Abstract
Neoplasms arising from scapula are rare. We herein, present a rare case of Ewing’s sarcoma of scapula in a 9-year-old male child. Extensive literature search reveals that less than 20 similar cases have been reported so far. The index case had been treated with multimodal therapies—chemotherapy, surgery, and radiotherapy. This case is reported to highlight the rarity of the case and discuss the review of literature comprehensively.
Keywords: Ewing’s sarcoma, Scapula, Multimodal therapies
Introduction
Ewing’s sarcoma (ES) is the second most common bone tumor in childhood and adolescence [1]. It usually arises in the metaphysis or diaphysis of long bones of extremities [2]. The lungs, bones, and bone marrow are the most common sites of metastasis [2]. The prognosis of ES has improved in recent years, and its successful management requires multidisciplinary approach involving surgery, radiotherapy, and chemotherapy as multimodal therapies [1]. Tumors of scapula in childhood are rare [3]. Here, we present a rare case of ES of left scapula in a 9-year-old boy and discuss pertinent literature on it. To the best of our knowledge, less than 20 cases of ES of scapula have been reported in English literature so far [3–6].
Case Report
A 9-year-old male child, with no significant past or family history presented with swelling around left shoulder for 2 months, which was progressively increasing in size and associated with pain and restriction of left shoulder joint movement. Local examination revealed a single large swelling of 8 × 9 cm2, firm in consistency over left scapular region. There was no distal neurovascular deficit. Contrast-enhanced computed tomography (CECT) scan of chest and abdomen was done which showed a large heterogenous soft tissue mass involving left scapula (Fig. 1). Biopsy from the mass was suggestive of Ewing’s sarcoma (Fig. 2a, b). Tumor cells were immunopositive for mic-2 and FLI-1 (Fig. 2c, d). Positron emission tomography-CT (PET-CT) scan showed a lytic expansile lesion with large soft tissue component involving almost entire scapula sparing its inferior angle only with infiltration of surrounding muscles with no other sites of metastases (Fig. 3a, b). He was started on chemotherapy with modified St. Jude’s protocol. After completion of 15 weeks of chemotherapy, he underwent a PET-CT which showed a complete metabolic response (Fig. 3c, d). Then he underwent left scapulectomy. Postoperative histopathologic examination revealed a residual Ewing’s sarcoma (4 × 3 × 1.5 cm3) which was breaching cortex and infiltrating adjacent muscle. All resection margins were free and area of necrosis constituted around 10% of the tumor area. He was given adjuvant radiotherapy of dose 45 gray in 25 fractions over 5 weeks to tumor bed by a three-dimensional conformal radiotherapy. He was continued on further adjuvant chemotherapy till week 29.
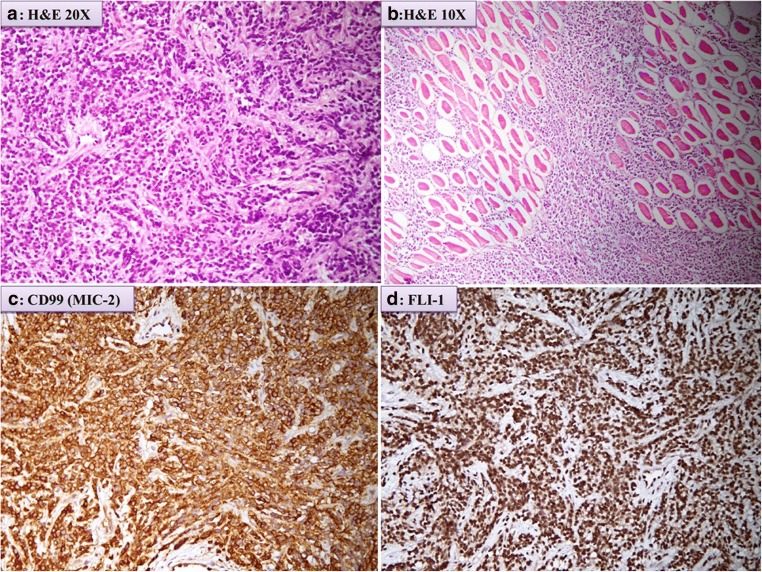
Fig. 1.
Axial section of CECT scan showing large heterogenous soft tissue mass involving left scapula
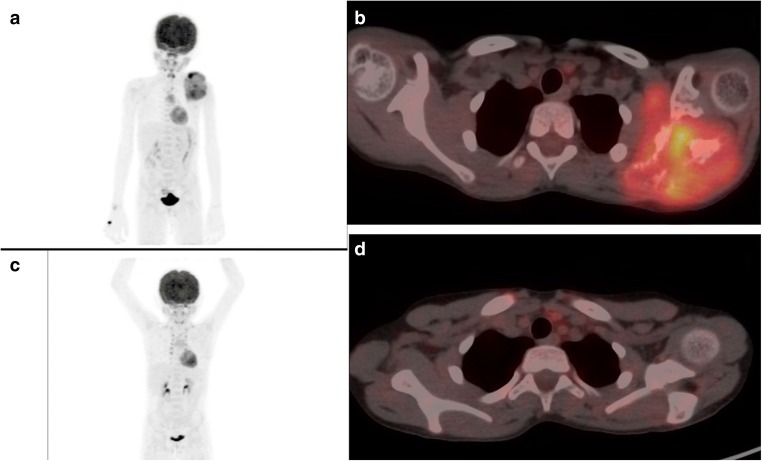
Fig. 2.
a Microphotograph showing a solidly packed, monotonous proliferation of malignant small round cell with a striking uniformity. The individual cells have round or ovoid nucleus with a distinct nuclear membrane, powdery chromatin chromatin, and indistinct nucleoli. b Section shows tumor infiltrating in to the surrounding skeletal muscle. c, d. Immunohistochemistry shows tumor cells are immunopositive for CD99 (MIC-2) strong membranous and FLI-1 (friend leukemia integration-1) shows nuclear positivity
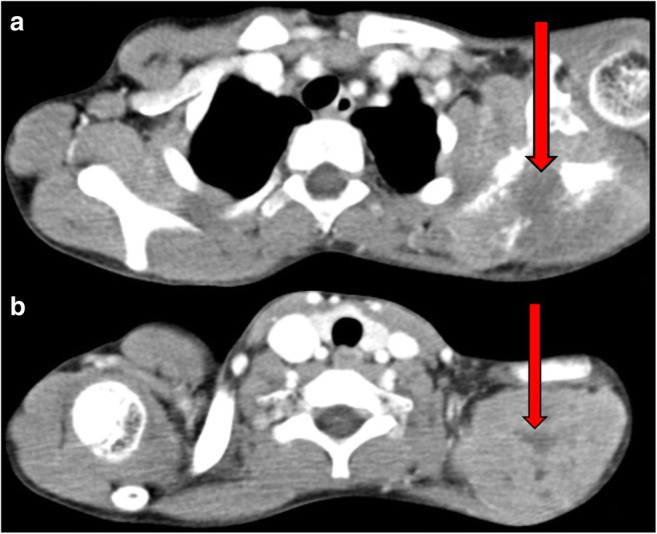
Fig. 3.
a, b PET-CT showing lytic expansile lesion with soft tissue component involving left scapula. c, d PET-CT showing complete metabolic response of tumor (post chemotherapy).
Discussion
ES is a highly malignant tumor composed of small round blue cells that primarily affects the skeletal system [1]. It is a neoplasm commonly affecting patients in the first two decades with a male predilection [5]. Similarly, the index case was a male child of 9 years old. It frequently involves the bones of the pelvis and extremities like the femur, tibia, humerus, and fibula, unlike in our case where it has involved scapula. Scapular neoplasms are rare, if at all occur, are usually malignant rather benign [5–7]. Ninety-five percent of ES tumors express a balanced translocation involving the EWS gene on chromosome 22 and a member of the ETS family of transcription factors [8]. Common presenting symptoms are pain and swelling. Symptoms of systemic disease occur at times, including low-grade fevers, malaise, and weakness [9]. Similarly in our presented case, the child presented with a local swelling around the left shoulder. Radiographically, a mottled or moth-eaten lesion is found. Subperiosteal reactive new bone may be present, producing an “onion skin” appearance [5]. A magnetic resonance imaging (MRI) of the primary lesion may be done to look for soft tissue extent and bone marrow involvement whereas a CT scan demonstrates the extent of bone destruction [9]. Systemic workup should include chest radiograph, CT chest, bone scan, bone marrow biopsy, or alternatively PET-CT [9]. Detailed investigations were done in our patient which revealed a localized, heterogeneously enhancing, bone destructing lesion of left scapula with surrounding muscle involvement. Microscopically ES tumors are composed of uniform small round cells with round nuclei containing fine chromatin and scant cytoplasm. Tumor cells frequently stain positive for CD99, which is a cell surface glycoprotein, the product of the MIC-2 genes [5].
Effective local and systemic therapy are necessary for its cure. Peri-operative intensive systemic chemotherapy with multiple anticancer drugs is the standard of care for ES [1]. Most chemotherapy regimens combine cyclophosphamide, adriamycin, vincristine, dactinomycin, ifosfamide, and etoposide [9]. Postoperative radiation should also be offered, if obtained surgical margin comes out to be close or positive or if there is a poor histologic response to induction chemotherapy [10]. Similarly, our patient received induction chemotherapy followed by surgery and radiation was administered in view of poor histologic response. Preoperative radiation can also be administered, if preoperative radiological examinations indicate difficult surgical excision or definitive radiation therapy may also be offered if the tumor is not amenable for surgery [10]. Important prognostic factors include the stage, anatomic location, the size of tumor, chemotherapy-induced necrosis, and treatment [11]. After successful management, these patients with ES require long-term follow-up in order to detect secondary malignancies and growth-related musculoskeletal complications.
Conclusion
Although scapular malignancies are rare, Ewing’s sarcoma should be considered in the differential diagnosis of scapular neoplasms. Surgical resection, multi agent chemotherapy, and radiotherapy are the mainstay of treatment of this entity.
Compliance with Ethical Standards
Conflicts of Interest
None
Contributor Information
Rituparna Biswas, Email: mail4r_biswas@yahoo.co.in.
Balaji Krishnan, Email: bhaajii47@gmail.com.
Ravi Hari Phulware, Email: ravipaarti@gmail.com.
Shambo Guha Roy, Email: shamboguharoy@gmail.com.
Ritesh Kumar, Phone: +91- 953774134, Email: riteshkr9@gmail.com.
Adarsh Barwad, Email: adawad@gmail.com.
Jagdish Prasad Meena, Email: drjpmeena@yahoo.com.
Shah Alam Khan, Email: shahalamkhan70@gmail.com.
References
- 1.Ozaki T. Diagnosis and treatment of Ewing sarcoma of the bone: a review article. J Orthop Sci. 2015;20(2):250–263. doi: 10.1007/s00776-014-0687-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waqar SH, Zahid MA. Ewing’s sarcoma in scapular region. APSP J Case Rep. 2011;2(3):22. [PMC free article] [PubMed] [Google Scholar]
- 3.Hoornenborg D, Veltman ES, Oldenburger F, Bramer JAM, Schaap GR. A patient with scapular Ewing sarcoma; 5-year follow-up after extracorporeal irradiation and re-implantation of the scapula, a case report. J Bone Oncol. 2013;2(1):30–32. doi: 10.1016/j.jbo.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayil Vahanan N, Mohanlal P, Bose JC, Gangadharan R, Karthisundar V. The functional and oncological results after scapulectomy for scapular tumours: 2–16-year results. Int Orthop. 2007;31:831–836. doi: 10.1007/s00264-006-0261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shahid M, Varshney M, Maheshwari V, Mubeen A, Siddiqui MA, Julfiqar J, GauR K. Ewing’s sarcoma of scapula: a rare entity. BMJ Case Reports. 2011;2011:bcr0220113810. doi: 10.1136/bcr.02.2011.3810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Puchner SE, Panotopoulos J, Puchner R, Schuh R, Windhager R, Funovics PT. Primary malignant tumours of the scapula—a review of 29 cases. Int Orthop. 2014;38(10):2155–2162. doi: 10.1007/s00264-014-2417-8. [DOI] [PubMed] [Google Scholar]
- 7.Asif N, Khan AQ, Siddiqui YS, Mustafa H. Metastasis from scapular Ewing’s sarcoma presenting as sutural diastasis: an unusual presentation. International journal of shoulder surgery. 2010;4(1):18–21. doi: 10.4103/0973-6042.68415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Delattre O, Zucman J, Plougastel B, Desmaze C, Melot T, Peter M, Kovar H, Joubert I, de Jong P, Rouleau G, Aurias A, Thomas G. Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours. Nature. 1992;359(6391):162–165. doi: 10.1038/359162a0. [DOI] [PubMed] [Google Scholar]
- 9.Halperin EC et al (2013) Perez and Brady’s principles and practice of radiation oncology, sixth edn. Lippincott Williams & Wilkins, Philadelphia, p 1689
- 10.Halperin EC et al (2013) Perez and Brady’s principles and practice of radiation oncology, sixth edn. Lippincott Williams & Wilkins, Philadelphia, p 1691
- 11.Picci P, Bohling T, Bacci G, et al. Chemotherapy-induced tumor necrosis as a prognostic factors in localized Ewing’s sarcoma of the extremities. J Clin Oncol. 1999;15:1553–1559. doi: 10.1200/JCO.1997.15.4.1553. [DOI] [PubMed] [Google Scholar]