Abstract
Background:
There has been a gradual increase in the revision TKA (RTKA) workload due to expanding indications of total knee arthroplasty (TKA), coupled with improving patient longevity. Western countries are already looking at their data on RTKA to plan for the future heath care needs of these patients. Limited data is available on RTKA from developing countries. Our study attempts to fill this gap in knowledge.
Materials and Methods:
We prospectively documented details of all RTKA performed at our centre for a period of six years (2011-16). We recorded the volume, causes and time to failure from index surgery of all RTKA and further recorded microbiological pattern in septic failures. We looked at the proportion of each cause of failure and time from index surgery.
Results:
Of the 5068 TKA procedures performed from January 2011 to December 2016, 201 (4%) were first-time revisions. The predominant cause of revisions was prosthetic infection (61%) followed by aseptic loosening (18%) and instability (7%). In the early, mid term, and late-failure groups, prosthetic infection remained the main cause of failure. In 47% of the septic revisions, the offending organisms could be identified and of those identified most (67%) were Gram-negative.
Conclusion:
The volume of first-time RTKA procedures (4%) at our center remained low compared with that of the Western countries. In Western countries, the incidence of late aseptic failures was higher than that of early-septic failures, whereas in our study, revisions were more commonly performed in the early-failure group (48%) and most failures were due to prosthetic infection (61%).
Keywords: Aseptic loosening, epidemiology, infection, revision, total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is one of the most common major surgical procedures being performed.1,2,3 Socioeconomic growth in developing countries has made the TKA accessible to a very large population of patients with arthritis. There has been a steady rise in the need for RTKA due to increasing longevity and expanding indications of primary TKA.4,5,6 Compared to primary TKA procedures, revision TKA (RTKA) surgery is skill, infrastructure, and cost intensive. Management of septic revisions costs considerably more than that of aseptic revisions. Developed Western countries have already recognized the socioeconomic burden of revision arthroplasty,2,4,5,6,7,8,9 whereas developing countries have just realized its impact. According to the recent literature (2011–2015) from developed Western countries, aseptic loosening, instability, and prosthetic infection, in that order, remain the predominant causes of knee revisions.10,11,12,13 Limited epidemiological data exist from developing countries till date.14,15,16,17,18 Presumably, they may have similar revision arthroplasty workload in the near future. Developing countries differ from the developed Western countries in many aspects. They have a distinctly different patient profile in terms of age, morphology, disease severity, and lifestyle. Quality of the primary arthroplasty care available to the patients also differs from that of the developed Western countries. Prevalence of severe deformities, poor bone stock, and rheumatoid disease increases surgical difficulties and impairs the success and longevity of the primary TKA procedures. Concurrently, use of modern implants with wear-resistant bearing surfaces in patients with limited activity levels may have a positive impact on the longevity of arthroplasties in developing countries. In the absence of comprehensive joint registries or large institutional databases, envisaging the volume and type of revision arthroplasty workload that developing countries are likely to experience in the near future is difficult.
The objective of the present study was to study the epidemiology of the RTKA procedures performed at a single, state-sponsored, tertiary-care joint replacement facility in India, for determining the volume and causes of failure, particularly, in terms of time-to-failure from the index surgery. Such analyses would assist surgeons and hospitals in effecting optimum clinical care guidelines and protocols in developing countries. The state could also use the data for planning health-care resources for optimum care delivery to patients.
Materials and Methods
Data source
The present study was conducted at an exclusive arthroplasty center co-located with a tertiary-care research and referral military hospital, which is a state-sponsored facility providing free medicare to patients referred from across country. Since its inception in 1997, there has been a gradual increase in the volume of primary TKA procedures performed. The center has maintained all patient records till date. Due to a substantial increase in primary arthroplasty procedures and a parallel rise in revision surgical procedures, the center automated its joint registry in 2011. After obtaining the approval of the institutional review board, we examined the data of all RTKA procedures performed between January 1, 2011 and December 31, 2016. With the assistance of operating surgeons, VK and BD, the research fellow completed questionnaires related to the causes of failure including intraoperative findings. We also recorded microbiological data in cases of septic revisions.
Variables
We considered the burden of revision as a proportion of the total arthroplasty workload. We recorded patient demographics, causes of failures, and time-to-failure from the index surgery. Furthermore, we determined whether the index TKA procedure was performed at our Institute or elsewhere. In septic revision cases diagnosed based on Musculoskeletal Infection Society (MSIS)19 criteria including knee aspiration, the microbiology reports were reviewed to determine the type of offending organism and antibiotic sensitivity pattern. We evaluated the clinical course of revisions for 6 years (2011–2016) with respect to their index procedure.
Statistics
Statistical analysis was performed with Stata Version 12 (Stata Corp LP, Texas, USA). We reviewed the patient demographic data including age, sex, body mass index (BMI), comorbidities and American Society of Anaesthesiologist (ASA) score in the primary TKA versus RTKA group in terms of mean, mode, and standard deviation if it was a continuous variable and rate if it was a dichotomous data. We then compared the failure rates as per cause and time to failure (Early <2 years from index procedure; midterm 2–10 years; and late >10 years). We also analyzed the trend over time (2011–2016).
Results
A total of 5068 TKA procedures were performed from January 2011 to December 2016, of which 201 (4%) were first-time revisions. Most of them (60%) underwent primary TKA procedures at other hospitals. The average age of patients undergoing revisions was 64.7 years (range 26–86 years). Revisions were performed for 175 posterior-stabilized knees, 8 cruciate-retaining knees, 16 primary constrained knees, and 2 unicondylar knees.
The yearly trend of first-time RTKA accounted for 2%–7% of the total procedures [Figure 1]. Early (<2 years from index procedure) failures accounted for almost half (48%) of the cases; midterm (2–10 years) and late (>10 years) failures were observed in 30% and 22% of cases, respectively. Infection was the cause of failure in 61% (n = 123) followed by aseptic loosening and instability [Figure 2]. Besides, we also evaluated the temporal profile of the causes of failure, and infection remained the main cause of early, midterm, and late-failure groups. Aseptic loosening was mainly observed in midterm and late-failure groups, whereas instability was the predominant cause of failure in the early-failure group after prosthetic infection; however, some cases of instability were also observed in the midterm and late-failure groups [Figure 3]. Age distribution of patients undergoing RTKA was similar to those undergoing primary TKA procedures and >60% of patients were aged 50–70 years. Functional comorbidity index, which indicates the number of comorbidities in a patient, was similar in both RTKA and primary TKA groups, with most patients having ≤2 comorbidities (90%). However, according to the ASA score, the anesthetic risk was assessed as Grade III (high risk) in 23% of revision cases and 11% of primary cases. 336 patients in primary TKA group (28%) and 356 patients in RTKA group (30%) were obese (BMI >30). In 53% of the septic revision cases (diagnosed preoperatively based on MSIS criteria), the offending organisms could not be cultured. Of the 47% positive cultures, 67% were Gram-negative infections and 33% were Gram-positive infections [Table 1]. The temporal profile of these infections indicated a steady rise in delayed and late infections, and most of these infections were due to Gram-negative fastidious organisms that could not be cultured [Figure 4]. Very few Gram-positive staphylococcal infections were noticed.
Figure 1.
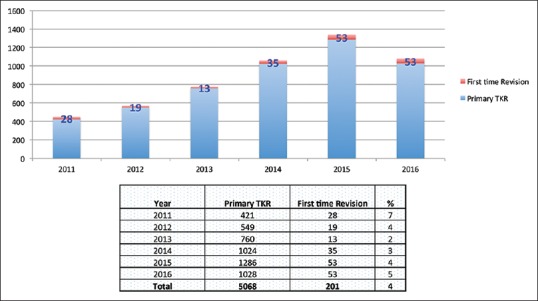
Revision total knee arthroplasty workload over 5 years at our institute (2011–2016)
Figure 2.
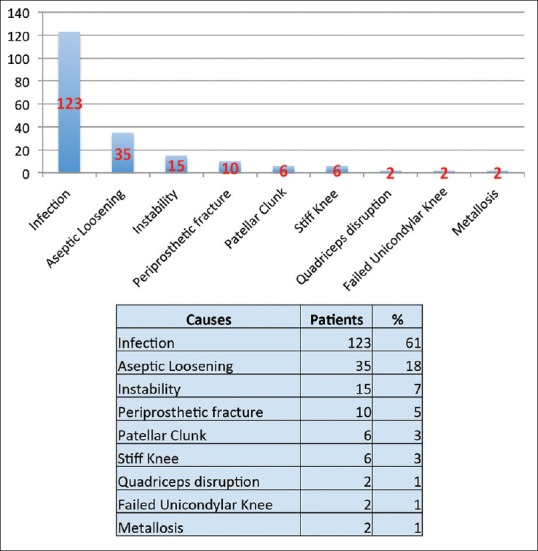
Causes of revision total knee arthroplasty
Figure 3.
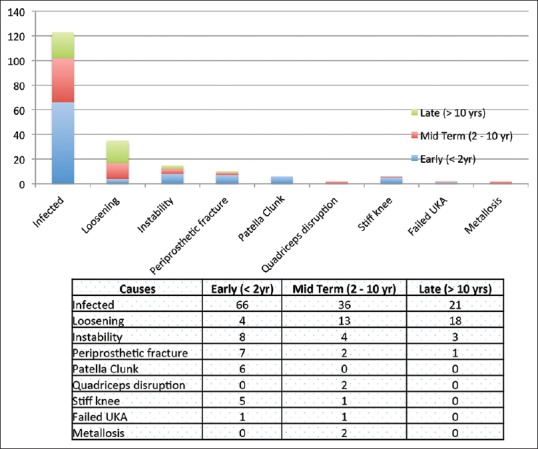
Causes of revision as per temporal profile (early, delayed and late failures)
Table 1.
Microbiological studies of infected total knee replacements (culture report and antibiotic sensitivity of organism grown)
| Culture result | (n) | ||
|---|---|---|---|
| Culture negative | 65 | ||
| Culture positive | 58 | ||
| Organism type | Organism | (n) | Antibiotic sensitivity |
| Gram positive | Staphylococcus aureus | 9 | Clindamycin, linezolid, vancomycin, trimethoprim/sulfamethoxaxole, rifampicin |
| Staphylococcus haemolyticus | 5 | Linezolid, teicoplanin, vancomycin, trimethoprim/sulfamethoxazole | |
| Staphylococcus epidermidis | 4 | Gentamicin, tigecycline, nitrofurantoin, rifampicin | |
| Staphylococcus hominis | 1 | Gentamicin, tigecycline, nitrofurantoin, rifampicin | |
| 19 | |||
| Gram negative | Acinetobacter baumannii | 4 | |
| Escherichia coli | 5 | Amikacin, piperacillin, meropenem | |
| Burkholderia cepacia | 11 | Ceftazidime, meropenem, minocycline, septran | |
| Stenotrophomonas maltophilia | 1 | Trimethoprim/sulfamethoxazole | |
| Klebsiella oxytoca | 1 | Ampicillin, piperacillin/tazobactam, ceftriaxone, cefepime, imipenem, amikacin, ciprofloxacin | |
| Pseudomonas aeruginosa | 7 | Imipenem, meropenem, amikacin, gentamicin, tobramycin, ciprofloxacin, moxifloxacin | |
| Enterobacter aerogenes | 3 | Ertapenem, meropenem, amikacin, gentamicin, tobramycin | |
| Providencia rettgeri | 1 | Piperacillin/tazobactam | |
| Klebsiella pneumoniae | 3 | Tigecycline, colistin, trimethoprim/sulfamethoxazole | |
| Enterobacter cloacae | 3 | Ertapenem, imipenem, meropenem amikacin | |
| 39 | |||
TKA=Total knee Arthroplasty
Figure 4.
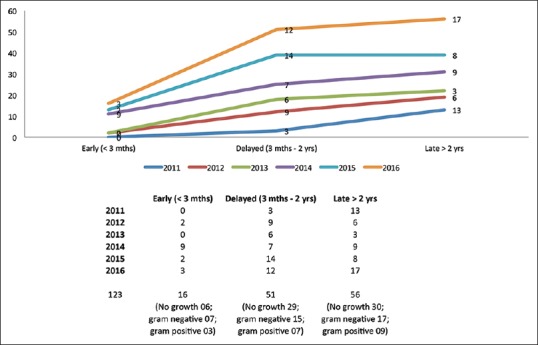
Temporal and microbiological profile of septic revisions
Discussion
Increasing longevity and extending the indications of TKA to young patients might lead to an increased need for RTKA procedures. Analysis of administrative health data from the developed Western countries5,6,19,20,21,22 predicts that the overall revision hip replacement and RTKA procedures performed would increase by 137% and 601%, from 2005 to 2030, respectively.5 Labek et al. studied cumulative results from worldwide joint register dataset and brought out a revision rate of TKA as 6.45% at 5 years of followup and 12.9% at 10 years.23 Collective socioeconomic impact of revision joint replacement needs to be scrutinized. This study endeavored to describe the burden of revision knee surgery at a single center in a developing country and to compare it with the current literature from the developed and developing countries [Table 2].
Table 2.
Summary of recent published literature from developed and developing countries including public health data
| Studies (institutional studies) | Years of operation | n* | n# | Percentage+ | Early revisions$ (%) | Infection (%) | Aseptic loosening and poly wear (%) | Instability (%) | Stiff knee (%) | Fracture (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Developed countries | ||||||||||
| Sharkey et al.3 | 2003-2012 | 781 | 10,003 | 7.8 | 38 | 27 | 40 | 8 | 5 | 5 |
| Le et al.8 | 2001-2011 | 253 | NA | NA | 46 | 24 | 14 | 26 | 18 | 2 |
| Thiele et al.24 | 2005-2010 | 358 | NA | NA | 46 | 15 | 22 | 22 | NA | NA |
| Schroer et al.13 | 2010-2011 | 844 | NA | NA | 35 | 16 | 31 | 19 | 7 | NA |
| Dalury et al.11 | 2000-2012 | 820 | NA | NA | 49 | 18 | 23 | 18 | 9 | NA |
| Callies et al.10 | 2001-2010 | 1449 | NA | NA | 14 | 32 | 24 | 7 | 5 | 3 |
| Developing countries | ||||||||||
| Motififard et al.18 | 2011-2013 | 24 | 353 | 6.8 | 7 | 44 | 9 | 1 | 1 | NA |
| Koh et al.17 | 2008-2012 | 643 | 20,234 | 3.2 | 0 | 38 | 33 | 7 | 3 | 2 |
| Kasahara et al.15 | 2006-2011 | 140 | 4047 | 3.4 | NA | 24 | 40 | 9 | NA | 4 |
| Kim et al.16 | 1992-2012 | 256 | 11,816 | 2.1 | NA | 25 | 45 | 16 | 3 | 3 |
| Hossain et al.14 | 1999-2008 | 349 | NA | NA | 32 | 33 | 28 | NA | NA | NA |
| Our study (India) | 2011-2015 | 201 | 5068 | 4.0 | 48 | 61 | 18 | 7 | 3 | 5 |
| Public health data | ||||||||||
| Bozic et al.25 | 2005-2010 | NA | NA | NA | NA | 25 | 16 | 10 | NA | 2 |
| Swedish Knee Arthroplasty Register annual report (2011)26 | 2002-2011 | NA | NA | NA | NA | 27 | 22 | 12 | NA | 2 |
| Bhandari (US health data)4 | 2010 | NA | NA | NA | NA | 40 | 13 | 20 | 11 | NA |
*Total revision TKA performed, #Total number of TKA performed in the same duration, +Revision workload percentage, $Revisions done within 2 years of index procedure. TKA=Total knee arthroplasty, NA=Not available
From 2011–2016, first-time RTKA procedures were 4% of the total TKA workload, which is in accordance with the rates (2%–7%) from a few studies from developing countries.14,15,16,17,18 However, it was less than the volume of revision workload documented by Rothman Institute (7.8%; 2003–2012) in their recent publication.3 In developed Western countries, the rate of early revisions (within 2 years from the index surgery) has decreased (30%–50%).3,10,11,12,13,24 In contrast, most of the RTKA procedures performed at our center were early revisions (48%). It seems that we are yet to experience large volumes of wear-related late-aseptic failures, which have already echoed as a prime reason for revisions in developed countries.
Prosthetic infection, aseptic loosening, and instability were the three main causes of RTKA. In recent literature from developed Western countries,10,11,12,13,24 aseptic loosening is the main cause of RTKA, whereas infection was the predominant cause of RTKA in our study; 61% of cases underwent revisions due to prosthetic infections. This finding is consistent with the high revision rates due to prosthetic infections observed in the published literature from Korea17 and the Middle East.14,18 Recent US health data published by Bhandari et al.4 revealed that infection was the cause of RTKA in 40% of the cases. In the present study, early, midterm, and late revisions were essentially due to prosthetic infections. This is a remarkably high incidence considering that at similar single centers data the incidence was 27% (Rothman Institute3), 15%,24 18%,11 and 16%.13 Incidence of prosthetic infection after primary TKA is multifactorial and different predisposing factors have to be considered depending on early or late presentation of prosthetic infection. Quality of primary TKA care, which includes preoperative patient optimization, multispecialty perioperative management, and modern surgical facility with standardized protocols, plays a crucial role in avoiding early infections. Compromise in any of the aforesaid factors might result in prosthetic infections. Conferring the literature from the Western countries, Gram-positive organisms remain the predominant cause of prosthetic infections. However, in our study, of the positive cultures (47%), 67% were Gram-negative and only 33% were Gram-positive. The offending organism could not be identified (as they may have been fastidious and of low virulence) in 53% of cases. On the basis of the trend from 2011 to 2016, there has been a steady rise in delayed and late prosthetic infections caused by low-virulence Gram-negative organisms. Gram-negative infections are generally hospital-acquired and could be due to a breach in sterility at any stage of care. This is a preventable cause of periprosthetic infection and practicing safe care delivery can dramatically reduce its incidence. This finding highlights the need to review the institutional prophylactic antibiotic protocols, including the use of antibiotic cements while performing primary arthroplasties and empirical extended-spectrum antibiotic use while managing septic revisions. The study observed a high rate of negative periprosthetic cultures (53%) in patients diagnosed with prosthetic joint infection based on MSIS criteria. Sixty percent patients who underwent RTKA at our institute were referred from other centers and in many cases, patients had already been exposed to multiple antibiotics before receiving definitive surgical treatment; this could have contributed to negative periprosthetic culture rates. Intraoperatively, in all cases, five samples from different regions of the knee were sent for microbiological testing. At our institute, conventional sampling and tissue culture techniques were used. Recently available advanced techniques such as sonification of retrieved prosthesis, specialized culture media, extended periods of culture, and polymerase chain reaction techniques to isolate and identify bacterial genome were not used. Using conventional microbiological techniques, the detection rate of tissue culture, as reported, in cases of septic revisions has been 55%–70%.27 However, newer techniques now can yield a positivity rate of 80%–100%.28 It is imperative to adopt newer standardized microbiological techniques to improve positive culture and guide treatment. Low virulence and drug resistance of these hospital-acquired infections may also be a cause of delayed and late presentation of prosthetic infections, and thus remains the main cause of revisions even in midterm-failure (2–10 years) and late-failure (>10 years) groups. We managed all prosthetic joint infections with two-stage revision. In culture negative infections, we had to use the broad-spectrum antibiotic cover for 6 weeks followed by an antibiotic free period of 2 weeks. Following this, patients were again evaluated (MSIS criteria) to rule out infection before taking up for implantation of the prosthesis. In some cases, we also had to perform repeated debridement and exchange of spacers to render the joints infection-free.
Aseptic loosening, which is a failure of prosthesis and implant interface, was the second common cause of RTKA (18%) in the present study. Although recent studies coming out of some countries show aseptic loosening as the main cause of RTKA (20%–40%),10,11,12,13,24 large population-based public health data from developed nations7,20,21,27,29,30 still maintain aseptic loosening as the second most common cause of revisions after prosthetic infections, which is consistent with the findings of our study. We observed PE wear-related aseptic loosening only in 16 cases, which were equally distributed among midterm-failure (2–10 years) and late-failure (>10 years) groups. Bearing surface wear is multifactorial; it depends on the quality of bearing surface, patient's activity level, patient's weight, and limb alignment. Bearing surface wear is generally observed in late-aseptic failures; however, half of the aseptic failures in our study were observed in early and midterm failures (17/35 cases). Articular surface wear was not observed in the midterm-failure group; however, considerable tilting of the tibial (8 cases) and femoral (3 cases) components was observed in addition to subchondral collapse and failure of the supporting bone. Debonding of cement from the prosthetic component was observed on the tibial side in the early-failure group (2 cases). We analyzed the postoperative full weight-bearing standing hip to ankle plain radiographs of these patients and observed that their limbs were in a 3°–7° of varus alignment. Furthermore, these patients were obese (BMI >30). Poor limb alignment and obesity coupled with dubious cementing technique may have contributed to these midterm-aseptic failures. In the late-failure group (18 cases), all cases experienced PE-wear particle induced synovial reaction and osteolysis, which led to aseptic loosening. However, PE-wear rates were very low (9%) and were consistent with those published in recent reports from the Western countries. Low PE-wear could be due to the improvement in contemporary bearing surface characteristics.3 Seven of these 18 cases received constrained inserts.
The third most common cause of RTKA observed in our study was instability (7%); this finding is consistent with the data provided by the Rothman Institute (7.5%).3 According to the recent literature and public health data [Table 2], instability remains the cause of revisions in 8%–26% of the cases. According to the temporal profile of causes of failure, the cases were well-distributed in early, midterm, and late-failure groups. Most cases (8/15) were observed in the early-failure group. The posterior cruciate failed in 4 cases of TKA with cruciate-retaining insert leading to instability. In the remaining 4 cases, improper balancing might have resulted in instability. The remaining cases of instability were observed in the midterm-failure (3 cases) and late-failure (4 cases) groups. In the midterm-failure group, two of the 3 cases received a constrained insert and wear at the stabilizing post was observed in addition to varus-valgus instability. In all cases of late instability, considerable PE-wear was observed in addition to the damage to the stabilizing post of the articular insert.
Periprosthetic fracture accounted for revision in 10 patients (5%); this finding is consistent with the Rothman Institute data (4.7%). Four of the nine-supracondylar femur fractures occurred due to considerable anterior femoral cortex notching (>10% of the width of the distal femur as seen in plain lateral radiograph at the upper border of the femoral implant) and remaining five fractures occurred in patients with rheumatoid disease and poor bone stock. The only case of proximal tibial fracture occurred in a patient with rheumatoid disease at the tibial keel tip.
Stiff knee (movement range <15°–90°, where it was better preoperatively) was the cause of revision in 6 patients (3%). However, the specific cause of stiffness could not be ascertained. It could have been due to poor rehabilitation leading to arthrofibrosis. One patient complained instability and gradually developed stiff knee, due to repeated synovitis. Three patients improved after extensive arthrolysis, capsular releases, and insert change. In the other three cases, implant revision and extensive soft tissue releases were performed, the deficient bone was treated using a stemmed implant and a constrained insert.
Patellar clunk was the cause of revision in six cases. In three cases, fat pad and excessive synovial tissue around patella were excised and secondary resurfacing of the patella was done. In two cases, the patella had already been resurfaced; therefore, only synovial tissue excision was performed along with lateral facetectomy. Only one patient underwent secondary patellar resurfacing for painful crepitus. Two patients had quadriceps tendon failure; one patient had avascular necrosis of the patella with complete fragmentation and resorption over 2-year postoperative period and the other had a neglected patellar tendon avulsion from the lower pole of patella after a fall at home. Only two cases of metallosis were observed after wear and breakage of the post of the constrained articular insert at long term followup (>10 years). Two symptomatic unicondylar knees were revised to total knee implant due to persistent activity related pain.
The study has a few limitations. Our center is a specialized tertiary care referral center for arthroplasty; therefore, we received patients from all over the country, and in many cases, primary TKA was performed elsewhere, thus precluding the exact calculation of incidence of RTKA. The study only shows the volume of revision surgery at one center. In the absence of a national registry, such data are valuable in planning strategies for improving arthroplasty practices in our country. We did not review the outcomes of these revisions in this study; however, we plan to evaluate and to present these outcomes in our future studies. Major strength of our study is that it involved a dedicated research team, which interacted with the surgical team conducting the revisions, and therefore, the causes of revisions recorded are likely to be accurate and reliable.
Prosthetic infection remains the predominant cause of RTKA procedures performed between 2011 and 2016 in our center. Aseptic loosening and instability are a distant second and third cause for revision, respectively. There has been a significant increase in delayed and late-septic revisions caused by low-virulence organisms, predominantly Gram-negative. Due to the nature of the offending organism (fastidious Gram-negative organisms), most septic revisions required multiple surgical procedures, which has a tremendous socioeconomic impact. We need to utilize our resources and expertise in controlling prosthetic infections. We not only need to practice a multipronged approach to abate infections but also need to create adequate infrastructure and proficiency to satisfy the increasing need for RTKA in our population. We need to closely monitor the probable increase in aseptic revisions, which are likely to occur with increasing age of the patients.
Financial support and sponsorship
“This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.”
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR, et al. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991-2010. JAMA. 2012;308:1227–36. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hooper G, Lee AJ, Rothwell A, Frampton C. Current trends and projections in the utilisation rates of hip and knee replacement in New Zealand from 2001 to 2026. N Z Med J. 2014;127:82–93. [PubMed] [Google Scholar]
- 3.Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today – Has anything changed after 10 years? J Arthroplasty. 2014;29:1774–8. doi: 10.1016/j.arth.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 4.Bhandari M, Smith J, Miller LE, Block JE. Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord. 2012;5:89–94. doi: 10.4137/CMAMD.S10859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 6.Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gómez-Barrena E, et al. International survey of primary and revision total knee replacement. Int Orthop. 2011;35:1783–9. doi: 10.1007/s00264-011-1235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurtz SM, Gawel HA, Patel JD. History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res. 2011;469:2262–77. doi: 10.1007/s11999-011-1872-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le DH, Goodman SB, Maloney WJ, Huddleston JI. Current modes of failure in TKA: Infection, instability, and stiffness predominate. Clin Orthop Relat Res. 2014;472:2197–200. doi: 10.1007/s11999-014-3540-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oduwole KO, Molony DC, Walls RJ, Bashir SP, Mulhall KJ. Increasing financial burden of revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:945–8. doi: 10.1007/s00167-010-1074-8. [DOI] [PubMed] [Google Scholar]
- 10.Calliess T, Ettinger M, Hülsmann N, Ostermeier S, Windhagen H. Update on the etiology of revision TKA - Evident trends in a retrospective survey of 1449 cases. Knee. 2015;22:174–9. doi: 10.1016/j.knee.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Dalury DF, Pomeroy DL, Gorab RS, Adams MJ. Why are total knee arthroplasties being revised? J Arthroplasty. 2013;28:120–1. doi: 10.1016/j.arth.2013.04.051. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi AV, Jr, Berend KR, Adams JB. Why knee replacements fail in 2013: Patient, surgeon, or implant? Bone Joint J. 2014;96-B:101–4. doi: 10.1302/0301-620X.96B11.34350. [DOI] [PubMed] [Google Scholar]
- 13.Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, et al. Why are total knees failing today. Etiology of total knee revision in 2010 and 2011? J Arthroplasty. 2013;28:116–9. doi: 10.1016/j.arth.2013.04.056. [DOI] [PubMed] [Google Scholar]
- 14.Hossain F, Patel S, Haddad FS. Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res. 2010;468:1221–8. doi: 10.1007/s11999-009-1204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kasahara Y, Majima T, Kimura S, Nishiike O, Uchida J. What are the causes of revision total knee arthroplasty in Japan? Clin Orthop Relat Res. 2013;471:1533–8. doi: 10.1007/s11999-013-2820-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim KT, Lee S, Ko DO, Seo BS, Jung WS, Chang BK, et al. Causes of failure after total knee arthroplasty in osteoarthritis patients 55 years of age or younger. Knee Surg Relat Res. 2014;26:13–9. doi: 10.5792/ksrr.2014.26.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koh IJ, Cho WS, Choi NY, Kim TK Kleos Korea Research Group. Causes, risk factors, and trends in failures after TKA in Korea over the past 5 years: A multicenter study. Clin Orthop Relat Res. 2014;472:316–26. doi: 10.1007/s11999-013-3252-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Motififard M, Pesteh M, Etemadifar MR, Shirazinejad S. Causes and rates of revision total knee arthroplasty: Local results from Isfahan, Iran. Adv Biomed Res. 2015;4:111. doi: 10.4103/2277-9175.157829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, et al. New definition for periprosthetic joint infection: From the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011;469:2992–4. doi: 10.1007/s11999-011-2102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Registry N.J. National Joint Registry 11th Annual Report 2014. The National Joint Registry (NJR) for England, Wales, Northern Ireland, and the Isle of Man. 2014 [Google Scholar]
- 21.Culliford DJ, Maskell J, Beard DJ, Murray DW, Price AJ, Arden NK, et al. Temporal trends in hip and knee replacement in the United Kingdom: 1991 to 2006. J Bone Joint Surg Br. 2010;92:130–5. doi: 10.1302/0301-620X.92B1.22654. [DOI] [PubMed] [Google Scholar]
- 22.Patel A, Pavlou G, Mújica-Mota RE, Toms AD. The epidemiology of revision total knee and hip arthroplasty in England and wales: A comparative analysis with projections for the United States. A study using the National Joint Registry Dataset. Bone Joint J. 2015;97-B:1076–81. doi: 10.1302/0301-620X.97B8.35170. [DOI] [PubMed] [Google Scholar]
- 23.Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: Cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293–7. doi: 10.1302/0301-620X.93B3.25467. [DOI] [PubMed] [Google Scholar]
- 24.Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R, et al. Current failure mechanisms after knee arthroplasty have changed: Polyethylene wear is less common in revision surgery. J Bone Joint Surg Am. 2015;97:715–20. doi: 10.2106/JBJS.M.01534. [DOI] [PubMed] [Google Scholar]
- 25.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swedish Knee Arthroplasty Register. Lund, Sweden: 2011. [Last accessed on 2017 Mar 07]. http://www.knee.se . [Google Scholar]
- 27.Vergidis P, Patel R. Novel approaches to the diagnosis, prevention, and treatment of medical device-associated infections. Infect Dis Clin North Am. 2012;26:173–86. doi: 10.1016/j.idc.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang X, Wang Q, Wang H, Wang S, Zhong Q, Li Z, et al. Comparison and estimation of different diagnostic methods in detecting the presence of periprosthetic joint infection. Zhonghua Wai Ke Za Zhi. 2016;54:251–7. doi: 10.3760/cma.j.issn.0529-5815.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 29.Fraser JF, Werner S, Jacofsky DJ. Wear and loosening in total knee arthroplasty: A quick review. J Knee Surg. 2015;28:139–44. doi: 10.1055/s-0034-1398375. [DOI] [PubMed] [Google Scholar]
- 30.Patel A, Pavlou G, Mújica-Mota RE, Toms AD. The epidemiology of revision total knee and hip arthroplasty in England and Wales: A comparative analysis with projections for the United States. A study using the National Joint Registry Dataset. Bone Joint J. 2015;97-B:1076–81. doi: 10.1302/0301-620X.97B8.35170. [DOI] [PubMed] [Google Scholar]


