Abstract
Objective
To present a guiding framework from the perspective of psychologists and technologists to develop effective mobile health (mHealth) interventions for pediatric populations.
Methods
This topical review uses the IDEAS framework as an organizational method to summarize current strategies to conceptualize, design, evaluate, and disseminate mHealth interventions.
Results
Incorporating theories of behavior change and feedback from target populations are essential when developing mHealth interventions. Following user-centered approaches that fully incorporate end users into design and development stages increases the likelihood that the intervention will be acceptable. Iterative design cycles and prototyping are important steps to gather user feedback to optimize an mHealth intervention. Broad sharing of knowledge and products generated during intervention development also is recommended. Assessment of behavioral principles, intervention components, or a full intervention package should be conducted to evaluate usability and efficacy.
Conclusions
Pediatric health-care researchers and clinicians are increasingly using mHealth technology to target health behaviors and improve related outcomes. Pediatric psychologists should consider applying the design strategies outlined in the IDEAS framework to produce and disseminate mHealth interventions tailored to the specific needs of pediatric populations.
Keywords: computer applications/eHealth, health behavior, health promotion and prevention
Mobile health (mHealth) interventions have proliferated because of the ubiquity of personal digital technologies (e.g., smartphones). The majority of adults (77%) and adolescents (73%) in the United States use smartphones (Lenhart, 2015; Pew Research Center, 2018). Adolescents spend >2.5 hr a day on these devices (Rideout, 2015), highlighting the utility of mHealth as a modality to intervene in pediatric populations. mHealth interventions are a burgeoning area in pediatric psychology (Fedele, McConville, et al., 2018; Hilliard et al., 2018) and hold promise to improve health outcomes in youth. However, their effectiveness is variable (Fedele, Cushing, Fritz, Amaro, & Ortega, 2017), and the mere addition of mHealth technologies to an intervention protocol does not necessarily improve behavior change (Jakicic et al., 2016; Thomas et al., 2017). Creating effective and sustainable mHealth interventions is complex, requiring multidisciplinary expertise, navigation of interdependent development stages, and consideration of unique factors (e.g., technology costs and commercialization) (Michie, Yardley, West, Patrick, & Greaves, 2017).
Following a structured method to integrate technology with intervention delivery is essential in developing effective mHealth interventions (Mummah, Robinson, King, Gardner, & Sutton, 2016). There are a number of mHealth intervention design frameworks, including agile design (Hekler et al., 2016), user-centered approaches (i.e., approaches to application development that emphasizes the importance of understanding how the target user will experience the application and their preferred ways of using it) (van Gemert-Pijnen et al., 2011; Yardley, Morrison, Bradbury, & Muller, 2015), and the behavioral intervention technology model (Mohr, Schueller, Montague, Burns, & Rashidi, 2014), among others, that offer guidance on mHealth intervention development.
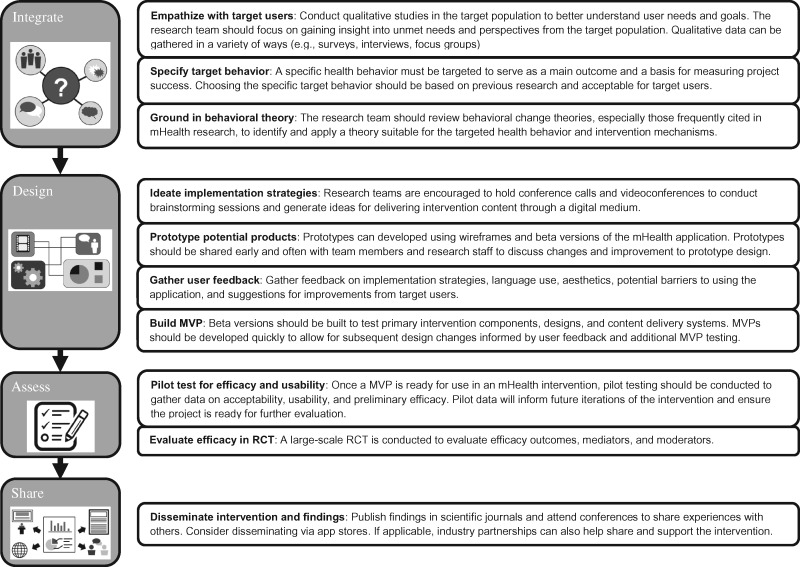
The goal of this review is to present a guiding framework from the perspective of psychologists and technologists to develop effective mHealth interventions for pediatric populations. We use the IDEAS framework (Mummah et al., 2016), a systematic, flexible, step-by-step mHealth intervention design framework as an organizational method to discuss common approaches to designing mHealth interventions. As outlined by Mummah et al. (2016), we chose to highlight the IDEAS framework instead of other mHealth intervention development models because of its comprehensiveness in guiding a researcher through the full life cycle of an mHealth project. Researchers have begun to use this framework to develop mHealth apps for pediatric populations (Gabrielli et al., 2017; Kazemi, Borsari, Levine, Lamberson, & Dooley, 2018). The IDEAS framework includes four multicomponent stages (Integrate, Design, Assess, and Share) to design and disseminate mHealth interventions for behavior change. We will discuss each stage and highlight examples of how principles of the IDEAS framework have been applied to pediatric mHealth interventions (Figure 1).
Figure 1.
Strategies and recommendations for using the IDEAS framework.
Gathering an Interdisciplinary Team
The critical initial step before embarking on the development of a pediatric mHealth intervention is convening a collaborative interdisciplinary team (Wu, Steele, Connelly, Palermo, & Ritterband, 2014). Pediatric psychologists often work in health-care settings on academic campuses and spend significant amounts of time collaborating with interdisciplinary medical teams. Pediatric psychologists are well positioned to partner with health-care providers and as part of an academic appointment may have access to technologists, engineers, and human–computer interaction researchers who would collaborate on mHealth projects. Designing mHealth interventions involves an iterative process with numerous decision points balancing behavioral theory, technological considerations, and user needs. Thus, an interdisciplinary team should establish frequent communication between members to minimize any miscommunication that may arise because of differences in nomenclature. A shared understanding of project goals and key intervention components will ensure development moves forward in a collaborative, professional, and expedient manner (Roess, 2017).
Integrate
The overarching goal of this foundational stage is to integrate feedback from target users (e.g., adolescents and parents) with principles of behavioral theory to inform the design of a mHealth intervention (Mummah et al., 2016). Formative research to understand the unmet needs of the population of interest is a cornerstone of developing mHealth interventions (Whittaker, Merry, Dorey, & Maddison, 2012). One or more of a variety of methods must be selected to gather stakeholder needs (e.g., focus groups, one-on-one interviews, and crowdsourcing) to better understand the perspective of target users and the factors that influence their engagement in health behaviors (e.g., self-management) (Brabham, Ribisl, Kirchner, & Bernhardt, 2014; Schnall et al., 2016). For example, Hilliard et al. (2018) conducted semi-structured qualitative interview with parents and adolescents with Type 1 diabetes before designing their mHealth app to compile input on desired features, content, and how the app would function to improve diabetes self-management. The needs identified by the target user population directly inform selection and operationalization of the target health behavior(s) that will be the focus of the mHealth intervention. The interdisciplinary team should strive to generate specific and measurable target behaviors that are likely to be accepted by target users and make a meaningful impact on outcomes of interest (Mummah et al., 2016). Finally, health behavior targets are incorporated with behavioral theory. The team may consider drawing from relevant theoretical models commonly used in pediatrics (e.g., social cognitive theory and social ecological approaches) or identifying plausible behavior change techniques (Michie, van Stralen, & West, 2011) that could be leveraged to target the identified health behavior(s) of interest. A shared understanding of the theoretical mechanisms of behavior change and their hypothesized course of action by the investigative team is a central goal to facilitate subsequent intervention design processes.
Design
The Design stage encompasses applying available resources most efficiently to realize the most appropriate mHealth configuration. After user needs have been compiled, they are evaluated relative to expert inputs for likely effectiveness, ranked by importance, and assessed for dependencies or conflicts. This process of grouping related needs of users and weighting by relative importance has been used in engineering for decades to facilitate designs that better incorporate the desires and expectations of target users (Hauser & Clausing, 1988). Solutions for each need are then generated during an ideation process (i.e., brainstorming). Through ideation, users, experts, and other relevant contributors (e.g., health-care providers) describe as many approaches to addressing each need as possible. Evaluation and preliminary selection of solutions occur in a second round of review that may engage additional experts. If possible, the leading and riskier solutions will be presented for feedback to users as mock-ups or limited prototypes that can directly capture rich and detailed information. Holtz et al. (2017), for example, presented a prototype of their mHealth app to both parents and adolescents with Type 1 diabetes to gather feedback on how it should be modified and what would motivate adolescents to use the app.
The selected set of solutions are next assembled into a “minimum viable product” (MVP), a term that refers to the minimum functionality believed to be required to meaningfully affect the targeted behavior(s). The MVP is a starting point for testing and iterative refinement, not a finalized intervention for dissemination. We used several MVPs during advisory board testing of the AIM2ACT smartphone app, an app for adolescents with poorly controlled asthma, after integrating user feedback related to intervention content and functionality from parents and adolescents (i.e., the target users; Fedele, McConville, et al., 2018). Work toward the MVP begins after initial completion of the Integrate and Design stages, the development team is assembled, and overall budget and schedule are agreed on. The schedule for an mHealth project is ideally built to accommodate an “agile” development process that allows for multiple rounds of quantifiable testing with users to provide actionable inputs to refine the design (Hekler et al., 2016).
Assess
Frequent assessment of the acceptability (e.g., satisfaction) and usability (e.g., operability) of mHealth intervention components from target users should occur during the iterative design phases. Common qualitative methods used to assess acceptability and usability include asking users to complete think aloud testing when interacting with the mHealth tool or conducting semi-structured interviews to evaluate user perspectives after they have had the opportunity to interact with the tool (Zapata, Fernández-Alemán, Idri, & Toval, 2015). As an example, Kenny et al. (2016) used focus group testing to gather adolescent feedback on the functionality and acceptability in response to a prototype mHealth app for monitoring mental health (e.g., mood). Quantitative approaches include examining usage patterns (e.g., frequency intervention components were used by participants) and questionnaires such as the System Usability Scale (Brooke, 1996). These data inform intervention refinements as development of the intervention progresses. mHealth projects allow for a uniquely rapid prototyping opportunity where users may be able to provide feedback on operable components in their natural context (e.g., at home and on their own smartphone).
Evaluating the efficacy of an mHealth intervention and/or its components to elicit meaningful changes in health behaviors or outcomes can take several forms (Michie et al., 2017). For example, initially, N-of-1 or single-arm pilot testing of an MVP in a small cohort of available target users can be used to examine whether the mHealth intervention produces hypothesized changes, generate estimates of intervention effect sizes, and gather important data on feasibility of the intervention protocol. A randomized controlled trial (RCT) with a fully developed mHealth intervention and larger sample of participants could be conducted to more formally evaluate intervention efficacy. Alternatively, given the high likelihood that an mHealth intervention would be outdated at the conclusion of a full-scale RCT, others have advocated for a stronger focus on assessment of underlying intervention principles (Mohr et al., 2015).
Share
Broad and open sharing of mHealth interventions and knowledge generated during their development and testing are encouraged. Many have argued for adopting a collective “early-and-often” sharing approach of MVP, computational models, algorithms, and other design components to achieve more efficient and rapid progress toward health behavior change (Hekler et al., 2016). This could include open sharing of code via GitHub (github.com) or offering free access to an mHealth platform (Mobile sensor data-to-knowledge (MD2K); md2k.org/software). Sharing a complete mHealth intervention can occur via the App Store or Google Play. The methods used to develop a mHealth intervention and key outcomes (e.g., acceptability and efficacy) should also be disseminated to the scientific community. Traditional approaches include presentations at national conferences and publishing in relevant journals (Mummah et al., 2016). As data sets are accrued, researchers are encouraged to post them online with appropriate safeguards for confidentiality, etc., so that others can contribute to analysis with different tools and perspectives.
Additional Considerations and Challenges
Researchers who embark on developing an mHealth intervention are likely to encounter a number of unanticipated challenges that arise during the project not fully captured via the design process. Holding to a process with which the team is already experienced provides resilience in the face of changes and unexpected difficulties. The principal investigator may benefit from learning some proven techniques of project management or team science to make best use of their time and ensure optimal contributions from team members (Hauser & Clausing, 1988). Resources are available that describe best practices in project initiation, operations, and maintenance if a researcher does not have access to formal training in project management (Cook, 2005). Second, it is recommended that investigators engage their local technology transfer office (if available) in the project at an early stage to review intellectual property rights and data use agreements. Third, navigating local Institutional Review Board and privacy office requirements to pursue the development and testing of a mHealth intervention can involve lengthy review periods because of institution-specific regulatory issues. For guidance on these issues, researches can look to Connected and Open Research Ethics (CORE; thecore.ucsd.edu), a network of shared resources, specifically related to emerging technologies in research. Finally, dissemination of mHealth interventions may be driven by commercial or research needs. Whereas the commercialization route emphasizes distributing mHealth products with industry partners for profit, dissemination highlights the need for products that are sustainable and effective. To better satisfy both ideals, pediatric psychologists can partner with commercial partners early to support their projects with funding and expertise. This, in many cases, requires varying degrees of infrastructure and support that can be burdensome for individual investigators. Commercialization through a business or nonprofit entity is one of the more effective and increasingly common options to apply appropriate resources to disseminate a functional form of an intervention.
Conclusions
mHealth interventions hold great promise for making a significant impact on the public health of children and adolescents. This review provides a targeted overview of mHealth intervention development to stimulate further interest in this innovative area of pediatric psychology. Interested readers are encouraged to pursue available interdisciplinary training opportunities in mHealth (e.g., National Institutes of Health mHealth Summer Training Institute) and consider attending conferences focused on the intersection of behavioral health and technology. Moving forward, there are several opportunities for future mHealth intervention research within pediatric psychology. Objective monitoring is commonly used within the field (e.g., actigraphy); however, integration of sensing with mobile intervention technology in pediatric psychology remains scarce. An inherent advantage of mobile technologies is the ability to assess and provide intervention in real time, when a person may be most in need of support (i.e., just-in-time) (Nahum-Shani et al., 2018). Moreover, the data processing abilities of mobile technologies give rise to opportunities to continuously adapt interventions over time to user needs. There are countless opportunities to leverage these features to develop dynamic, individually tailored interventions to improve common health behavior targets in pediatric psychology.
Funding
This work was supported in part by a grant from the National Institutes of Health (grant number 1R21HD083830-01A1).
Conflicts of interest: None declared.
References
- Brabham D. C., Ribisl K. M., Kirchner T. R., Bernhardt J. M. (2014). Crowdsourcing applications for public health. American Journal of Preventive Medicine, 46, 179–187. [DOI] [PubMed] [Google Scholar]
- Brooke J. (1996). SUS: A “quick and dirty” usability scale In Jordan P. W., Thomas B., Weerdmeester B. A., McClelland A. L. (Eds.), Usability evaluation in industry (pp. 189–194). London: Taylor & Francis. [Google Scholar]
- Cook C. R. (2005). Just enough project management : The indispensable four-step process for managing any project, better, faster, cheaper. New Delhi: McGraw-Hill. [Google Scholar]
- Fedele D. A., Cushing C. C., Fritz A., Amaro C. M., Ortega A. (2017). – interventions for improving health outcomes in youth. JAMA Pediatrics, 171, 461.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedele D. A., McConville A. G., Thomas J., McQuaid E. L., Janicke D. M., Turner E. M., Moon J., Abu-Hasan M. (2018). Applying interactive mobile health to asthma care in teens (AIM2ACT): Development and design of a randomized controlled trial. Contemporary Clinical Trials, 64, 230–237. 10.1016/j.cct.2017.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrielli S., Dianti M., Maimone R., Betta M., Filippi L., Ghezzi M., Forti S. (2017). Design of a mobile app for nutrition education (TreC-LifeStyle) and formative evaluation with families of overweight children. JMIR MHealth and UHealth, 5, e48.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser J. R., Clausing D. (1988). The house of quality. Harvard Business Review, 66, 63–73. [Google Scholar]
- Hekler E. B., Klasnja P., Riley W. T., Buman M. P., Huberty J., Rivera D. E., Martin C. A. (2016). Agile science: Creating useful products for behavior change in the real world. Translational Behavioral Medicine, 6, 317–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard M. E., Eshtehardi S. S., Minard C. G., Saber R., Thompson D., Karaviti L. P., Rojas Y., Anderson B. J. (2018). Strengths-based behavioral intervention for parents of adolescents with type 1 diabetes using an mhealth app (type 1 doing well): Protocol for a pilot randomized controlled trial. JMIR Research Protocols, 7, e77.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtz B. E., Murray K. M., Hershey D. D., Dunneback J. K., Cotten S. R., Holmstrom A. J., Vyas A., Kaiser M. K., Wood M. A. (2017). Developing a patient-centered mhealth app: A tool for adolescents with type 1 diabetes and their parents. JMIR MHealth and UHealth, 5, e53.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakicic J. M., Davis K. K., Rogers R. J., King W. C., Marcus M. D., Helsel D., Rickman A. D., Wahed A. S., Belle S. H. (2016). Effect of wearable technology combined with a lifestyle intervention on long-term weight loss. JAMA, 316, 1161–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemi D. M., Borsari B., Levine M. J., Lamberson K. A., Dooley B. (2018). REMIT: Development of a mHealth theory-based intervention to decrease heavy episodic drinking among college students. Addiction Research and Theory, 26, 377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny R., Dooley B., Fitzgerald A. (2016). Developing mental health mobile apps: Exploring adolescents’ perspectives. Health Informatics Journal, 22, 265–275. [DOI] [PubMed] [Google Scholar]
- Lenhart A. (2015). Teens, social media & technology overview 2015. Retrieved from http://www.pewinternet.org/2015/04/09/teens-social-media-technology-2015/ [Google Scholar]
- Michie S., van Stralen M. M., West R. (2011). The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science, 6, 42 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Yardley L., West R., Patrick K., Greaves F. (2017). Developing and evaluating digital interventions to promote behavior change in health and health care: Recommendations resulting from an international workshop. Journal of Medical Internet Research, 19, e232.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D. C., Schueller S. M., Montague E., Burns M. N., Rashidi P. (2014). The behavioral intervention technology model: An integrated conceptual and technological framework for eHealth and mHealth interventions. Journal of Medical Internet Research, 16, e146.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D. C., Schueller S. M., Riley W. T., Brown C. H., Cuijpers P., Duan N., Kwasny M. J., Stiles-Shields C., Cheung K. (2015). Trials of intervention principles: Evaluation methods for evolving behavioral intervention technologies. Journal of Medical Internet Research, 17, e166.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mummah S. A., Robinson T. N., King A. C., Gardner C. D., Sutton S. (2016). IDEAS (Integrate, Design, Assess, and Share): A framework and toolkit of strategies for the development of more effective digital interventions to change health behavior. Journal of Medical Internet Research, 18, e317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahum-Shani I., Smith S. N., Spring B. J., Collins L. M., Witkiewitz K., Tewari A., Murphy S. A. (2018). Just-in-Time Adaptive Interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Annals of Behavioral Medicine, 52, 446–462. 10.1007/s12160-016-9830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. (2018). Demographics of mobile device ownership and adoption in the United States. Retrieved from http://www.pewinternet.org/fact-sheet/mobile/. Retrieved April 13, 2018.
- Rideout V. (2015). The common sense census: Media use by tweens and teens Retrieved from https://www.commonsensemedia.org/research/the-common-sense-census-media-use-by-tweens-and-teens
- Roess A. (2017). The promise, growth, and reality of mobile health—Another data-free zone. New England Journal of Medicine, 377, 2010–2011. [DOI] [PubMed] [Google Scholar]
- Schnall R., Rojas M., Bakken S., Brown W., Carballo-Dieguez A., Carry M., Gelaude D., Mosley J. P., Travers J. (2016). A user-centered model for designing consumer mobile health (mHealth) applications (apps). Journal of Biomedical Informatics, 60, 243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas J. G., Raynor H. A., Bond D. S., Luke A. K., Cardoso C. C., Foster G. D., Wing R. R. (2017). Weight loss in Weight Watchers Online with and without an activity tracking device compared to control: A randomized trial. Obesity, 25, 1014–1021. [DOI] [PubMed] [Google Scholar]
- van Gemert-Pijnen J. E. W. C., Nijland N., van Limburg M., Ossebaard H. C., Kelders S. M., Eysenbach G., Seydel E. R. (2011). A holistic framework to improve the uptake and impact of eHealth technologies. Journal of Medical Internet Research, 13, e111.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittaker R., Merry S., Dorey E., Maddison R. (2012). A development and evaluation process for mhealth interventions: Examples from New Zealand. Journal of Health Communication, 17, 11–21. [DOI] [PubMed] [Google Scholar]
- Wu Y. P., Steele R. G., Connelly M. A., Palermo T. M., Ritterband L. M. (2014). Commentary: Pediatric eHealth interventions: Common challenges during development, implementation, and dissemination. Journal of Pediatric Psychology, 39, 612–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yardley L., Morrison L., Bradbury K., Muller I. (2015). The person-based approach to intervention development: application to digital health-related behavior change interventions. Journal of Medical Internet Research, 17, e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapata B. C., Fernández-Alemán J. L., Idri A., Toval A. (2015). Empirical studies on usability of mhealth apps: A systematic literature review. Journal of Medical Systems, 39, 1.. 10.1007/s10916-014-0182-2 [DOI] [PubMed] [Google Scholar]