Abstract
The acceleration of prevention of mother-to-child transmission (PMTCT) activities, coupled with the rollout of 2010 World Health Organization (WHO) guidelines, led to important discussions and innovations at global and country levels. One paradigm-shifting innovation was Option B+ in Malawi. It was later included in WHO guidelines and eventually adopted by all 22 Global Plan priority countries. This article presents Malawi’s experience with designing and implementing Option B+ and provides complementary narratives from Cameroon and Tanzania. Malawi’s HIV program started in 2002, but by 2009, the PMTCT program was lagging far behind the antiretroviral therapy (ART) program because of numerous health system challenges. When WHO recommended Option A and Option B for PMTCT in 2010, it was clear that Malawi’s HIV program would not be able to successfully implement either option without increasing existing barriers to PMTCT services and potentially decreasing women’s access to care. Subsequent stake-holder discussions led to the development of Option B+. Operationalizing Option B+ required several critical considerations, including the complete integration of ART and PMTCT programs, systematic reduction of barriers to facilitate doubling the number of ART sites in less than a year, building consensus with stakeholders, and securing additional resources for the new program. During the planning and implementation process, several lessons were learned which are considerations for countries transitioning to “treat-all”: Comprehensive change requires effective government leadership and coordination; national clinical guidelines must accommodate health system limitations; ART services and commodities should be decentralized within facilities; the general public should be well informed about major changes in the national HIV program; and patients should be educated on clinic processes to improve program monitoring.
Keywords: prevention of mother-to-child transmission, Option B+, HIV/AIDS, scaling up of services
INTRODUCTION AND BACKGROUND
The acceleration of Malawi’s prevention of mother-to-child transmission (PMTCT) activities in 2008–2009, coupled with the rollout of the 2010 World Health Organization (WHO) guidelines, led to important programmatic developments in 2011 and programmatic innovations that had global ramifications for PMTCT. Implementation of Option B+ [initiation of antiretroviral therapy (ART) for life in any pregnant or breastfeeding woman identified as HIV positive, regardless of CD4 count or clinical stage] for PMTCT among the 21 Global Plan priority countries in Africa has facilitated the initiation of ART in over 908,000 HIV-positive women, preventing HIV transmission to their infants while also providing them with treatment before their immune systems become impaired. All 21 priority countries in sub-Saharan Africa have adopted Option B+ and are in various stages of implementation, with 80% ART coverage of pregnant women living with HIV in 2015. As countries position themselves to implement the 2015 WHO guidelines—which recommend the “test and start” approach to ART for everyone who tests HIV positive, regardless of clinical stage or CD4 count—the rapid scale-up of lifelong ART among HIV-positive pregnant and lactating women in the 4 years leading up to these guidelines provides a clear opportunity to reflect on lessons learned and to ensure successes are replicated and failures are avoided.
In this article, we will review the progression of Malawi’s PMTCT program as it related to the development of Option B+, which was a country-led “treat-all” program in a highly resource-constrained setting. We also will present experiences of Cameroon and the United Republic of Tanzania and describe the successes and challenges observed during implementation in these countries. Finally, in line with the global initiative to achieve HIV epidemic control by 2030, we will offer some considerations for countries that are preparing to transition to test and start.
The Start of Malawi’s National PMTCT Program, 2002–2003
Malawi’s HIV program started in 2002 with a grant from the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund). By the end of 2003, 117 health facilities and freestanding voluntary counseling and testing sites delivered HIV testing and counseling services and more than 215,000 tests had been performed. PMTCT services were free but available in only 17 of the approximately 700 public sector antenatal care clinics; 3383 (11.4%) of the 29,791 pregnant women tested in 2003 were found to be HIV positive. Of those, 2198 (65.0%)—or 2.7% of the country’s estimated 80,000 HIV-positive pregnant women—received single-dose nevira-pine tablets. Very few women were referred to ART clinics for their own health, and ART services were available in only 7 facilities, where only 3703 patients had ever initiated ART.1 Under a fee-based system for ART in government clinics, which was in place until 2004, ART services faced severe challenges, including high loss to follow-up.2
PMTCT Scale-up, 2004–2009
Between 2004 and 2007, PMTCT lagged behind ART scale-up, partly because of separate central administration of the 2 programs and different prioritization within the Ministry of Health’s HIV and AIDS and Reproductive Health Units. Several problems were identified related to implementation and scale-up of PMTCT, including insufficient human and financial resource allocation, erratic supply of HIV test kits, inadequate logistics management, poor retention of PMTCT staff, inadequate laboratory services, and cultural barriers that prevented the active involvement of male partners.3 By 2007, with encouragement from the Global Fund, progress had been made through several strategies, including the integration of HIV testing into antenatal care clinics, developing longitudinal cohort registers with integrated HIV indicators for antenatal care clinics to follow women throughout their pregnancy, and introducing a zidovudine combination prophylaxis regimen in 2008 (zidovudine from 28 weeks of gestation and zidovudine/lamivudine during labor until 1 week after delivery, in combination with single-dose nevirapine tablets during labor).
By March 2010, the national ART supervision schedule included quarterly supportive supervision visits to PMTCT sites and Ministry of Health quarterly HIV program reports began to include comprehensive validated national PMTCT data.4 Nearly 70% of antenatal care sites (454 of 650) provided PMTCT services, and 224 antenatal care sites (34%) provided ART. Some 74% of women attending antenatal care had their HIV status ascertained, and nearly three-quarters (74%) of pregnant women diagnosed as HIV positive received antiretroviral medicines during pregnancy. Of these, 19% were already on ART at the start of pregnancy or started ART for their own health, 39% received the recommended zidovudine combination prophylaxis regimen, and 42% received only single-dose nevirapine tablets. Just 13% received a take-home packet of single-dose nevirapine syrup for their infants. In addition, although an estimated 50% of HIV-positive pregnant women were considered eligible for ART, coverage was only 15%.5
Despite concerted efforts, persistent and pervasive health system challenges limited expansion of HIV laboratory services. Only 42 facilities, or 15% of ART sites, had CD4 testing machines that had performed at least one test in the previous quarter, and only 57% of pregnant women received a CD4 count. Reflective of the overall situation, a cohort study in Zomba District in 2009, with follow-up to 18–20 months postpartum, reported very high mortality among HIV-infected women (42.4 deaths/1000 person-years) and HIV-free infant survival of only 66%.6,7
Between a Rock and a Hard Place, 2009–2010
In November 2009, the WHO released its Rapid Advice: Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants in advance of the complete 2010 guidelines.8 The new guidance recommended that all HIV-positive pregnant women with a CD4 count ≤350 should start ART and that women with CD4 count >350 should start either Option A (a regimen of zidovudine from 14 weeks of gestation onward, then single-dose nevirapine tablets at onset of labor, followed by zidovudine plus lamivudine during labor and delivery and for 7 days postpartum to prevent development of resistance to nevirapine) or Option B (a triple ART regimen to the HIV-positive pregnant woman, from 14 weeks of gestation through the breastfeeding period, with the HIV-exposed infant receiving daily nevirapine for prophylaxis until 1 week after all exposure to breast milk has ended). Both Option A and Option B required a baseline CD4 count, and Malawi had consistently struggled to scale-up its laboratory capacity, despite intensive technical and financial investments over several years.
THE CONCEPTUALIZATION OF OPTION B+
During joint meetings of the Malawi Ministry of Health’s ART and prevention of mother-to-child transmission technical working groups (TWGs) in January 2010, it was concluded that Malawi would not be able to successfully implement a PMTCT program based on a CD4 testing requirement. There was a real danger that simultaneously introducing a requirement of CD4 testing before ART initiation in HIV-positive pregnant women and phasing out single-dose nevirapine tablets and the combination prophylaxis regimens would reduce (rather than increase) access to PMTCT services. It was during these joint TWG meetings that the new Option B+ policy—which had a clear and logical rationale (Box 1)—was conceptualized as a more practical and feasible approach to improving PMTCT in Malawi.5
Box 1. Malawi’s Rationale Behind the Development of Option B+.
Perceived challenges either with no program change or with implementing WHO’s Option B:
Potential increased drug resistance with single-dose nevirapine tablets prescribed to women with advanced HIV disease.
Unresolved health system barriers to the rapid scale-up of CD4 testing for ART eligibility could reduce access to PMTCT if eligibility criteria were applied for prophylaxis.
High fertility rates would result in a start-stop-start approach to ART under Option B.
Viral rebound after stopping ART could affect transmission to a partner or fetus in a subsequent pregnancy or to the child during breastfeeding.
Stopping ART could result in reactivation of the hepatitis B virus, which affects an estimated 10–15 percent of people living with HIV.
Perceived benefits of Option B+:
Increased potential to reach maximum coverage of HIV prevention benefits and the virtual elimination of pediatric HIV.
Reduced HIV transmission to spouse or partner.
Simplicity of integrating ART and PMTCT would streamline implementation.
Subsequent pregnancies would be protected from conception, rather than from the second or third trimester.
Reduced maternal mortality, with the secondary benefit of improved child survival.11
PLANNING AND IMPLEMENTING OPTION B+
Moving Option B+ from a concept in January 2010 to a reality by July 2011 was a formidable task. Three major challenges were faced. First, this was not just another step forward in one part of the HIV program; for Option B+ to succeed, there would have to be a complete integration of ART and PMTCT into a single program at each level of the health sector. Second, Options A and B assumed laboratory capacity not available in Malawi, and the proposed solution under Option B+ meant a complete divergence from the preferred global standard of laboratory testing to identify patients eligible for ART. For a country that historically relied heavily on WHO guidance to direct national programs, this was major departure from the norm. The Ministry of Health, United Nations, and donor agencies had to be convinced of its validity, particularly as this was an untried intervention proposed for rapid and complete national scale-up, with no provision for a pilot or phasing-in of the approach. The third hurdle was mobilizing adequate resources for implementing Option B+, as there would be both an increased number of people on ART and a more expensive tenofovir and efavirenz-based first-line regimen, which could be safely tolerated by pregnant women (unlike the stavudine- and nevirapine-based regimen in use at the time for the nonpregnant population).
Complete Integration of ART and PMTCT Programs
Given the historical separation of the prevention and treatment programs that had anecdotally contributed to the lag of PMTCT expansion—and the fact that Option B+ was essentially the provision of ART to a subset of the population—it was critical that the national ART and PMTCT programs merge, starting with the TWGs and extending through every aspect of program planning, implementation, and monitoring. This led to the integration of ART and PMTCT guidelines, training curricula, supply chain management systems, monitoring and evaluation tools, and reporting and supervisory systems at the site, district, zonal, and national levels. Long-term ART monitoring within the mother, newborn, and child health setting would not be feasible using the gestation-limited antenatal care monitoring and evaluation tools; instead, ART tools were recommended for use in antenatal care settings where women would receive all pregnancy and subsequent HIV services in a single location. HIV-exposed infant patient cards were also provided to maternity wards to facilitate timely enrolment of infants into care, rather than relying on the identification of infants as HIV exposed at under-5 clinics.
Systematic Reduction of Barriers to Rapid ART Scale-up
To maximize the impact of Option B+ and ensure that access to PMTCT services was not reduced when single-dose nevirapine was removed from the available regimens, every facility offering antenatal care also needed to offer ART. This meant that the program had to double the number of ART sites in a single year—a number that had taken almost a decade of expansion to accomplish. To make this possible while maintaining adequate quality of services, the following significant changes took place.
Malawi national policy review to allow task shifting: Nurse technicians and medical assistants, the cadres below registered nurses and clinical officers, were included in those allowed to prescribe ART.
Training and retraining of clinicians on the integrated curriculum: All health workers previously trained in ART were retrained in PMTCT, and all PMTCT providers were retrained in ART. Previously untrained providers were also trained in an effort to saturate the national health services system with staff qualified to provide ART.
Review of the supply chain management system for HIV commodities: The ART and PMTCT supply chain management systems were combined and the buffer stock increased. The supply chain needed to serve double the number of health facilities: Before Option B+, the PMTCT supply chain was separate and frequently experienced stock-outs, whereas the ART supply chain functioned well.
Change of first-line regimen: The previous stavudine-containing regimen was no longer a feasible option because of toxicity concerns if used during pregnancy. The new national first-line combined tenofovir/lamivudine/efavirenz regimen was chosen in part for its tolerability in pregnant women with high CD4 counts, and so it had to be “ring-fenced”—strictly prioritized for this population only—in the first few months of Option B+. This would ensure that the remaining stocks of the existing stavudine-based first-line regimen were used up by current ART patients while Option B+ rolled out using the new regimen, thus avoiding multimillion dollar commodity wastage.
Confirmatory testing in ART clinic: Routine confirmatory HIV testing was introduced as a requirement before ART initiation to reduce the risk of starting people who receive false positives on lifelong ART.
Resource reallocations by donors and implementing partners coupled with efficient and effective resource utilization: Involvement and support of the implementing partners were needed at a far larger scale than ever before. US President’s Emergency Fund for AIDS Relief (PEPFAR) partners were requested to support the Malawian Ministry of Health as much as possible while the Ministry ensured each district had at least one partner to support them and asked implementing partners to work with their districts to develop implementation plans and organize and fund training at the district level.
Timing Option B+ rollout: The decision was made to both train providers and transition to Option B+ in all health facilities over a very short time (between July and December 2011). This was purposefully done to both maintain simplicity in supply chain processes and avoid confusion that could have arisen as a result of having different protocols existing concurrently after providers received training in the new integrated curriculum. By December 2011, the number of health facilities providing ART had more than doubled to 702 and all antenatal care and maternity clinics had ART available.
Building Consensus With Ministry of Health Management, Donors, and the United Nations Family
The first step in the process to gain broad consensus for Option B+ was made by the TWGs in March 2010 through consultations with PEPFAR, WHO, and other funding agencies. Because of the active engagement by these agencies in the TWGs and the participation of their technical staff in developing this proposed solution, much of the groundwork was already laid in preparing their senior staff for this discussion. In mid-2010, a policy paper on Option B+ was prepared by the HIV and AIDS Programme of the Ministry of Health, approved by senior management at the Ministry, and endorsed by the Global Fund.
Securing Additional Resources for Option B+
Global Fund grant budgets were revised to identify adequate funding for the implementation of Option B+, and approval for funding from the Global Fund and other partners was received by August 2010. This was coupled with the redirection of resources from the newly awarded one-time US $10 million PEPFAR PMTCT “Plus-up” monies at the request of the Ministry of Health, which provided most clinical and laboratory trainers and covered training costs. This tightly coordinated combination of newly available financial resources, provision of technical assistance to the Ministry of Health at national and district levels, and increased human resource capacity for initiating ART facilitated the rapid rollout of Option B+ in all health facilities over a very short time (between July and December 2011).
THE IMPACT OF OPTION B+ ON ART ACCESS AND VERTICAL TRANSMISSION OF HIV
Impact on ART Access
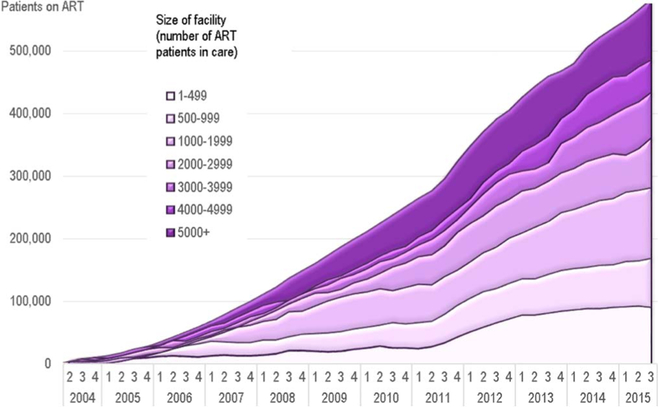
Option B+ boosted the national quarterly uptake of ART after the decentralization and integration of ART into every antenatal care facility. HIV testing and ART were now available at the smallest rural health centers, making it much more accessible to the population. The decision was made to provide ART in these small sites not only to HIV-positive pregnant and lactating women but also to other nonpregnant HIV-positive patients; it was a policy that facilitated the transfer of other ART patients to smaller facilities closer to home. As seen in Figure 1 (below), there was a sharp rise in the number of patients on ART in mid-2011, the greatest of which was seen at the smallest sites. By September 2015, 48% of the national ART patient cohort was in care at sites with fewer than 2000 patients.9
FIGURE 1.
Patients alive and on ART at the end of each quarter, stratified by size of facility.
Impact on the PMTCT Program
Option B+ had the anticipated positive impact on the coverage of the PMTCT program. In 2012, only 19.4% of known HIV-positive pregnant women coming for their first antenatal care visit were already on ART. By September 2015 (Q3), this had increased to 50% as a result of Option B+ (Fig. 2). There was, however, no corresponding increase in the uptake of infant antiretroviral medicine prophylaxis.
FIGURE 2.
Option B+ uptake in Malawi. ANC, antenatal care; ART/ARVs, antiretroviral therapy; AZT, zidovudine; sd NVP, single-dose nevirapine
The ongoing National Evaluation of Malawi’s PMTCT Program study, which started in 2014, has documented reduced early infant transmission under Option B+. Preliminary results showed that only 2.5% of infants <12 weeks of age whose mothers were on ART during pregnancy were HIV infected.10 Among women who were on ART before pregnancy, transmission was 1.4%, confirming the original rationale that Option B+ would also protect babies during subsequent pregnancies.
OPTION B+ LESSONS LEARNED AND CONSIDERATIONS FOR THE IMPLEMENTATION OF TREAT-ALL
There are several important lessons that Malawi learned during the implementation of Option B+, which are also considerations for countries transitioning to treat-all. These lessons cut across all levels, from the central Ministry of Health down to the individual patient.
Comprehensive Change Requires Effective Leadership, Coordination, and Technical Assistance
Option B+ was conceptualized not just as a new version of PMTCT but as part of a fundamental shift in the entire HIV program: the full integration of PMTCT and ART programs at each level, from the nationally standardized training curriculum and guidelines to the provision of antiretroviral medicines in antenatal care and maternity settings. This would not have been possible without the leadership of (1) the national HIV TWG, which set clear priorities and effectively steered the process, bringing all key stakeholders to the table and building consensus for this new and unproven approach; (2) the Ministry of Health’s senior management, who courageously endorsed this logical but (as yet) evidence-short intervention; and (3) the donors and other partners who were willing to provide technical and financial support for implementation. Regulatory bodies were key to decentralizing Option B+ by allowing the cadres posted to lower level health facilities (nurse technicians and medical assistants) to initiate and prescribe ART.
Clinical Guidelines Must Accommodate Health System Limitations
Option B+ simplified previous PMTCT and ART guidelines, removing documented barriers to ART access. When applied to national ART programs, the treat-all approach holds the same potential as Option B+ to streamline access and care, minimize barriers, and ensure that supportive components of services (such as human resources and the supply chain) benefit from the efficiency of the simplified programmatic approach. This streamlined and simplified approach to ART, however, requires the intentional simplification and streamlining of national guidelines to realize its maximum effect.
The primary health system challenges were inadequate human resources for health (as evidenced by an average 70% vacancy rate in facilities) and inadequate infrastructure (most facilities were constructed when the population was less than 30% of what it is today). Option B+ took a public health approach with guidelines simple enough to implement at the smallest and most remote health facilities and by lower level health cadres. It also removed the need for a CD4 count to determine ART eligibility, which was a major bottleneck to ART initiation in pregnant women.
Decentralize ART Services and Commodities Within Facilities
Additional programmatic changes that were implemented to ameliorate the high early defaulter rate in Option B+ included the further integration of ART services directly into antenatal care settings. The expansion of ART services to the site was not far enough; however, ART services and commodities needed to be available to the patient as part of their other health care services. Waiting in more than one multi-hour line on a single day’s visit is not a patient-friendly approach to care, and antenatal care clinics were advised to provide ART services and bottles of antiretroviral medicines to pregnant women during their antenatal care visit—a “one-stop shop” approach to service integration at the site level.
Educate the General Public About Changes in the Clinical Management of HIV
Ensuring that the general public understands the connection between treatment and epidemic control is an important area that countries need to proactively address as they transition to treat-all. Starting lifelong ART in HIV-infected people who are “otherwise well” was a complete paradigm shift from what the general public had been taught about the management of HIV disease. Ideally, a well-coordinated public and patient education campaign to ensure people understand the benefits and anticipated challenges of Option B+ had to be implemented at the same pace as the program.
This, however, was an area that was not addressed adequately in Malawi. Financial, human resource, and time constraints at all levels created unsurpassable barriers to keeping patient education at the forefront along with the other program areas, despite the acknowledged need. Technical effort across government and partners was prioritized ensuring that guidelines and training materials were developed, providers in the health sector were trained, district plans were developed, the program was launched, and services were available at every antenatal care clinic. Although patient education at health facilities was done with group sessions and one-on-one counseling sessions, it was not implemented consistently and new standardized educational tools were not provided for providers or patients.
Educate Patients About Clinic Processes to Improve Program Monitoring
Of the Option B+ women lost to follow-up who were successfully traced at a large urban ART clinic in the capital city of Lilongwe, it was found that 54% had stopped ART, 36% had transferred to another facility or received antiretroviral medicines from a different source, and 4% had died.11 These results suggest that the actual retention of patients on Option B+ is likely to be higher than national data indicate, underscoring the need to educate all ART patients about the process for transferring between facilities.
Challenges With Same-Day ART Initiation
When Option B+ started, the national guidelines advised providers to start women on ART the same day as diagnosis. The first 6-month retention data in the national program, however, indicated that defaulting was higher in Option B+ patients than in other ART patients: 17% of Option B+ patients were lost to follow-up at 6 months after initiating ART. Of those patients, 95% had defaulted, 4% had died, and 1% had stopped ART.12 Anecdotal evidence from the providers and quarterly clinical supervisors indicated the cause was inade quate time for counseling and preparation of healthy patients to take ART for the rest of their lives. Analysis of a large electronic patient-level database showed that starting ART on the same day as receiving a positive HIV test result was associated with early attrition, and the initial dip in retention was primarily the result of patients who never returned for a refill after the first 1 month supply was given. The conclusion was that many early Option B+ defaulters may not have ever started ART, despite being documented as initiated on ART when given the first month of antiretroviral medicines.
With these early results, the Ministry of Health immediately adjusted its national guidance and distributed a circular to all districts recommending that HIV-positive pregnant women start ART within 1 week of diagnosis and after a second counseling session with a treatment buddy, as was the requirement for the rest of the patients in the ART program. It is for this reason that as Malawi moves to treat-all, adequate counseling and preparation must be given to patients before initiating ART. This may depend on patient readiness and willingness (or lack thereof) to start ART on the same day as diagnosis.
Frequently Monitored and Validated Program Data Facilitate Rapid Program Improvement
Malawi has a very robust paper-based cohort monitoring system for ART that is validated every quarter during site visits by Ministry of Health staff and entered into a single database at the central level. This paper-based system has proven successful in the longitudinal monitoring of nearly 800,000 patients. The HIV program’s supervision and reporting structure also have facilitated the responsiveness of the national program in both identifying and responding to challenges, such as higher than expected early defaulter rates in Option B+ patients.
Because of the careful monitoring by the Ministry of Health through the quarterly supervision visits, it was both feasible to recognize the need for rapid programmatic adjustments and to make them. Although some early patient defaulting under Option B+ still occurs, it is not as great as when Option B+ started, and the Ministry of Health has documented that the gap between Option B+ retention and the overall national program retention almost closes between 24 and 36 months after starting ART.13 The importance of the routine site visits for supervision and data validation cannot be underestimated: To rapidly identify and respond to emerging challenges with the implementation of new programmatic guidelines, proactive monitoring of site-level data is required.
CONCLUSIONS
After Malawi’s courageous step forward into the unchartered territory of universal ART access and subsequent positive reports on progress achieved,9 WHO issued guidelines in 2013 that recommended Option B+, and it has since become the global standard of care. In Malawi, Cameroon and the United Republic of Tanzania (Boxes 2 and 3), Option B+ clearly demonstrated that universal ART is feasible to implement and that it achieves favorable patient outcomes in resource-constrained settings with serious health system challenges. It also showed the advantage of increasing access to ART through the complete decentralization of services across and within facilities and of task shifting to the lowest possible cadres.
Box 2. Evaluation of Early Experience Implementing Option B+ in the Northwest and Southwest Regions of Cameroon: 2013–February 2016.
Cameroon adopted Option B+ in 2012, but it chose to start with a pilot program in 22 facilities, funded by PEPFAR through the Centers for Disease Control and Prevention. Trained nurses and midwives offered ART to all HIV-positive antiretroviral medicine–naive pregnant and breastfeeding women. Peer educators tracked defaulters using home visits and telephone calls. Women who experienced miscarriage, stillbirth, and neonatal and infant deaths were transferred to the nearest ART clinic for ongoing HIV care and treatment.
From October 2013 to June 2015, 669 antiretroviral medicine–naive pregnant and breastfeeding women enrolled in the evaluation, the majority (99%) of whom accepted lifelong ART. Less than 1% refused lifelong ART but did agree to take ART during the pregnancy and breastfeeding periods. Fourteen women (2%) died, 141 (21%) were lost to follow-up, and 46 (7%) discontinued treatment. Retention at 12 months was 76%. Of the 540 HIV-exposed infants enrolled in the study, 93% had a DNA polymerase chain reaction test at 6–8 weeks postpartum, and early HIV transmission was 2.6%. Ten (2%) of the 536 HIV-exposed infants (HEIs) died, and 36 (7%) were lost to follow-up.
Option B+ is highly accepted by HIV-positive pregnant and breastfeeding women in Cameroon. Ensuring consistent availability and continuity of services required training many health workers at each facility. A robust tracking system using peer educators and Bikers for Health favors mother–baby pair retention and early infant diagnosis uptake. Transferring mothers from mother, newborn, and child health to ART clinics soon after ART initiation, delivery, or miscarriage often resulted in discontinuation of treatment. Laboratory tests are challenging, despite sample transportation system and cost subsidies. The loss to follow-up rate in Cameroon likely will improve as “treat-all” expands access and reduces the number of required laboratory tests.
Box 3. The United Republic of Tanzania’s PMTCT Option B+ Scale-up: Initiating ART Is Not the Same as Staying on ART.
In 2013, the United Republic of Tanzania piloted Option B+ or Lifelong ART for Pregnant and Lactating Mothers living with HIV (LLAPLa). In early 2014, the Ministry of Health assessed LLAPLa to identify preliminary programmatic gaps, challenges, and bottlenecks needed to be addressed for successful scale-up of the programme. A major finding of the assessment was the 36% retention rate at 3 months after ART initiation.
Building on the lessons learned during the pilot phase and in line with the subnational scale-up plan, the United Republic of Tanzania achieved a rapid and nationwide scale-up of Option B+ services. By the end of 2014, 84% of the 5892 reproductive and child health clinics could provide lifelong ART. During the same period, there was 90% ART coverage in the total estimated HIV-infected pregnant or breastfeeding women living with HIV. Additionally, there was an estimated 72% reduction in the number of new pediatric HIV infections from 2009.
The most pressing challenge remains the retention of women and their infants along the continuum of care. Although initiation rates are high, many mothers and infants disengage from HIV care in the postpartum period. This situation is made worse by the fact that although PMTCT data management was integrated into the routine national health management information system and care and treatment patient monitoring system, neither of these 2 systems can systematically report retention rates of mother–baby pairs in the context of HIV services.
To improve retention of women and infants, the program developed a national cohort follow-up system for mother–baby pairs. Based on results from the pilot phase, 60% of the PMTCT cohort started treatment for the first time in antenatal care, whereas 40% were already on ART by the time they attended the reproductive and child health (RCH) clinic. Retention in PMTCT care at 6 and 12 months was 75% and 72%, respectively. Women already on ART were more likely to be retained (84% and 80% at 6 and 12 months, respectively) than those starting treatment for the first time in antenatal care.
Retention monitoring as early as 1 or 3 months may help address the challenge of retention, especially among those initiating ART in antenatal care. By linking the health outcomes of mothers and infants, cohort monitoring can provide important information to health care providers on the HIV services provided to mother and infant and flag any gaps in care. This information is used to initiate corrective action, such as improving defaulter tracing programs.
Option B+ also has facilitated discussion about pediatric HIV treatment. As maternal ART has become the norm, the treatment gap between mothers and children has become more obvious. This has led to efforts to find ways to strengthen services for mother–infant pairs, including early infant diagnosis, pediatric ART, follow-up, and evaluation. The collective efforts of the 21 priority countries of the Global Plan in Africa will continue to contribute to a firm foundation for others now establishing treat-all in their own national ART programs.
Over time, we anticipate—and indeed hope—that the use of the term “Option B+” will disappear as treat-all becomes the norm. Although Option B+ may end up forgotten over time, its legacy will endure: it was one giant step toward ending AIDS by 2030.
Acknowledgments
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Estimating National HIV Prevalence in Malawi From Sentinel Surveil-lance Data: Technical Report. Lilongwe, Africa: National AIDS Commission; 2003. [Google Scholar]
- 2.van Oosterhout J, Bodasing N, Kumwanda J, et al. Evaluation of antiretroviral therapy results in a resource-poor setting in Blantyre, Malawi. Trop Med Int Health. 2005;10:464–470. [DOI] [PubMed] [Google Scholar]
- 3.Malawi HIV and AIDS Monitoring and Evaluation Report. Lilongwe, Africa: Malawi National AIDS Commission; 2008. [Google Scholar]
- 4.Malawi Ministry of Health Quarterly HIV Programme Report: January–March 2010. Lilongwe, Africa: Malawi Ministry of Health; 2010. [Google Scholar]
- 5.Schouten E, Jahn A, Midiani D, et al. Prevention of mother-to-child transmission of HIV and the health-related millenium development goals: time for a public health approach. Lancet. 2011;378: 282–284. [DOI] [PubMed] [Google Scholar]
- 6.van Lettow M, Bedell R, Landes M, et al. Update and outcomes of a prevention-of-mother-to-child (PMTCT) program in Zomba District, Malawi. BMC Public Health. 2011;11:426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Landes M, van Lettow M, Chan A, et al. Mortality and health outcomes of HIV-exposed and unexposed children in a PMTCT cohort in Malawi. PLoS One. 2012;7:e47337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rapid Advice: Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Infants. Geneva, Switzerland: World Health Organization; 2009. [PubMed] [Google Scholar]
- 9.Malawi Ministry of Health Integrated HIV Program Report July–September 2015 Lilongwe, Africa: Malawi Ministry of Health; 2015. [Google Scholar]
- 10.National HIV Transmission in 4–12 Week Olds in Malawi’s PMTCT Option B+ Program. Conference on Retroviruses and Opportunistic Infections (CROI); 2016; Boston. [Google Scholar]
- 11.Tweya H, Gugsa S, Hosseinipour M, et al. Understanding factors, outcomes and reasons for loss to follow-up among women in Option B+ programme in Lilongwe, Malawi. Trop Med Int Health. 2014;19:1360–1366. [DOI] [PubMed] [Google Scholar]
- 12.Integrated HIV Program Report April–June 2012. Lilongwe, Africa: Malawi Ministry of Health; 2012. [Google Scholar]
- 13.Integrated HIV Program Report July–September 2015. Lilongwe, Africa: Malawi Ministry of Health; 2015. [Google Scholar]