Abstract
Purpose:
The purpose of this study was to identify and prioritize the information that persons living with HIV (PLWH) in a limited-resource setting need to effectively manage their health.
Design and Methods:
A data sources triangulation method was used to compare data from three separate sources: (a) 107 interviews with Spanish-speaking PLWH being seen at a healthcare clinic in the Dominican Republic (DR); (b) 40 interviews with Spanish-speaking healthcare providers from the same clinic in the DR; and (c) an integrative literature review of English- and Spanish-language articles that assessed the health information needs of PLWH in Latin America and the Caribbean. We compared information needs across sources and developed a prioritized list of the topics important to provide PLWH in a clinical setting.
Findings:
Triangulation identified the most important topics for HIV-related health education for PLWH as medication and adherence, followed by transmission, including risks and prevention strategies, mental health management, and knowledge of HIV in general.
Conclusions:
The identification of evidence-based health education priorities establishes a guide that healthcare providers may use to help PLWH effectively manage their health and creates a foundation from which further studies on improving clinical interactions may be generated.
Clinical Relevance:
Using the priorities identified, nurses and other health educators can improve patient education, and consequently self-management, by making evidence-based choices about what information to provide to their patients.
Keywords: Data triangulation, Dominican Republic, health education, HIV, information needs
Linking and engaging persons living with HIV (PLWH) with healthcare services and ensuring adherence to antiretroviral therapy (ART) remain challenges to HIV management globally (Simoni et al., 2017). In the Dominican Republic (DR), HIV prevalence has steadily declined since the mid-1990s, when ART coverage became widespread, and remains stable at approximately 1% among the general population (De Boni, Veloso, & Grinsztejn, 2014). However, HIV prevalence is much higher (up to 11%) in high-risk populations, such as men who have sex with men, transgender women, or those living in rural communities (Johnston, Vaillant, Dolores, & Vales, 2013; Rojas, Malow, Ruffin, Rothe, & Rosenberg, 2011). Lack of management among institutions, limitations of government programs, and constrained resources create substantial barriers to the development and maintenance of uniform, high-quality healthcare services in the DR (Rojas et al., 2011). Consequently, considerable differences in treatment and prevention programs exist across geographic regions, with main treatment and education centers in the larger, urban areas. An added barrier to effective HIV care in the DR is the presence of heavy stigma, as HIV is associated with either being unfaithful to a partner or with homosexuality, which affects willingness to seek care and disclose status (Castro, et al., 2014; Johnston et al., 2013; Luft & Larson, 2017). Additionally, the DR’s appeal as a sexual tourism destination heightens vulnerability to infection through increased risk behaviors such as transactional sex, drug and alcohol use, and number of sexual partners (Castro et al., 2014; Guilamo-Ramos et al., 2015; Padilla, Guilamo-Ramos, Bouris, & Reyes, 2010). High rates of poverty also contribute to HIV susceptibility in the DR, as lack of employment opportunities can lead to migration to tourist centers, limit access to education and information, and transportation to, or payment for, healthcare services may be cost prohibitive (Padilla et al., 2010; Rojas et al., 2011). Furthermore, in the DR, the predominant method of HIV transmission is unprotected heterosexual contact, which likely indicates a lack of sufficient treatment and prevention information nationally (García, Bayer, & Cárcamo, 2014; Rojas et al., 2011).
Self-management may be referred to as “the ability of an individual, in conjunction with family, community, and health care professionals, to manage symptoms, treatments, and lifestyle changes” (Mackey, Doody, Werner, & Fullen, 2016, p. 1). It is a critical component of chronic disease management and a key priority for nursing practice and research (National Institute of Nursing Research, 2016). Unfortunately, the effective self-management of HIV is particularly challenging as it is a complex chronic condition that requires patients to obtain and understand large amounts of health information in order to successfully complete health management activities (Millard, Elliott, & Girdler, 2013). For instance, to achieve optimal treatment adherence, PLWH must know where to access medication, have the resources to get there, learn to take the medications (timing, with or without food, etc.), and know how to handle side effects while managing any other health conditions and responsibilities. Additionally, HIV-related symptoms may present another unique set of challenges for self-management (Iribarren et al., 2018). Barriers to obtain the information needed for effective self-management in limited-resource settings, such as the DR, are numerous, since services may be difficult to access, language and cultural differences and stigma are present, and patients’ limited educational backgrounds and low health literacy are likely to complicate healthcare interactions (Gebre, Forbes, & Peters, 2016; Rojas et al., 2011). Given these vast information needs and numerous sociocultural challenges to obtaining that information, health education interventions must be appropriately tailored to meet patients’ needs in order to improve their HIV self-management behaviors (Gakumo, Enah, Vance, Sahinoglu, & Raper, 2015).
The specific information patients need for effective self-management is not well established in the literature. The clinical encounter is a critical time for sharing information to teach, motivate, and reinforce self-management for PLWH, but a limited evidence base to guide what information or educational topics patients need make it difficult for providers to know what information to share (Swendeman, Ingram, & Rotheram-Borus, 2009). Systematic reviews and frameworks of self-management interventions for PLWH, or those with other chronic illnesses, may include techniques and skills that patients must master, but typically do not include specific health information topics (Millard et al., 2013; Swendeman et al., 2009). Other studies to guide HIV self-management have focused on specific topics, such as symptom management and the strategies to manage them (Iribarren et al., 2018). However, the current literature provides little evidence of what information would be the most useful to PLWH living in limited-resource settings to improve their self-management behaviors. Thus, the purpose of this study was to identify and prioritize the most important information to share with PLWH in limited-resource settings to enable effective self-management. This research fills this substantial gap in the literature by establishing evidence-based and prioritized self-management education topics that healthcare providers can use to guide what information they share with patients.
Methods
This study was conducted with a data sources triangulation method, a research methodology that can reveal diverse dimensions of data, ensure completeness of findings, and confirm results (Begley, 1996; Fenech Adami & Kiger, 2005). In data sources triangulation, multiple data sources focusing on the same research question that vary by time, place, or person are collected and compared (Hussein, 2015; Thurmond, 2001). This combination and comparison of data from various sources can ensure comprehensiveness and overcome deficiencies or biases that can arise from a single study or data source (Hussein, 2015; Mitchell, 1986).
Three data sources were included in data sources triangulation for this study: (a) perspectives of PLWH, (b) perspectives of healthcare providers who provide clinical services to PLWH, and (c) the scientific literature. Data representing the perspectives of PLWH and scientific literature review were collected during preliminary studies (Stonbraker & Larson, 2016; Stonbraker et al., 2017). These three data sources were selected for data sources triangulation because, in order to determine what information PLWH need to facilitate effective self-management, input from both patients and healthcare providers must be included, as each may have varying perspectives regarding what information is needed and when (Hartzler & Pratt, 2011). Furthermore, including the target population during intervention or guideline development can ensure more effective results and minimize barriers between patients and their providers (Solomon, O’Brien, Baxter, MacLachlan, & Robinson, 2016). Then, by comparing the more subjective findings of providers and patients with the more objective findings from the literature, it is possible to ensure findings are comprehensive and evidence based.
Ethical Approval
All research activities involving human subjects were approved by both the Columbia University Institutional Review Board and the Consejo Nacional de Bioética en Salud (CONABIOS), the ethical review committee in the DR.
Study Setting
Interviews with patients and healthcare providers took place at Clínica de Familia in La Romana, DR. Founded in 2004 through Columbia University’s International Family AIDS Program, Clínica de Familia is a primary care clinic located on the southeast coast. It is now an independently licensed Dominican nongovernmental organization that provides free treatment and support services to more than 2,000 PLWH annually, making it the third largest HIV treatment center in the DR (Clínica de Familia, 2015).
Data Sources
Interviews with PLWH.
Interviews were conducted in Spanish with 107 PLWH in autumn 2015 as part of a separate study that used a survey to assess participants’ information behavior. The full study methodology is reported elsewhere (Stonbraker et al., 2017), but in brief, the survey instrument that guided interviews was developed based on Wilson’s model of information behavior and assessed how individuals need, seek, and use health information (Wilson, 1999). During recruitment, healthcare providers referred eligible participants (adults ≥18 years of age, Spanish speaking, and living with HIV) to speak to the on-site researcher (S.S.). Individuals who were not able to provide informed consent or were Creole speaking were excluded. The on-site researcher further explained the study, obtained verbal informed consent, and conducted interviews using the survey. Participants’ responses were recorded in REDCap, an electronic database hosted at Columbia University (Harris et al., 2009). Data included in the triangulation process for the current study were participants’ answers to the question, “What have been the two most helpful things that you have learned to help you with your HIV?” with the prompt, “or what has helped you the most?” Patients were encouraged to give two responses, and up to three were recorded.
Interviews with healthcare providers.
Data were collected from healthcare providers for the current triangulation analysis. For recruitment, administrators at the clinic identified eligible providers (adults ≥18 years of age and Spanish speaking). To ensure comprehensive findings that included interdisciplinary viewpoints, all employees who provide services to adult PLWH were eligible. A member of the research team contacted potential participants, and interested providers were scheduled for an individual interview. Providers who do not directly interact with PLWH were excluded. Interviews were conducted in Spanish in February 2017 by three bilingual researchers using an interview guide to collect basic demographic information and explore providers’ perceptions of the most important information to provide PLWH. Questions were designed to elicit parallel information to the data obtained in interviews with PLWH. For example, providers were asked, “What do patients say are the two most useful things that they have learned to help them with their HIV?” Providers were also asked what information they think is the most important to provide PLWH during a clinical encounter. All interviewers were trained in the interviewing techniques that were used during interviews with PLWH, and mock interviews were conducted to ensure questions were uniformly understood and administered across interviews. Responses from provider interviews were also recorded in REDCap.
Scientific literature.
An integrative literature review was conducted to identify published literature that reported health information needs of PLWH in Latin America or the Caribbean. The full methodology of this study is reported elsewhere (Stonbraker & Larson, 2016), but to summarize, English- and Spanish-language searches were conducted in six databases to identify studies that explored or measured patients’ perspectives on their health information needs. The quality of each included article was assessed, and relevant characteristics were extracted and compared (Stonbraker & Larson, 2016). For the current study, the literature was reviewed to ensure that no new articles had been published since initial searches.
To complement the review, a search of the websites and online publications of the following HIV-related research and service organizations were conducted: World Health Organization (WHO), United Nations Educational, Scientific, and Cultural Organization’s action against HIV/AIDS (EDUCAIDS) program, Joint United Nations Programme on HIV/AIDS (UNAIDS), U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), Centers for Disease Control and Prevention (CDC), and the Health Resources & Services Administration’s (HRSA’s) National HIV/AIDS Strategy and Global HIV/AIDS programs.
Data Triangulation
Conventional content analysis was used to iteratively code responses from patient and provider interviews. Codes were arranged by the main topic of responses to questions and were then further organized into categories of health information needs according to meaning (White & Marsh, 2006). Coding was done in Spanish by one bilingual researcher (S.S.) and then verified by a second bilingual researcher (S.R.) to enhance dependability of findings (Thomas & Magilvy, 2011). Discrepancies were discussed until consensus was reached. Frequencies of responses from final categories were calculated and compared. The credibility of qualitative findings was established through peer debriefing at clinic meetings and through prolonged and varied time spent with participants, interview techniques, and transcripts (Thomas & Magilvy, 2011). Transferability was established through thorough description of the population studied and representative samples of patients and providers (Thomas & Magilvy, 2011). Final categories were prioritized based on the combined frequency of patient and provider responses and were subsequently compared with the findings from the literature to confirm results and ensure a comprehensive list had been generated. Final categories were translated to English for this report. Translations were performed by the first author (S.S.), who is bilingual in English and Spanish, and were then independently confirmed by two other co-authors (S.R., M.H.), who are also bilingual English and Spanish speakers.
Results
Survey Results From PLWH
Demographic characteristics.
The demographic characteristics of 107 participants living with HIV were reflective of the PLWH population at the clinic and are fully reported elsewhere (Stonbraker et al., 2017). Briefly, participants had an average age of 40.8 years (range = 19–75), had been living with HIV for an average of 7.7 years (range = 0.17–20), were mostly female (59.8%), and lived in La Romana (57.9%).
Most useful information for health management.
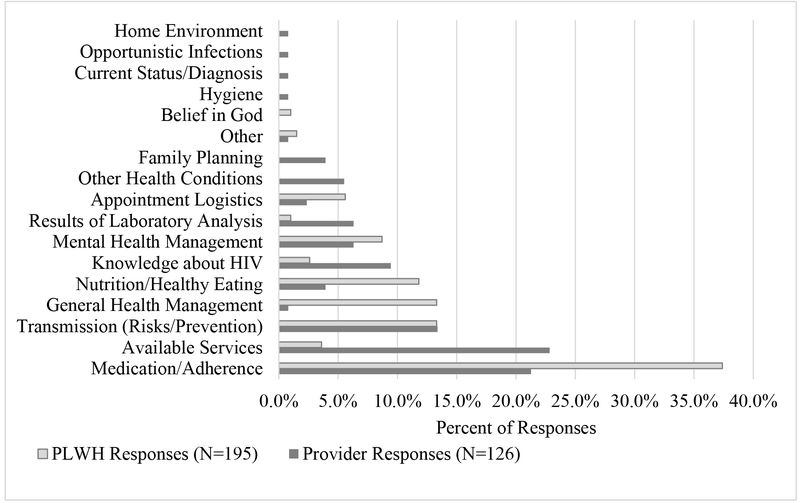
PLWH provided 195 responses about the most useful information to manage HIV. The most commonly identified topic was medication or adherence (37.4%, Figure 1), which patients described as “how to take my medication” or “to always take my medications on time.” Prevention or transmission, such as “use condoms so as not to infect others,” and general health management, such as “you have to take care of yourself,” were the next most commonly identified topics, with each category receiving 13.3% of responses. Information about nutrition or healthy eating was the fourth most common topic, with 11.8% of responses. Mental health management, appointment logistics, and services offered at the clinic were other topics identified. The only topic that PLWH mentioned as helpful that was not noted by providers was belief in God.
Figure 1.
The most useful information for self-management according to persons living with HIV (PLWH) and their healthcare providers.
Survey Results From Healthcare Providers
Demographic characteristics.
A majority of the 40 providers who completed interviews were female (90%), and the average age was 38.2 years (range = 25–62). The average time they had worked in health care was 10.9 years (range = 2–33) and the average length of time they had worked at the clinic was 5.2 years (range = 0.25–25). Respondents comprised eight physicians (20%), eight community health promoters (20%), seven nurses (17.5%), five medical specialists (12.5%), four counselors (10%), three research and program monitoring staff (7.5%), two pharmacy auxiliary staff (5%), two social services workers (5%), and one psychologist (2.5%).
Most useful information for self-management.
Providers gave 126 responses regarding what information they think patients find to be the most useful to manage HIV. Services offered at the clinic, which included quotes such as “that we [the Clinic] offer transportation assistance” or “that they can find free medications here” was the most commonly identified topic, with 22.8% of responses (see Figure 1). Medication or adherence, described as “the importance of medications” or simply “adherence,” was the second most commonly identified topic, with 21.3% of responses. Prevention or transmission was the next most common topic, with 13.4% of responses and was described by providers as “methods of transmission and how to prevent HIV” or “the prevention of sexually transmitted infections.” The next most useful reported topics by providers were knowledge about HIV, mental health management, results of laboratory analysis, and other health conditions. Healthcare providers identified several topics that they thought PLWH would find useful that none of the PLWH mentioned, such as other health conditions, family planning, hygiene, opportunistic infections, the home environment, and knowing current status or diagnosis.
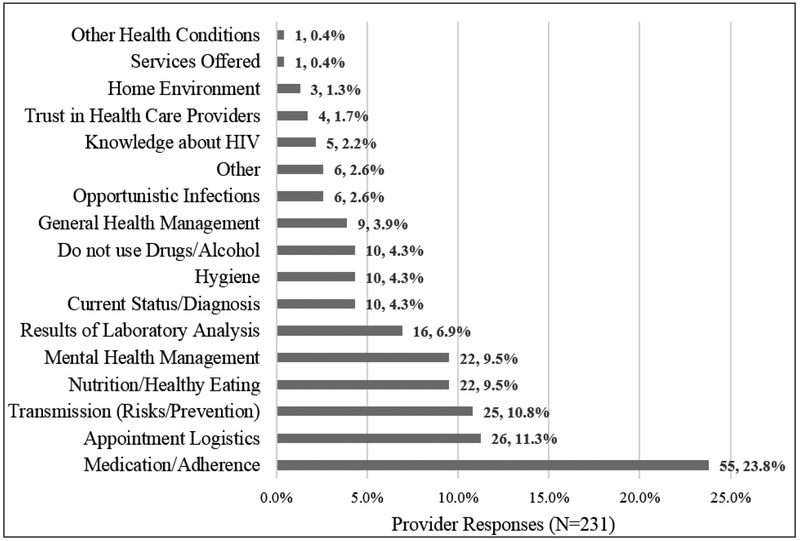
Information most important to teach during a clinical encounter.
There was little consensus about what should be taught to patients during a clinical encounter. Of the 231 responses provided, medication or adherence was the most commonly identified topic (23.8%, Figure 2), but was reported by less than one fourth of the healthcare providers. The next most identified topics were appointment logistics (11.3%), transmission (10.8%), nutrition or healthy eating (9.5%), and mental health management (9.5%). Notably, what providers identified as the most important information to teach patients was not the same as what they thought patients would find to be the most useful. For instance, over 20% of provider responses indicated that available services for PLWH would be the most useful information, but only one provider (0.4% of responses) indicated that was an important topic to teach during a clinical visit.
Figure 2.
The most important information to teach patients during a clinical visit according to healthcare providers.
Scientific Literature
A detailed report of the literature review can be found elsewhere (Stonbraker & Larson, 2016), but in summary, 11 articles from 8 out of 33 countries met inclusion criteria. From these studies, the predominant information needs of PLWH in Latin America and the Caribbean were identified as information about HIV in general (including symptoms, illness trajectory, and laboratory results), more knowledge about HIV medications, and information about other sexually transmitted infections or about secondary (opportunistic) infections. How to modify one’s lifestyle following a positive diagnosis, methods of effective communication with providers and friends or family members, and effective coping mechanisms were also identified as information needs (Stonbraker & Larson, 2016). Additional searches conducted for this study did not find any new publications on the information needs of PLWH.
Numerous guidelines on treatment, self-testing, partner notification, management of opportunistic infections, and monitoring of the global response were identified in websites and reports searched (CDC, 2017; PEPFAR, 2017; WHO, 2017). Evaluation guidelines for prevention and treatment programs, frameworks for action, global plans to eliminate HIV infections, and reports detailing risk factors and characteristics of high-risk populations were other components of online materials (CDC, 2017; UNAIDS, 2017a, 2017b; EDUCAIDS, 2017). The HRSA’s Ryan White HIV/AIDS Program has numerous AIDS Education and Training Centers supported through a network of over 8 regional, 3 national, and 11 international centers (none located in the Caribbean), with 130 local affiliated sites to conduct targeted multidisciplinary education and training programs for healthcare providers treating PLWH (HRSA, 2017). Their website (https://www.aidsetc.org/) includes a thorough topic list, but it does not specify what information may be important to share in a clinical encounter. Of sites searched, only the U.S. Department of Health and Human Services’ (HHS’s) 2014 guide for HIV/AIDS clinical care identified educational topics related to HIV (HHS, 2014). In this guide, 13 topics are identified for patient education, along with the recommendation that information should be provided to patients in a way that is both language and literacy appropriate.
Triangulation
Table 1 presents the results of the triangulation analysis. Medication or adherence was the topic most frequently identified as useful by PLWH and the second most useful topic identified by providers, and was included in the literature. Medication or adherence was also the most important topic to address during a clinical visit according to providers (see Figure 2). Transmission (risk or prevention) was the second most commonly identified useful topic by PLWH and the third most identified by providers, and was identified in the literature. The most commonly cited category as useful by healthcare providers was available services, though this was not a priority for PLWH and was not identified in the literature. Notably, across categories identified, patients and providers did not agree on the information that is the most useful to teach in a clinical setting.
Table 1.
Comparison Between the Most Useful Topics Identified in Patient and Provider Responses and Their Identification in the Integrative Review and U.S. Department of Health and Human Services (HHS) Guidelines
| Most useful topics for PLWH | PLWH (N = 195) | Providers (N = 126) | Integrative reviewa | HHS guidelinesa |
|---|---|---|---|---|
| n (%) | n (%) | Present (Y/N) | Present (Y/N) | |
| Medication/adherence | 73 (37.4) | 27 (21.3) | Y | Y |
| Transmission (risks/prevention) | 26 (13.3) | 17 (13.4) | Y | Y |
| Available services | 7 (3.6) | 29 (22.8) | N | Y |
| Mental health management | 17 (8.7) | 8 (6.3) | Y | Y |
| Knowledge about HIV | 5 (2.6) | 12 (9.4) | Y | Y |
| Results of laboratory analysis | 2 (1.0) | 8 (6.3) | Y | Y |
| General health management | 26 (13.3) | 1 (0.8) | Y | N |
| Nutrition and healthy eating | 23 (11.8) | 4 (3.9) | N | N |
| Appointment logistics | 11 (5.6) | 3 (2.4) | N | N |
| Opportunistic infections | 0 (0.0) | 1 (0.8) | Y | N |
| Other health conditions | 0 (0.0) | 7 (5.5) | Y | N |
| Family planning | 0 (0.0) | 5 (3.9) | N | N |
| Other | 3 (1.5) | 1 (0.8) | N | N |
| Belief in God | 2 (1.0) | 0 (0.0) | N | N |
| Hygiene | 0 (0.0) | 1 (0.8) | N | N |
| Home environment | 0 (0.0) | 1 (0.8) | N | N |
Note. PLWS = persons living with HIV.
Y indicates yes (i.e., that topic was present in that information source) and N indicates no (i.e., that topic was not present in that information source).
From the triangulation of these three sources, the prioritized list of the topics of the most useful information for PLWH to receive during a clinical encounter is as follows: medication or adherence, transmission (risk or prevention), mental health management, knowledge of HIV, available services, results of laboratory analysis, general health management, nutrition and healthy eating, followed by appointment logistics.
Discussion
Because the effective treatment and management of HIV is now a long-term commitment, understanding what information patients need in order to manage their health is essential to inform effective health education activities. In this study, we used a data sources triangulation method that compared the perspectives of PLWH and their healthcare providers as well as the scientific literature to comprehensively identify what information is the most important for healthcare providers to share with PLWH to enable self-management. Findings showed little agreement regarding what information is the most useful for health management among patients or providers but still provide a comprehensive evidence base regarding the information that PLWH need to receive in order to effectively manage their health.
Findings demonstrate that PLWH need to acquire, synthesize, and apply health information on a variety of topics to achieve effective self-management. This may be complicated because information needs evolve over time. For example, PLWH may initially focus on understanding the condition and necessary treatments and then may gradually shift to consider what is needed for long-term self-management (Minion, Bath, & Albright, 2009). Furthermore, information needs may vary depending on age or gender, or among high-risk groups (Stonbraker & Larson, 2016). For instance, in the DR, despite similar HIV prevalence rates among men and women, men are more likely to report higher-risk sexual behaviors than women (Curtis & Sutherland, 2004) and are more likely to be active information seekers (Stonbraker, Befus, Lerebours Nadal, Halpern, & Larson, 2016). This is important to consider in a cultural context where heterosexual transmission of HIV between stable partners is common (Jimenez, Andrade, Raffaelli, & Iwelunmor, 2015). This is relevant for researchers and clinicians, since the individual characteristics and behaviors of patients must be consistently explored and taken into account so the information provided to patients can be tailored according to their needs.
PLWH and providers in our study agreed on some of the information that is the most useful for effective self-management but differed in others. This is highlighted in Table 1, with the varying proportions of responses provided by patients and providers for each educational topic. For instance, patients and providers agreed that medication or adherence and transmission including risks and prevention were important. But, while over 20% of provider responses indicated that information about available services would be useful to patients, less than 5% of patient responses mentioned the same. There are many reasons these discrepancies may exist; for example, differing areas of expertise and experience may be principal contributors (Hartzler & Pratt, 2011). Regardless, this is clinically relevant, as healthcare providers must consider patients’ needs, abilities, and limitations to ensure the information that patients want and need is delivered in an understandable way.
Beyond what information needs to be provided to patients, an important consideration for clinical practice is how health information is communicated and provided to patients. The importance of targeted and tailored clinical communication was highlighted in the integrative review (Stonbraker & Larson, 2016), in the HHS guidelines (HHS, 2014), in other studies (Mallinson, Rajabiun, & Coleman, 2007; Street, 2013), and is especially important in limited-resource settings where patients are more likely to have low health literacy. One corresponding clinical recommendation to improve health education is to use an interdisciplinary team-based approach to education, since this technique may make information provision more comprehensive and can help to address some of the psychosocial concerns facing patients (Gakumo et al., 2015). Healthcare providers can also explore additional methods to enhance individual clinical communication, such as by leaning techniques to more effectively communicate with individuals who have low health literacy or by providing print materials to augment patient education. Additionally, researchers are beginning to assess the clinical utility of using information visualizations (infographics) as a tool to ensure information is provided in a culturally appropriate and comprehensible way that improves understanding, health behaviors, attention span, and ability to recall information (Garcia-Retamero, Okan, & Cokely, 2012).
The priority list of health information generated in this study may be used clinically to inform the content of clinical discussions or health education activities, or in the design of relevant information visualizations or patient education materials that could help communicate pertinent information to PLWH. On the organizational or policy level, international governments and agencies that provide resources and services to improve treatment and services to PLWH globally could include priority health education topics in their published recommendations and guidelines on how to effectively communicate with patients as the HHS’s guide does. Providing clear content guidelines for health education will enable more widespread access to this evidence base, which can help providers and organizations provide comprehensive and tailored health education to their clients.
One limitation of this study is that we did not ask participants for specific details regarding what information should be included for each identified education topic. Thus, from our data, it is not clear what exactly should be taught about medication or adherence or the risks for or prevention of transmission, for example. Another limitation of the study is that we are not able to show at what point in disease progression health information may be the most relevant to patients. For instance, we cannot say what information would be the most useful following initial diagnosis versus what would be more useful after having lived with HIV infection for many years. Future research should elucidate the details of the specific information needed by patients and at what point in disease progression that information is the most relevant. Lastly, participants were recruited from one health center, which could limit generalizability. However, results are expected to be generalizable across limited-resource settings where patients may have similar levels of education and health literacy.
Despite limitations, we were able to generate a comprehensive, evidence-based list of priority education topics for PLWH living in limited-resource settings. Although the findings themselves are not novel, this study provides a rigorously developed and comprehensive evidence base to indicate what information topics will be the most useful to address during a clinical encounter or in other health education activities in order to support the self-management of PLWH. By using these priorities to guide health education, nurses and other health educators will be able to improve services by making more informed choices about what information to provide their patients.
Clinical Resources.
Centers for Disease Control and Prevention. HIV training and educational resources. https://npin.cdc.gov/training/featured-hiv-training-and-educational-resources
U.S. Department of Health and Human Services. 2014 Guide for HIV/AIDS clinical care. https://hab.hrsa.gov/sites/default/files/hab/clinical-quality-management/2014guide.pdf
Acknowledgments
During this research, Samantha Stonbraker was supported by the Reducing Health Disparities Through Informatics (RHeaDI) training grant (T32 NR007969), funded by the National Institute of Nursing Research, National Institutes of Health.
References
- Begley CM (1996). Using triangulation in nursing research. Journal of Advanced Nursing, 24(1), 122–128. [DOI] [PubMed] [Google Scholar]
- Castro P, Cameroamortegui F, Nolasco A, Li I, Hillard J, & Nassiri R (2014). Psycho-social and care delivery challenges of HIV/AIDS in the Dominican Republic: Impairment of patient outcomes. Journal of AIDS and Clinical Research, 5(12). [Google Scholar]
- Centers for Disease Control and Prevention. (2017). HIV/AIDS. Retrieved from https://www.cdc.gov/hiv/default.html
- Clínica de Familia. (2015). Reporte annual [Annual report]. La Romana, Dominican Republic: Retrieved from http://www.clinicadefamilia.org.do/wordpress/wp-content/uploads/2012/07/Reporte-Anual-2015_Cl%C3%ADnica-de-Familia-La-Romana.pdf [Google Scholar]
- Curtis SL, & Sutherland EG (2004). Measuring sexual behaviour in the era of HIV/AIDS: The experience of demographic and health surveys and similar enquiries. Sexually Transmitted Infections, 80(Suppl. 2), ii22–ii27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Boni R, Veloso V, & Grinsztejn B (2014). Epidemiology of HIV in Latin America and the Caribbean. Current Opinion in HIV and AIDS, 9(2), 192–198. doi: 10.1097/COH.0000000000000031 [DOI] [PubMed] [Google Scholar]
- Fenech Adami M, & Kiger A (2005). The use of triangulation for completeness purposes. Nurse Researcher, 12(4), 19–29. [DOI] [PubMed] [Google Scholar]
- Gakumo CA, Enah CC, Vance DE, Sahinoglu E, & Raper JL (2015). “Keep it simple”: Older African Americans’ preferences for a health literacy intervention in HIV management. Patient Preference and Adherence, 9, 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García P, Bayer A, & Cárcamo C (2014). The changing face of HIV in Latin America and the Caribbean. Current HIV/AIDS Reports, 11(2), 146–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Retamero R, Okan Y, & Cokely ET (2012). Using visual aids to improve communication of risks about health: A review. Scientific World Journal, 2012, Article 562637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebre Y, Forbes NM, & Peters A (2016). Review of HIV treatment progress, gaps, and challenges in the Caribbean, 2005–2015. Revista Panamericana de Salud Publica, 40(6), 468–473. [PubMed] [Google Scholar]
- Guilamo-Ramos V, Lee JJ, Ruiz Y, Hagan H, Delva M, Quiñones Z, … Robles G (2015). Illicit drug use and HIV risk in the Dominican Republic: Tourism areas create drug use opportunities. Global Public Health, 10(3), 318–330. [DOI] [PubMed] [Google Scholar]
- Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde J (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartzler A, & Pratt W (2011). Managing the personal side of health: How patient expertise differs from the expertise of clinicians. Journal of Medical Internet Research, 13(3), e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resources Health & Administration Services. (2017). HRSA Ryan White & Global HIV/AIDS Programs. Retrieved from https://hab.hrsa.gov/about-ryan-white-hivaids-program/about-ryan-white-hivaids-program
- Hussein A (2015). The use of triangulation in social sciences research: Can qualitative and quantitative methods be combined? Journal of Comparative Social Work, 4(1). [Google Scholar]
- Iribarren S, Siegel K, Hirshfield S, Olender S, Voss J, Krongold J, … Schnall R (2018). Self-management strategies for coping with adverse symptoms in persons living with HIV with HIV associated non-AIDS conditions. AIDS and Behavior, 22(1), 297–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez MM, Andrade FC, Raffaelli M, & Iwelunmor J (2015). Heterosexual transmission of HIV in the Dominican Republic: Gendered indicators are associated with disparities in condom use. BMC Public Health, 15(1), 1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston L, Vaillant T, Dolores Y, & Vales H (2013). HIV, hepatitis B/C and syphilis prevalence and risk behaviors among gay, transsexuals and men who have sex with men, Dominican Republic. International Journal of STD and AIDS, 24(4), 313–321. [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2017a). AIDSinfo. Retrieved from http://aidsinfo.unaids.org/ [PubMed]
- Joint United Nations Programme on HIV/AIDS. (2017b). Monitoring and evaluation guidance. Retrieved from http://www.unaids.org/en/dataanalysis/monitoringandevaluationguidance?utm_source=unaids-site-design&utm_medium=display&utm_campaign=en-top-nav-menu
- Luft H, & Larson E (2017). Psychosocial correlates of safe sex communication between Latina women and their stable male partners: An integrative review. AIDS Care, 29(5), 618–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey LM, Doody C, Werner EL, & Fullen B (2016). Self-management skills in chronic disease management what role does health literacy have? Medical Decision Making, 36(6), 741–759. [DOI] [PubMed] [Google Scholar]
- Mallinson RK, Rajabiun S, & Coleman S (2007). The provider role in client engagement in HIV care. AIDS Patient Care and STDS, 21(Suppl. 1), S-77–S-84. [DOI] [PubMed] [Google Scholar]
- Millard T, Elliott J, & Girdler S (2013). Self-management education programs for people living with HIV/AIDS: A systematic review. AIDS Patient Care and STDS, 27(2), 103–113. [DOI] [PubMed] [Google Scholar]
- Minion J, Bath P, & Albright K (2009). From sponge to source: Health information in the lives of gay men living with HIV. Presented at the 8th Global Conference Making Sense of Health, Illness and Disease, Oxford, United Kingdom. [Google Scholar]
- Mitchell ES (1986). Multiple triangulation: A methodology for nursing science. Advances in Nursing Science, 8(3), 18–26. [DOI] [PubMed] [Google Scholar]
- National Institute of Nursing Research. (2016). NINR’s strategic plan. Retrieved from https://www.ninr.nih.gov/aboutninr/ninr-mission-and-strategic-plan
- Padilla MB, Guilamo-Ramos V, Bouris A, & Reyes AM (2010). HIV/AIDS and tourism in the Caribbean: An ecological systems perspective. American Journal of Public Health, 100(1), 70–77. doi: 10.2105/AJPH.2009.161968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas P, Malow R, Ruffin B, Rothe E, & Rosenberg R (2011). The HIV/AIDS epidemic in the Dominican Republic: Key contributing factors. Journal of the International Association of Providers of AIDS Care, 10(5), 306–315. doi: 10.1177/1545109710397770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Aunon FM, Kemp CG, Kutner BA, Ramaiya MK, Velloza J, & Yang JP (2017). Implementation research on HIV adherence interventions: no time to wait. Lancet Infectious Diseases, 17(6), 564–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon P, O’Brien KK, Baxter L, MacLachlan D, & Robinson G (2016). Community involvement in development of evidence-informed recommendations for rehabilitation for older adults living with HIV. Progress in Community Health Partnerships: Research, Education, and Action, 10(1), 83–88. [DOI] [PubMed] [Google Scholar]
- Stonbraker S, Befus M, Lerebours Nadal L, Halpern M, & Larson E (2016). Factors associated with health information seeking, processing, and use among HIV positive adults in the Dominican Republic. AIDS and Behavior, 21(6), 1588–1600. doi: 10.1007/s10461-016-1569-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stonbraker S, & Larson E (2016). Health-information needs of HIV-positive adults in Latin America and the Caribbean: An integrative review of the literature. AIDS Care, 28(10), 1223–1229. doi: 10.1080/09540121.2016.1173645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stonbraker S, Smaldone A, Luft H, Cushman LF, Lerebours Nadal L, Halpern M, & Larson E (2017). Associations between health literacy, HIV-related knowledge, and information behavior among persons living with HIV in the Dominican Republic. Public Health Nursing, 35(3), 166–175. doi: 10.1111/phn.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street RL (2013). How clinician–patient communication contributes to health improvement: modeling pathways from talk to outcome. Patient Education and Counseling, 92(3), 286–291. [DOI] [PubMed] [Google Scholar]
- Swendeman D, Ingram BL, & Rotheram-Borus MJ (2009). Common elements in self-management of HIV and other chronic illnesses: An integrative framework. AIDS Care, 21(10), 1321–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas E, & Magilvy JK (2011). Qualitative rigor or research validity in qualitative research. Journal for Specialists in Pediatric Nursing, 16(2), 151–155. [DOI] [PubMed] [Google Scholar]
- Thurmond VA (2001). The point of triangulation. Journal of Nursing Scholarship, 33(3), 253–258. [DOI] [PubMed] [Google Scholar]
- United Nations Educational Scientific and Cultural Organization. (2017). EDUCAIDS. Retrieved from United Nations Educational Scientific and Cultural Organization. [Google Scholar]
- U.S. Department of Health and Human Services. (2014). Guide for HIV/AIDS clinical care. Rockville, MD: Author. Retrieved from https://hab.hrsa.gov/clinical-quality-management/clinical-care-guidelines-and-resources [Google Scholar]
- U.S President’s Emergency Plan for AIDS Relief. (2017). Guidance. Retrieved from https://www.pepfar.gov/reports/guidance/index.htm
- White MD, & Marsh EE (2006). Content analysis: A flexible methodology. Library Trends, 55(1), 22–45. [Google Scholar]
- Wilson T (1999). Models in information behaviour research. Journal of Documentation, 55(3), 249–270. [Google Scholar]
- World Health Organization. (2017). WHO guidelines on HIV/AIDS. Retrieved from http://www.who.int/publications/guidelines/hiv_aids/en/