Abstract
Background
Diagnosing capitellar osteochondritis dissecans (OCD) can be difficult, causing delay in treating young athletes. The main aim of this retrospective diagnostic study was to determine which radiological technique is preferred to identify and classify elbow OCD.
Methods
We identified young patients who underwent elbow arthroscopy because of symptomatic OCD. We included all patients who had pre-operative radiographs, a computed tomography (CT) scan and magnetic resonance imaging (MRI) available. We assessed whether the osteochondral lesion could be identified using the various imaging modalities. All lesions were classified according to previous classifications for X-ray, CT and MRI, respectively. These results were compared with findings at arthroscopy.
Results
Twenty-five patients had pre-operative radiographs as well as CT scans and MRI. In six patients, the lesion was not visible on standard X-ray. In 20 patients, one or two loose bodies were found during surgery, consistent with an unstable lesion. Pre-operatively, this was seen on 11 X-rays, 13 MRIs and 18 CT scans.
Conclusions
Capitellar OCD lesions are not always visible on standard X-rays. A CT appears to be the preferred imaging technique to confirm diagnosis of OCD. Loose bodies are often missed, especially on standard X-rays and MRIs.
Keywords: arthroscopy, diagnostic study, elbow, osteochondritis dissecans, humeral capitellum, loose bodies
Introduction
Osteochondritis dissecans (OCD) of the elbow is a condition of the subchondral bone and overlying cartilage, mostly affecting a part of the humeral capitellum. The capitellum of the immature elbow has a tenuous vascular supply consisting of one or two posterior vessels. There is no metaphyseal blood supply until the physis closes.1,2 This makes the capitellum vulnerable to repetitive microtrauma in overhead athletes.
During overhead sports, such as baseball, gymnastics, volleyball, javelin throwing and tennis, tremendous valgus forces are generated across the elbow joint.3,4 These valgus forces result in attenuation on the medial side and compression of the lateral side. These compression forces can lead to injury of the poorly vascularized growth plate of the capitellum.5–9 This is why OCD most commonly occurs in the adolescent age.
The onset of symptoms is insidious and many athletes will initially only complain of inexplicit lateral-sided elbow pain. As signs and symptoms are vague primarily, obtaining the definite diagnosis in these young athletes is delayed for months or even years. Symptoms average 1–2 years before an appropriate treatment takes place.8
Treatment is conservative or operative, depending on type, stage and stability of the lesion.9,10 Early recognition and appropriate intervention may protect them from fragmentation of the OCD lesion and developing irreversible cartilage damage.7,8
Imaging usually starts with standard anteroposterior (AP) and lateral plain radiographs; however, plain radiographs lack sensitivity, which is approximately 44% to 47% according to previous studies.8,11,12 Magnetic resonance imaging (MRI) and computed tomography (CT) scans are probably more sensitive. There are some reports on the sensitivity and specificity of MRI versus X-rays. Satake et al.12 found a MRI sensitivity of 84%. Itsubo et al.13 found 100% sensitivity and 80% specificity for diagnosing OCD on MRI. Jans et al.14 reported a sensitivity of 100% on MRI, only when using all kinds of characteristics of an unstable elbow OCD lesion together. None of the characteristics was sensitive by itself. No data exist on the comparison of all three imaging techniques: standard X-ray, MRI and CT scans.
It is important to classify the lesion to determine whether it is stable or unstable. This will determine the type of treatment and is closely related to the prognosis. A stable lesion will most likely heal naturally with rest of the elbow but, when a lesion has become unstable, surgery provides significantly better results.8,9,12
The aim of the present study was to determine which radiological technique is preferred for the identification of OCD of the young elbow joint and to classify the OCD lesion.
Materials and methods
We retrospectively identified patients who underwent arthroscopy of the elbow because of a symptomatic OCD lesion between January 2008 and July 2014. All arthroscopies were performed by a single orthopedic surgeon (DE). Most patients were referred to us from other hospitals, whereas others came directly to our clinic. Therefore, patients had variable imaging modalities performed. Most patients had a pre-operative X-ray and MRI or a pre-operative X-ray and a CT scan. Some of these patients had undergone all three imaging modalities, mostly because they had been seen by several different doctors. We included just this last group of patients, who had pre-operative radiographs, MRI and a CT scan available, aiming to achieve a direct comparison of the imaging studies within one patient (Figures 1 to 3). Therefore, all patients missing one or more of these pre-operative imaging modalities were excluded.
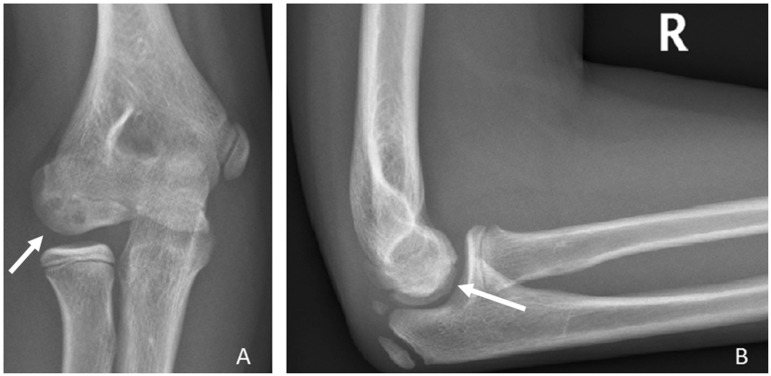
Figure 1.
Plain radiograph of the right elbow. The arrow shows an osteochondritis dissecans lesion of the capitellum. This lesion would be classified as Minami type I.15 (A) Anteroposterior. (B) Lateral.
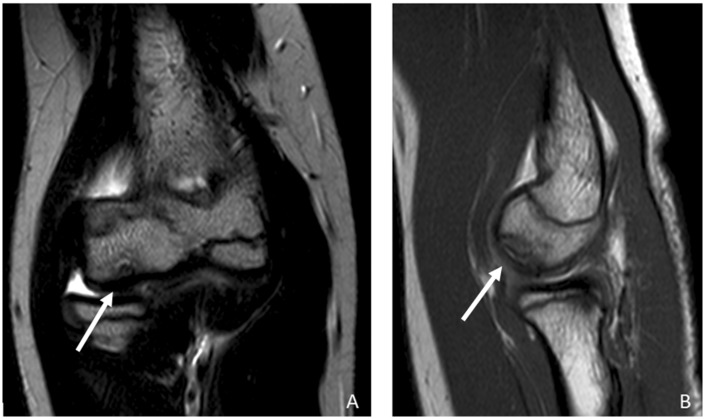
Figure 2.
Magnetic resonance images of an elbow affected with osteochondritis dissecans of the capitellum. The arrow is pointing at the lesion, which would be classified as type 3 according to Itsubo et al.13 (A) Coronal view. (B) Sagittal view.
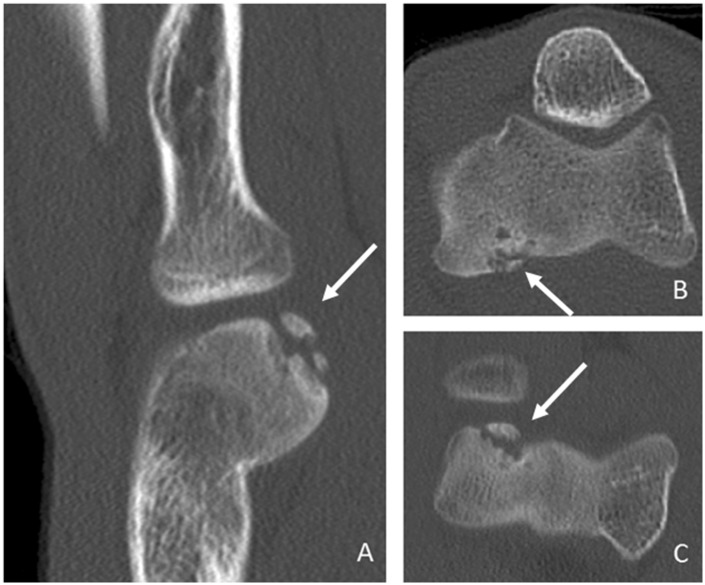
Figure 3.
Computed tomography scans of an elbow, with the arrows showing capitellar osteochondritis dissecans, stage 3 when classified by Clanton and DeLee16 (A–C).
All three imaging studies were reviewed by two experienced elbow and sports orthopedic surgeons (DE and MvdB). Both assessed independently whether or not the osteochondral lesion could be identified using the various imaging modalities. Any discrepancies were resolved by a consensus discussion.
All lesions were classified according to the classifications of Minami et al.,15 Clanton and DeLee,16 and Itsubo et al.13 for X-ray, CT and MRI, respectively (Table 1). There is no verified classification of OCD of the elbow for CT images; therefore we used the classification of Clanton and DeLee16 for osteochondritis dissecans of the knee. This is a well-known and validated classification system for OCD lesions.13,15,16
Table 1.
Classifications of capitellar osteochondritis dissecans (OCD)
| Minami classification of capitellar OCD (X-ray) | Itsubo classification of capitellar OCD (MRI) | Clanton and DeLee classification of knee OCD (CT) | |||
|---|---|---|---|---|---|
| I | Localized flattening or radiolucency | 1 | Normally shaped capitellum with several spotted areas of high signal intensity lower than that of cartilage | 1 | Depressed osteochondral fracture |
| 2 | Stage 1 + several spotted areas of higher intensity than that of cartilage | 2 | Osteochondral fragment attached by an osseous bridge | ||
| 3 | Stage 2 + both discontinuity and noncircularity of the chondral surface signal of capitellum and no high signal interface between lesion and floor | ||||
| II | Nondisplaced fragment | 4 | Lesion separated by a high intensity line in comparison with cartilage | 3 | Detached non-displaced fragment |
| III | Displaced or detached fragment | 5 | Capitellar lesion displaced from floor or defect of the capitellar lesion | 4 | Displaced fragment |
CT, computed tomography; MRI, magnetic resonance imaging.
Stable lesions: Minami grade I, Itsubo stages 1–2 and Clanton and DeLee stages 1–2.
Unstable lesions: Minami grade II–III, Itsubo stages 3–5, and Clanton and DeLee stages 3–4.
The location of the OCD lesion was described in the sagittal and coronal plane. The sagittal plane of the capitellum was equally divided into three parts: anterior, central and posterior. The coronal plane of the capitellum was also equally divided into three parts: lateral, central and medial.
A stable lesion was determined by the following classifications: Minami grade I, Itsubo stages 1 and 2, and Clanton and DeLee stages 1 and 2. An unstable lesion was in its turn classified by Minami grades II and III, Itsubo stages 3, 4 and 5, and Clanton and DeLee stages 3 and 4.12,13,15,16
All imaging results were compared to the gold standard defined as the findings observed at arthroscopy. The International Cartilage Repair Society has proposed an arthroscopic classification system for OCD lesions.17 Grade 1 indicates a stable lesion with a continuous but softened area covered by intact cartilage; grade 2 is a lesion with partial discontinuity that is stable when probed; grade 3 is a lesion with a complete discontinuity that is not yet dislocated; and grade 4 is an empty defect, as well as a defect with a dislocated fragment or a loose fragment lying within the bed. All lesions were defined as stable or unstable intra-operatively.
Patient records provided information on patients’ sex, age at the time of surgery, hand dominance, athletic activity, and time between onset of symptoms and diagnosis.
Results
Patient demographics
Of the 106 patients who underwent arthroscopy of the elbow because of symptomatic OCD of the capitellum, 25 patients had pre-operative radiographs as well as a CT scan and MRI available. The average age was 17 years, ranging from 12 years to 23 years. Thirteen patients were male and 12 were female. In 18 patients, the right elbow was affected and, in seven patients, the left elbow was affected. This was the dominant arm in 17 patients. All patients participated in at least one sport. Half of them were either gymnasts or tennis players (Table 2). The median period between onset of symptoms and diagnosis was 24 months, ranging from 1 month to 192 months. Patients all complained of vague lateral elbow pain with loading of the elbow that worsened with activity. Some also showed loss of motion or locking symptoms. Six of the 25 patients reported an acute trauma to their elbow.
Table 2.
Patient characteristics
| Patient | Age (years) | Sex | Operated side | Hand dominance | Duration symptoms (months) | Sport |
|---|---|---|---|---|---|---|
| 1 | 12 | F | R | L | 192 | Gymnastics |
| 2 | 15 | F | R | R | 10 | Volleyball |
| 3 | 13 | M | R | R | 48 | Gymnastics |
| 4 | 16 | F | R | R | 72 | Handball |
| 5 | 16 | F | R | R | 24 | Swimming |
| 6 | 16 | M | R | R | 2 | Tennis |
| 7 | 13 | F | R | R | 72 | Gymnastics |
| 8 | 19 | M | R | R | 29 | Tennis |
| 9 | 20 | M | R | R | 120 | Field hockey/tennis |
| 10 | 22 | M | R | R | 24 | Canoeing/water polo |
| 11 | 17 | M | R | R | 60 | Tennis |
| 12 | 14 | F | R | R | 40 | Gymnastics |
| 13 | 20 | M | L | R | 108 | Bike cross |
| 14 | 19 | F | L | R | 6 | Gymnastics |
| 15 | 15 | M | R | R | 3 | Soccer |
| 16 | 13 | F | R | R | 48 | Kickboxing |
| 17 | 12 | F | R | R | 12 | Gymnastics |
| 18 | 23 | M | R | R | 1 | Darts/fitness training |
| 19 | 22 | F | L | R | 12 | Horseback riding/gymnastics |
| 20 | 15 | F | R | R | 24 | Tennis |
| 21 | 20 | M | R | L | 10 | Soccer goalkeeper |
| 22 | 15 | M | L | R | 1,5 | Field hockey goalkeeper |
| 23 | 18 | M | L | R | 11 | Korfball/fitness training |
| 24 | 15 | M | L | L | 120 | Judo |
| 25 | 21 | F | L | R | 24 | Fitness training |
M, male; F, female; R, right; L, left.
Pre-operative imaging
The OCD lesion was visible on X-ray in 19 of the 25 elbows. It was seen on nine X-rays only on the AP radiograph and, on 10 X-rays, the lesion was seen on both AP and lateral views. Grading of all OCD lesions is presented in Table 3. The radiographic grading did not correspond to either the MRI or CT grading.
Table 3.
Pre-operative classification of the osteochondritis dissecans lesion of the humeral capitellum
| No. of lesions | % | |
|---|---|---|
| Pre-operative radiography grade (Minami) | ||
| Not visible | 6 | 24 |
| I | 4 | 16 |
| II | 8 | 32 |
| III | 7 | 28 |
| Pre-operative MRI stage (Itsubo) | ||
| Not visible | 1 | 4 |
| 1 | 0 | 0 |
| 2 | 2 | 8 |
| 3 | 5 | 20 |
| 4 | 14 | 56 |
| 5 | 3 | 12 |
| Pre-operative CT stage (Clanton and DeLee) | ||
| Not visible | 0 | 0 |
| 1 | 1 | 4 |
| 2 | 1 | 4 |
| 3 | 7 | 28 |
| 4 | 16 | 64 |
CT, computed tomography; MRI, magnetic resonance imaging.
One lesion that was not observed on X-ray was also not seen on MRI. The other lesions were all visible on MRI. All lesions were diagnosed on CT. The sagittal views appeared to be most sensitive; the OCD lesion was visible in 22 of 25 MRIs and 25 of 25 CT scans. The coronal views showed the lesion in 21 of 25 MRIs and 25 of 25 CT scans. The axial views were the least accurate, showing the lesion in 16 of 25 MRIs and 21 of 25 CT scans.
During surgery, the OCD lesion was unstable and accompanied by one or two loose bodies in 20 of the 25 patients (Table 4). Pre-operatively, this was seen in 11 of the X-rays, in 13 of the MRIs and in 18 of the CT scans. This means that the sensitivity of these imaging techniques for determining whether the lesion is unstable is 55%, 65% and 90%, respectively.
Table 4.
Stability of the capitellar osteochondritis dissecans lesion: comparing imaging with intra-operative findings
| Unstable intra-operative | Stable intra-operative | |
|---|---|---|
| X-ray | ||
| Unstable (II, III) | 11 | 4 |
| Stable (0*, I) | 9 | 1 |
| MRI | ||
| Unstable (4, 5) | 13 | 4 |
| Stable (0*, 1, 2, 3) | 7 | 1 |
| CT | ||
| Unstable (3, 4) | 18 | 5 |
| Stable (1, 2) | 2 | 0 |
CT, computed tomography; MRI, magnetic resonance imaging.
0*, no lesion or loose body seen.
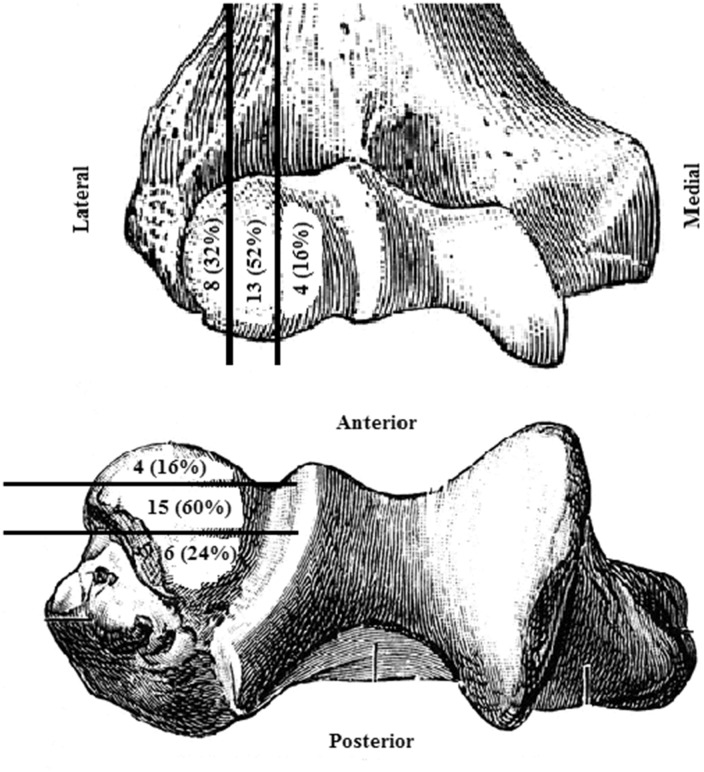
Localization of the OCD lesion was determined by CT (Figure 4). Most lesions were located in the central-central region of the capitellum.
Figure 4.
To describe the location of the osteochondritis dissecans lesions, the coronal and sagittal planes of the capitellum are equally divided into three parts. Coronal plane: lateral, central and medial. Sagittal plane: anterior, central and posterior. The number of lesions (and their percentage) is stated in the parts where they were localized according to the CT scan.
Discussion
Capitellar OCD occurs mainly in young athletes who are engaged in overhead sports. Unfortunately, there is still a serious delay in diagnosis and treatment. It is noteworthy that the average age of our patients is fairly high at 17 years, ranging up to 23 years, as a result of a missed or delayed diagnosis. One patient was, in fact, symptomatic for 16 years.
Early recognition and appropriate intervention may protect adolescents from fragmentation of the OCD lesion and developing irreversible cartilage damage. Treatment depends on type, stage and stability of the lesion. In the present study, CT of the elbow is the best radiological technique for identifying and classifying capitellar OCD.
Satake et al.12 also compared radiographs, CT scans and MRIs with intra-operative findings, although their patients did not all have CT and MRI studies for a direct comparison. It was found that pre-operative radiographs correlated with an intra-operative diagnosis of unstable lesions in 44% of cases when using the Minami classification. When specifically looking at closure of the capitellar epiphyseal line on X-ray, a sensitivity of 88% of detecting was found for an unstable lesion. Articular irregularity and T2 high signal intensity interface on MRI correlated with the intra-operative finding of whether the lesion was stable or unstable, both with a sensitivity of 73%.12
Jans et al.14 looked at specific findings of an unstable OCD lesion of the elbow on MRI: high T2 signal intensity rim, cysts, high T2 signal intensity fracture line extending through the articular cartilage overlying an OCD lesion, and a fluid-filled OCD. A sensitivity of 100% was reported when using all criteria together. None of these criteria was sensitive by itself.14
To our knowledge, there are no studies describing the sensitivity of CT in OCD of the elbow. One reason for this could be that, in clinical practice, CT scans might not be used as much as MRI for detecting OCD lesions. However, CT can accurately identify and localize a lesion at the same time as defining its extent. Furthermore, CT had the advantage of a wider availability and a shorter acquisition time compared to MRI.18
Of course, hazards of radiation exposure must always be weighed against their clinical utility when ordering imaging studies, especially when delivered to a largely skeletally immature population. Nevertheless, it is good to keep in mind that the effective dose for a CT scan of the elbow is only 0.14 mSv. In comparison, the effective doses of CT scans of the shoulder and thoracic spine are 2.06 mSv and 17.99 mSv, respectively. The background dose as a result of natural radiation exposure is approximately 3 mSv per person per year.19
In the present study, localization of the OCD lesion was determined by CT. It is our opinion that defining localization of the lesion during surgery is not suffiently accurate and reliable. It also shows a great discrepancy compared to a CT scan. Kimball et al.2 showed a predominant posterior blood supply to the distal lateral humerus and a relative watershed area on the medial side. This is not coherent with the localizations of the lesions in the present study. Therefore, this probably is not the only issue concerning the development of capitellar OCD.
The strengths of the present study include the relative large group of patients who all had pre-operative X-ray as well as MRI and CT scans of their elbow. To our knowledge, this is the first study comparing all three pre-operative imaging techniques with the surgical findings of OCD of the humeral capitellum. In the present study, well known, validated, classification systems have been used.13,15,16
We acknowledge limitations to the present study. First, it is a retrospective study in which all patients had already undergone surgery for symptomatic OCD of the elbow. We did not include a control group of patients without OCD when assessing radiographs, MRI and CT scans. Nevertheless, it shows how many OCD lesions are missed on standard radiographs.
Second, the intra- and inter-observer reproducibility of the findings of the three imaging techniques was not assessed. Both orthopedic surgeons reviewed all images independently. However, any discrepancies were resolved by a consensus discussion. When looking at grading the OCD lesions, Claessen et al.20 demonstrate that the inter-observer reliability of the currently used classification systems for OCD of the humeral capitellum is poor to fair. The Minami classification was significantly the most reliable when classifying the different stages of OCD of the humeral capitellum, although still with only fair agreement.20
Third, Takahara et al.8 suggest using an anterior image of the elbow in 45° flexion because OCD lesions may be underdiagnosed on the basis of AP radiographs of the elbow in extension. In the present study, none of the patients had AP radiographs taken in 45° of elbow flexion. Changing that protocol might improve the sensitivity of radiographic imaging of OCD. Fourth, the quality of the MRI was variable. Referring hospitals do not all use the same resolution power. Next to that, our patients are younger and more active, which might have resulted in more body movement. This has a greater effect on MRIs than on CT.
Conclusions
In conclusion, based on the findings in the present study, it appears that a CT of the elbow is the best imaging technique for confirming the diagnosis of OCD, especially in the unstable stage. An OCD lesion of the capitellum is not always visible on X-ray and loose bodies are often missed on standard X-rays and by MRI.
A young patient with lateral elbow pain has OCD until proven otherwise. To prevent delay in diagnosis, we strongly recommend additional imaging studies, preferably CT.
Acknowledgements
This study has been presented at the yearly convention of the Dutch Orthopedic Society.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Not required for this article.
References
- 1.Haraldsson S. The intra-osseous vasculature of the distal end of the humerus with special reference to the capitulum. Acta Orthop Scand 1958; 27: 81–93. [PubMed] [Google Scholar]
- 2.Kimball JP, Glowczewskie F, Wright TW. Intraosseous blood supply to the distal humerus. J Hand Surg 2007; 32A: 642–646. [DOI] [PubMed] [Google Scholar]
- 3.Bradley JP, Petrie RS. Osteochondritis dissecans of the humeral capitellum. Diagnosis and treatment. Clin Sports Med 2001; 20: 565–590. [DOI] [PubMed] [Google Scholar]
- 4.Eygendaal D, Rahussen FT, Diercks RL. Biomechanics of the elbow joint in tennis players and relation to pathology. Br J Sports Med 2007; 41: 820–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith MV, Bedi A, Chen NC. Surgical treatment for osteochondritis dissecans of the capitellum. Sports Health 2012; 4: 425–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takahara M, Ogino T, Sasaki I, et al. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res 1999; 363: 108–115. [PubMed] [Google Scholar]
- 7.Takahara M, Ogino T, Takagi M, et al. Natural progression of osteochondritis dissecans of the humeral capitellum: initial observations. Radiology 2000; 216: 207–212. [DOI] [PubMed] [Google Scholar]
- 8.Takahara M, Mura N, Sasaki J, et al. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. Surgical technique. J Bone Joint Surg Am 2008; 90(Suppl 2): 47–62. [DOI] [PubMed] [Google Scholar]
- 9.Van den Ende KI, McIntosh AL, Adams JE, et al. Osteochondritis dissecans of the capitellum: a review of the literature and a distal ulnar portal. Arthroscopy 2011; 27: 122–128. [DOI] [PubMed] [Google Scholar]
- 10.Ruchelsman DE, Hall MP, Youm T. Osteochondritis dissecans of the capitellum: current concepts. J Am Acad Orthop Surg 2010; 18: 557–567. [DOI] [PubMed] [Google Scholar]
- 11.Kijowski R, De Smet AA. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol 2005; 34: 266–271. [DOI] [PubMed] [Google Scholar]
- 12.Satake H, Takahara M, Harada M, Maruyama M. Preoperative imaging criteria for unstable osteochondritis dissecans of the capitellum. Clin Orthop Relat Res 2013; 471: 1137–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Itsubo T, Murakami N, Uemura K, et al. Magnetic resonance imaging staging to evaluate the stability of capitellar osteochondritis dissecans lesions. Am J Sports Med 2014; 42: 1972–1977. [DOI] [PubMed] [Google Scholar]
- 14.Jans LBO, Ditchfield M, Anna G, et al. MR imaging findings and MR criteria for instability in osteochondritis dissecans of the elbow in children. Eur J Radiol 2012; 81: 1306–1310. [DOI] [PubMed] [Google Scholar]
- 15.Minami M, Nakashita K, Ishii S, et al. Twenty-five cases of osteochondritis dissecans of the elbow. Rinsho Seikei Geka 1979; 14: 805–810. [Google Scholar]
- 16.Clanton TO, DeLee JC. Osteochondritis dissecans. History, pathophysiology and current treatment concepts. Clin Orthop Relat Res 1982; 167: 50–64. [PubMed] [Google Scholar]
- 17.Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 2003; 85A(Suppl 2): 58–69. [DOI] [PubMed] [Google Scholar]
- 18.Verhagen RA, Maas M, Dijkgraaf MG, et al. Prospective study on diagnostic strategies in osteochondral lesions of the talus. Is MRI superior to helical CT? J Bone Joint Surg Br 2005; 87: 41–46. [PubMed] [Google Scholar]
- 19.Biswas D1, Bible JE, Bohan M, et al. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am 2009; 91: 1882–1889. [DOI] [PubMed] [Google Scholar]
- 20.Claessen FM, van den Ende KI, Doornberg JN, et al. Shoulder and Elbow Platform & Science of Variation Group. Osteochondritis dissecans of the humeral capitellum: reliability of four classification systems using radiographs and computed tomography. J Shoulder Elbow Surg 2015; 24: 1613–1618. [DOI] [PubMed] [Google Scholar]