Despite the great progress in cancer care, we have too often neglected to capitalize upon a highly feasible, readily available, and very cost-effective route to improve cancer treatment success and cancer recovery. While effective smoking cessation treatments exist, they are not consistently provided to patients as part of their cancer care. Doing so offers a clear opportunity to advance cancer care because approximately 30% of cancer deaths are directly caused by smoking1, and research advances have produced numerous interventions that double or triple a smoker’s chance of quitting successfully. Moreover, new innovations keep emerging that further boost quitting success.
Our failure to treat smoking effectively in cancer patients exacts steep costs. Evidence shows that continued smoking after a cancer diagnosis is associated with increased adverse outcomes from cancer treatment, increased mortality post treatment, increased risk of a new primary cancer, and an increased risk of cancer recurrence.1,2 Conversely, quitting smoking after a cancer diagnosis can reduce virtually all of these negative outcomes, producing longer survival and a reduced risk of new cancers.1 The evidence is clear; a cancer diagnosis signals a unique and highly feasible opportunity to improve cancer treatment effectiveness and avoid future cancers in a highly at-risk population.
Unfortunately, smoking treatment is an often-neglected element of cancer care. For example, a 2009 survey of 58 NCI-Designated Clinical and Comprehensive Cancer Centers in the U.S. showed that 21% offered no tobacco use treatment services to their patients, only 62% routinely provided tobacco education materials to their patients, only half reported systems in place to identify which of their patients use tobacco, and fewer than half reported having a staff person dedicated to providing tobacco treatment services or a commitment from center leadership to provide such services. Such inattention has had a predictable impact on the delivery of smoking interventions. Data show that fewer than half of cancer care clinicians consistently discuss cessation medication options with their patients who smoke or actively treat or refer their patients to treatment resources.3 Among individuals who have had cancer but continue to smoke, only about 15% report having received counseling or support to quit in the past year.4 The failure to reliably deliver effective smoking treatments in oncology settings may be a key reason that patients with cancer diagnoses tend to be no more likely to quit smoking than members of the general population.4
This important gap in cancer care has many causes. Understandably, clinicians are often focused on the exigent need to treat the patient’s cancer per se, so tobacco treatment becomes an afterthought. Also, many clinicians believe they are inadequately trained to deliver effective treatment for smoking, and they believe that their patients will resist such treatment or that it will not be effective.3 Some clinicians may believe that focusing attention on smoking may exacerbate the guilt and shame that smokers often feel after developing cancer. Such factors, plus resource limitations, have hindered the delivery of effective smoking treatment in cancer patients for far too many years.5 A strong and strategically engineered program is needed to support and organize resources to overcome the obstacles that have prevented the effective treatment of smoking in cancer care.
To address this cancer treatment gap, the National Cancer Institute (NCI), as part of the Cancer MoonshotSM, is launching a nationwide effort to help people quit smoking while they are undergoing treatment for cancer. The Cancer Center Cessation Initiative (C3I) is designed to jumpstart the reach and effectiveness of smoking cessation treatment at NCI-Designated Cancer Centers through implementation science. In late 2017, 22 NCI-designated cancer centers received two years of funding ($250,000/year for 2 years) to begin or expand smoking cessation treatment programs. In 2018, 20 additional cancer centers will begin receiving such funding. Findings from the initiative, including the identification of best practices and highly effective smoking cessation interventions for this population, will ultimately be synthesized and shared with clinical cancer facilities nationwide. The overall goal is to ensure that every cancer patient who smokes is provided with smoking cessation support and assistance at the time of his or her cancer care.
C3I is strategically designed to achieve significant, nationwide clinical impact. Its key innovative features include the following:
Funded centers must take a population-based approach; i.e., the aims are that every cancer patient who smokes and presents to the cancer center will be identified, urged to quit, offered evidence-based cessation treatment, and tracked in terms of treatment outcomes.
Centers must take a systems-based approach, integrating evidence-based tobacco dependence treatment into cancer care workflows and utilizing electronic health record technology to facilitate that integration.
Centers are required to address program sustainability; i.e., have a plan that sustains the program after NCI funding ends
Finally, C3I funding targets cancer centers for funding that have had clear gaps in their smoking treatment programs, but that have developed innovative and highly feasible plans to address those gaps.
As an implementation science effort, C3I is focused not only on what to implement, but how to implement it. The funded cancer centers vary greatly in organizational context and approaches to treatment for tobacco use. This affords a critical opportunity to determine how the evidence-based tobacco interventions identified in large randomized clinical trials can be translated into day-to-day cancer care clinical practice. Because successful local adaptation within individual centers is expected to depend in part on modifications to the electronic health record, this has been a special area of focus of the initiative.
For the first cohort of centers funded in late 2017, each center has identified ways to strategically address limitations or leverage opportunities to improve smoking treatment in its clinical care programs. These strategies include enhancements to the electronic health record so that it facilitates and guides the key steps in smoking treatment: identifying patients who smoke, offering evidence-based smoking treatment, delivering smoking treatment, and providing follow-up support. In addition, some centers are using C3I support to fund new positions, improve program workflows to reduce burden, and develop new billing and reimbursement strategies to help sustain the smoking treatment program after NCI funding has ended.
The C3I initiative is an expression of the promise of the Cancer Moonshot, a national research initiative to reduce cancer morbidity and mortality. Established by Congress in 2016 as part of the 21st Century Cures Act, the Cancer Moonshot is designed “to accelerate cancer research to make more therapies available to more patients, while improving our ability to prevent cancer and detect it in an early stage.” The National Cancer Institute’s Cancer Center Cessation Initiative is designed to meet these goals by increasing the participation of cancer patients in smoking treatment, affording this highly at-risk group the tools to enhance the effectiveness of their cancer treatment and to address the leading preventable cause of cancer recurrence. C3I has the potential to transform clinical cancer care so that, moving forward, evidence-based smoking cessation treatment is an integral and necessary component of care for every cancer patient who smokes.
Figure:
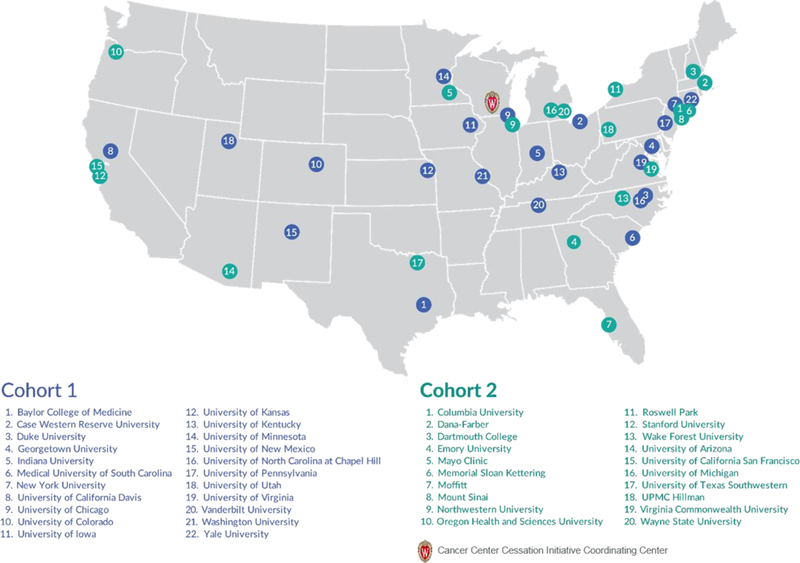
NCI-Designated Cancer Centers selected as part of the Cancer Center Cessation Initiative (C3I) -grantees from Cohort 1 (2017–2019) and Cohort 2 (2018–2020).
References
- 1.Gritz ER, Toll BA, Warren GW. Tobacco use in the oncology setting: advancing clinical practice and research. Cancer Epidemiol Biomarkers Prev. 2014;23(1):3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. The health consequences of smoking - 50 years of progress: A report of the Surgeon General. Atlanta, GA. 2014.
- 3.Warren GW, Dibaj S, Hutson A, Cummings KM, Dresler C, Marshall JR. Identifying targeted strategies to improve smoking cessation support for cancer patients. J Thorac Oncol. 2015;10(11):1532–1537. [DOI] [PubMed] [Google Scholar]
- 4.Ramaswamy AT, Toll BA, Chagpar AB, Judson BL. Smoking, cessation, and cessation counseling in patients with cancer: A population-based analysis. Cancer. 2016;122(8):1247–1253. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein AO, Ripley-Moffitt CE, Pathman DE, Patsakham KM. Tobacco use treatment at the U.S. National Cancer Institute’s designated Cancer Centers. Nicotine Tob Res. 2013;15(1):52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]


