Abstract
Background:
There are a few reports on the healing status of the cartilage after the treatment of tibial plateau fracture. In this study, we analyzed the healing status of articular cartilage using second-look arthroscopy with clinical and radiological results from patient's in schatzker Type I, II, and III tibial plateau fracture.
Materials and Methods:
43 patients operated between January 2011 and December 2013 were included in this retrospective study. Radiological evaluation was performed by comparing simple radiographs from the preoperative, postoperative, and final followup period. Clinical evaluations were performed using the Knee Society Knee Score (KSKS) and the Knee Society Functional Score (KSFS). Moreover, second-look arthroscopic evaluation was performed during implant removal, and cartilage healing status was classified according to the International Cartilage Repair Society grading system (ICRS).
Results:
In all 43 patients, bony union was achieved with a mean duration of 13.7 weeks. The degree of cartilage healing was poor when the step-off was high (P = 0.016). Furthermore, even in cases with satisfactory step-off <2 mm, there was no case with complete cartilage healing. Between ICRS grade and clinical results, the respective Pearson coefficient for KSKS and KSFS were r = −0.62 and r = −0.59 indicating mean statistically significant negative correlations (P = 0.001).
Conclusion:
Even though step off was reduced anatomically and clinical outcome was excellent or good, there was not always complete cartilage healing in a followup on second-look arthroscopy. Therefore, we focused on not only radiologic and clinical outcome but also the actual status of cartilage with second-look arthroscopy.
Keywords: Cartilage healing, second-look arthroscopy, tibial plateau fracture
Introduction
Tibial plateau fracture invades the articular surface of the knee and accounts for 1% of all fractures.1 The resulting incongruity and step off of the tibial plateau lead to abnormal loading of the cartilage and subchondral bone, which gradually induces degeneration of the cartilage. Hence, the treatment for displaced tibial plateau fracture aims to achieve accurate reduction and firm fixation of the articular surface and to provide proper treatment for accompanying injuries such as meniscus tearing and ligament injury, enabling to minimize articular dysfunction by traumatic arthritis.2,3,4
Several surgical techniques have been introduced to treat complex tibial plateau fracture involving displacement of the articular surface.5,6 Arthroscopic reduction and internal fixation (ARIF) first were introduced by Caspari et al. and Jennings in 1980, enabling direct visualization of intraarticular fractures and accurate anatomical reduction. In addition, this technique enable the diagnosis and treatment of accompanying intraarticular injuries, complete irrigation and removal of loose bodies. These advantages significantly reduce the incidence of postoperative complications. Therefore, when surgical treatment is needed for tibial plateau fractures, especially Schatzker classification Type I, II, and III, the ARIF procedure is widely utilized.7,8,9,10,11,12,13
Despite the development of these surgical techniques, malalignment and secondary arthritis have been reported after surgery for tibial plateau fracture.14 Despite radiological examination showing the absence of step-off of the articular surface, arthroscopic examination in a few other studies showed step-off of the articular surface with incomplete articular regeneration and cartilage injury which induce posttraumatic arthritis.15,16 These secondary arthritis after tibial plateau fracture may occur because of the inherent characteristics of the human chondrocyte: once damaged, complete regeneration is difficult, and the extent of the damage increases progressively with time.4,17,18
While previous studies on the surgical treatment of the tibial plateau fractures showed improved clinical and radiological outcomes, few studies directly focused on the healing status of the cartilage.15,16 Therefore, in this study, we compared the healing status of the articular cartilage in patients with Schatzker Type I, II, and III tibial plateau fracture, treated using ARIF, during second-look arthroscopy with clinical and radiological results.
Materials and Methods
48 patients who underwent ARIF for tibia plateau fracture with the Schatzker10 classification of Type I, II, or III between January 2011 and December 2013 were included in this tudy. Our operative indications in tibial plateau fracture were as follows: step-off of the articular surface >3 mm, tibial condylar widening 5 mm, and tibial condylar tilt >5°.19 However, the following cases were performed through open reduction and internal fixation without arthroscopy: cases that have multiple damages or comminuted fracture, and cases that have the high risk of compartment syndrome due to articular fluid leakage. Five cases in which the patient refused the removal of the implant after bony union due to old age or underlying diseases were excluded. Finally, 43 patients treated with second-look arthroscopy during implant removal after bony union were included in this retrospective study.
Out of 43 patients, 31 were men and 12 were women. The mean age was 49 years (range 23-66 years) at the time of second-look arthroscopy. The mean followup period was 38 months (range 24-60 months). The most common causes of injury were car accidents (n = 34) followed by falls (n = 5), sports accidents (n = 3), and other incident (n = 1).
This study was conducted after approval of the Institutional Review Board at present hospital.
The study relates to Before surgery, simple radiograph and computed tomography were performed to evaluate the fracture pattern and extent of depression. In addition, magnetic resonance imaging (MRI) was used to identify other injuries including meniscus, cruciate ligament and collateral ligament injuries. All 43 cases were categorized using the Schatzker classification; 7 cases were Type I (16%), 28 cases were Type II (65%), and 8 cases were Type III (18%).
Operative procedure
All patients were treated using ARIF. The depressed articular surface of Schatzker type II and type III fractures, in particular, were elevated with an impactor operated through a small window during fluoroscopy and arthroscopy. In the event of large proximal metaphyseal defects, allogenic cancellous chip bone (TranZgraft; Tissue Banks International, Baltimore, MD, USA), or autogenous iliac bone was filled to support the articular surface and prevent collapse. Osteosynthesis was performed with a cannulated screw (Zimmer, Warsaw, US) and/or an AO locking plate (LCP proximal tibia plate; Synthes, West Chester, PA, USA).15,20
After obtaining the complete bony union of the fracture site, the risks and benefits of second-look arthroscopy and metal removal were explained to the patients. These procedures were performed for consenting patients. Similar to the first surgery, second-look arthroscopy was performed through the anterolateral and anteromedial portal, and the cartilage healing status was classified using the International Cartilage Repair Society (ICRS) grading system.21 The ICRS classification system is used to characterize cartilage injury on the basis of lesion area and depth and classified from Grade I to Grade IV: Grade I for chondral softening or blistering with an intact surface, Grade II for shallow superficial ulceration, fibrillation, or fissuring involving <50% of the depth of the articular surface, Grade III for deep ulceration, fibrillation, fissuring or a chondral flap involving 50% or more of the depth of the articular cartilage without exposure of subchondral bone, and Grade IV for full-thickness chondral wear with exposure of subchondral bone [Figure 1].21 Additional procedures such as arthroscopic debridement, adhesiolysis, and additional meniscectomy were performed when abnormal arthroscopic findings were found.
Figure 1.
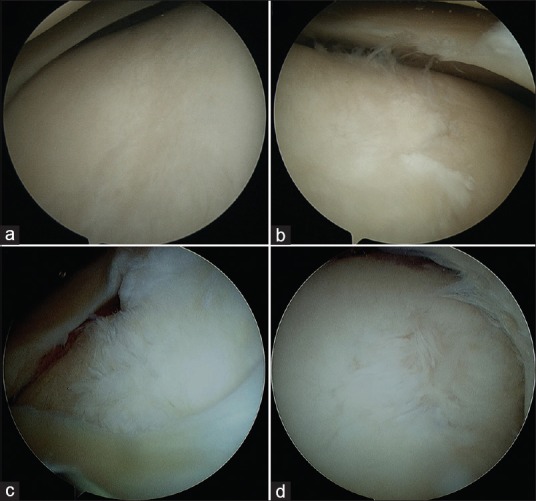
Arthroscopic International Cartilage Repair Society grade (a) International Cartilage Repair Society Grade I, (b) International Cartilage Repair Society Grade II, (c) International Cartilage Repair Society Grade III, (d) International Cartilage Repair Society Grade IV
The accompanying injuries were as follows: two cases of anterior cruciate ligament injury, 22 cases of lateral meniscus tear, 6 cases of medial meniscus tear, and 20 cases of medial collateral ligament injury.
In the 2 cases with an anterior cruciate ligament injury, we confirmed 1 case of avulsion fracture and 1 case of partial tear through MRI taken before surgery. In the case of avulsion fracture, physical examination before surgery under anesthesia confirmed instability and pull out suture was used for fixation. In the case with partial tear, no instability was observed on physical examination under anesthesia and tear was only present in anteromedial bundle on arthroscopic evaluation. Therefore, conservative treatment was performed for these stable anterior cruciate ligament injuries. In 20 of the 22 cases with a confirmed lateral meniscal tear, meniscus repair was performed with the Inside-Out technique using nonabsorbable sutures during tibial plateau fracture surgery. In the other two cases, partial meniscectomy was performed because the tear site was in the inner third section of the meniscus. In 4 out of 6 cases where medial meniscal tearing was confirmed, meniscus repair was performed. Moreover, partial meniscectomy was performed in the other 2 cases.
All 20 cases of medial collateral ligament injury were Grades I, or II with 30° flexion valgus stress test of knee joint. These cases were treated conservatively.
Immediately after surgery, removable cylinder splint was used along with antibiotics and sterilization to control inflammation and elevation of lower limb and ice packing were used to resolve swelling. Through patella movement exercise, contracture of the patellofemoral joint was prevented. In addition, straight leg raising exercises and quadriceps femoris strengthen exercises were performed for preventing atrophy of the quadriceps femoris.22 Moreover, continuous passive motion of the knee joints was started from 0° to 90° on the second postoperative day. After 2 weeks, active ROM with assistance was recommended until ROM of 90°. At the 4th week, the cylinder splint was replaced with a hinged knee brace and toe-touch weight bearing with crutches was started and limited weight-bearing was allowed only after obtaining radiographic evidence of healing. In the 6th week, partial weight bearing of 25% started followed by a gradual increase. After 10–12 weeks, bony union was confirmed through radiological evaluation and full weight-bearing exercise was performed.22
Radiological, clinical, and second-look arthroscopic evaluation
Radiological evaluation was performed by comparing simple radiographs in the preoperative, postoperative, and final followup period. Satisfactory reduction was defined as step off <2 mm in final followup radiograph.9
Clinical evaluation was performed by comparison of the ROM, patient's pain, alignment and stability of the lower extremity by using the Knee Society Knee Score (KSKS). KSKS defines “Excellent” as a score ≥90, “Good” as a score between 80 and 89, “Fair” as a score between 70 and 79, and “Poor” as a score 69. To evaluate walking and climbing stairs and whether to use assistive equipment for walking, Knee Society and Functional Score (KSFS) was used; KSFS has also defined “Excellent” as score ≥90, “Good” as score between 80 and 89, “Fair” as score between 70 and 79, and “Poor” as score <70.23
At the final followup, healing status of the articular cartilage using second-look arthroscopy was classified with the ICRS grade. Moreover, those results were compared and analyzed with radiological and clinical results.
Statistical method
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software version 20.0 (IBM Corporation, Armonk, NY). A Chi-square test was used to analyze the relationship between the final followup radiological results and the ICRS grade which were regarded as categorical data. For analysis of the relationship between KSKS or KSFS and the ICRS grade which were regarded as continuous data, the Pearson correlation test was used. For all tests, P < 0.05 was considered statistically significant.
Results
In all 43 cases, bony union was achieved with an average time of 13.7 weeks (range 12–17 weeks). There was no loss in the reduction of the articular surface or need for secondary surgery for the bony union in all cases. The final followup radiographs showed step-off of <2 mm in 40 cases and step-off over 2 mm in 3 cases.
Regarding the ROM of the knee at final followup, flexion contracture averaged 3.2° (range 0°–15°), further flexion averaged 128.5° (range 120°–140°). The average KSKS was 89.8 (range 70–100) with 27 excellent cases, 9 good cases, and 7 fair cases. Furthermore, average KSFS was 88.3 (range 70–100) with 27 excellent cases, 9 good cases, and 7 fair cases which were the same as KSKS.
Finally, the healing status of the articular cartilage determined through second-look arthroscopy was ICRS Grade 1 for 2 cases, Grade 2 for 28 cases, Grade 3 for 12 cases, and Grade 4 for 1 case.
Based on these results, we compared the radiological results with the status of cartilage healing with Chi-square test. In cases with step-off <2 mm in the simple radiograph, two were ICRS Grade 1, 29 were Grade 2, and 9 were Grade 3. In cases with step-off over 2 mm, two were Grade 3, and one was Grade 4. Chi-square test demonstrated a significantly worse cartilage healing status in cases with step-off over than 2 mm (P = 0.016). However, there was no complete cartilage healing even in cases with step-off <2 mm [Figure 2].
Figure 2.
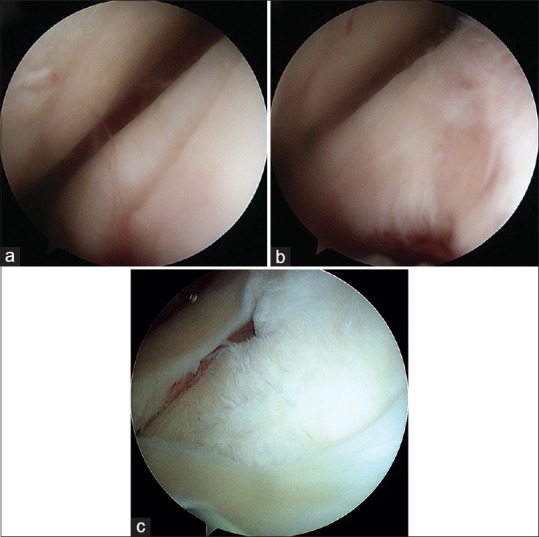
(a) A 42-year-old male patient with Schazcher Type-II fracture. (b) Even though primary anatomic reduction is achieved, (c) International Cartilage Repair Society grade III chondral injury is seen during second-look arthroscopy in postoperative 18 months. ICR: International Cartilage Repair Society
The clinical results at the final followup were compared with the ICRS grade representing cartilage healing status with Pearson correlation test. In cases classified as ICRS Grade 1, 1 case was excellent according to KSKS and 1 case was good. In cases of ICRS Grade 2, 26 cases were excellent, 2 cases were good and 2 cases were fair. In cases of ICRS Grade 3, 8 cases were good and 2 cases were fair. Finally, in case of ICRS Grade 4, 1 case was fair. The Pearson coefficient was that r = −0.62 (P = 0.001) indicating a statistically significant negative correlation between ICRS grade and KSKS. For KSFS, in cases classified as ICRS 1, 1 case was excellent, and 1 case was good. In cases of ICRS Grade 2, 25 cases were excellent, 3 cases were good and 2 cases were fair. In cases of ICRS Grade 3, 5 cases were good and 5 cases were fair. Finally, in the case of ICRS Grade 4, 1 case was excellent. The Pearson coefficient was r = −0.59 (P = 0.001), indicating a significant negative correlation Between ICRS grade and KSFS. Therefore, this means that cartilage healing status was worse, the clinical outcome was worse.
Discussion
In this study, we evaluated and compared the degree of reduction, clinical outcomes, and cartilage healing status through second-look arthroscopy in patients with tibial plateau fractures of Schatzker type I, II, and III underwent ARIF. As a result, we confirmed that in cases with step-off over 2 mm, cartilage healing status was significantly poor than cases with step-off less 2 mm. Moreover in second look arthroscopy, as cartilage healing status is worse, clinical outcome was worse. However, even with satisfactory reduction which occurred in cases with step-off <2 mm, there was no case with complete cartilage healing, and most cases had cartilage injury over ICRS Grade 2.
In previous animal studies, it was reported that when the degree of step-off is similar or thinner than the cartilage of the articular surface, there is a higher chance of cartilage healing.24 In an animal experiment with rabbits, it is reported that group with complete reduction showed cartilage healing with hyaline cartilage.25 However, humans and animals have different biochemical characteristics and cartilage healing abilities. Moreover, it is difficult to obtain long term followup results with animal due to the limitation of animal research. Therefore, it is difficult to apply the results of animal studies to human clinical cases. Human cartilage cells have a long lifespan andcannot be replaced by hyaline cartilageunlike animal cells, even with a turnover to other tissue.26 In addition, regenerative ability of chondrocyte is impaired after impaction injuries such as tibial plateau fracture, which make it difficult for cartilage to heal perfectly in spite of complete anatomical reduction.26 In studies by Cetik, 12 cases with the bony union in tibial plateau fractures had incomplete articular recovery and cartilage defects.15 In addition, in another study by Lee, involving 20 patients with Schatzkar Type II tibial plateau fracture treated by open reduction and internal fixation, 16 cases had step-off <2 mm. 11 of the 16 cases had ICRS Grade II and III cartilage injuries.16 Similarly, in our study, there was no case with complete cartilage healing in second-look arthroscopy although 40 of 43 cases achieved reduction with step-off <2 mm and most of the cases were clinically “Excellent” or “Good.”
The injured cartilage can worsen as times goes on even if the radiographic and clinical results are good and cartilage injury is small size.26 We think it will be important to check the cartilage healing status regardless of the radiographic and clinical results after tibial plateau fracture surgery, especially in case of the young and active patient. Therefore, we used arthroscopy for estimating the cartilage status because it is the most accurate method to evaluate the postoperative status of articular cartilage. Arthroscopy is possible to detect minimal damage of articular cartilage with incipient osteoarthritis and allows for the debridement, adhesiolysis, meniscectomy, and removal of loose bodies and chondral fragment to mechanical irritation and synovial inflammation.27,28,29 Furthermore, arthroscopic procedure provides pain relief and functional improvement in short-term followup. In addition, these procedures delay the progression of traumatic arthritis and delay or prevent total knee arthroplasty in long term followup, especially in patients with a traumatic osteoarthritis.28,30,31
There are a few limitations in this study. First, it was a retrospective study. Second, this study only included Schatzker type I, II, and III injuries, which makes it difficult to generalize the result to all tibial plateau fractures. Finally, the followup period was relatively short to explain the incidence of traumatic arthritis by cartilage injury. In spite of these limitations, this study has much meaningful strengths. First, we try to minimize other factors affecting cartilage healing by managing the meniscus and ligament appropriately that we can do. Second, this study included 43 cases, which is a larger sample than previous studies. Third, all patients had an operation by the same surgeon using the same method and treated with same protocol after the operation. Furthermore, this study is noteworthy in that it focused on the actual state of the cartilage by second-look arthroscopy which is different from previous studies that focused on the clinical and radiological result.
Conclusion
In this study, most patients with Schatzker Type I, II, and III tibial plateau fracture who treated using ARIF obtained a normal joint range of motion and good clinical and radiological results. Despite these results, we found there was no complete cartilage healing on second-look arthroscopy because regeneration of human cartilage is limited. Therefore, we think it will be important to focus on not only radiological and clinical outcome but also the actual status of cartilage healing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lubowitz JH, Elson WS, Guttmann D. Part I: Arthroscopic management of tibial plateau fractures. Arthroscopy. 2004;20:1063–70. doi: 10.1016/j.arthro.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Mehin R, O’Brien P, Broekhuyse H, Blachut P, Guy P. Endstage arthritis following tibia plateau fractures: Average 10-year followup. Can J Surg. 2012;55:87–94. doi: 10.1503/cjs.003111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scheerlinck T, Ng CS, Handelberg F, Casteleyn PP. Medium-term results of percutaneous, arthroscopically-assisted osteosynthesis of fractures of the tibial plateau. J Bone Joint Surg Br. 1998;80:959–64. doi: 10.1302/0301-620x.80b6.8687. [DOI] [PubMed] [Google Scholar]
- 4.Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P, et al. Tibial plateau fractures: Functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop. 2010;34:565–70. doi: 10.1007/s00264-009-0790-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Musahl V, Tarkin I, Kobbe P, Tzioupis C, Siska PA, Pape HC, et al. New trends and techniques in open reduction and internal fixation of fractures of the tibial plateau. J Bone Joint Surg Br. 2009;91:426–33. doi: 10.1302/0301-620X.91B4.20966. [DOI] [PubMed] [Google Scholar]
- 6.Dall’oca C, Maluta T, Lavini F, Bondi M, Micheloni GM, Bartolozzi P, et al. Tibial plateau fractures: Compared outcomes between ARIF and ORIF. Strategies Trauma Limb Reconstr. 2012;7:163–75. doi: 10.1007/s11751-012-0148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fowble CD, Zimmer JW, Schepsis AA. The role of arthroscopy in the assessment and treatment of tibial plateau fractures. Arthroscopy. 1993;9:584–90. doi: 10.1016/s0749-8063(05)80410-4. [DOI] [PubMed] [Google Scholar]
- 8.Guanche CA, Markman AW. Arthroscopic management of tibial plateau fractures. Arthroscopy. 1993;9:467–71. doi: 10.1016/s0749-8063(05)80324-x. [DOI] [PubMed] [Google Scholar]
- 9.Holzach P, Matter P, Minter J. Arthroscopically assisted treatment of lateral tibial plateau fractures in skiers: Use of a cannulated reduction system. J Orthop Trauma. 1994;8:273–81. doi: 10.1097/00005131-199408000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The toronto experience 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 11.Burdin G. Arthroscopic management of tibial plateau fractures: Surgical technique. Orthop Traumatol Surg Res. 2013;99:S208–18. doi: 10.1016/j.otsr.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Chan YS, Chiu CH, Lo YP, Chen AC, Hsu KY, Wang CJ, et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year followup results. Arthroscopy. 2008;24:760–8. doi: 10.1016/j.arthro.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 13.Kiefer H, Zivaljevic N, Imbriglia JE. Arthroscopic reduction and internal fixation (ARIF) of lateral tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc. 2001;9:167–72. doi: 10.1007/s001670000175. [DOI] [PubMed] [Google Scholar]
- 14.Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Results of a multicenter, prospective, randomized clinical trial. J Bone Joint Surg Am. 2006;88:2613–23. doi: 10.2106/JBJS.E.01416. [DOI] [PubMed] [Google Scholar]
- 15.Cetik O, Cift H, Asik M. Second-look arthroscopy after arthroscopy-assisted treatment of tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc. 2007;15:747–52. doi: 10.1007/s00167-006-0276-6. [DOI] [PubMed] [Google Scholar]
- 16.Lee HJ, Jung HJ, Chang EC, Lee JS, Jung HS. Second-look arthroscopy after surgical treatment of schatzker type II plateau fractures through the lateral submeniscal approach. Arch Orthop Trauma Surg. 2014;134:495–9. doi: 10.1007/s00402-014-1932-9. [DOI] [PubMed] [Google Scholar]
- 17.Marsh JL, Buckwalter J, Gelberman R, Dirschl D, Olson S, Brown T, et al. Articular fractures: Does an anatomic reduction really change the result? J Bone Joint Surg Am. 2002;84-A:1259–71. [PubMed] [Google Scholar]
- 18.Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer followup. J Bone Joint Surg Am. 2002;84-A:1541–51. doi: 10.2106/00004623-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Honkonen SE. Indications for surgical treatment of tibial condyle fractures. Clin Orthop Relat Res. 1994;302:199–205. [PubMed] [Google Scholar]
- 20.Siegler J, Galissier B, Marcheix PS, Charissoux JL, Mabit C, Arnaud JP, et al. Percutaneous fixation of tibial plateau fractures under arthroscopy: A medium term perspective. Orthop Traumatol Surg Res. 2011;97:44–50. doi: 10.1016/j.otsr.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(Suppl 2):58–69. doi: 10.2106/00004623-200300002-00008. [DOI] [PubMed] [Google Scholar]
- 22.Suh JT, Ahn JM, Kim TW, Cho HM. Arthroscopically assisted reduction and internal fixation of intraarticular fractures of tibial plateau. J Korean Orthop Assoc. 2012;47:96–103. [Google Scholar]
- 23.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;248:13–4. [PubMed] [Google Scholar]
- 24.Lovász G, Llinás A, Benya PD, Park SH, Sarmiento A, Luck JV, Jr, et al. Cartilage changes caused by a coronal surface stepoff in a rabbit model. Clin Orthop Relat Res. 1998;354:224–34. doi: 10.1097/00003086-199809000-00027. [DOI] [PubMed] [Google Scholar]
- 25.Lefkoe TP, Walsh WR, Anastasatos J, Ehrlich MG, Barrach HJ. Remodeling of articular step-offs. Is osteoarthrosis dependent on defect size? Clin Orthop Relat Res. 1995;314:253–65. [PubMed] [Google Scholar]
- 26.Minas T. A primer in cartilage repair. J Bone Joint Surg Br. 2012;94:141–6. doi: 10.1302/0301-620X.94B11.30679. [DOI] [PubMed] [Google Scholar]
- 27.Nakamae A, Ochi M, Deie M, Adachi N, Shibuya H, Ohkawa S, et al. Clinical outcomes of second-look arthroscopic evaluation after anterior cruciate ligament augmentation: Comparison with single- and double-bundle reconstruction. Bone Joint J. 2014;96-B:1325–32. doi: 10.1302/0301-620X.96B10.34282. [DOI] [PubMed] [Google Scholar]
- 28.Grieshober JA, Stanton M, Gambardella R. Debridement of articular cartilage: The natural course. Sports Med Arthrosc Rev. 2016;24:56–62. doi: 10.1097/JSA.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 29.Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: Systematic review and meta-analysis of benefits and harms. Br J Sports Med. 2015;49:1229–35. doi: 10.1136/bjsports-2015-h2747rep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee DJ, Elfar JC. Utility of arthroscopic surgery for osteoarthritis of the knee. Geriatr Orthop Surg Rehabil. 2015;6:47–9. doi: 10.1177/2151458514552722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stuart MJ, Lubowitz JH. What, if any, are the indications for arthroscopic debridement of the osteoarthritic knee? Arthroscopy. 2006;22:238–9. doi: 10.1016/j.arthro.2006.01.008. [DOI] [PubMed] [Google Scholar]


