). Changes in adolescents’ daily interactions with their families from ages 10 to 18: Disengagement and transformation. Developmental Psychology, 32, 744–754. [Google Scholar]
- Law BMF & Shek DTL (2016). A 6-year longitudinal study of self-harm and suicidal behaviors among chinese adolescents in Hong Kong. Journal of Pediatric and Adolescent Gynecology, 29, S38–S48. 10.1016/j.jpag.2015.10.007. [DOI] [PubMed] [Google Scholar]
- Lieb R, Bronisch T, Hofler M, Schreier A, & Wittchen H (2005). Materinal suicidality and risk of suicidality in offspring: Findings from a community study. The American Journal of Psychiatry, 162, 1665–1671. [DOI] [PubMed] [Google Scholar]
- McGue M, Elkins I,Walden B, & Iacono WG (2005). Perceptions of parent-adolescent relationship: A longitudinal investigation. Developmental Psychology, 41, 971–984. [DOI] [PubMed] [Google Scholar]
- McKinnon B, Gariepy G, Sentenac M, & Elgar FJ (2016). Adolescent suicidal behaviors in 32 low- and middle-income countries. Bulletin of the World Health Organization, 94, 340. doi: 10.2471/BLT.15.163295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melhem NM, Brent DA, Ziegler M, Iyengar Z, Kolko D, Oquendo M…Mann J (2007). Familial pathways to early-onset suicidal behavior: Familial and individual antecedents to suicidal behavior. The American Journal of Psychiatry, 164, 1364–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, Esposito-Smythers C, & Leichtweis RN (2015). Role of social support in adolescent suicidal ideation and suicide attempts. Journal of Adolescent Health, 56, 286–292. doi: 10.1016/j.jadohealth.2014.10.265. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, & Poulton R (2010). How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine, 40, 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkansah-Amanktra S, Deidhio A, Agbanu SK, Agbanu HLK, Opoku-Adomako NS, Twumasi-Ankrah P (2012). A longitudinal evaluation of religiosity and psychosocial determinants of suicidal behaviors among a population-based sample in the United States. Journal of Affective Disorders, 139, 40–51. 10.1016/j.jad.2011.12.027. [DOI] [PubMed] [Google Scholar]
- Nock MK (2016). Recent and needed advances in the understanding, prediction, and prevention of suicidal behavior. Depression and Anxiety, 33, 460–463. [DOI] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson BA, Zaslavsky AM, & Kessler RC (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the national comorbidity survey replication adolescent supplement. JAMA Psychiatry,70, 300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-injurious thoughts and behaviors interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19, 309–317. [DOI] [PubMed] [Google Scholar]
- Oppenheimer CW, & Hankin BL (2011). Relationship quality and depressive symptoms among adolescents: A short-term multi-wave investigation of longitudinal, reciprocal associations. Journal of Clinical Child and Adolescent Psychology, 40, 486–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samm A, Tooding L, Siasask M, Kolves K, Aasvee K, & Varnik A (2010). Suicidal thoughts and depressive feelings amongst Estonian schoolchildren: Effect of family relationship and family structure. European Child and Adolescent Psychiatry, 19, 457–468. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau (2010). QuickFacts: Denver County, Colorado. Available from https://www.census.gov/quickfacts/fact/table/denvercountycolorado,denvercitycolorado,CO/RHI125216#viewtop.
- Wagner BM (1997). Family risk factors for child and adolescent suicidal behavior. Psychological Bulletin, 12, 246–298. [DOI] [PubMed] [Google Scholar]
- Winfree LT, & Jiang S (2010). Youthful suicide and social support. Youth Violence and Juvenile Justice, 8, 19–37. [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithewaite SR, Selby EA, & Joiner TE (2010). The interpersonal theory of suicide. Psychological Review, 117, 575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]


